Abstract
Purpose of Review
To provide a contemporary overview of the pathophysiology, evaluation, and treatment of hyponatremia in heart failure (HF).
Recent Findings
Potassium and magnesium losses due to poor nutritional intake and treatment with diuretics cause an intracellular sodium shift in HF that may contribute to hyponatremia. Impaired renal blood flow leading to a lower glomerular filtration rate and increased proximal tubular reabsorption lead to an impaired tubular flux through diluting distal segments of the nephron, compromising electrolyte-free water excretion.
Summary
Hyponatremia in HF is typically a condition of impaired water excretion by the kidneys on a background of potassium and magnesium depletion. While those cations can and should be easily repleted, further treatment should mainly focus on improving the underlying HF and hemodynamics, while addressing congestion. For decongestive treatment, proximally acting diuretics such as sodium-glucose co-transporter-2 inhibitors, acetazolamide, and loop diuretics are the preferred options.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hyponatremia, defined as a serum sodium (Na+) concentration < 135 mmol/L, is the most common electrolyte disorder in hospitalized patients, affecting up to one-third of patients with heart failure (HF), being more frequent in advanced disease [1,2,3,4,5]. The presence of hyponatremia is associated with functional impairment (e.g., worse cognitive status [6, 7] and an increased risk for falls) as well as poor clinical outcomes in both acute and chronic HF [8]. Both admission and hospital-acquired hyponatremia are associated with a longer hospital stay, more frequent need for discharge to a short- or long-term care facility, and a higher risk for hospital readmissions or all-cause mortality [9,10,11,12]. Up until now, it remains unclear whether hyponatremia itself is merely a marker of risk versus a causal risk factor with an impact on disease progression and prognosis. This review provides a contemporary overview of the clinical problem of hyponatremia in HF, discussing its pathophysiology, general approach, and treatment.
Pathophysiology of Hyponatremia in Heart Failure
Serum Sodium Concentration and Plasma Osmolality
Under normal circumstances, plasma osmolality is strictly regulated within a close range (i.e., 275–295 mOsm/L), as the brains can poorly cope with osmotic stress. Indeed, brain tissue swells when hypotonicity is present (creating a risk for intracranial hypertension within the rigid skull), while it shrinks in a hypertonic environment. Therefore, even a tiny increase in plasma osmolality of 10 mOsm/L results in a doubling of the plasma arginine vasopressin (AVP) or “anti-diuretic hormone” concentration, promoting thirst and water retention to protect normal plasma osmolality [13].
Typically, hyponatremia indicates a low plasma osmolality (< 275 mOsm/L) and hypotonicity [5, 14]. Notable exceptions are pseudo-hyponatremia (i.e., low serum Na+ concentration due to a laboratory artifact caused by hyperlipidemia or abnormally high protein levels that may be seen in monoclonal gammopathies, malignancy, chronic hepatitis C, or human immunodeficiency virus infection) and true hyponatremia with normal or elevated plasma osmolality due to hyperglycemia, uremia, contrast agents, or another source of osmoles. These conditions should always be excluded in any case of hyponatremia to avoid inappropriate treatment. A correction factor with a 1.6–2.4 mmol/L decrease in serum Na+ per 100 mg/dL increase in glucose concentration may be employed in case of significant hyperglycemia [15, 16].
Hypotonic Hyponatremia in Heart Failure
Hypotonic hyponatremia in HF is typically a condition with normal or elevated total body Na+, resulting from impaired water excretion rather than true Na+ depletion (Fig. 1). However, due to poor nutritional intake and frequent use of diuretics, potassium and magnesium depletion are very common and contribute to low serum Na+ levels.
Depletional Hyponatremia
Potassium and magnesium are abundantly present in fruits, vegetables, whole grains, nuts, and seeds, which are all part of a healthy diet. While some patients with HF may have unhealthy dietary habits (e.g., processed food), even those with good nutritional intake are at increased risk for deficiencies. Both loop and thiazide-like diuretics to prevent or treat congestion cause considerable potassium and magnesium wasting [17], which is even more pronounced when acetazolamide is added for sequential nephron blockade. Moreover, neurohumoral activation that plays a central role in HF with reduced ejection fraction stimulates Na+ retention at the cost of increased potassium losses in the distal nephron [18]. Both aldosterone and sympathetic nervous system activation promote magnesium loss as well. As potassium and magnesium are the most abundant intracellular cations, their depletion causes a Na+ shift toward the intracellular compartment to maintain its osmotic load and limit cell shrinkage [19]. Furthermore, magnesium is an essential cofactor for adequate functioning of the Na+/potassium ATPase pump that keeps Na + in the extracellular environment [20]. The resulting intracellular Na+ shift contributes to low serum Na+ levels that are easily corrected with adequate repletion, hence, depletional hyponatremia. Serum potassium levels of ~ 4.5 mmol/L are associated with the lowest cardiovascular risk in HF [21]. Importantly, serum potassium levels 3.5–3.9 mmol/L (generally reported within the normal range) may already indicate substantial potassium deficits of up to 200 mmol [22]. Also for serum magnesium concentration, it is prudent to aim for the higher side of the normal range, as serum magnesium only represent 0.3% of total body stores and therefore poorly reflects total body and especially intracellular magnesium [23].
In rare cases, patients with HF may present with a true Na+ deficit. Usually, this is caused by either overzealous use of diuretics or increased extra-renal losses (e.g., diarrhea or vomiting). Increased Na+ avidity is a characteristic finding that is already present in preclinical HF [24]. Therefore, patients with HF usually have increased total body Na+ stores, with a buffer system for non-osmotic storage by glycosaminoglycan networks in the interstitium and skin, offering effective protection against Na+ depletion [25, 26]. However, in patients who adhere scrupulously to salt restriction and are treated with intensive diuretic regimens, depletional hyponatremia may still occur. Per definition, the presence of clinical signs of extracellular fluid overload (which contains abundant Na+) excludes this possibility and rather points toward water retention with dilutional hyponatremia.
Distal-working diuretics [i.e., thiazide-like diuretics, mineralocorticoid receptor antagonists (MRA), and amiloride] may contribute in particular to the occurrence of hyponatremia, as they interfere with the urine dilution capacity of the kidneys [13, 27]. More often than not, however, this form of hyponatremia occurs in normo- or hypervolemia and thus reflects a problem of free water excretion rather than true Na+ depletion. In patients with HF, treatment with thiazide-like diuretics elicits the risk of hyponatremia, usually occurring soon after initiation and reversible after stopping [27, 28]. In the double-blind, placebo-controlled Safety and Efficacy of the Combination of Loop with Thiazide-type Diuretics in Patients with Decompensated Heart Failure (CLOROTIC) trial, including 230 patients with AHF randomized to receive oral hydrochlorothiazide or placebo in addition to an intravenous furosemide regimen, 8.8% developed hyponatremia ≤ 130 mmol/L in the thiazide group versus only 5.2% in the placebo arm, a difference that was not statistically significant [29]. In a Japanese cohort study with 1844 consecutive AHF cases, the risk of hyponatremia was significantly higher in patients treated with thiazide-like diuretics, regardless of the dose of loop diuretics [30].
Dilutional Hyponatremia
As explained, hyponatremia in HF is usually a state of water overload rather than Na+ depletion, hence, dilutional hyponatremia. The cause of dilutional hyponatremia is reduced urine dilution capacity and impaired free water excretion by the kidneys. Urine dilution is performed in the distal nephron (i.e., distal convoluted tubules, collecting tubules, and collecting ducts) through Na+ reabsorption by the Na+-chloride co-transporter (NCC) and epithelial Na+ channels (ENaCs) in an otherwise water-impermeable part of the nephron (Fig. 2). To achieve this process efficiently, three conditions must be met: (1) active NCCs and ENaCs; (2) impermeability of the distal nephron for water; and (3) adequate flux of tubular fluid through the distal nephron. In contrast, urine concentration requires the build-up of an osmotic gradient in the renal interstitium, partly driven by sodium and chloride uptake in the ascending part of Henle’s loop.
Both the NCC and ENaCs are stimulated by neurohumoral activation, in particular, via the renin–angiotensin–aldosterone system [18]. As a result they are almost always normally active to hyperactive in HF. However, as explained, thiazide-like diuretics and MRA specifically inhibit these receptors, thereby reducing free water excretion while promoting natriuresis, which may cause or worsen hyponatremia.
Additionally, the capacity of the kidneys for urine dilution is reduced in HF because the distal nephron is leakier for water. AVP (i.e., anti-diuretic hormone) leads to the movement of aquaporin-2 channels toward the luminal membrane of these ducts [31]. Because the renal medulla is hypertonic, permeability of the ducts for water promotes free water reabsorption according to an osmotic gradient [32]. Several studies have demonstrated that AVP levels are elevated in HF, making the collecting ducts more permeable for water [33, 34].
These elevated levels are mainly caused by neurohumoral activation with non-osmotic AVP release, explaining why hyponatremia is more frequent in advanced HF with low cardiac output [13]. Because of a reduced effective circulatory volume in such cases, the plasma volume is defended at a higher set point [35]. Yet, patients with HF benefit from a normal to slightly contracted plasma volume, which is associated with a lower risk of hospital admissions or death [36]. Potent neurohumoral inhibition with guideline-directed medical therapies may help to reduce the plasma volume set point and decrease the risk of hyponatremia. In particular, Na+-glucose co-transporter-2 (SGLT2) inhibitors that inhibit proximal tubular reabsorption and bring more Na+ (and chloride) to the distal nephron, diminish the plasma volume without further deleterious neurohumoral activation [18, 37].
An often overlooked, but main contributor to hyponatremia in HF is insufficient tubular flow through the diluting (distal) tubular segments of the nephron [13]. The amount of tubular fluid that flows through the distal convoluted tubules, collecting tubules, and collecting ducts represents the theoretical maximal free water excretion (if complete Na+ reabsorption without any permeability for water would be achieved). Because of the aforementioned rise in AVP and potentially the use of thiazide-like diuretics and ENaC blockers, this theoretical maximum is however significantly reduced. Many patients with HF have a reduced glomerular filtration rate and their proximal tubular absorption is usually increased because of higher angiotensin II levels and impaired renal blood flow [18]. As a result, distal tubular flow may be easily decreased to 2–2.5 L or less per 24 h, significantly impacting on the kidneys’ ability for free water excretion [13]. Improving renal blood flow through hemodynamic optimization and inhibiting proximal tubular Na+ absorption with diuretics (i.e., acetazolamide and SGLT2 inhibitors) may (partly) restore the urine dilution capacity.
Approach to the Patient with Heart Failure and Hyponatremia
General Diagnostic Approach
A comprehensive medical history taking, review of the medications, and clinical exam should be performed in any patient presenting with hyponatremia. Patients should be asked about fluid intake, extra-renal losses, concomitant acute or chronic illnesses, alcohol and illicit drug misuse, and the use of specific medications. Clues may point toward reasons for hyponatremia other than HF, which are beyond the scope of this review. There should be a very low threshold to confirm low plasma osmolality if pseudo-hyponatremia or hyponatremia with normal or elevated plasma osmolality cannot be reliably excluded (e.g., hyperglycemia). Laboratory testing should include a complete set of electrolytes with chloride, potassium, and magnesium, thyroid-stimulating hormone to exclude significant thyroid disease, and within a suggestive clinical setting tests to exclude adrenal insufficiency. With this general work-up, hypotonic hyponatremia in the context of HF can usually be confirmed. As most patients with HF and hyponatremia are taking maintenance diuretics, classic urine indices of osmolality and Na+ concentration are often difficult to interpret and usually unhelpful for differentiating between causes of hyponatremia, or in particular to establish a diagnosis of the syndrome of inappropriate anti-diuretic hormone (SIADH). The latter is mainly a diagnosis of exclusion, but should be considered also in patients with HF when hyponatremia is severe and/or an unfavorable trajectory of serum Na+ levels is observed despite appropriate treatment. For SIADH, an important part of the treatment is to increase to oral osmotic load with salt or preferable oral urea intake.
Severe Symptomatic Hyponatremia
Severe symptoms of hyponatremia such as coma, seizures, deep somnolence, and cardiorespiratory distress are usually not present unless hyponatremia is severe (serum Na+ concentration < 120–125 mmol/L) and more likely to occur with an acute or subacute onset of hyponatremia [38, 39]. Such patients should definitely be managed in an intensive care or stepdown unit with the possibility of frequent serum Na+ controls. In patients with severe, symptomatic hyponatremia, guidelines recommend the administration of 150 mL of 3% hypertonic saline, administered over 10–20 min through a central or peripheral line [38, 39]. Concerns about the use of hypertonic saline via a peripheral line originate from older studies with caustic amino acid solutions and are unfounded as the risk of phlebitis is actually low (~ 6.2%) and comparable with other solutions [40•]. An increase in serum Na+ concentration > 5 mmol/L or above the level of 125 mmol/L should be enough to reverse most severe symptoms and if not should lead to the consideration of alternative causes [41, 42]. In patients with HF, the risk of worsening congestion with hypertonic saline should always be balanced against the need to reverse severe symptoms of hyponatremia [43]. However, because the combination of hypertonic saline with diuretics markedly improves diuretic efficiency, this problem is usually easily managed and the risk of worsening congestion should not be overstated [44•].
It is rather unusual for HF to be the sole cause of severe hyponatremia < 120–125 mmol/L, so its occurrence should prompt the investigation for alternative causes after addressing urgent symptoms. This is mainly important because rapid correction of chronic, severe hyponatremia may result in the osmotic demyelination syndrome [45]. Occurrence of this condition remains anecdotal, but the neurological consequences are devastating and permanent. Therefore, after the initial increase in serum Na+ concentration to abate severe symptoms, it is generally recommended not to increase Na+ levels further than 10 mmol/L during the next 24 h or 18 mmol/L over 48 h. Intriguingly, a recent, large (n = 3274), multi-center, observational study has called this practice into question, as it found a shorter length of hospitalization and lower in-hospital mortality with more rapid correction [46••]. About a third of the population had HF and those patients seemed to benefit more from rapid correction. All but one of the seven patients who developed osmotic demyelination syndrome in the study (corresponding to an overall incidence of 0.2%) had alcohol use disorder, malnutrition, hypokalemia, or hypophosphatemia, indicating that more caution is needed when these risk factors are present.
Treating Depletional Hyponatremia
Because low potassium and magnesium levels directly contribute to low serum Na+ levels, the first step when treating hyponatremia in HF is aggressive repletion of those cations. We aim for serum potassium levels > 4 mmol/L and serum magnesium levels > 0.85 mmol/L (or 2.1 mg/dL) at the higher end of the normal laboratory range. In those patients with clear signs and symptoms of hypovolemia, halting all diuretics is indicated and a fluid bolus of isotonic crystalloid solution may be considered. The benefit of using an isotonic rather than a hypertonic solution if no severe symptoms are present is that it constitutes a diagnostic test at the same time. In case of true Na+ depletion, the serum Na+ concentration will rise subsequently, while an unrecognized SIADH will see the Na+ concentration drop further. In most scenarios of depletion, Na+ is lost as Na-chloride with concomitant losses of potassium-chloride as well. Therefore, serum chloride levels are often disproportionally low, hence, “contraction or hypochloremic alkalosis.” A serum Na+ minus chloride concentration > 40 mmol/L is thus another good clue that hyponatremia is mainly depletional. When providing fluids (or diuretics as explained below), it is always a good idea to obtain a fresh urine sample afterward and measure the urine Na+ and potassium concentrations. The electrolyte-free water clearance, which ultimately determines the impact on the serum Na+ concentration, may be calculated from those [47]. If the sum of the serum concentrations of Na+ and potassium exceeds their respective counterparts in the urine, electrolyte-free water is excreted and the serum Na+ concentration will rise. Vice versa, if the sum of both urine concentrations is higher than the total plasma concentration, the serum Na+ concentration falls. This knowledge allows anticipation and early treatment changes in case of any unforeseen and unwanted effects.
Treating Dilutional Hyponatremia
Optimizing Hemodynamics and Renal Blood Flow
As explained, poor distal nephron perfusion is the most important contributor to dilutional hyponatremia in HF. Therefore, any therapy that improves renal blood flow would be expected to restore serum Na+ levels in this scenario. Indeed, increased renal blood flow translates into a higher glomerular filtration rate and hence total tubular flux, as well as a decreased filtration fraction, which is associated with less proximal reabsorption and thus more flow toward the distal nephron, boosting free water excretion capacity [13, 18]. Optimizing systemic hemodynamics with vasoactive therapies, diuretics, and carefully selected use of inotropes and/or mechanical circulatory support may aid renal perfusion in acute and advanced HF [48] with subsequent, favorable effect on the serum Na+ concentration.
Implementing Guideline-Directed Medical Therapies for Heart Failure
Increased neurohumoral activation contributes to systemic and renal vasoconstriction, while promoting non-osmotic AVP release, both facilitating hyponatremia development. At least in HF with reduced ejection fraction (where hyponatremia is more frequent), it is also a central driver of disease progression. Therefore, rapid initiation and up-titration of guideline-directed medical therapies such as renin-angiotensin system blockers or angiotensin-neprilysin inhibitors, beta blockers, and MRA is at least equally if not more important in patients with HF and hyponatremia [49, 50]. With an improving underlying HF status, these treatments may provide a durable restoration of normal serum Na+ levels as well. Renin-angiotensin system blockers, in particular, promote predominant vasodilation of the efferent arterioles of the nephron, thereby increasing renal blood flow and decreasing the intra-glomerular pressure and filtration fraction. Consequently, their use in HF has been consistently associated with small increases in serum Na+ levels [51, 52].
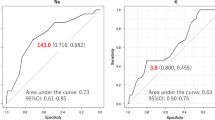
MRA are a foundational therapy in HF with reduced ejection fraction and among the first medications considered in HF with preserved ejection fraction [49, 50]. MRA promote natriuresis through inhibition of ENaCs in the distal nephron [18]. Therefore, they reduce the kidneys’ capacity of free water excretion and—just like thiazide-like diuretics—may promote hyponatremia [13]. In the Eplerenone Post-Acute Myocardial Infarction Heart Failure Efficacy and Survival Study (EPHESUS), the use of eplerenone versus placebo in patients with left ventricular dysfunction after a myocardial infarction was associated with a serum Na+ concentration that was on average 1 mmol/L lower (with a highly significant p-value of < 0.0001) and with a higher incidence of hyponatremia (15% vs. 11%; p = 0.0001) [53••]. Importantly, favorable effects of eplerenone on mortality or HF hospitalizations were observed among the whole spectrum of serum Na+ concentrations. Consequently, clinicians should probably be permissive for low-grade chronic hyponatremia caused by MRA in HF, as benefits seem to clearly outweigh the risk. Nonetheless, only a minority of patients in the EPHESUS actually had hyponatremia at baseline (i.e., 6%) and most of these cases were not severe. In HF with severe hyponatremia, temporarily interrupting MRA with reintroduction after achieving reasonably safe serum Na+ levels > 130 mmol/L may still be considered in individual cases, especially at the higher end of the left ventricular ejection fraction spectrum where the evidence in favor of MRA is less compelling.
Sodium-Glucose Co-transporter-2 Inhibitors
SGLT2 inhibitors are a foundational therapy in any patient with HF, irrespective of the ejection fraction [49, 50]. Some features of SGLT2 inhibitors make them of particular interest to patients with hyponatremia. Because the SGLT2 is only present in the proximal tubules of the nephron, SGLT2 inhibitors decrease proximal tubular reabsorption, thereby increasing distal nephron flow, which improves the capacity for free water excretion [54]. Moreover, predominantly in patients with hyperglycemia, SGLT2 inhibitors cause glycosuria as well, which acts as an osmotic diuretic, thereby removing electrolyte-free water. Recent data suggest that SGLT2 inhibitors are also effective in SIADH, with a more pronounced effect in severe hyponatremia < 125 mmol/L [55••]. Consequently, SGLT2 inhibitors protect against (worsening) hyponatremia, which is further helped by their favorable long-term effects on the underlying HF. Indeed, mortality and HF readmissions are reduced to a similar extent in patients with versus without hyponatremia [56•]. Thus, SGLT2 inhibitors are probably the first guideline-directed medical therapy to consider in patients with HF and hyponatremia.
Fluid Restriction
General recommendations for fluid restriction in HF are under increased scrutiny because of questionable benefits and poor adherence. The soon-to-report Fluid Restriction in Heart Failure versus Liberal Fluid Uptake (FRESH-UP) study will provide more insight, as it is currently studying the impact of fluid restriction < 1.5 L versus usual care on quality of life and safety in HF [57].
In patients with hyponatremia however, most clinicians still recommend strict fluid restriction. The rationale is that hyponatremia in HF is classically a dilutional hyponatremia, resulting from water overload rather than Na+ depletion. However, one should not forget that in most patients, the intracellular volume is actually slightly contracted (Fig. 1). Moreover, because the central pathophysiological culprit is poor distal nephron flow through a leakier tubular system, the capacity for free water excretion may be decreased well below 500 mL, a target that is obviously not attainable with fluid restriction [13]. Thus, while moderate to strict fluid restriction may somewhat help to keep the serum Na+ concentration within the desired range, it should probably not be the primary focus of management.
Diuretic Therapy
Dilutional hyponatremia is often present in patients with acute HF and fluid overload, which may pose a challenge for diuretic treatment. Indeed, especially those patients with persistent hyponatremia have more advanced HF with more severe diuretic resistance, less successful decongestion, and hence poor long-term outcomes [12]. The primary focus in such patients should remain with achieving complete decongestion rather than focusing too heavily on the serum Na+ concentration. In fact, the best chance to obtain and keep normal serum Na+ levels on the long term in those patients is with a state-of-the-art treatment of the underlying HF. Nevertheless, choosing diuretic combinations carefully may help to keep the serum Na+ concentration within range and will often resolve the problem of hyponatremia.
Loop diuretics are the backbone of diuretic treatment in acute HF [49, 58, 59]. They inhibit the Na+-potassium-chloride co-transporter in the ascending limb of Henle’s loop. This transport plays a crucial role to trap Na+ and chloride within the renal interstitium, thereby creating a hypertonic gradient toward the medulla that is needed for the process of urine concentration and represents the driving force for water absorption in the collecting ducts [18]. Inhibition of this process by loop diuretics generally produces hypotonic urine, providing relative protection against hyponatremia. The addition of acetazolamide to loop diuretics leads to more efficient and faster decongestion, as was shown in the Acetazolamide in Decompensated Heart Failure with Volume Overload (ADVOR) trial [60]. Because acetazolamide is a potent inhibitor of proximal tubular Na+ reabsorption, it markedly increases distal tubular flow, promoting free water excretion [13]. Therefore, it probably represents the first-choice agent (together with SGLT2 inhibitors) to tackle diuretic resistance in patients with HF and hyponatremia, with a low threshold if not universal upfront use in hospitalized patients with acute HF. For reasons explained, thiazide-like diuretics may worsen hyponatremia, making them less suitable in this population. However, in cases of severe diuretic resistance, sequential nephron blockade with thiazide-like diuretics may be needed, also in patients with hyponatremia. In those cases, monitoring urine indices is very helpful. A urine Na+ concentration > 80 mmol/L indicates good diuretic efficiency and was associated with higher odds for decongestion and better outcomes in the ADVOR trial [61]. We would currently only consider the use of thiazide-like diuretics in patients with HF and hyponatremia who demonstrate a urine Na+ concentration ≤ 80 mmol/L despite treatment with acetazolamide on top of adequately dosed loop diuretics (on a background of SGLT2 inhibitors and low-dose MRA). At the same time, a negative electrolyte-free water clearance should be avoided as it indicates worsening hyponatremia. Therefore, a urine Na+ concentration 80–100 mmol/L is probably about the target range in such difficult cases, also depending on the amount of kaliuresis and the actual serum Na+ level.
Conclusions
Hyponatremia in HF is associated with worse functional and cognitive status as well as adverse outcomes, but it remains unclear whether this relationship is causal. Typically, it represents impaired water excretion by the kidneys because of diminished renal blood flow that leads to compromised tubular flux through the distal diluting part of the nephron on a background of increased neurohumoral activation with non-osmotic AVP release, making this part more permeable to water. Low potassium and magnesium levels often contribute to hyponatremia in HF and should be aggressively repleted. Further treatment should focus on the underlying HF and adequately address congestion. For this goal, proximally acting diuretics including SGLT2 inhibitors, acetazolamide, and loop diuretics are preferred, with thiazide-like diuretics being reserved for severe diuretic resistance. Our therapeutic approach toward a patient with HF and hyponatremia is provided in Fig. 3.
Data Availability
No datasets were generated or analysed during the current study.
Abbreviations
- AVP:
-
Arginine vasopressin
- ENaCs:
-
Epithelial sodium channels
- HF :
-
Heart failure
- MRA:
-
Mineralocorticoid receptor antagonists
- Na+ :
-
Sodium
- NCC:
-
Sodium-chloride co-transporter
- SGLT2:
-
Sodium-glucose co-transporter-2
- SIADH:
-
Syndrome of inappropriate anti-diuretic hormone
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Davila CD, Udelson JE. Hypervolemic hyponatremia in heart failure. Front Horm Res. 2019;52:113–29.
Upadhyay A, Jaber BL, Madias NE. Incidence and prevalence of hyponatremia. Am J Med. 2006. https://doi.org/10.1016/J.AMJMED.2006.05.005.
Adrogué HJ, Madias NE. Hyponatremia. N Engl J Med. 2000;342:1581–9.
Mohan S, Gu S, Parikh A, Radhakrishnan J. Prevalence of hyponatremia and association with mortality: results from NHANES. Am J Med. 2013. https://doi.org/10.1016/J.AMJMED.2013.07.021.
Adrogué HJ, Tucker BM, Madias NE. Diagnosis and management of hyponatremia: a review. JAMA. 2022;328:280–91.
Renneboog B, Musch W, Vandemergel X, Manto MU, Decaux G. Mild chronic hyponatremia is associated with falls, unsteadiness, and attention deficits. Am J Med. 2006;119:71.e1-71.e8.
Albabtain M, Brenner MJ, Nicklas JM, Hummel SL, McCormick MP, Pawlowski JL, Remington TL, Gure TR, Dorsch MP, Bleske BE. Hyponatremia, cognitive function, and mobility in an outpatient heart failure population. Med Sci Monit. 2016;22:4978–85.
Gheorghiade M, Rossi JS, Cotts W, et al. Characterization and prognostic value of persistent hyponatremia in patients with severe heart failure in the ESCAPE Trial. Arch Intern Med. 2007;167:1998–2005.
Wald R, Jaber BL, Price LL, Upadhyay A, Madias NE. Impact of hospital-associated hyponatremia on selected outcomes. Arch Intern Med. 2010;170:294–302.
Omar HR, Charnigo R, Guglin M. Prognostic significance of discharge hyponatremia in heart failure patients with normal admission sodium (from the ESCAPE Trial). Am J Cardiol. 2017;120:607–15.
Holland-Bill L, Christiansen CF, Heide-Jørgensen U, Ulrichsen SP, Ring T, Jørgensen JOL, Sørensen HT. Hyponatremia and mortality risk: a Danish cohort study of 279 508 acutely hospitalized patients. Eur J Endocrinol. 2015;173:71–81.
Verbrugge FH, Grodin JL, Mullens W, Taylor DO, Starling RC, Tang WHW. Transient hyponatremia during hospitalization for acute heart failure. Am J Med. 2016;129:620–7.
Verbrugge FH, Steels P, Grieten L, Nijst P, Tang WHW, Mullens W. Hyponatremia in acute decompensated heart failure: depletion versus dilution. J Am Coll Cardiol. 2015;65:480–92.
Adrogué HJ, Madias NE. The challenge of hyponatremia. J Am Soc Nephrol. 2012;23:1140–8.
Katz MA. Hyperglycemia-induced hyponatremia — calculation of expected serum sodium depression. N Engl J Med. 2010;289:843–4.
Hillier TA, Abbott RD, Barrett EJ. Hyponatremia: evaluating the correction factor for hyperglycemia. Am J Med. 1999;106:399–403.
Wester PO, Dyckner T. Problems with potassium and magnesium in diuretic-treated patients. Acta Pharmacol Toxicol (Copenh). 1984;54(Suppl 1):59–65.
Verbrugge FH, Dupont M, Steels P, Grieten L, Swennen Q, Tang WHW, Mullens W. The kidney in congestive heart failure: “are natriuresis, sodium, and diuretics really the good, the bad and the ugly?” Eur J Heart Fail. 2014;16:133–42.
Re C, We S, Db C, Fe C, Dc D. The extrarenal correction of alkalosis associated with potassium deficiency. J Clin Invest. 1952;31:798–805.
Al Alawi AM, Majoni SW, Falhammar H. Magnesium and human health: perspectives and research directions. Int J Endocrinol. 2018. https://doi.org/10.1155/2018/9041694.
Collins AJ, Pitt B, Reaven N, Funk S, Mcgaughey K, Wilson D, Bushinsky DA. Association of serum potassium with all-cause mortality in patients with and without heart failure, chronic kidney disease, and/or diabetes. Am J Nephrol. 2017;46:213–21.
Aboujamous H, Walton T, Doran JJ. Evaluation of the change in serum potassium levels after potassium administration. J Clin Nephrol Ren Care. 2016;2:013.
Workinger JL, Doyle RP, Bortz J. Challenges in the diagnosis of magnesium status. Nutrients. 2018. https://doi.org/10.3390/NU10091202.
McKie PM, Schirger JA, Costello-Boerrigter LC, et al. Impaired natriuretic and renal endocrine response to acute volume expansion in pre-clinical systolic and diastolic dysfunction. J Am Coll Cardiol. 2011;58:2095–103.
Nijst P, Verbrugge FH, Grieten L, Dupont M, Steels P, Tang WHW, Mullens W. The pathophysiological role of interstitial sodium in heart failure. J Am Coll Cardiol. 2015;65:378–88.
Nijst P, Olinevich M, Hilkens P, Martens P, Dupont M, Tang WHW, Lambrichts I, Noben JP, Mullens W. Dermal interstitial alterations in patients with heart failure and reduced ejection fraction: a potential contributor to fluid accumulation? Circ Heart Fail. 2018. https://doi.org/10.1161/CIRCHEARTFAILURE.117.004763.
Jentzer JC, Dewald TA, Hernandez AF. Combination of loop diuretics with thiazide-type diuretics in heart failure. J Am Coll Cardiol. 2010;56:1527–34.
Liamis G, Filippatos TD, Elisaf MS. Thiazide-associated hyponatremia in the elderly: what the clinician needs to know. J Geriatr Cardiol. 2016;13:175–82.
Trullàs JC, Morales-Rull JL, Casado J, et al. Combining loop with thiazide diuretics for decompensated heart failure: the CLOROTIC trial. Eur Heart J. 2023;44:411–21.
Yamazoe M, Mizuno A, Kohsaka S, Shiraishi Y, Kohno T, Goda A, Higuchi S, Yagawa M, Nagatomo Y, Yoshikawa T. Incidence of hospital-acquired hyponatremia by the dose and type of diuretics among patients with acute heart failure and its association with long-term outcomes. J Cardiol. 2018;71:550–6.
Bankir L. Antidiuretic action of vasopressin: quantitative aspects and interaction between V1a and V2 receptor-mediated effects. Cardiovasc Res. 2001;51:372–90.
Oren RM. Hyponatremia in congestive heart failure. Am J Cardiol. 2005;95:2–7.
Goldsmith SR, Francis GS, Cowley AW, Barry Levine T, Cohn JN. Increased plasma arginine vasopressin levels in patients with congestive heart failure. J Am Coll Cardiol. 1983;1:1385–90.
Francis GS, Benedict C, Johnstone DE, Kirlin PC, Nicklas J, Liang CS, Kubo SH, Rudin-Toretsky E, Yusuf S. Comparison of neuroendocrine activation in patients with left ventricular dysfunction with and without congestive heart failure. A substudy of the Studies of Left Ventricular Dysfunction (SOLVD). Circulation. 1990;82:1724–9.
Miller WL, Lobo R, Grill DE, Mullan BP. Diuresis-related weight loss reflects interstitial compartment decongestion with minimal impact on intravascular volume expansion or outcomes in post-acute heart failure: metrics of decongestion and volume status. J Card Fail. 2021;27:445–52.
Martens P, Nijst P, Dupont M, Mullens W. The optimal plasma volume status in heart failure in relation to clinical outcome. J Card Fail. 2019;25:240–8.
Griffin M, Rao VS, Ivey-Miranda J, et al. Empagliflozin in heart failure. Circulation. 2020;142:1028–39.
Verbalis JG, Goldsmith SR, Greenberg A, Korzelius C, Schrier RW, Sterns RH, Thompson CJ. Diagnosis, evaluation, and treatment of hyponatremia: expert panel recommendations. Am J Med. 2013. https://doi.org/10.1016/J.AMJMED.2013.07.006.
Spasovski G, Vanholder R, Allolio B, et al. Clinical practice guideline on diagnosis and treatment of hyponatraemia. Nephrol Dial Transplant. 2014. https://doi.org/10.1093/NDT/GFU040.
• Madieh J, Hasan B, Khamayseh I, Hrizat A, Salah T, Nayfeh T, Gharaibeh K, Hamadah A. The safety of intravenous peripheral administration of 3% hypertonic saline: a systematic review and meta-analysis. Am J Med Sci. 2023;366:135–42. Systematic review and meta-analysis showing that hypertonic saline can be safely administered through a peripheral line.
Koenig MA, Bryan M, Lewin JL, Mirski MA, Geocadin RG, Stevens RD. Reversal of transtentorial herniation with hypertonic saline. Neurology. 2008;70:1023–9.
Sterns RH, Nigwekar SU, Hix JK. The treatment of hyponatremia. Semin Nephrol. 2009;29:282–99.
Rodriguez M, Hernandez M, Cheungpasitporn W, Kashani KB, Riaz I, Rangaswami J, Herzog E, Guglin M, Krittanawong C. Hyponatremia in heart failure: pathogenesis and management. Curr Cardiol Rev. 2019;15:252–61.
• Griffin M, Soufer A, Goljo E, et al. Real world use of hypertonic saline in refractory acute decompensated heart failure: a U.S. center’s experience. JACC Heart Fail. 2020;8:199–208. Large cohort study on the use of hypertonic saline in acute heart failure.
Plrzada NA, Au II. Central pontine myelinolysis. Mayo Clin Proc. 2001;76:559–62.
•• Seethapathy H, Zhao S, Ouyang T, et al. Severe hyponatremia correction, mortality, and central pontine myelinolysis. NEJM Evidence. 2023. https://doi.org/10.1056/EVIDOA2300107. Large meta-analysis that surprisingly suggested that faster correction of hyponatremia may be potentially associated with better outcomes, in particular in patients with heart failure.
Mallie JP, Bichet DG, Halperin ML. Effective water clearance and tonicity balance: the excretion of water revisited. Clin Invest Med. 1997;20:16–24.
Vanhentenrijk S, Verbrugge FH, Tang WHW, Menon V. PRO: vasodilators remain an indispensable treatment for acute heart failure. Eur Heart J Acute Cardiovasc Care. 2022;11:850–7.
McDonagh TA, Metra M, Adamo M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42:3599–726.
Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022;145:E895–1032.
Balling L, Kober L, Schou M, Torp-Pedersen C, Gustafsson F. Efficacy and safety of angiotensin-converting enzyme inhibitors in patients with left ventricular systolic dysfunction and hyponatremia. J Card Fail. 2013;19:725–30.
Packer M, Medina N, Yushak M. Correction of dilutional hyponatremia in severe chronic heart failure by converting-enzyme inhibition. Ann Intern Med. 1984;100:782–9.
•• Martens P, Ferreira JP, Vincent J, et al. Serum sodium and eplerenone use in patients with a myocardial infarction and left ventricular dysfunction or heart failure: insights from the EPHESUS trial. Clin Res Cardiol. 2022;111:380–92. Important secondary analysis from the EPHESUS trial showing that although eplerenone, and presumably other mineralocorticoid receptor antagonists as well, modestly lowers serum sodium concentrations, treatment is still associated with benefits on hard clinical endpoints such as death or heart failure readmissions in patients with mild hyponatremia.
Verbrugge FH, Martens P, Mullens W. SGLT-2 inhibitors in heart failure: implications for the kidneys. Curr Heart Fail Rep. 2017;14:331–7.
•• Refardt J, Imber C, Sailer CO, et al. A randomized trial of empagliflozin to increase plasma sodium levels in patients with the syndrome of inappropriate antidiuresis. J Am Soc Nephrol. 2020;31:615–24. This randomized trial showed that the sodium-glucose co-transporter-2 inhibitor empagliflozin has favorable effects on the plasma sodium level in patients with hyponatremia due to the syndrome of inappropriate anti-diuretic hormone.
• Yeoh SE, Docherty KF, Jhund PS, et al. Relationship of dapagliflozin with serum sodium: findings from the DAPA-HF Trial. JACC Heart Fail. 2022;10:306–18. Secondary analysis from the DAPA-HF trial, showing that the favorable effects of dapagliflozin on death and heart failure readmissions were maintained over the entire range of serum sodium concentrations.
Herrmann JJ, Beckers-Wesche F, Baltussen LEHJM, et al. Fluid REStriction in Heart Failure vs Liberal Fluid UPtake: rationale and design of the randomized FRESH-UP Study. J Card Fail. 2022;28:1522–30.
Meani P, Pagnoni M, Mondellini GM, Fiorenza S, Brunner-La Rocca HP. Impact of loop diuretic dosage in a population of patients with acute heart failure: a retrospective analysis. Front Cardiovasc Med. 2023. https://doi.org/10.3389/FCVM.2023.1267042.
Mullens W, Damman K, Harjola VP, et al. The use of diuretics in heart failure with congestion - a position statement from the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2019;21:137–55.
Mullens W, Dauw J, Martens P, et al. Acetazolamide in acute decompensated heart failure with volume overload. N Engl J Med. 2022;387:1185–95.
Verbrugge FH, Martens P, Dauw J, et al. Natriuretic response to acetazolamide in patients with acute heart failure and volume overload. J Am Coll Cardiol. 2023;81:2013–24.
Author information
Authors and Affiliations
Contributions
Both authors wrote the manuscript together.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mondellini, G.M., Verbrugge, F.H. Evaluation and Management of Hyponatremia in Heart Failure. Curr Heart Fail Rep 21, 252–261 (2024). https://doi.org/10.1007/s11897-024-00651-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11897-024-00651-3