Abstract
Purpose of Review
To review ongoing and planned clinical trials of weight loss among individuals with or at high risk of heart failure.
Recent Findings
Intentional weight loss via semaglutide among persons with heart failure and preserved ejection fraction and obesity significantly improves weight loss and health status as assessed by the KCCQ-CSS score and is associated with improvements in 6-min walk test.
Summary
Ongoing and planned trials will explore the role of intentional weight loss with treatments such as semaglutide or tirzepatide for individuals with heart failure across the entire ejection fraction spectrum.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The rising prevalence of obesity is a worldwide public health problem responsible for approximately 4 million deaths and 120 million disability-adjusted life years in 2015 alone [1, 2]. Rates of obesity continue to rise in both adults and children, with up to 40% of the overall population in the United States currently reporting a body mass index (BMI) of ≥ 30 kg/m2 [3]. Though obesity is associated with a high risk of multiple cardiovascular complications, patients with obesity are at the highest risk of heart failure (HF), even after adjustment for other traditional risk factors [4, 5]. Results from analyses of data from the Framingham Heart Study found that 13.9% of all HF in women and 10.9% of all HF in men could be attributed to obesity. [6••]. The increasing prevalence of obesity has been matched by a rising incidence of HF in the US population, and these two conditions frequently co-exist, particularly in the case of HF with preserved ejection fraction (HFpEF) [7]. The impact of obesity on the clinical presentation and management of heart failure remains poorly understood, and the impact of intentional weight loss on HF outcomes remains undefined.
Among individuals with HF, those with obesity face higher symptom burden, lower quality of life, and lower exercise capacity, as well as markedly higher frequency of HF hospitalization than those without obesity [8,9,10]. Obesity has historically been regarded as a comorbidity of HF, but evidence points to causal mechanisms involving excess visceral adiposity with hemodynamic, inflammatory, and hormonal abnormalities that affect cardiac and non-cardiac organ functions [11,12,13]. Coupled with higher rates of inflammation, individuals living with obesity and related comorbidities such as hyperlipidemia and hypertension are also at a greater risk of atherosclerotic disease, which may contribute to higher risk of ischemic cardiomyopathy [14]. Sleep-disordered breathing and atrial arrhythmias associated with obesity may also play a role in the incidence of HF [15]. Importantly, the treatment of obesity among patients with HFpEF has been shown to result in significant improvements in clinical status [16••].
There are several knowledge gaps that remain to be filled. The effect of intentional weight loss on functional or clinical outcomes among patients with HF with reduced ejection fraction (HFrEF) and on clinical outcomes such as death or hospitalization in patients with HFpEF remains unclear. Furthermore, the effect of intentional weight loss in patients with HF on intersecting cardiovascular and medical conditions such as metabolic associated fatty liver disease (MAFLD) or diabetes is yet unanswered. It has been difficult to generate high-quality randomized clinical trial data in these areas given (1) the low success rates observed in inducing and maintaining intentional weight loss, even in highly supported trials [17] and (2) the inherent difficulties surrounding randomizing persons treated with bariatric intervention vs sham surgery. These questions will be addressed, at least in part, by planned and ongoing trials of weight loss therapies, including but extending beyond current trials of semaglutide, tirzepatide, and bariatric surgery [18,19,20,21]. Moreover, ongoing cardiovascular trials of novel weight loss medications will offer new insights into the safety and efficacy of emerging therapies and help to determine whether mechanism or magnitude of weight loss might drive differences in clinical status and outcomes. Here, we discuss results from recently completed trials of weight loss medications in patients with obesity with or at high risk of cardiovascular disease and review expectations for ongoing trials.
Weight Management and Heart Failure: Current Evidence
Despite being a well-established risk factor for HF, the impact of obesity on HF-related outcomes has historically been under-studied. This may in part be because of concerns that inducing weight loss among patients with HF may adversely affect mortality risk, based on long-observed trends that patients with HF who were overweight or obese had lower mortality risk than patients who were normal or underweight, a phenomenon known as the “obesity paradox” [6••, 22]. Results from prior retrospective analyses have also suggested that weight loss, even among patients with obesity, may be associated with higher mortality risk. However, analyses of retrospective data cannot differentiate the impact of intentional weight loss, prompted by deliberate intervention, from unintentional weight loss, as occurs in the setting of advancing disease status and progressive cachexia. It is well-known that among patients with chronic disease, including HF, unintentional weight loss is an ominous sign of worsening health, signaling a higher risk of death [23]. This paradox is also partially explained by collider bias, where two parallel risk factors for prognosis (e.g., having obesity and HF) conceal the true association with risk due to residual confounding [24]. Furthermore, when using anthropometric indices other than BMI, no paradox of prognosis was seen [25]. The role of intentional weight loss on HF outcomes therefore remains unclear, and there exists a clear need for randomized data evaluating the impact of intentional weight loss on outcomes in this population.
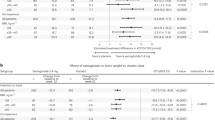
There is, however, new evidence to suggest that intentional weight loss can lead to improvements in clinical status for patients with obesity and HFpEF. In the STEP HFpEF trial (Semaglutide Treatment Effect in People with obesity and HFpEF), pharmacologic intervention with the glucagon-like peptide-1 receptor agonist (GLP-1 RA), semaglutide 2.4 mg subcutaneously once weekly, led to improvements in co-primary endpoints of weight loss and KCCQ-CSS at 1 year in 529 patients with HFpEF and a BMI ≥ 30 kg/m2 [16••]. Patients randomized to semaglutide had mean decreases in body weight of 13.3% at 52 weeks overall, as compared to only 2.6% in the placebo group (10.7% difference, p < 0.001). Semaglutide also led to a significant improvement in health status, assessed by KCCQ-CSS [16••, 26]; participants randomized to semaglutide had a mean improvement in their KCCQ-CSS score of 16.6 points, 7.8 points more than what was observed in the placebo arm (p < 0.001). Previous work has suggested that KCCQ-CSS changes of ~ 7 are clinically significant among patients with HFpEF [27].
In addition to improvements in the co-primary outcomes, the group receiving semaglutide experienced improvements in the secondary outcomes of 6-min walk test (6MWT, 21.5-m improvement vs 1.2 m in placebo group, difference 20.3 m, p < 0.001) and a hierarchy of clinical outcomes including death, worsening HF, and differences in change in health status; and in the inflammatory marker, C-reactive protein (CRP) [16••]. Importantly, the magnitude of improvement in KCCQ-CSS score and 6MWT was found to track closely with magnitude of weight lost over the course of the trial, with a 6.4-point improvement (95% CI 4.1 to 8.8) in KCCQ-CSS and 14.4-m improvement (95% CI 5.5 to 23.3) in 6MWT for each 10% reduction in body mass [28]. Though this trial was not powered to assess clinical outcomes and limited by extremely low event rates, semaglutide was associated with numerically fewer HF hospitalizations with one hospitalization among those randomized to semaglutide and 12 among study participants randomized to placebo.
STEP-HFpEF represents a new and important step forward in identifying better management strategies for patients with HF and is the first large-scale, randomized trial to show that management of obesity can lead to improved clinical status for patients with HF and comorbid obesity. Despite this, important questions remain, including the reproducibility of these results across other trials and other weight loss interventions, mechanistic explanations for benefit from weight loss, potential benefit on comorbidities associated with HF that worsen HF prognosis, and the impact of weight loss on clinical outcomes such as death and hospitalization for HF (Fig. 1). The Semaglutide Effects on Cardiovascular Outcomes in People With Overweight or Obesity (SELECT) trial found that intentional weight loss via semaglutide reduced a composite endpoint of cardiovascular death, non-fatal myocardial infarction, and non-fatal stroke by 20% (HR 0.80, 95% CI 0.72 to 0.90, p < 0.001) [29]. Though patients with and without HF appeared to derive a similar degree of benefit, subgroup analysis surrounding patients with HFpEF vs HFrEF are not yet available. Furthermore, it remains to be seen how results may impact the evolution of treatment of obesity and the diseases it drives, how weight loss maintenance will be addressed, and whether loss of lean mass may be problematic in subgroups of patients. Fortunately, ongoing trials in this space promise to help answer these questions and show that the medical community has finally started “putting more weight” on obesity trials in HF (Table 1).
Weight Loss and Changes in Health Status and Physical Function
The results of STEP-HFpEF will be complemented by results from The Study of Tirzepatide in Participants with Heart Failure With Preserved Ejection Fraction and Obesity (SUMMIT; NCT: NCT04847557) [20], expected to complete July 2024. Tirzepatide causes greater weight loss than does semaglutide (20% vs 15%) at the dose approved for the treatment of obesity and may help to further illustrate the relationship between magnitude of weight loss and degree of clinical benefit [30]. The role of bariatric surgery and other non-surgical weight loss procedures (such as endoscopic sleeve gastroplasty) in the treatment of obesity and HF remain to be determined.
Taken together, these trials will help determine the role of intentional weight loss on clinical status in patients with HFpEF and, by virtue of the hierarchical endpoint used in SUMMIT, may offer new insights into the likelihood that a patient will derive benefit from weight loss intervention (specifically tirzepatide) vs placebo. If the results of SUMMIT show consistent magnitude of benefit compared to STEP-HFpEF, then the cardiovascular community will have compelling evidence that weight loss interventions can offer benefit for patients with HFpEF and obesity. However, neither STEP-HFpEF nor SUMMIT is powered to definitively determine the impact of weight loss on clinical outcomes in patients with obesity and HFpEF, nor will they establish evidence of benefit among patients with HFrEF.
Effect of Weight Loss on Risk of Death or Hospitalization for Heart Failure
Recent and ongoing cardiovascular outcomes trials may offer new insights into the role of intentional weight loss on clinical outcomes in patients with cardiovascular disease, including (though not specifically limited to) patients with HFrEF and HFpEF. The recently completed Semaglutide Effects on Cardiovascular Outcomes in People With Overweight or Obesity (SELECT; NCT:03574597) trial tested the impact of semaglutide, given at the dose approved for weight loss (2.4 mg weekly subcutaneous injection) on a composite outcome of cardiovascular mortality, non-fatal myocardial infarction, and non-fatal stroke in patients with atherosclerotic cardiovascular disease. Notably, among patients with diabetes, semaglutide has previously been shown to improve this outcome at lower doses approved for the treatment of patients with type 2 diabetes (0.5 mg or 1 mg once weekly subcutaneous injection) when compared with placebo (HR 0.74, 95% CI, 0.58–0.95, p = 0.02 for superiority) [31]. The SELECT trial enrolled 17,604 patients with established atherosclerotic cardiovascular disease, including prior myocardial infarction, prior stroke, and/or established peripheral arterial disease, excluding persons with diabetes. Of these patients, 24.3% (n = 4274) also had established HF, including 2268 patients with HFpEF and 1341 patients with HFrEF [32]. This represents the largest population of patients with HF studied with a pharmacologic weight loss intervention to date. Topline results from SELECT, reported by press release, indicate a 20% relative risk reduction in the primary composite outcome; results from additional endpoints and subgroup analyses remain unknown [33]. Among these individuals, the impact of semaglutide on (1) cardiovascular death and (2) incident HF events will be of great interest as other data regarding effects of GLP-1 RA therapy on HF outcomes have been mixed, particularly in those with HFrEF who were not necessarily obese [34].
In the Functional Impact of GLP-1 for HF Treatment (FIGHT) trial, patients with HFrEF and a recent HF hospitalization within the past 14 days (both with and without type 2 diabetes) had a numerical though not statistically significant increase in risk of hospitalization for HF (63 vs. 50 events; HR 1.30, 95% CI 0.89–1.88) and for the composite of hospitalization for HF/CV death (72 vs. 57 events; HR 1.30, 95% CI 0.92–1.83) at 180 days when compared with placebo [35]. In the Effect of Liraglutide on Left Ventricular Function in Stable Chronic Heart Failure Patients (LIVE) trial, liraglutide in patients with HFrEF with and without diabetes was associated with a higher risk of adverse cardiac events (10% vs 3%, p = 0.04), though this was based on only 15 events overall across the entire trial [36]. Importantly, neither of these trials was limited to study participants with obesity, and so the impact of weight loss among patients with obesity and comorbid HF remains unclear. The sub-population of patients with HFrEF in SELECT will therefore represent the largest evaluation of a GLP-1 RA in patients with HFrEF to date, and the only evaluation of such a therapy in patients with both HFrEF and obesity. Results from SELECT are anticipated in late 2023.
Another ongoing cardiovascular outcomes trial is being conducted with tirzepatide, a once-weekly injectable dual GLP-1/GIP receptor agonist with proven efficacy for weight loss [30]. The Study of Tirzepatide on the Reduction on Morbidity and Mortality in Adults with Obesity (SURMOUNT MMO; NCT:05556512) trial will test the impact of tirzepatide vs placebo on a composite of death, non-fatal myocardial infarction, non-fatal stroke, coronary revascularization and heart failure in approximately 15,000 patients with a BMI ≥ 27 kg/m2, without T2DM, and with or at high risk of vascular disease [19]. This trial will offer additional insight into the impact of intentional weight loss on HF outcomes, albeit as an exploratory secondary endpoint.
Unanswered Questions and Future Directions
Despite the promise of ongoing trials of semaglutide and tirzepatide in patients with HF, important questions will remain unanswered at the completion of these clinical trials. Semaglutide, a GLP-1 RA, and tirzepatide, a GLP-1/GIP RA, belong to adjacent classes, with overlapping mechanisms of action. It will remain unclear, therefore, whether any impact of these medications on clinical outcomes is driven exclusively by weight loss, or whether there might be additional mechanisms related to the specific modality by which that weight loss is achieved. The association between obesity and HF, particularly HF with preserved ejection fraction (HFpEF), appears to be mediated via multiple mechanisms, including inflammation, adipokines, and insulin resistance [11,12,13]. The impact of specific weight loss drugs on these and other mechanisms driving the relationship between HF and obesity remains to be elucidated. Similarly, some evidence suggests that certain distributions of adipose tissue, particularly visceral and epicardial adipose tissue, are more likely to contribute to adverse cardiovascular outcomes [37,38,39, 40•]. It is not yet known whether certain forms of weight loss might preferentially target these higher-risk depots of adipose.
It is not clear at this time whether the benefits observed in STEP-HFpEF were directly driven by improvement in HF, or whether improvements in quality of life (as measured by KCCQ) and exercise capacity (as measured by 6-min walk test) might have been driven not due to improvement in HF-related symptoms per se, but rather by improvement in obesity-related symptoms. We believe that both are likely true and contributing. In STEP-HFpEF, the strongest objective evidence for cardiac benefit is the observation that randomization to semaglutide was associated with significant improvements in NT-proBNP concentrations, despite the fact that obesity is associated with lower NT-proBNP concentrations for any given left ventricular end-diastolic pressure, and that weight loss in patients without HF is typically associated with an increase in NT-pBNP [41,42,43]. Based on the baseline inverse relationship between BMI and NT-proBNP, in which NT-proBNP decreases as BMI rises, it would be expected that NT-proBNP would have increased as patients randomized to semaglutide lost weight, in the absence of any effect on HF status. The fact that the opposite occurred suggests that there may be significant changes in HF physiology among patients with HFpEF who receive management (via intentional weight loss) of their obesity. STEP-HFpEF enrolled a fairly low-risk population of persons with HFpEF, and future work among patients with HFpEF and obesity will hopefully emphasize the impact of intentional weight loss on clinical events such as hospitalization for heart failure among higher-risk individuals.
Given previous data suggesting that GLP-1 RAs may not be well tolerated in patients with HFrEF without obesity, the role of agents from other classes to pursue weight loss is of particular interest. It is also possible that even if weight loss leads to improvements in outcomes for patients with HFrEF and obesity, the use of a GLP-1 RA to achieve that weight loss may moderate, or even outweigh, any benefit from weight loss overall. If this is the case, then other modes of weight loss may represent safer and more effective routes for weight loss, assuming that a clinical benefit exists. The differential impact of various weight loss therapies on other obesity-related comorbidities such as metabolic dysfunction–associated liver disease, type 2 diabetes, sleep apnea, atrial fibrillation, and hypertension and their corresponding relationship with HF risk will also be important.
New and emerging therapies for weight loss, including therapies that do not rely on the same mechanism for weight loss, will be of particular interest in the assessment of these unanswered questions [44,45,46,47,48]. These medications include survodutide, a GLP-1 and glucagon receptor dual agonist; retatrutide, a GLP-1/GIP/glucagon receptor agonist; and cagrisema, a combination of semaglutide and an amylin analogue [44, 45, 47]. Other drugs of interest currently being developed for weight loss include AMG-133, a GLP-1 RA, and GIP receptor antagonist (rather than agonist) that requires only once-monthly administration and HU6, a controlled metabolic accelerator that acts via mitochondrial uncoupling to increased oxidation of fats and sugars [48, 49]. Non-randomized observational data consistently demonstrate associations between bariatric surgery and lower cardiovascular risk, including risk of HF [50,51,52], and pilot work is ongoing to assess the differential impact of bariatric surgery vs other forms of medical weight management on cardiovascular outcomes for persons at high risk [21].
It remains unclear exactly how much weight loss might be necessary to derive greatest benefit, though some data from STEP-HFpEF suggests that greater weight loss is associated with greater incremental benefit without any obvious plateau [28]. There is also a great interest in better understanding the duration of treatment necessary to maintain significant weight loss: some initial data in patients without HF suggests that withdrawal of semaglutide after 68 weeks resulted in regain of approximately two-thirds of lost body weight and reversion of cardiometabolic markers to baseline levels [53]. It has been hypothesized but not yet shown that prolonged use of these therapies may cause a new, lower body weight “set point” that allows individuals to taper therapies without weight gain [54]. In addition to determining absolute impact on risk of clinical events, understanding necessary duration of therapy will be important to understanding the economics of these therapies, which can be expensive [55].
Taken together, ongoing and recently completed trials will offer important and new insights into the role of intentional weight loss for persons with established HF and obesity. The results from these trials will help to establish the impact of intentional weight loss functional status, symptom burden, and quality of life, as well as on clinical outcomes such as death and hospitalization. However, important questions will remain regarding whether the impact of such weight loss is driving purely by magnitude of weight loss, or whether medication type and mechanism also play a role. Emerging therapies with differing mechanisms of action may offer further insight into this issue, while further establishing what role intentional weight loss may plan in the management of patients with HF and comorbid obesity.
References
The GBD 2015 Obesity Collaborators. Health effects of overweight and obesity in 195 countries over 25 Years. N Engl J Med. 2017;377:13–27.
Sarma S, Sockalingam S, Dash S. Obesity as a multisystem disease: trends in obesity rates and obesity-related complications. Diabetes Obes Metab. 2021;23(Suppl 1):3–16.
Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity among adults and youth: United States, 2015–2016. NCHSData Brief. 2017;288:8.
Sattar N, McMurray J, Borén J, Rawshani A, Omerovic E, Berg N, et al. Twenty years of cardiovascular complications and risk factors in patients with type 2 diabetes: a nationwide Swedish cohort study. Circulation. 2023;147:1872–86.
Rawshani A, Rawshani A, Franzén S, Sattar N, Eliasson B, Svensson A-M, et al. Risk factors, mortality, and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2018;379:633–44.
Kenchaiah S, Pocock SJ, Wang D, Finn PV, Zornoff LAM, Skali H, et al. Body mass index and prognosis in patients with chronic heart failure. Circulation. 2007;116:627–36. Landmark paper showing that each 1 point increase in BMI is associated with a 5% increase in risk of HF for men, and 7% increase in risk for women.
Ndumele CE, Matsushita K, Lazo M, Bello N, Blumenthal RS, Gerstenblith G, et al. Obesity and subtypes of incident cardiovascular disease. J Am Heart Assoc. 2016;5:e003921.
Obokata M, Reddy YNV, Pislaru SV, Melenovsky V, Borlaug BA. Evidence supporting the existence of a distinct obese phenotype of heart failure with preserved ejection fraction. Circulation. 2017;136:6–19.
Adamson C, Jhund PS, Docherty KF, Bělohlávek J, Chiang C-E, Diez M, et al. Efficacy of dapagliflozin in heart failure with reduced ejection fraction according to body mass index. Eur J Heart Fail. 2021;23:1662–72.
Adamson C, Kondo T, Jhund P, de Boer RA, Honorio JWC, Claggett B, et al. Dapagliflozin for heart failure according to body mass index: the DELIVER trial. Eur Heart J. 2022;43:4406–17.
Alexander JK, Amad KH, Cole VW. Observations on some clinical features of extreme obesity, with particular reference to cardiorespiratory effects. Am J Med. 1962;32:512–24.
Kasper EK, Hruban RH, Baughman KL. Cardiomyopathy of obesity: a clinicopathologic evaluation of 43 obese patients with heart failure. Am J Cardiol. 1992;70:921–4.
Rabbia F, Silke B, Conterno A, Grosso T, De Vito B, Rabbone I, et al. Assessment of cardiac autonomic modulation during adolescent obesity. Obes Res. 2003;11:541–8.
Henning RJ. Obesity and obesity-induced inflammatory disease contribute to atherosclerosis: a review of the pathophysiology and treatment of obesity. Am J Cardiovasc Dis. 2021;11:504–29.
Alpert MA, Lavie CJ, Agrawal H, Aggarwal KB, Kumar SA. Obesity and heart failure: epidemiology, pathophysiology, clinical manifestations, and management. Transl Res. 2014;164:345–56.
Kosiborod MN, Abildstrøm SZ, Borlaug BA, Butler J, Rasmussen S, Davies M, et al. Semaglutide in Patients with heart failure with preserved ejection fraction and obesity. N Engl J Med. 2023;389:1069–84. STEP HFpEF is the first randomized clinical trial to show that intentional weight loss (via semaglutide) results in significant improvement in clinical status for patients with heart failure and preserved ejection fraction.
The LOOK AHEAD Investigators. Cardiovascular effectsof intensive lifestyle intervention in type 2 diabetes. N Engl J Med. 2013;369:145–54.
Novo Nordisk. SELECT - Semaglutide Effects on Cardiovascular Outcomes in People With Overweight or Obesity [Internet]. 2023. https://clinicaltrials.gov/ct2/show/NCT03574597. Accessed 6 Apr 2023.
Eli Lilly and Company. A study of tirzepatide (LY3298176) on the reduction on morbidity and mortality in adults with obesity (SURMOUNT-MMO) [Internet]. https://clinicaltrials.gov/study/NCT05556512. Accessed 8 Jul 2023.
Eli Lilly and Company. A study of tirzepatide (LY3298176) in participants with heart failure with preserved ejection fraction and obesity [Internet]. ClinicalTrials.gov. https://clinicaltrials.gov/ct2/show/NCT04847557. Accessed 22 Jul 2023.
Hamilton Health Sciences Corporation. Bariatric surgery for the reduction of cardiovascular events feasibility randomized controlled trial (BRAVE) [Internet]. Report No.: NCT04226664. 2022. https://clinicaltrials.gov/study/NCT04226664.
Sharma A, Lavie CJ, Borer JS, Vallakati A, Goel S, Lopez-Jimenez F, et al. Meta-analysis of the relation of body mass index to all-cause and cardiovascular mortality and hospitalization in patients with chronic heart failure. Am J Cardiol. 2015;115:1428–34.
Anker SD, Ponikowski P, Varney S, Chua TP, Clark AL, Webb-Peploe KM, et al. Wasting as independent risk factor for mortality in chronic heart failure. Lancet. 1997;349:1050–3.
Sperrin M, Candlish J, Badrick E, Renehan A, Buchan I. Collider bias is only a partial explanation for the obesity paradox. Epidemiology. 2016;27:525–30.
Butt JH, Petrie MC, Jhund PS, Sattar N, Desai AS, Køber L, et al. Anthropometric measures and adverse outcomes in heart failure with reduced ejection fraction: revisiting the obesity paradox. Eur Heart J. 2023;44:1136–53.
Wilding JPH, Batterham RL, Calanna S, Davies M, Van Gaal LF, Lingvay I, et al. Once-weekly semaglutide in adults with overweight or obesity. N Engl J Med. 2021;384:989–1002.
Butler J, Shahzeb Khan M, Lindenfeld J, Abraham WT, Savarese G, Salsali A, et al. Minimally clinically important difference in health status scores in patients with HFrEF vs HFpEF. JACC Heart Fail. 2022;10:651–61.
Borlaug BA, Kitzman DW, Davies MJ, Rasmussen S, Barros E, Butler J, et al. Semaglutide in HFpEF across obesity class and by body weight reduction: a prespecified analysis of the STEP-HFpEF trial. Nat Med. 2023;29:2358–65.
Lincoff AM, Brown-Frandsen K, Colhoun HM, Deanfield J, Emerson SS, Esbjerg S, et al. Semaglutide and cardiovascular outcomes in obesity without diabetes. N Engl J Med. 2023;389:2221–32.
Jastreboff AM, Aronne LJ, Ahmad NN, Wharton S, Connery L, Alves B, et al. Tirzepatide once weekly for the treatment of obesity. N Engl J Med. 2022;387:205–16.
Marso SP, Bain SC, Consoli A, Eliaschewitz FG, Jódar E, Leiter LA, et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2016;375:1834–44.
Lingvay I, Brown-Frandsen K, Colhoun HM, Deanfield J, Emerson SS, Esbjerg S, et al. Semaglutide for cardiovascular event reduction in people with overweight or obesity: SELECT study baseline characteristics. Obesity (Silver Spring). 2023;31:111–22.
News Details [Internet]. Novo Nordisk. https://www.novonordisk.com/content/nncorp/global/en/news-and-media/news-and-ir-materials/news-details.html. Accessed 29 Aug 2023.
Khan MS, Fonarow GC, McGuire DK, Hernandez AF, Vaduganathan M, Rosenstock J, et al. Glucagon-Like Peptide 1 Receptor Agonists and Heart Failure. Circulation. 2020;142:1205–18.
Margulies KB, Hernandez AF, Redfield MM, Givertz MM, Oliveira GH, Cole R, et al. Effects of liraglutide on clinical stability among patients with advanced heart failure and reduced ejection fraction: a randomized clinical trial. JAMA. 2016;316:500–8.
Jorsal A, Kistorp C, Holmager P, Tougaard RS, Nielsen R, Hänselmann A, et al. Effect of liraglutide, a glucagon-like peptide-1 analogue, on left ventricular function in stable chronic heart failure patients with and without diabetes (LIVE)-a multicentre, double-blind, randomised, placebo-controlled trial. Eur J Heart Fail. 2017;19:69–77.
Rao VN, Fudim M, Mentz RJ, Michos ED, Felker GM. Regional adiposity and heart failure with preserved ejection fraction. Eur J Heart Fail. 2020;22:1540–50.
Sorimachi H, Obokata M, Takahashi N, Reddy YNV, Jain CC, Verbrugge FH, et al. Pathophysiologic importance of visceral adipose tissue in women with heart failure and preserved ejection fraction. Eur Heart J. 2020;42:1595–605.
Xu C, Guo Y, Zhang S, Lai Y, Huang M, Zhan R, et al. Visceral adiposity index and the risk of heart failure, late-life cardiac structure, and function in ARIC study. Eur J Prev Cardiol. 2023;30:1182–92.
Borlaug BA, Jensen MD, Kitzman DW, Lam CSP, Obokata M, Rider OJ. Obesity and heart failure with preserved ejection fraction: new insights and pathophysiological targets. Cardiovasc Res. 2022;18(18):3434–50. An excellent review of the mechanisms and pathophysiology underlying heart failure with preserved ejection fraction in patients with obesity.
Madamanchi C, Alhosaini H, Sumida A, Runge MS. Obesity and natriuretic peptides, BNP and NT-proBNP: mechanisms and diagnostic implications for heart failure. Int J Cardiol. 2014;176:611–7.
Hollstein T, Schlicht K, Krause L, Hagen S, Rohmann N, Schulte DM, et al. Effect of various weight loss interventions on serum NT-proBNP concentration in severe obese subjects without clinical manifest heart failure. Sci Rep. 2021;11:10096.
Fedele D, Bicchiega V, Collo A, Barutta F, Pistone E, Gruden G, et al. Short term variation in NTproBNP after lifestyle intervention in severe obesity. PLoS ONE. 2017;12:e0181212.
Survodutide (BI 456906) [Internet]. Boehringer Ingelheim. 2023. https://www.boehringer-ingelheim.com/survodutide-bi-456906. Accessed 29 Aug 2023.
Eli Lilly and Company. A phase 2 study of once-weekly LY3437943 compared with placebo in participants who have obesity or are overweight with weight-related comorbidities [Internet]. clinicaltrials.gov. Report No.: NCT04881760. 2023. https://clinicaltrials.gov/study/NCT04881760.
News details [Internet]. http://www.novonordisk.com/media/news-details.2129162.html. Accessed 1 Apr 2018.
Novo Nordisk A/S. The cardiovascular safety of cagrilintide 2.4 mg s.c. in combination with semaglutide 2.4 mg s.c. (CagriSema 2.4 mg/2.4 mg s.c.) once-weekly in participants with obesity and established cardiovascular disease [Internet]. clinicaltrials.gov. Report No.: NCT05669755. 2023. https://clinicaltrials.gov/ct2/show/NCT05669755.
Rivus Pharmaceuticals, Inc. Exploratory Phase 2A, double-blind, placebo-controlled, dose escalation study to determine the safety, tolerability, PD, and PK of HU6 for the Treatment of subjects with obese heart failure with preserved ejection fraction (HFpEF) [Internet]. clinicaltrials.gov. Report No.: NCT05284617. 2023. https://clinicaltrials.gov/study/NCT05284617.
Amgen. A Phase 2 randomized, placebo-controlled, double-blind, dose-ranging study to evaluate the efficacy, safety, and tolerability of AMG 133 in adult subjects with overweight or obesity, with or without type 2 diabetes mellitus [Internet]. clinicaltrials.gov. Report No.: NCT05669599. https://clinicaltrials.gov/study/NCT05669599. Accessed Aug 2023.
Batsis JA, Sarr MG, Collazo-Clavell ML, Thomas RJ, Romero-Corral A, Somers VK, et al. Cardiovascular risk after bariatric surgery for obesity. Am J Cardiol. 2008;102:930–7.
Doumouras AG, Wong JA, Paterson JM, Lee Y, Sivapathasundaram B, Tarride J-E, et al. Bariatric surgery and cardiovascular outcomes in patients with obesity and cardiovascular disease. Circulation. 2021;143:1468–80.
Fisher DP, Johnson E, Haneuse S, Arterburn D, Coleman KJ, O’Connor PJ, et al. Association between bariatric surgery and macrovascular disease outcomes in patients with type 2 diabetes and severe obesity. JAMA. 2018;320:1570–82.
Wilding JPH, Batterham RL, Davies M, Van Gaal LF, Kandler K, Konakli K, et al. Weight regain and cardiometabolic effects after withdrawal of semaglutide: The STEP 1 trial extension. Diabetes Obes Metab. 2022;24:1553–64.
St Clair Gibson A, Goedecke JH, Harley YX, Myers LJ, Lambert MI, Noakes TD, et al. Metabolic setpoint control mechanisms in different physiological systems at rest and during exercise. J Theor Biol. 2005;236:60–72.
Obesity: How do we treat America’s silent killer without breaking the economy? [Internet]. MedicalEconomics 2023. https://www.medicaleconomics.com/view/obesity-how-do-we-treat-america-s-silent-killer-without-breaking-the-economy-. Accessed 27 Jan 2024.
Acknowledgements
The editors would like to thank Dr. Joe Cuthbert for handling the review of this manuscript.
Funding
No funding was received for this article.
Author information
Authors and Affiliations
Contributions
JH and DM prepared the initial draft: all authors contributed extensively to revisions and to subsequent iterations of the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Conflict of Interest
JH has no disclosures. JLJ is a trustee of the American College of Cardiology; is a board member of Imbria Pharma; has received research support from Abbott, Applied Therapeutics, HeartFlow Inc, Innolife, and Roche Diagnostics; has consulting income from Abbott, AstraZeneca, Bayer, Beckman, Boehringer-Ingelheim, Janssen, Jana Care, Novartis, Merck, and Roche Diagnostics; and participates in clinical endpoint committees/data safety monitoring boards for Abbott, AbbVie, Bayer, CVRx, Intercept, Pfizer, and Takeda. CSPL is supported by a Clinician Scientist Award from the National Medical Research Council of Singapore; has received research support from Novo Nordisk and Roche Diagnostics; has served as a consultant or on the advisory board/steering committee/executive committee for Alleviant Medical, Allysta Pharma, AnaCardio AB, Applied Therapeutics, AstraZeneca, Bayer, Biopeutics, Boehringer Ingelheim, Boston Scientific, Bristol Myers Squibb, CardioRenal, Cytokinetics, Darma Inc., EchoNous Inc, Eli Lilly, Impulse Dynamics, Intellia Therapeutics, Ionis Pharmaceutical, Janssen Research & Development LLC, Medscape/WebMD Global LLC, Merck, Novartis, Novo Nordisk, ProSciento Inc, Quidel Corporation, Radcliffe Group Ltd., Recardio Inc, ReCor Medical, Roche Diagnostics, Sanofi, Siemens Healthcare Diagnostics, and Us2.ai; and serves as co-founder and non-executive director of Us2.ai. HVS was funded by the Canadian Institutes of Health Research. GMF has received research grants from NHLBI, American Heart Association, Amgen, Bayer, BMS, Merck, Cytokinetics, and CSL-Behring; has acted as a consultant to Novartis, Amgen, BMS, Cytokinetics, Medtronic, Cardionomic, Boehringer-Ingelheim, American Regent, Abbott, Astra-Zeneca, Reprieve, Myovant, Sequana, Windtree Therapeutics, and Whiteswell; and has served on clinical endpoint committees/data safety monitoring boards for Amgen, Merck, Medtronic, EBR Systems, V-Wave, LivaNova, Siemens, and Rocket Pharma. NJP reports research support from Amgen, Boehringer Ingelheim, Eggland’s Best, Eli Lilly, Novartis, Novo Nordisk, and Verily Life Sciences; has served as a consultant or on an advisory panel for Bayer, Boehringer Ingelheim, CRISPR Therapeutics, Eli Lilly, Esperion, AstraZeneca, Merck, Novartis, and Novo Nordisk; is an executive committee member for trials sponsored by Novo Nordisk and Amgen on DSMBs for trials sponsored by Janssen and Novartis. NS has consulted for and/or received speaker honoraria from Abbott Laboratories, Amgen, AstraZeneca, Boehringer Ingelheim, Eli Lilly, Hanmi Pharmaceuticals, Janssen, Merck Sharp & Dohme, Novartis, Novo Nordisk, Pfizer, Roche Diagnostics, and Sanofi; and received grant support paid to his University from AstraZeneca, Boehringer Ingelheim, Novartis, and Roche Diagnostics outside the submitted work. AP has received research support from the National Institute on Aging GEMSSTAR Grant (1R03AG067960-01), the National Institute on Minority Health and Disparities (R01MD017529), and the National Institute of Heart, Lung, and Blood Institute (R21HL169708). He has received grant funding (to the institution) from Applied Therapeutics, Gilead Sciences, Ultromics, Myovista, and Roche; has served as a consultant for and/or received honoraria outside of the present study as an advisor/consultant for Tricog Health Inc, Lilly USA, Rivus, Cytokinetics, Roche Diagnostics, Sarfez Therapeutics, Edwards Lifesciences, Merck, Bayer, Novo Nordisk, Alleviant, and Axon Therapies; and has received nonfinancial support from Pfizer and Merck. He is also a consultant for Palomarin Inc. with stocks compensation. DKM reports personal fees from Boehringer Ingelheim, Sanofi US, Merck & Co., Merck Sharp and Dohme Corp., Eli Lilly USA, Novo Nordisk, AstraZeneca, Lexicon Pharmaceuticals, Eisai, Pfizer, Metavant, Applied Therapeutics, Afimmune, Bayer, CSL Behring and Esperion; research support for Clinical Trials Leadership from Boehringer Ingelheim, Pfizer, AstraZeneca, Novo Nordisk, Esperion, Lilly USA, CSL Behring, and honoraria for consultancy from Lilly USA, Pfizer, Boehringer Ingelheim, Lexicon, Novo Nordisk, Applied Therapeutics, Altimmune, CSL Behring, Bayer, Intercept, New Amsterdam.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Harrington, J., Sattar, N., Felker, G.M. et al. Putting More Weight on Obesity Trials in Heart Failure. Curr Heart Fail Rep 21, 194–202 (2024). https://doi.org/10.1007/s11897-024-00655-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11897-024-00655-z