Abstract
While there have been significant advances in curbing the HIV disease epidemic worldwide, there continues to be significant number of incident cases with 2.3 million new infections in the year 2012 alone. Treatment as prevention (TasP), which involves the use of antiretroviral drugs to decrease the likelihood of HIV illness, death and transmission from infected individuals to their noninfected sexual and /or drug paraphernalia-sharing injecting partners, must be incorporated into any HIV prevention strategy that is going to be successful on a large scale. Especially in resource-limited settings, the focus of the prevention approach should be on high-risk groups who contribute disproportionately to community HIV transmission, including people who inject drugs (PWID), men who have sex with men (MSM) and sex workers. Innovative strategies including integrated care services adapted to different patient care settings have to and can be employed to reach these at-risk populations.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Even in the fourth decade of the HIV pandemic, there continues to be an unacceptably high number of incident cases—50,000 in the US and 2.3 million globally; the latter number is equivalent to 2 % of babies born worldwide each year [1–3]. In the USA, the number of newly diagnosed HIV cases has not changed over the past 15 years! This is despite reports of 362,000 infections averted by prevention efforts between 1991 and 2006 [4–6]. While there has been much progress in global scale up of HIV testing, expanding access to antiretroviral therapy (ART) and resultant life expectancy gains, there is still much work left to be done [7–9]. In some regions of the world, there are still more individuals acquiring HIV than are initiated on ART [10].
It is increasingly recognized that current global HIV prevention and control strategies are insufficiently applied (e.g. syringe exchange, condom use, etc.) to halt the transmission of HIV infection and achieve the goal of an AIDS-free generation. The emphasis has traditionally been on scaling up and expanding HIV testing and treatment services while prevention efforts have not been equally advanced. Among certain vulnerable and high-risk groups, including people who inject drugs (PWID), prisoners, female sex workers and men who have sex with men (MSM), there is concern that transmission rates will plateau or continue to increase despite an overall global decline in HIV incidence [2].
The development of highly active ART was a quantum surge in reducing morbidity and mortality related to HIV, and the expansion of treatment remains a critical priority for the millions infected with HIV. ART was found to have efficacy in reducing the transmission of HIV to uninfected individuals in the mid-1990s in the context of preventing the vertical HIV transmission from mother to child [11]. More recent data has brought treatment as prevention (TasP) to new levels of prominence following the HPTN 052 trial. This trial demonstrated a phenomenal 96 % reduction in linked HIV transmission among serodiscordant, predominantly heterosexual African couples when the infected partner was treated with ART [12].
TasP has since been incorporated into national and international guidelines for HIV disease management. There is now renewed focus by governments, funding agencies and advocacy groups on this unique approach to HIV prevention [13]. There remain significant obstacles to widespread adoption of TasP, however, including challenges with the identification of infected individuals, linking them to care, access to ART, optimal medication adherence and achievement of fully suppressed viral loads which are in and of themselves prerequisites for its success [14]. An alternative universal test and treat strategy, advocated by some and in which all individuals who test positive for HIV infection are treated as soon as detected, overlaps with the goals of TasP, and together, they represent a new prevention effort paradigm shift [15, 16].
The HIV Care Gap and Vulnerable Populations
The gains in HIV treatment outcomes have not been uniform across patient risk groups. While there are no reliable global estimates on HIV treatment coverage for vulnerable populations—PWID, MSM and sex workers (SWs)—there are reports which suggests that coverage is suboptimal, if not dismal [2]. Understanding the critical role that vulnerable populations play in the on-going HIV epidemic, it is concerning that reliable global estimates are lacking.
PWID are disproportionately impacted by the HIV epidemic. They account for 10 % of prevalent HIV cases globally while only representing 0.34 % of the population [17]. PWID have also experienced lower life expectancy gains compared to noninjecting HIV counterparts in the era of ART [8]. While this is not solely due to HIV-related morbidity, there are well-reported disparities in care. Of the 11–21.2 million PWID worldwide, 0.8–6.6 million acquire HIV annually but only 4 per 100 (range 2–18) are on ART with disproportionately poor coverage in low-resource countries [18]. It is well known that to successfully address HIV prevention and treatment among this population, integrated medication-assisted treatment (MAT) and needle-syringe exchange programmes (NSPs) are key [19–21]. Tragically, however, the implementation of key interventions with maximal impact such as combined ART, MAT and NSP [22] virtually never occur together in an integrated environment operationalized on a scale to impact HIV incidence. MAT access alone, which focuses predominantly on opioid use, is limited globally with only 13 % of middle east and north African countries, 16 % of Caribbean nations, 27 % of Sub-Saharan African, and 48 % of Eastern European countries offer MAT to PWID [18]. Coverage in many of those countries is dismal where programmes remain in the “pilot” stage and have failed to scale up to a meaningful number able to address the HIV epidemic [23]. There continues to be high rates of stigma and discrimination against PWID who are often unacknowledged by policy makers with resultant inaction.
A similar disparity has been observed among MSM. These men are, as a demographic, disproportionately impacted by the epidemic, and in the USA, the rates of HIV infection among MSM of colour has increased to the point where they now constitute the majority of incident cases [24, 25]. It has been reported that an alarming 48 % of MSM with HIV are unaware of their status [26]. Awareness of status appears to be lost in the life of many MSM amidst a host of other factors including stigma, discrimination, disparities in care, socioeconomic factors (joblessness, low income and lack of health insurance) and high rates of incarceration. An increase in risky sexual behaviours fuelled by drug and alcohol use and high HIV prevalence in sexual networks has driven these incidence trends [26–28]. Some individuals who are aware of their infection status continue to engage in unprotected anal intercourse [29, 30]. Furthermore, the internet age has increased sexual networking and as such innovative strategies to reach MSMs in the digital age are needed [31, 32].
Complicating HIV prevention efforts in these vulnerable populations are that they frequently have multiple and overlapping risk behaviours. PWID also engage in sex and MSM and sex workers may engage in risky drug and alcohol use; therefore, multimodal interventions that understand the complexities of drug and sexual behaviours are important if interventions are to be effective [21]. Some studies have found that while MAT and NSP impact risks of HIV acquisition through needle sharing, they may have lesser impact on sexual risk behaviours [33]. Further confounding matters among PWID is the reality that not all MAT is equal, with new data favouring methadone over buprenorphine for HIV prevention [34] and MAT successfully addresses opioid users who are only a portion of the global PWID. Sexual relationships are equally as complicated with individuals forgoing HIV barrier protection such as condoms because they change the sexual experience.
In a world where MAT and NSP are not available at the scale that is required and barrier protection for HIV is unpopular because it changes the sexual experience, it is clearly time to build into global HIV prevention other evidence-based initiatives such as TasP. Regardless of CD4 count, TasP should be instituted as a component of HIV prevention for these high-risk groups given the high prevalence of HIV in these populations and their impact upon the epidemic [17]. And, while there are adherence concerns, the success of HIV pre-exposure prophylaxis (PrEP) debunks the often-held presumption that active PWID cannot and do not adhere to medical therapy [35].
Expanding HIV Testing: Challenges and Promise
Despite a large investment of human and financial capital globally, a significant proportion of individuals with HIV infection are unaware of their status. Estimates range from 15.8 % in the USA to 61 % in some countries in Sub-Saharan Africa [36, 37]. This is a critical statistic as only individuals who are aware of their infection status can be linked to care and treated in a TasP model.
The optimal strategy to improve HIV case detection rates is universal opt-out testing. Since 2006, the CDC has recommend this method of testing which has been shown to be an effective approach to detect cases and is cost effective for areas with HIV prevalence rates >0.1 % [38]. Universal testing may also help to destigmatize the process since everyone is offered testing. Unfortunately, support for this strategy by guideline issuing agencies does not always significantly influence clinicians’ behaviour [39]. Studies have shown that opt-out testing is well accepted and results in improved testing rates compared to opt-in testing.
To successfully implement universal HIV testing, creative and strategic methods tailored to individual locales are needed. The reliance upon physicians and nurses to conduct testing and health interventions must end. Many individuals with HIV do not attend medical clinics until they have AIDS and many clinics are populated with staff that does not have open attitudes towards sexual behaviour and drug use. Multi-modal community health campaigns have been demonstrated as successful models to test large components of a population for HIV and other diseases [40]. These community-based approaches including door-to-door visits and mobile testing or at strategic sites such as the workplace, schools and gay sex clubs may be necessary to reach everyone. One large systematic review assessing first-time testing acceptance rates of community-based HIV testing showed rates ranging from 62 to 88 % and increased HIV testing and uptake compared to facility-based approaches (RR-10.65, 95 % confidence interval 6.27–18.08) [41]. The lowest acceptance rates were observed in schools (62 %) and workplace settings (67 %). Studies like these inform appropriate highest yield sites for HIV testing.
Testing initiatives must also be tailored to high-risk individuals for whom annual testing is recommended. Strategies particularly effective in high-risk individuals such as PWID, MSM and SW must also be prioritized. Programmes like opt-out testing for HIV among PWID entering into methadone treatment is one example [42].
Lastly, factors which impact testing include stigma, cultural and religious beliefs, language barrier, an individual’s perception of risk and knowledge of HIV testing, the doctor-patient relationship, testing in suitable sites and maintenance of anonymity [43]. Arguably, not all of these are modifiable, however, proven interventions including using a testing team familiar to patients, making testing cheap and convenient such as with point-of-care tests, preserving confidentiality, provision of linguistic and culturally appropriate services, and credible tests can all improve testing rates [44].
Modelling the Impact of Universal ART Coverage on HIV Disease Transmission and Prevalence
The proof of concept on the impact of increased ART use on preventing HIV transmission was seen in ecologic models where countries with high ART coverage rates have lower incident cases of HIV compared to those with lower ART coverage rates. Ecological studies, however, are subject to fallacies and, as a result, have been the subject of controversy. Observational studies have also shown a similar relationship. A population-based survey in British Columbia showed that between 1996 and 2009, there was a 547 % increase in ART use and a 52 % decrease in incident cases [45]. For every 100 individuals on ART, new HIV diagnoses declined by a factor of 0.97 (95 % CI 0.96–0.98) [45]. A similar survey performed in San Francisco also showed that a decrease in “community” HIV viral load was associated with a significant decline in new HIV diagnoses [46]. Importantly, Tanser and colleagues were able to directly measure the time to HIV sero-conversion in each individual in a cohort of over 16,000 patients in KwaZulu-Natal, thereby controlling for a wide range of possible individual-level confounders and providing strong evidence for higher levels of ART coverage [47]. This study found that an HIV-uninfected individual who is living in a community with 30 to 40 % ART coverage of all HIV-infected individuals saw a 38 % reduction in HIV acquisition compared to someone living in a low ART coverage community (<10 % on ART).
The impact of TasP for other HIV transmission risk groups such as MSM and PWID has not been sufficiently explored. A large retrospective observational study in China involving 38,682 serodiscordant couples over 101,295 person years of follow-up showed a 26 % reduction in HIV transmissions where the infected partner was treated with ART [48].
Montaner et al., using a population-based prevention-centred model based on TasP, showed that if all HIV infected people worldwide were treated with ART, in a 45-year period, the worldwide prevalence of HIV would decline from 7 cases to 0.1 cases per thousand people; that is a reduction from 38 million to 1 million individuals [49]. This optimistic model made certain unrealistic assumptions including that no transmissions would occur after the first year of roll out of the programme and that cheaper generic antiretrovirals would be universally available. Granich et al. tested a model based on parameters in South Africa, a high prevalence HIV setting, with more realistic estimates for ART uptake and coverage including allowing for ART refusal and treatment drop outs due to drug resistance, poor tolerability and adherence, and showed that to achieve an R o <1 (R o being the number of secondary cases resulting from a primary case), all adolescents and adults would have to be tested annually and ART initiation at time of diagnosis. In the latter model, with 90 % coverage, the HIV epidemic would be driven to an elimination phase in 1–2 years and there would be a 95 % reduction in incident cases in 10 years [50]. These studies are helpful as they help define the minimum level of coverage required to achieve a prespecified impact on HIV prevalence.
Prevailing issues which are not fully elucidated and hard to capture in models include the transmission implications of viral blips which occur in treated persons, the impact of secondary drug resistance on disease transmission, and the recognized phenomena of pill fatigue and diminishing ART adherence rates which surely occurs over time. Also, because TasP is usually a component of multiple interventions including risk reduction counselling, as was done in the HPTN-052 trial, the directly attributable impact on HIV transmission may be overestimated.
Patient Selection
Understanding that key populations such as PWID, MSM and sex workers may act as drivers of the HIV epidemic in many locations, these populations should be prioritized for ART both for the treatment of their own HIV but also for the public health benefit in reducing transmission [22]. Tanzania’s HIV epidemic among PWID highlights this where approximately 5.6 % of the population in Tanzania, 9 % in Dar es Salaam and 42 % of PWID in Dar es Salaam have HIV (the rates among the female subpopulation are over 60 % and pull up the lower, relative to the women, HIV prevalence among men) [51]. These high rates of HIV among PWID clearly create the possibility of a destabilization of the HIV epidemic in Dar es Salaam and are what prompted the creation of MAT programmes to address PWID risks. In addition to protecting others, recent evidence suggests that the earlier use of ART at higher CD4 counts may mitigate the adverse effects of uncontrolled HIV viremia and resultant exaggerated immune activation. This immune activation is thought to be causal or contributory to observed premature aging, development of HIV-associated neurologic complications, increased rates of non AIDS-defining cancers and cardiovascular disease [52].
In an era when treatment exists which both benefits the individuals infected with the disease as well as people who come into contact with that individual, the larger question is as follows: why would anyone deny treatment given these benefits? This combination health benefit and prevention benefit positioned the US Department of Health and Human Services (DHHS) to strongly recommend the use of TasP for all transmission risk groups including PWID and MSMs based on expert opinion [53].
An inherent problem with patient identification and evaluation for TasP is the low uptake of testing among PWID, SW or MSM, often linked to an understandable reluctance to disclose their sexual and injection use practices for varying reasons including the fear of being stigmatized and or discriminated against by their providers and their community [54]. These vulnerable populations may have multiple risk factors for HIV transmission at the same time and need to be assessed tactfully. The good news is that clinicians can be successfully trained to elicit behavioural risks to overcome this problem [13]. More importantly, if treatment is expanded widely irrespective of immunological status, the need to disclose risk categories may diminish overtime and this may make accessing testing and treatment even more palatable for some.
TasP Implementation Challenges/Resource Considerations
Funding levels for HIV care and prevention have increased remarkably on a global scale in the recent decade, and donors and governments must work in concert to maximize support and move towards universal access to care for all infected individuals [50]. The irony of the AIDS epidemic is that it disproportionately impacts countries with the least resources to combat the scourge. UNAIDS reports that 51 countries worldwide depended on international sources for three quarters of HIV-related spending in 2012 and donor countries must continue their support if civil society will achieve zero new HIV infections [2]. Prioritizing and channelling resources to the most effective interventions must be performed, especially for low-income countries and for vulnerable populations [55]. Models exist in mobilizing ART and MAT to drug users in resource-limited settings [56, 57]. On-going work in Tanzania has demonstrated the ability to integrate both HIV and tuberculosis care into the MAT clinic to increase access to care and treatment [42].
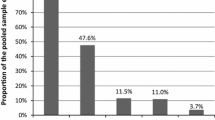
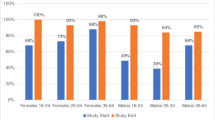
The provocative 2011 “Gardner cascade” of HIV care elegantly showed the dismal real-life performance of current HIV treatment strategies in achieving disease control in infected individuals but its greatest contribution, in our opinion, was revealing the different “drop-off” points in the continuum of care that could guide prioritization and targeting of responses to improve observed deficiencies in the status quo [58]. Most, if not all, of the problems plaguing current care strategies impact TasP implementation. These include under-identification of infected individuals, suboptimal linkage to and retention in care, limited availability of ART and infrastructure to support their use and inadequate adherence support and monitoring. Many governments are already struggling under the weight of new WHO guidelines on treatment initiation, finding the increased number of individuals they need to treat a daunting task in a resource-constrained environment. The number of individuals eligible for ART under a TasP strategy would further increase the number of individuals governments would be required to treat; however, this burden must be balanced with the reality that individuals who remain untreated will have resultant morbidity and mortality as well as loss in productivity which is costly and was preventable. Although daunting, governments with struggling health care infrastructure must redouble their efforts.
Cost-effectiveness analyses for TasP have been performed for general populations [59–61] as well as populations at greater risk of HIV, such as PWID [62]. Long et al. found that expanded use of ART among PWID in St. Petersburg, Russia, could prevent 40,000 infections, but a failure to increase ART would result in a growing HIV epidemic among PWID. Unfortunately, ART remains difficult for HIV-infected PWID in Russia to obtain [63]. Lack of ART coupled with the ongoing inability to obtain MAT with methadone and buprenorphine for Russian PWID, due to both being illegal in the Russian Federation, means a reduction in the HIV epidemic among PWID in Russia remains scant.
Although an intervention may be cost-effective, there remains a cost that some governments may not be able to afford. Simply put, the cheaper the intervention, the more individuals that can be reached by that intervention. The decreasing costs of ART with the availability of generics has resulted in an increase in the availability of ART globally. Additionally, lower delivery costs are necessary to get the medication from the site of manufacturing, through the supply chain, to the clinical environment and finally to the patient. An on-going project in Tanzania is examining a cost-containment strategy for clinical staff so that financial resources can be maximally utilized to increase the volume of PWID onto MAT. In many low-resource settings, buy-in from policy makers including local, state and national governments are necessary for the implementation and success of large-scale interventions. Until universal testing is operationalized, working to move higher-risk groups “to the front of the line” to increase testing and access to treatment is an important step. Stigma, however, may limit the number of high-risk groups that are willing to be identified and move up in the line for testing. Again, universal testing and access to treatment protects everyone. The sex worker obtained HIV from someone, but she would not have been infected had that sexual partner known his status and had been on ART.
Making It Work
With the anticipated increase in HIV treatment eligibility under a TasP strategy, there needs to be a concurrent changes in resources—human (e.g. task shifting, changes in delivery models) and material (simplification of protocols, reductions in cost of medications and medication delivery)—as well as the challenge of prescription and provision of ART. In addition, effective, efficient and sustainable care-delivery models will have to be developed and implemented.
From a human resource standpoint, a trained, versatile and skilled health care provider workforce is essential [64]. Nurse practitioners and physician assistants should be utilized as primary care providers and have been shown to offer excellent HIV management that parallels that of expert physicians [65]. Involvement of the entire health care community is essential as many locations cannot depend solely upon primary care physicians, let alone infectious diseases or HIV experts, in the care of HIV-infected patients. Task shifting to community stakeholders such as community health workers will contribute to enlarging the provider workforce [66, 67].
The use of incentives [68], mobile services [69, 70], home visits [71], targeted messaging (brochures, verbal and cell phone text messages) [32, 72, 73] and directly observed therapy (DOT) [42, 74–76] are some innovative strategies which have been shown to be effective for HIV testing, treatment and/or adherence support for hard-to-reach populations and should be adapted where possible. Multidisciplinary care facilities that offer case management, mental health, drug counselling and treatment services are more likely to be successful than those without them [77]. Furthermore, important social determinants of engagement in care such as homelessness or poor living situation, lack of health insurance and unemployment need to be addressed [78]. In our clinical experience, these factors are significant barriers to engagement in care of hard-to-treat populations and once addressed can result in a remarkable turnaround in patient care outcomes.
Concerns About Universal TasP Strategy
There are some concerns regarding the widespread implementation of TasP that have been discussed elsewhere [17]. One of the most stubborn objections is the fear of nonadherence and the development of resistance. PWID can be adherent to treatment and individuals who do not use drugs can struggle with adherence [79]. Interventions exist to support even the most difficult patient if such support is needed [17, 76, 80]. The fear of nonadherence and the development of resistance are insufficient reasons to deny treatment. Knowing that treatment is efficacious and that MSM, PWID and sex workers all have the same right to health as everyone else, it is the responsibility of civil society to provide treatment in a manner in which those in need may benefit.
Ethical Considerations
PWID, MSM and sex workers have historically been isolated from treatment as the stigma of their behaviours acts a barrier to governments and the public wanting to provide needed clinical care [63]. TasP, while including the prevention of morbidity and mortality to the individual, extends the benefits of ART to their drug and sexual partners. Not only does beneficence require that we provide access to HIV treatment for those in need regardless of how HIV was acquired, but also there is a duty to the partners of the HIV-infected person. In a world with discrimination and violence, many individuals may be afraid to disclose their behaviours or HIV status. With TasP, that individual lives a healthier life on ART and the transmission of HIV is drastically reduced even if the individual does not want to disclose that she injects drugs with others, engages in sex work to support her family etc. To refrain from providing treatment is to do harm, harm to both the individual in need of treatment and harm to her partners who obtained HIV due to a lack of public health interventions and TasP implementation.
Future ART Options and Impact on TasP
Until an effective vaccine or cure is available, ART must remain a cornerstone of HIV prevention and control efforts. The development of longer-acting and safer ART may not eliminate but should improve long-term medication adherence and make universal adoption and implementation of TasP a more palatable and achievable HIV prevention strategy [81, 82]. Such newer antiretroviral agents include long-acting formulations of the nonnucleoside reverse transcriptase inhibitor, rilpivirine and GSK-744, an integrase inhibitor, which may be administered once every 3 months [81]. A pro-drug formulation of tenofovir disoproxil fumarate (tenofovir alafenamide), a favoured HIV PrEP drug, is currently being evaluated in phase 3 clinical trials and is expected to have less toxicity than its predecessor [83].
Conclusion
TasP represents a win-win strategy for HIV disease control and prevention with mutual benefit to the infected individual and the uninfected community as a whole. Understanding the key role that PWID, MSM and SW play in the epidemic, a prioritizing of TasP for these groups is needed. Widespread ART use can be an effective strategy to significantly reduce and potentially eradicate HIV transmission in the community. Concerted and collective efforts by all stakeholders including patients, the medical community, nongovernmental organizations and governments—local, state and national—will be important to ensure the implementation and success of TasP.
References
HIV surveillance—United States, 1981–2008. MMWR Morb Mortal Wkly Rep. 2011;60(21):689–93.
Global report: Unaids report on the global aids epidemic 2013. Press Release; 2013. http://www.unaids.org/en/media/unaids/contentassets/documents/epidemiology/2013/gr2013/UNAIDS_Global_Report_2013_en.pdf.
World fertility data 2012. 2013. http://www.un.org/esa/population/publications/WFD2012/MainFrame.html.
Farnham PG, Holtgrave DR, Sansom SL, Hall HI. Medical costs averted by HIV prevention efforts in the United States, 1991–2006. J Acquir Immune Defic Syndr. 2010;54(5):565–7.
Lansky A, Brooks JT, DiNenno E, Heffelfinger J, Hall HI, Mermin J. Epidemiology of HIV in the United States. J Acquir Immune Defic Syndr. 2010;55 Suppl 2:S64–8.
Hall HI, Song R, Rhodes P, Prejean J, An Q, Lee LM, et al. Estimation of HIV incidence in the United States. JAMA J Am Med Assoc. 2008;300(5):520–9.
Mills EJ, Bakanda C, Birungi J, Chan K, Ford N, Cooper CL, et al. Life expectancy of persons receiving combination antiretroviral therapy in low-income countries: a cohort analysis from Uganda. Ann Intern Med. 2011;155(4):209–16.
Samji H, Cescon A, Hogg RS, Modur SP, Althoff KN, Buchacz K, et al. Closing the gap: increases in life expectancy among treated HIV-positive individuals in the United States and Canada. PLoS One. 2013;8(12):e81355.
Life expectancy of individuals on combination antiretroviral therapy in high-income countries: a collaborative analysis of 14 cohort studies. Lancet. 2008;372(9635):293–99.
Getting to zero: HIV in eastern and Southern Africa. Press Release; 2013. http://www.unicef.org/esaro/Getting-to-Zero-2013.pdf.
Connor EM, Sperling RS, Gelber R, Kiselev P, Scott G, O’Sullivan MJ, et al. Reduction of maternal-infant transmission of human immunodeficiency virus type 1 with zidovudine treatment. Pediatric aids clinical trials group protocol 076 study group. N Engl J Med. 1994;331(18):1173–80.
Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365(6):493–505.
van Asten L, Prins M. Infection with concurrent multiple hepatitis c virus genotypes is associated with faster HIV disease progression. AIDS. 2004;18(17):2319–24.
McNairy ML, Cohen M, El-Sadr WM. Antiretroviral therapy for prevention is a combination strategy. Curr HIV/AIDS Rep. 2013;10(2):152–8.
Dodd PJ, Garnett GP, Hallett TB. Examining the promise of HIV elimination by ‘test and treat’ in hyperendemic settings. AIDS. 2010;24(5):729–35.
Hayes R, Sabapathy K, Fidler S. Universal testing and treatment as an HIV prevention strategy: research questions and methods. Curr HIV Res. 2011;9(6):429–45.
Bruce RD. Is it time for treatment as prevention among people who inject drugs? J Acquir Immune Defic Syndr. 2013;63(5):545–7.
Mathers BM, Degenhardt L, Ali H, Wiessing L, Hickman M, Mattick RP, et al. Hiv prevention, treatment, and care services for people who inject drugs: a systematic review of global, regional, and national coverage. Lancet. 2010;375(9719):1014–28.
Baral SD, Stromdahl S, Beyrer C. The potential uses of preexposure prophylaxis for HIV prevention among people who inject drugs. Curr Opin HIV AIDS. 2012;7(6):563–8.
Stimson GV, Fitch C, DesJarlais D, Poznyak V, Perlis T, Oppenheimer E, et al. Rapid assessment and response studies of injection drug use: knowledge gain, capacity building, and intervention development in a multisite study. Am J Public Health. 2006;96(2):288–95.
Huang YF, Yang JY, Nelson KE, Kuo HS, Lew-Ting CY, Yang CH, et al. Changes in HIV incidence among people who inject drugs in Taiwan following introduction of a harm reduction program: a study of two cohorts. PLoS Med. 2014;11(4):e1001625.
Kato M, Granich R, Bui DD, Tran HV, Nadol P, Jacka D, et al. The potential impact of expanding antiretroviral therapy and combination prevention in Vietnam: towards elimination of HIV transmission. J Acquir Immune Defic Syndr. 2013;63(5):e142–9.
Parsons D, Burrows D, Bolotbaeva A. Advocating for opioid substitution therapy in central Asia: much still to be done. Int J Drug Policy. 2014.
Rhodes SD, Hergenrather KC, Vissman AT, Stowers J, Davis AB, Hannah A, et al. Boys must be men, and men must have sex with women: a qualitative cbpr study to explore sexual risk among African American, Latino, and white gay men and MSM. Am J Men’s Health. 2011;5(2):140–51.
Maulsby C, Millett G, Lindsey K, Kelley R, Johnson K, Montoya D, et al. A systematic review of HIV interventions for black men who have sex with men (MSM). BMC Public Health. 2013;13(625).
Phillips 2nd G, Wohl A, Xavier J, Jones K, Hidalgo J. Epidemiologic data on young men of color who have sex with men. AIDS Patient Care STDs. 2011;25 Suppl 1:S3–8.
HIV prevention among Black/African American gay, bisexual, and other men who have sex with men: highlights of activities of the centers for disease control and prevention. Atlanta; 2013. http://www.cdc.gov/hiv/risk/racialethnic/aa/brief/index.html.
Scheer S, Kellogg T, Klausner JD, Schwarcz S, Colfax G, Bernstein K, et al. HIV is hyperendemic among men who have sex with men in San Francisco: 10-year trends in HIV incidence, HIV prevalence, sexually transmitted infections and sexual risk behaviour. Sex Transm Infect. 2008;84(6):493–8.
Cunha CB, De Boni RB, Guimaraes MR, Yanavich C, Veloso VG, Moreira RI, et al. Unprotected sex among men who have sex with men living with HIV in Brazil: a cross-sectional study in Rio de Janeiro. BMC Public Health. 2014;14(379).
Crepaz N, Marks G, Liau A, Mullins MM, Aupont LW, Marshall KJ, et al. Prevalence of unprotected anal intercourse among HIV-diagnosed MSM in the United States: a meta-analysis. AIDS. 2009;23(13):1617–29.
Muessig KE, Pike EC, Fowler B, LeGrand S, Parsons JT, Bull SS, et al. Putting prevention in their pockets: developing mobile phone-based HIV interventions for black men who have sex with men. AIDS Patient Care STDs. 2013;27(4):211–22.
Sullivan PS, Grey JA, Simon Rosser BR. Emerging technologies for HIV prevention for MSM: what we have learned, and ways forward. J Acquir Immune Defic Syndr. 2013;63 Suppl 1:S102–7.
Gowing L, Farrell MF, Bornemann R, Sullivan LE, Ali R. Oral substitution treatment of injecting opioid users for prevention of HIV infection. Cochrane Database Syst Rev. 2011;(8):Cd004145.
Woody GE, Bruce D, Korthuis PT, Chhatre S, Poole S, Hillhouse M, et al. HIV risk reduction with buprenorphine-naloxone or methadone: findings from a randomized trial. J Acquir Immune Defic Syndr. 2014;66(3):288–93.
Choopanya K, Martin M, Suntharasamai P, Sangkum U, Mock PA, Leethochawalit M, et al. Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (the Bangkok Tenofovir study): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2013;381(9883):2083–90.
Gap report. Press Release; 2014. http://www.unaids.org/en/media/unaids/contentassets/documents/unaidspublication/2014/UNAIDS_Gap_report_en.pdf.
Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 U.S. Dependent areas—2011. Press Release; 2013.
Paltiel AD, Weinstein MC, Kimmel AD, Seage 3rd GR, Losina E, Zhang H, et al. Expanded screening for HIV in the United States—an analysis of cost-effectiveness. N Engl J Med. 2005;352(6):586–95.
Delamothe T. Wanted: guidelines that doctors will follow. BMJ. 1993;307(6898):218.
Chamie G, Kwarisiima D, Clark TD, Kabami J, Jain V, Geng E, et al. Uptake of community-based HIV testing during a multi-disease health campaign in rural Uganda. PLoS One. 2014;9(1):e84317.
Suthar AB, Ford N, Bachanas PJ, Wong VJ, Rajan JS, Saltzman AK, et al. Towards universal voluntary HIV testing and counselling: a systematic review and meta-analysis of community-based approaches. PLoS Med. 2013;10(8):e1001496.
Bruce RD, Lambdin B, Chang O, Masao F, Mbwambo J, Mteza I, et al. Lessons from tanzania on the integration of HIV and tuberculosis treatments into methadone assisted treatment. Int J Drug Policy. 2014;25(1):22–5.
Kaai S, Bullock S, Burchell AN, Major C. Factors that affect HIV testing and counseling services among heterosexuals in Canada and the United Kingdom: an integrated review. Patient Educ Couns. 2012;88(1):4–15.
Angotti N, Bula A, Gaydosh L, Kimchi EZ, Thornton RL, Yeatman SE. Increasing the acceptability of HIV counseling and testing with three c’s: convenience, confidentiality and credibility. Soc Sci Med. 2009;68(12):2263–70.
Montaner JS, Lima VD, Barrios R, Yip B, Wood E, Kerr T, et al. Association of highly active antiretroviral therapy coverage, population viral load, and yearly new HIV diagnoses in British Columbia, Canada: a population-based study. Lancet. 2010;376(9740):532–9.
Das M, Chu PL, Santos GM, Scheer S, Vittinghoff E, McFarland W, et al. Decreases in community viral load are accompanied by reductions in new HIV infections in San Francisco. PLoS One. 2010;5(6):e11068.
Tanser F, Barnighausen T, Grapsa E, Zaidi J, Newell ML. High coverage of art associated with decline in risk of HIV acquisition in rural Kwazulu-natal, South Africa. Science. 2013;339(6122):966–71.
Jia Z, Mao Y, Zhang F, Ruan Y, Ma Y, Li J, et al. Antiretroviral therapy to prevent HIV transmission in serodiscordant couples in China (2003–11): a national observational cohort study. Lancet. 2013;382(9899):1195–203.
Montaner JS, Hogg R, Wood E, Kerr T, Tyndall M, Levy AR, et al. The case for expanding access to highly active antiretroviral therapy to curb the growth of the HIV epidemic. Lancet. 2006;368(9534):531–6.
Granich RM, Gilks CF, Dye C, De Cock KM, Williams BG. Universal voluntary HIV testing with immediate antiretroviral therapy as a strategy for elimination of HIV transmission: a mathematical model. Lancet. 2009;373(9657):48–57.
Williams ML, McCurdy SA, Bowen AM, Kilonzo GP, Atkinson JS, Ross MW, et al. HIV seroprevalence in a sample of Tanzanian intravenous drug users. AIDS Educ Prev. 2009;21(5):474–83.
Maartens G, Celum C, Lewin SR. HIV infection: epidemiology, pathogenesis, treatment, and prevention. Lancet. 2014.
Services DoHaH. Panel on antiretroviral guidelines for adults and adolescents. Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents. In.
Choi KH, Lui H, Guo Y, Han L, Mandel JS. Lack of HIV testing and awareness of HIV infection among men who have sex with men, Beijing, China. AIDS Educ Prev Off Publ Int Soc AIDS Educ. 2006;18(1):33–43.
Ainsworth M, Teokul W. Breaking the silence: setting realistic priorities for aids control in less-developed countries. Lancet. 2000;356(9223):55–60.
Bruce RD. Methadone as HIV prevention: high volume methadone sites to decrease HIV incidence rates in resource limited settings. Int J Drug Policy. 2010;21(2):122–4.
USAID Ukraine: report on integrated treatment for HIV-infected opioid dependent persons: Ukraine. Press Release; 2010.
Gardner EM, McLees MP, Steiner JF, Del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis Off Publ Infect Dis Soc Am. 2011;52(6):793–800.
Granich R, Kahn JG, Bennett R, Holmes CB, Garg N, Serenata C, et al. Expanding art for treatment and prevention of HIV in South Africa: estimated cost and cost-effectiveness 2011–2050. PLoS One. 2012;7(2):e30216.
Kahn JG, Marseille EA, Bennett R, Williams BG, Granich R. Cost-effectiveness of antiretroviral therapy for prevention. Curr HIV Res. 2011;9(6):405–15.
Walensky RP, Ross EL, Kumarasamy N, Wood R, Noubary F, Paltiel AD, et al. Cost-effectiveness of HIV treatment as prevention in serodiscordant couples. N Engl J Med. 2013;369(18):1715–25.
Long EF, Brandeau ML, Galvin CM, Vinichenko T, Tole SP, Schwartz A, et al. Effectiveness and cost-effectiveness of strategies to expand antiretroviral therapy in St. Petersburg, Russia. AIDS. 2006;20(17):2207–15.
Sarang A, Rhodes T, Sheon N. Systemic barriers accessing HIV treatment among people who inject drugs in Russia: a qualitative study. Health Policy Plan. 2012.
Wilson IB, Landon BE, Ding L, Zaslavsky AM, Shapiro MF, Bozzette SA, et al. A national study of the relationship of care site HIV specialization to early adoption of highly active antiretroviral therapy. Med Care. 2005;43(1):12–20.
Wilson IB, Landon BE, Hirschhorn LR, McInnes K, Ding L, Marsden PV, et al. Quality of HIV care provided by nurse practitioners, physician assistants, and physicians. Ann Intern Med. 2005;143(10):729–36.
Samb B, Celletti F, Holloway J, Van Damme W, De Cock KM, Dybul M. Rapid expansion of the health workforce in response to the HIV epidemic. N Engl J Med. 2007;357(24):2510–4.
Katz MH. Human immunodeficiency virus is (once again) a primary care disease. Arch Intern Med. 2011;171(8):719–20.
Kranzer K, Govindasamy D, van Schaik N, Thebus E, Davies N, Zimmermann M, et al. Incentivized recruitment of a population sample to a mobile HIV testing service increases the yield of newly diagnosed cases, including those in need of antiretroviral therapy. HIV Med. 2012;13(2):132–7.
van Schaik N, Kranzer K, Wood R, Bekker LG. Earlier HIV diagnosis—are mobile services the answer? S Afr Med j = Suid-Afrikaanse tydskrif vir geneeskunde. 2010;100(10):671–4.
Ahmed S, Delaney K, Villalba-Diebold P, Aliyu G, Constantine N, Ememabelem M, et al. HIV counseling and testing and access-to-care needs of populations most-at-risk for HIV in Nigeria. AIDS Care. 2013;25(1):85–94.
Wang H, Zhou J, Huang L, Li X, Fennie KP, Williams AB. Effects of nurse-delivered home visits combined with telephone calls on medication adherence and quality of life in HIV-infected heroin users in Hunan of China. J Clin Nurs. 2010;19(3–4):380–8.
Gardner LI, Marks G, Craw JA, Wilson TE, Drainoni ML, Moore RD, et al. A low-effort, clinic-wide intervention improves attendance for HIV primary care. Clin Infect Dis Off Publ Infect Dis Soc Am. 2012;55(8):1124–34.
Horvath T, Azman H, Kennedy GE, Rutherford GW. Mobile phone text messaging for promoting adherence to antiretroviral therapy in patients with HIV infection. Cochrane Database Syst Rev. 2012;3, Cd009756.
Gaur AH, Belzer M, Britto P, Garvie PA, Hu C, Graham B, et al. Directly observed therapy (dot) for nonadherent HIV-infected youth: lessons learned, challenges ahead. AIDS Res Hum Retrovir. 2010;26(9):947–53.
Flanigan TP, Taylor LE, Mitty JA. Use of community-based, directly observed therapy for HIV infection: lessons learned for treatment of hepatitis c virus infection. Clin Infect Dis. 2005;40 Suppl 5:S346–8.
Berg KM, Litwin A, Li X, Heo M, Arnsten JH. Directly observed antiretroviral therapy improves adherence and viral load in drug users attending methadone maintenance clinics: a randomized controlled trial. Drug Alcohol Depend. 2011;113(2–3):192–9.
Cunningham CO, Sohler NL, Wong MD, Relf M, Cunningham WE, Drainoni ML, et al. Utilization of health care services in hard-to-reach marginalized HIV-infected individuals. AIDS Patient Care STDs. 2007;21(3):177–86.
Wolitski RJ, Kidder DP, Pals SL, Royal S, Aidala A, Stall R, et al. Randomized trial of the effects of housing assistance on the health and risk behaviors of homeless and unstably housed people living with HIV. AIDS Behav. 2010;14(3):493–503.
Wood E, Hogg RS, Yip B, Dong WW, Wynhoven B, Mo T, et al. Rates of antiretroviral resistance among HIV-infected patients with and without a history of injection drug use. AIDS. 2005;19(11):1189–95.
Altice FL, Bruce RD, Lucas GM, Lum PJ, Korthuis PT, Flanigan TP, et al. HIV treatment outcomes among HIV-infected, opioid-dependent patients receiving buprenorphine/naloxone treatment within HIV clinical care settings: results from a multisite study. J Acquir Immune Defic Syndr. 2011;56 Suppl 1:S22–32.
Dolgin E. Long-acting HIV drugs advanced to overcome adherence challenge. Nat Med. 2014;20(4):323–4.
Cohen J. Virology. A bid to thwart HIV with shot of long-lasting drug. Science. 2014;343(6175):1067.
Sax PE, Zolopa A, Brar I, Elion R, Ortiz R, Post F, et al. Tenofovir alafenamide vs. Tenofovir disoproxil fumarate in single tablet regimens for initial HIV-1 therapy: a randomized phase 2 study. J Acquir Immune Defic Syndr. 2014.
Compliance with Ethics Guidelines
Conflict of Interest
Onyema Ogbuagu and R. Douglas Bruce declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ogbuagu, O., Bruce, R.D. Reaching the Unreached: Treatment as Prevention as a Workable Strategy to Mitigate HIV and Its Consequences in High-Risk Groups. Curr HIV/AIDS Rep 11, 505–512 (2014). https://doi.org/10.1007/s11904-014-0238-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11904-014-0238-4