Abstract
Purpose of Review
To analyze the pathophysiologic importance of the right heart in different types of congenital heart disease (CHD), summarize current diagnostic modalities, and discuss treatment options.
Recent Findings
The right ventricle (RV) plays a key role in disease progression and prognosis, either as the subpulmonary or as the systemic ventricle. Volume and/or pressure overload as well as intrinsic myocardial disease are the main factors for RV remodeling. Echocardiography and cardiac magnetic resonance imaging are important noninvasive modalities for assessing anatomy, size, and function of the right heart. Timely repair of related lesions is essential for preventing RV dysfunction. Few inconclusive data exist on conventional pharmacotherapy in CHD-related RV dysfunction. Cardiac resynchronization therapy and ventricular assist devices are an option in patients with advanced systemic RV failure.
Summary
Right heart disease is highly related with adverse clinical outcomes in CHD. Research should focus on early identification of patients at risk and development of medical and interventional treatments that improve RV function.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In patients with congenital heart disease (CHD), the right ventricle (RV) plays a key role in disease progression and prognosis, either as the subpulmonary ventricle, mostly affected by volume or pressure overload in patients with atrial septal defects (ASD), tetralogy of Fallot (TOF), Ebstein’s anomaly of the tricuspid valve, pulmonary stenosis, and pulmonary valve atresia or as the systemic ventricle encountered in congenitally corrected transposition of the great arteries (cc-TGA), d-transposition of the great arteries (TGA) with previous atrial switch repair, and hypoplastic left heart syndrome (HLHS) with Fontan palliation. In many of these patients, congenital malformations, palliations, residual defects, and their resultant physiology as well as the high-pressure pulmonary or systemic circulation impact the RV, and this relationship impacts morbidity and mortality [1]. Apart from the RV, the right atrium (RA) is also affected in many repaired or unrepaired defects, in which atrial arrhythmias, thrombi formation, and/or paradoxical emboli are frequently encountered [2]. The increased morbidity caused by right heart dysfunction is also related to re-interventions and lengthy hospitalizations posing a high economic burden on healthcare systems [3].
In this paper, we will review the pathophysiologic mechanisms of right heart dysfunction and related complications in different CHD entities, summarize current noninvasive diagnostic modalities and their role in risk stratification, and discuss treatment options.
Pathophysiological Mechanisms of Right Heart Disease
Basic pathophysiologic mechanisms that are primarily responsible for right heart disease in several patients with CHD are volume and/or pressure overload (Figure 1). The RV adapts better to chronic volume overload caused by chronic left-to-right shunt or pulmonary valve regurgitation than to pressure overload, encountered in severe pulmonary hypertension (PH) or presence of a systemic RV [2]. In addition, the RV tolerates better an excess volume than the left ventricle (LV) does [4]; therefore, RV systolic dysfunction manifests later than LV dysfunction owing to LV volume overload. Adaptation of the right heart to chronic volume overload entails progressive dilatation of a compliant thin-walled RV and RA, associated with an increased risk of atrial tachyarrhythmias, especially in patients with septal defects. Tricuspid regurgitation (TR) secondary to tricuspid annular dilatation may also lead to additional chamber dilatation and progression of right heart dysfunction. Moreover, a combination of RV pressure and volume overload, as observed in patients with ToF and mixed pulmonary stenosis and regurgitation, may contribute to a progressive right heart disease.
Impact of different pathophysiologic mechanisms in the right heart disease. ASD: atrial septal defect, BNP: brain natriuretic peptide, CPET: cardiopulmonary exercise testing, EA: Ebstein’s anomaly, hs-TnT: high-sensitive troponine T, RHD: right heart disease, RV: right ventricle, PA: pulmonary artery, SCD: sudden cardiac death, ToF: tetralogy of Fallot
In patients with cc-TGA or surgical palliation of d-transposition of the great arteries with atrial switch and in patients with HLHS, the RV adopts the role of the systemic ventricle (SRV) and transforms itself from a low-resistance pulmonary pump to a high resistance systemic pump, with a long-term exposure to a high-pressure circuit, leading to a higher likelihood of RV dilatation, systemic atrioventricular valve regurgitation (SAVVR), and systemic RV failure [5]. In these patients, myocardial ischemia may also contribute to the progression of RV failure.
Moreover, diastolic RV dysfunction may be encountered in certain CHD groups, manifesting with increased RV filling pressures, ventricular relaxation or RV restrictive filling patterns. Evaluation of RV diastolic parameters may be challenging in the presence of significant TR.
Finally, it is acknowledged that any anatomical or functional abnormalities of the right heart may also affect the left heart, since both ventricles coexist in the same pericardial sack and share the circumferential layer of myocardial fibers (mechanical coupling). Adverse ventricular interdependence is prominent in all patients with CHD that affect primarily the right heart [6]. A diastolic and/or systolic movement of the interventricular septum to the left, as well as pericardial constraint caused by the RV volume overload, impairs LV geometry and thus affect LV preload. In addition, reduced distensibility of the shared myocardial fibers, caused by dilated RV, impairs the LV contractility according to the Frank-Starling law.
Subpulmonary Right Ventricle
Atrial Septal Defects
ASD is one of the most common CHD, with ostium secundum ASD accounting for 80% of all ASDs, followed by ostium primum defect and sinus venosus ASD [7]. ASDs may be encountered as isolated lesions or in combination with anomalous pulmonary venous connections, persistent left superior vena cava, pulmonary stenosis, and mitral valve prolapse. The shunt volume depends on RV to LV compliance, defect size, and left atrium (LA) to right atrial (RA) pressure gradient. RV volume overload and pulmonary overcirculation occur initially in the setting of a significant left-to-right shunt. Aging decreases LV compliance (along with arterial hypertension and valvular or ischemic heart disease) and increases LA pressure, resulting in shunt increase and symptom worsening. If ASD is not timely closed, right heart volume overload leads to increased morbidity (exercise intolerance, HF, atrial arrhythmias, thromboembolic events, and PH) and mortality [8].
Transthoracic echocardiogram (TTE) is the first-line imaging modality to assess the location, size and shape of the defect, the degree and direction of shunting, and the hemodynamic impact on the size and shape of the right heart chambers [7]. Echocardiographic signs of RV volume overload are RV dilatation and interventricular septal flattening during diastole, indicative of a hemodynamic significant ASD that merits closure. The presence of RV hypertrophy, interventricular septal flattening during diastole and systole (D-shaped LV), short right ventricular outflow tract (RVOT) acceleration time of pulmonary ejection with midsystolic notching, and elevated RV systolic pressure (RVSP), determined from peak TR velocity by the simplified Bernoulli equation, are indicative of increased pulmonary vascular resistance that merits right heart catheterization (RHC) to guide optimal management. 3D echocardiography, especially with transoesophageal echocardiography (TOE), might provide incremental information on the rims of tissue surrounding the ASD and other technical aspects before transcatheter closure.
Cardiovascular magnetic resonance (CMR) can be used as a complementary method to assess hemodynamic and quantitative data. Noninvasive flow analysis is used to quantify shunt degree by measuring the ratio of the pulmonary flow over the systemic flow (Qp/Qs), and cine images enable accurate quantification of the volume and function of the dilated right heart chambers [9]. CMR can also detect partial anomalous pulmonary venous connections commonly associated with sinus venosus ASDs.
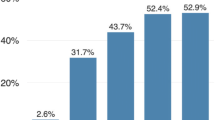
In general, RV volume overload is the most important parameter to guide ASD closure. Transcatheter device closure is the method of choice in secundum ASDs when technically feasible. After ASD closure, a marked decrease in RV volume is observed within the first year, with normalization of RV volume to be related with smaller preoperative RV volume [10]. A serial follow-up post-ASD closure is recommended, especially when defect closure occurs late during adulthood, to early diagnose atrial arrythmias and signs of PAH after defect closure, which is encountered in 3% of these patients [11].
Ebstein’s Anomaly of the Tricuspid Valve
Ebstein’s anomaly is a rare CHD of moderate or severe complexity characterized by abnormal formation and apical displacement of the septal and posterior leaflet of the tricuspid valve (TV), while the anterior leaflet is attached to the annulus, but is enlarged and sail-like in appearance. This apical displacement of the TV leaflets translates into an atrialized portion of the RV, a small remaining functional RV, and various degrees of tricuspid regurgitation [12]. Phenotypic expression and prognosis may vary and depend on the severity of the TV dysfunction, the degree of atrialization of the RV, the systolic function of the remaining RV, the degree of RA dilatation, and the arrhythmic burden [13]. Furthermore, mechanical dyssynchrony of the functional RV is associated with RV dysfunction and impaired exercise capacity [14].
Echocardiography sheds light on the anatomy and function of the TV (apical displacement of the septal or posterior leaflet (in adults ≥ 0.8 cm/m2 BSA), size of the anterior leaflet, tethering of the septal, or posterior TV leaflet on the septum or ventricular wall) and size and function of the right heart structures (RA, atrialized RV, remaining functional RV, RVOTO, and associated lesions) (Figure 2).
Imaging assessment of lesions affecting the subpulmonary right ventricle (RV). A 40-year-old patient with repaired tetralogy of Fallot and severe pulmonary regurgitation. A Transthoracic echocardiographic 4-chamber view shows a dilated RV with bulging of interventricular septum towards the left ventricle. B Continuous wave doppler in the pulmonary valve of the same patient shows a triangular diastolic trace indicative of severe pulmonary regurgitation. C Late gadolinium enhancement (LGE) is depicted in the akinetic right ventricular outflow tract (RVOT) region in CMR. A 30-year-old patient with a “mild” unoperated Ebstein’s anomaly. D Transthoracic echocardiographic 4 chamber view shows an apical displacement of the septal tricuspid valve leaflet (18mm), a dilated right atrium (RA) containing an atrialized portion of the RV and a quite sufficient remaining functional RV. E Color doppler shows a mild tricuspid regurgitation (yellow arrow). F CMR can be used to quantify the volume and function of the remaining functional RV as well as to better visualize the tricuspid valve anatomy
Estimating the severity of TR and RV size and function is crucial for decision-making regarding the time of surgery. Significant right heart dysfunction is an independent predictor of early post-surgical mortality [15]. TV reconstruction should be performed timely before excess RV volume overload and function worsening to achieve reverse RV remodeling.
TR assessment may be challenging due to the absence of systolic flow reversal in the hepatic veins (equalization of pressures between the RA and RV) and the inability to calculate vena contracta and proximal isovelocity surface area (possibility of more than one color jet) [9]. TOE can aid in better visualizing the tricuspid leaflet anatomy and evaluating the color Doppler jet. CMR is unvaluable for pre- and post-operative patient evaluation and risk stratification, as it enables high-quality views for quantification of the dilated right heart, RV function, and TV function. A CMR study showed impaired RV global radial strain (GRS) and global circumferential strain (GCS), with GRS being significantly compromised in patients with a severely displaced TV (>16 mm/m2) [16]. CMR-assessed variables, such as RVEF, total R/L volume index, RV/LV end diastolic volume ratio, and apical septal leaflet displacement/total LV septal length, are able to predict first-onset atrial tachycardia in patients with Ebstein’s anomaly of the tricuspid valve. In addition, RV and LV function assessed by CMR predicted major cardiovascular events [17].
Tetralogy of Fallot
TOF is the most common cyanotic CHD, consisting of a nonrestrictive subaortic ventricular septal defect (VSD) and varying degrees of RVΟΤ obstruction (RVOTO), due to anterior deviation of the conal septum. Although early surgical TOF repair has significantly improved survival into late adulthood, even patients with a “well-repaired” TOF (r-TOF) may have residual hemodynamic and electrophysiological abnormalities, related primarily with right heart disease [18].
Severe chronic pulmonary regurgitation (PR) is the most common residual lesion in patients with a transannular patch repair; although well tolerated for years, it eventually leads to symptomatic RV dilation and dysfunction associated with a worse prognosis [19]. With advances in transcatheter and surgical pulmonary valve replacement (PVR), early detection of RV enlargement and dysfunction has become increasingly important to optimize time for intervention. RV function in ToF is affected by preload (RV volume overload due to PR), afterload (RVOTO), and contractility, as well as by synchrony of contraction and ventricular interdependence [20]. Significant PR, RV outflow tract aneurysm, and akinesia can decrease cardiac output [21]. Co-existing RVOTO or distal pulmonary arterial stenoses augment the deleterious effects of severe PR on RV. Elevated RV pressure and RV hypertrophy due to RVOTO have been described as independent risk factors for poor outcome and decreased exercise performance, despite smaller RV volumes [22].
Echocardiography is an easily available and cost-effective tool to evaluate patients with ToF pre- and post-operatively. Echocardiographic assessment of RV size and function is challenging because of the shape of the RV [1]. Indirect 2D measures of the RV function, easily obtainable from the RV-focused apical 4-chamber view, are fractional area change (FAC) and tricuspid annular plane systolic excursion (TAPSE). Moreover, speckle tracking echocardiography has been introduced as a sensitive technique to assess myocardial deformation. RV free wall longitudinal strain has been shown to be an independent predictor of adverse clinical outcomes in patients with repaired TOF [23,24]. When technically feasible, 3D evaluation of RV volumes and RV ejection fraction (RVEF) is recommended in centers with experience in 3D TTE [9].
RV dilatation and interventricular septal flattening during diastole are indicative of a severe PR ± RVOTO in repaired TOF that needs further assessment. Significant TR may occur secondary to RV dilatation. In patients with TOF, an elevated RVSP may be attributed to RVOTO and/or pulmonary stenosis or may be indicative of PH in the absence of the previous etiologies. Furthermore, the presence of pulmonary arterial end-diastolic forward flow as assessed with continuous wave Doppler is indicative of a restrictive RV physiology that despite being a negative prognostic marker, especially in the early post-operative period, may have a protective role, when it emerges late in the course of ToF, as a less compliant RV may be protected from further enlargement in the presence of severe PR [25]. CMR is considered the gold standard to assess RV volume and function as well as the location and degree of myocardial fibrosis in patients with TOF, while it allows accurate quantification of PR and measurement of size, shape, and expansion of the pulmonary arteries in these patients.
Optimal timing for PVR remains challenging. PVR improves symptoms and reduces RV volumes, but a survival benefit still needs to be shown [26]. In asymptomatic patients with severe PR and/or RVOTO, when CMR measured end-systolic index exceeds 80 mL/m2 and/or the end-diastolic volume index exceeds 160 mL/m2 and/or there is progression of TR or RV systolic dysfunction, PVR should be considered [1]. RV to pulmonary arterial (PA) coupling indices could be sensitive markers of a progressive maladaptive RV response to long-standing volume overload that could guide timely PVR, before the onset of clinical symptoms and RV systolic dysfunction [27]. RV acceleration isovolumic contraction correlates with PR severity, demonstrating a reduced contractile function in relation to the degree of PR, and may be another early, sensitive index for selecting patients for PVR [28]. Finally, worsening of cardiopulmonary exercise indices in asymptomatic patients is associated with impaired RV function and may guide decision for PVR [29].
Ventricular tachycardia (VT) and sudden cardiac death (SCD) may be encountered later in life post-TOF repair and are closely related to RV dilatation and dysfunction. The length of the RVOT akinetic region was found to be a predictor of ventricular arrhythmias in adult TOF patients [30]. RV late gadolinium enhancement (LGE) at surgical sites is common after RVOT patching and/or resection of infundibular stenosis and correlates with RV dysfunction, exercise intolerance, neurohormonal activation, and clinical arrhythmias in TOF (Figure 2) [31, 32]. A recent analysis among 550 consecutive r-TOF patients that underwent CMR in an expert center demonstrated that the extent of RV LGE and a reduced RV ejection fraction ≤47%, along with the presence of LV LGE and LV dysfunction, were independent predictors of all-cause mortality together with an increased B-type natriuretic peptide, a reduced peak exercise oxygen uptake, prior sustained atrial arrhythmia, and age ≥50 years [33•]. Finally, T1 mapping as a novel technique to quantify diffuse RV myocardial fibrosis in ToF patients showed that the amount of diffuse RV myocardial fibrosis is associated with RV volume overload [34]. All these parameters should be taken into consideration, when selecting TOF patients at high risk for SCD that will benefit from the insertion of an implantable cardioverter defibrillator (ICD).
Pulmonary Arterial Hypertension/Eisenmenger Syndrome
The presence of a chronic systemic left-to-right shunt leads to pulmonary overcirculation that results in pulmonary vascular remodeling and a progressive increase in pulmonary vascular resistance. If the trigger factor persists, irreversible changes evolve to the development of PAH, which mainly affects RV size and function, related to a worse long-term prognosis [35]. With progression of the disease, bidirectional shunting occurs, which turns into a predominant right-to-left shunt with further worsening of the disease [36]. Maladaptation of the RV to the increased pulmonary artery pressures and resistance eventually results in progressive RV failure. Eisenmenger syndrome (ES) comprises the extreme end of PAH associated with CHD, which can occur in patients with large, unrepaired intracardiac or extracardiac shunts. RV is offloaded by the right-to-left shunt, sustaining cardiac output at the expense of cyanosis [37]. However, prognosis of ES is not as promising as previously thought due to immortal time bias [38]. In general, patients with a pre-tricuspid shunt tolerate the increase in pulmonary blood flow much better than patients with post-tricuspid shunts, and only a minority with an unrepaired pre-tricuspid shunt develops ES at an old age. In patients with ES, a mortality prediction model based on echocardiographic indices of right heart disease has been proposed, indicating the impact of right heart on the survival of these patients [39]. Unlike other patients with PAH, ES patients have an increased RV free wall transverse strain that correlates with a better survival compared to patients with idiopathic PAH [40].
Systemic Right Ventricle
Biventricular Systemic Right Ventricle Physiology
Patients with congenitally corrected TGA (ccTGA) and d-TGA after an atrial switch (Mustard or Senning) procedure have a biventricular circulation with a morphologic SRV supporting the systemic circulation. Major long-term complications encountered in these patients are systemic RV dysfunction and RV failure, severe secondary systemic atrioventricular valve regurgitation (SAVVR), and arrhythmias associated with increased morbidity and mortality [41].
RV dysfunction is attributed to multifactorial mechanisms and appears after the third decade of life (Figure 1) [4, 5, 41]; (1) chronic persistent pressure overload leads to RV hypertrophy, which initially compensates for systemic afterload, but in the long term, it is associated with a potential right coronary artery supply to RV demand mismatch; (2) neonatal perioperative hypoxia and potential myocardial ischemia could influence RV function later in life; (3) SRV shortening, as assessed with TTE and MRI speckle tracking, shifts from a predominant longitudinal to a circumferential one without torsion as normally found in the systemic LV; (4) RV fibrosis identified with CMR LGE and T1 mapping techniques is highly related to SRV dysfunction and ventricular arrhythmias; (5) neurohormonal activation similar to that seen in acquired left HF is related with SRV remodeling, myocardial apoptosis, and fibrosis; (6) there is impaired atrioventricular blood flow because of rigid atrial baffles in patients with TGA and atrial switch; (7) SAVVR is usually secondary to annular dilatation or due to an abnormal tricuspid valve observed in cc-TGA; and (8) associated cardiac defects are mostly in patients with a cc-TGA, such as severe pulmonary stenosis or ventricular septal defect.
Echocardiography is the first-line diagnostic modality, providing information on size and systolic function of the SRV, the subpulmonary LV and outflow tract obstruction, severity of SAVVR, and leakage or obstruction of the atrial baffles. CMR is widely used to thoroughly assess SRV volumes and function, SRV fibrosis, and potency or leakage of atrial baffles (Figure 3). Predicting HF events in patients with a SRV and a biventricular circulation is important for timely intensification of follow-up [42]. Estimation of RV GLS, measured with STE, in combination with RVEF%, as well as RV volumes and mass, determined with CMR can well identify patients at highest risk of advanced HF or death [42, 43•].
Imaging assessment of a 38-year-old patient with a systemic right ventricle (sRV) after Mustard operation for d-transposition of the great arteries. Echocardiographic 4 chamber views in end-diastole (A) and end-systole (B) showing reduced function of the sRV as assessed by fractional area change (FAC) that is 27.8% (<35%). SRV is usually accompanied by various degrees of regurgitation of the systemic atrioventricular valve (yellow arrow), as assessed with color doppler (C). CMR has the advantage to provide high quality images of the atrial baffles in order to assess possible leakage or obstruction (D, E). LV: left ventricle, LA: left atrium, RA: right atrium
In asymptomatic patients with a severe SAVVR, quantification of progression of SRV dilatation and RV function is crucial to determine the time of surgery. Despite a preserved EF at rest, both ventricles are unable to increase stroke volume and EF in response to exercise associated with an impaired exercise capacity [44, 45].
A minority of patients with a systemic RV may present with PH as a consequence of pulmonary baffle obstruction or failing SRV. Signs of PH are often subtle including decreased flattening of the interventricular septum in systole, an abnormally wide PA, or elevated systolic pressure in the subpulmonary LV estimated from the mitral valve regurgitation in the absence of pulmonary stenosis and can be difficult to recognize [46]. Suspicion of PH dictates diagnostic heart catheterization to exclude/confirm PH as it impacts management and prognosis.
Single Right Ventricle Physiology
Patients with a hypoplastic left heart syndrome (HLHS) have a single functional RV and are palliated with the Fontan procedure in three stages. As a result, systemic venous return is passively directed to the pulmonary arteries (Figure 4). Long-term complications include thromboembolic events, arrhythmias, progressive SAVVR, RV dysfunction, HF symptoms, protein losing enteropathy, liver or renal insufficiency, and PH as a result of a chronic increase in the central venous pressure and a failing RV [47, 48]. Smaller RV size during the initial stages of palliation is related with better transplant free survival and higher likelihood of Fontan completion among children with HLHS [49]. Higher RV end-diastolic volumes are independently associated with a higher mortality risk in patients with a Fontan circulation. RV dominance has been associated with a greater increase in end-systolic volume index, a greater decrease in EF, and a higher rate of heart transplantation (HT), HT listing, or death [50]. CMR flow analysis provides accurate noninvasive hemodynamic data, including collateral flow and shunt through a fenestration if present.
Imaging assessment of a patient with hypoplastic left heart syndrome (HLHS) and a single right ventricle morphology (sRV). Echocardiographic 4-chammber (A) and parasternal short axis view (B) show a hypertrophied dilated sRV and a hypoplastic left ventricle (LV). Echocardiographic speckle tracking analysis of the sRV shows a reduced global longitudinal strain (GS=-15%) and a free wall strain (FWS=-18%). Tricuspid annular systolic excursion (TAPSE) is also reduced (C). CMR shows a patent extracardiac total cavopulmonary connection (TCPC) that directs the systemic venous blood to the pulmonary arteries (yellow arrows) (D, E). sRV volume and function as well as dimensions of the ascending aorta and aortic valve function can be also assessed (F). RA: right atrium
Treatment Options
Prevention
Timely repair of right heart defects and related lesions that impact RV size and function is essential for preventing progressive RV failure and adverse clinical outcomes in patients with CHD. Close follow-up in asymptomatic patients, using noninvasive imaging modalities and blood biomarkers, is necessary to detect early signs of RV enlargement or dysfunction and timely guide interventional procedures or surgery [51]. Impaired RV function, increased RV volumes, and the presence and extent of myocardial fibrosis have been associated with increased risk of exercise intolerance, arrhythmias, all-cause mortality, and SCD in patients with a subpulmonary RV or SRV [10, 17, 24, 33•, 40, 42, 52,53,54] (Table 1). Cardiopulmonary exercise test (CPET) can be utilized as an objective measure of exercise capacity to unmask exercise intolerance in apparently asymptomatic patients. [55, 56].
Medical Therapy
Unlike pivotal clinical trials, establishing disease-modifying drugs in acquired left-sided HF, very few inconclusive data exist on conventional HF pharmacotherapy in ACHD, derived from small cohorts [57]. Guideline recommendations, mostly based on clinical experience or position statements, support the use of conventional HF treatment in patients with a biventricular circulation and impaired systemic LV function [1]. There are no robust data to support the use of angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, beta-blockers, or aldosterone antagonists, alone or in combination, to improve outcome in patients with a failing SRV and a uni- or biventricular heart or in patients with subpulmonary RV dysfunction [58]. Recently, a few small prospective studies on the safety and efficacy of sacubitril/valsartan in patients with a systemic RV demonstrated significant improvement in NT-proBNP, ventricular function, and exercise capacity without serious adverse reactions [59, 60]. However, robust evidence regarding the use of this agent in ACHD is still lacking [61, 62]. Finally, no data exist about the use of sodium-glucose cotransporter 2 inhibitors in ACHD patients with a systemic RV. Diuretics may provide relief of symptoms if overt HF is present. Given the pre-load dependency of the Fontan patients, diuretics should be used with caution. The only evidence-based medical treatment of RV impairment in CHD is the target of PH with PAH drugs (endothelin receptor antagonists, phosphodiesterase type 2 inhibitors, prostanoid analogs, and soluble guanylate cyclase stimulators) which has been shown to improve symptoms, exercise capacity, right heart hemodynamics, RV size and function, quality of life, and survival [63, 64].
Devices and Procedures
On top of medical treatment, cardiac resynchronization therapy (CRT) may be considered in ACHD patients with HF, despite little evidence on indications and outcomes. Efficacy of CRT may vary with the underlying anatomy of the systemic ventricle (left, right, or functionally single), the presence and degree of structural SAVVR, primary myocardial disease or scarring, and type of electrical conduction delay [65]. Resynchronization of systemic RVs, subpulmonary RVs, and LVs with RBBB is challenging but can yield beneficial results. Targeted multidisciplinary pacing strategies have been shown to improve ventricular function and symptoms in selected patients [66]. In addition, ACHD patients that require a pacemaker should be considered for biventricular pacing to avoid dyssynchrony.
The benefit of ICD therapy in primary prevention for single or systemic RVs is less well established [67]. According to the latest ACHD guidelines, ICD implantation may be considered for primary prevention in patients with advanced single or systemic RV dysfunction (EF systemic RV <35%) in the presence of additional risk factors (HF symptoms, nonsustained VT, severe SAVVR, and wide QRS >140 ms) with a IIb recommendation [1]. In patients with a baffle leak who require a PM/ICD, closure of the baffle leak should be considered, when technically feasible, prior to insertion of transvenous leads. Subcutaneous ICD (S-ICD) is an alternative for patients with a complex anatomy and venous access problems (Fontan circuit) or at a high risk for infections needing ICD therapy or in patients with an ICD indication not requiring pacing for bradycardia, CRT, or antitachycardiac pacing [68•, 69].
Maintenance of sinus rhythm (SR) is a priority in patients with a systemic RV or ES, as arrhythmias are associated with symptom worsening and HF decompensation. Synchronized cardioversion should be performed in tertiary centers to restore SR. Catheter ablation is recommended as first-line therapy and preferred over long-term pharmacological treatment, in case of amenable, circumscribed substrates, as antiarrhythmic drugs are often associated with negative inotropic and/or dromotropic effects [1].
Mechanical Support and Heart Transplantation
Heart or heart-lung transplantation, although limited by donor shortage, may also be considered a therapeutic option for end-stage HF [65]. The number of ACHD recipients worldwide has increased over the decades. ACHD patients listed tend to be younger with less cardiovascular comorbidities than non-ACHD ones considered for transplantation; however, they may have multiorgan involvement that requires combined organ transplantation. Whereas early post-transplantation mortality appears increased in ACHD, long-term prognosis is better in ACHD than in other cohorts [70].
Ventricular assist devices (VAD) can bridge patients to transplantation, increasing the probability of a successful transplantation with prolongation of waiting time. In selected patients, it may be also a destination therapy. However, ACHD patients are not often considered for VAD support because of the complexity of the anatomy, paucity of VAD programs focused on ACHD, and the need for surgeons with expertise in ACHD. A systemic RV morphology is not a contraindication for a VAD, although coarse trabeculation may merit special approach, since it may block the inflow cannula; in this case, selective myomectomy should be considered [71].
Conclusions
Right heart dysfunction is highly related with adverse clinical outcomes in CHD. Thorough evaluation and management of right heart disease are a challenging task. Research should focus on early identification of patients at risk for RV dysfunction in order to timely repair the responsible lesion to prevent RV failure. To this direction, noninvasive imaging modalities with new software applications may help to early detect subtle signs of maladaptive RV remodeling. Clinical trials for the development of medications and devices that improve RV function are also warranted. Close follow-up of CHD patients in expert centers is important for the prevention and management of RHD.
Abbreviations
- ACHD:
-
Adult congenital heart disease
- ASD:
-
Atrial septal defects
- CHD:
-
Congenital heart disease
- CMR:
-
Cardiac magnetic resonance imaging
- cc-TGA:
-
Congenitally corrected transposition of the great arteries
- CRT:
-
Cardiac resynchronization therapy
- d-TGA:
-
d-Transposition of the great arteries
- ES:
-
Eisenmenger syndrome
- FAC:
-
Fractional area change
- GCS:
-
Global circumferential strain
- GDF-15:
-
Growth-differentiation factor 15
- GRS:
-
Global radial strain
- HF:
-
Heart failure
- HLHS:
-
Hypoplastic left heart syndrome
- HT:
-
Heart transplantation
- hs-TnT:
-
High-sensitive troponin-T
- ICD:
-
Implantable cardioverter defibrillator
- LGE:
-
Late gadolinium enhancement
- LV:
-
Left ventricle
- NT-proBNP:
-
N-terminal proB-type natriuretic peptide
- NYHA:
-
New York Heart Association
- PAH:
-
Pulmonary arterial hypertension
- PR:
-
Pulmonary regurgitation
- PVR:
-
Pulmonary valve replacement
- RA:
-
Right atrium
- RHC:
-
Right heart catheterization
- RV:
-
Right ventricle
- RVEF:
-
RV ejection fraction
- RVOT:
-
Right ventricular outflow tract
- RVOTO:
-
Right ventricular outflow tract obstruction
- RVSP:
-
Right Ventricular systolic pressure
- SAVVR:
-
Systemic atrioventricular valve regurgitation
- S-ICD:
-
Subcutaneous ICD
- SCD:
-
Sudden cardiac death
- STE:
-
Speckle tracking echocardiography
- SRV:
-
Systemic right ventricle
- SV:
-
Systemic ventricle
- TAPSE:
-
Tricuspid annular plane systolic excursion
- TOE:
-
Transesophageal echocardiography
- TOF:
-
Tetralogy of Fallot
- TR:
-
Tricuspid regurgitation
- TTE:
-
Transthoracic echocardiogram
- TV:
-
Tricuspid valve
- VAD:
-
Ventricular assist device
- VT:
-
Ventricular tachycardia
- VSD:
-
Ventricular septal defect
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Baumgartner H, De Backer J, Babu-Narayan SV, Budts W, Chessa M, Diller GP, et al. 2020 ESC Guidelines for the management of adult congenital heart disease. Eur Heart J. 2020;
Guihaire J, Haddad F. The right heart in congenital heart disease, mechanisms and recent advances. J Clin Exp Cardiol. 2012;8(10):1.
Ntiloudi D, Dimopoulos K, Tzifa A, Karvounis H, Giannakoulas G. Hospitalizations in adult patients with congenital heart disease: an emerging challenge. Heart Fail Rev. 2021;26(2):347–53.
Voges I, Al-Mallah MH, Scognamiglio G, Di Salvo G. Right heart-pulmonary circulation unit in congenital heart diseases. Heart Fail Clin. 2018;14(3):283–95.
Brida M, Diller G-P, Gatzoulis MA. Systemic right ventricle in adults with congenital heart disease. Circulation. 2018;137(5):508–18.
Walker RE, Moran AM, Gauvreau K, Colan SD. Evidence of adverse ventricular interdependence in patients with atrial septal defects. Am J Cardiol. 2004;93(11):1374–7.
Budts W, Miller O, Babu-Narayan SV, Li W, Valsangiacomo Buechel E, Frigiola A, et al. Imaging the adult with simple shunt lesions: position paper from the EACVI and the ESC WG on ACHD. Endorsed by AEPC (Association for European Paediatric and Congenital Cardiology). Eur Heart J Cardiovasc Imaging. 2021;22(6):e58–70.
Webb G, Gatzoulis MA. Atrial septal defects in the adult: recent progress and overview. Circulation. 2006;114(15):1645–53.
Di Salvo G, Miller O, Babu Narayan S, Li W, Budts W, Valsangiacomo Buechel ER, et al. Imaging the adult with congenital heart disease: a multimodality imaging approach—position paper from the EACVI. Eur Heart J Cardiovasc Imaging. 2018;19(10):1077–98.
Umemoto S, Sakamoto I, Abe K, Ishikita A, Yamasaki Y, Hiasa K-i, et al. Preoperative threshold for normalizing right ventricular volume after transcatheter closure of adult atrial septal defect. Circ J. 2020;84(8):1312–9.
Lammers AE, Bauer LJ, Diller GP, Helm PC, Abdul-Khaliq H, Bauer UMM, et al. Pulmonary hypertension after shunt closure in patients with simple congenital heart defects. Int J Cardiol. 2020;308:28–32.
Paranon S, Acar P. Ebstein's anomaly of the tricuspid valve: from fetus to adult: congenital heart disease. Heart. 2008;94(2):237–43.
Singh DP, Hussain K, Mahajan K. Ebstein anomaly and malformation. Treasure Island (FL): StatPearls; 2022.
Akazawa Y, Fujioka T, Yazaki K, Strbad M, Horer J, Kuhn A, et al. Right ventricular electromechanical dyssynchrony and its relation to right ventricular remodeling, dysfunction, and exercise capacity in Ebstein anomaly. J Am Soc Echocardiogr. 2023;36(6):634–43.
Brown ML, Dearani JA, Danielson GK, Cetta F, Connolly HM, Warnes CA, et al. The outcomes of operations for 539 patients with Ebstein anomaly. J Thorac Cardiovasc Surg. 2008;135(5):1120–36.
Baessato F, Furtmüller C, Shehu N, Ferrari I, Reich B, Nagdyman N, et al. Detection of early signs of right ventricular systolic impairment in unoperated Ebstein’s anomaly by cardiac magnetic resonance feature tracking. Cardiovasc Diagn Ther. 2022;12(3):278–88.
Rydman R, Shiina Y, Diller G-P, Niwa K, Li W, Uemura H, et al. Major adverse events and atrial tachycardia in Ebstein’s anomaly predicted by cardiovascular magnetic resonance. Heart. 2018;104(1):37–44.
Cohen MI, Khairy P, Zeppenfeld K, Van Hare GF, Lakkireddy DR, Triedman JK. Preventing arrhythmic death in patients with tetralogy of Fallot. J Am Coll Cardiol. 2021;77(6):761–71.
Samad MD, Wehner GJ, Arbabshirani MR, Jing L, Powell AJ, Geva T, et al. Predicting deterioration of ventricular function in patients with repaired tetralogy of Fallot using machine learning. Eur Heart J Cardiovasc Imaging. 2018;19(7):730–8.
Villafañe J, Feinstein JA, Jenkins KJ, Vincent RN, Walsh EP, Dubin AM, et al. Hot topics in tetralogy of Fallot. J Am Coll Cardiol. 2013;62(23):2155–66.
Davlouros PA, Kilner PJ, Hornung TS, Li W, Francis JM, Moon JC, et al. Right ventricular function in adults with repaired tetralogy of Fallot assessed with cardiovascular magnetic resonance imaging: detrimental role of right ventricular outflow aneurysms or akinesia and adverse right-to-left ventricular interaction. J Am Coll Cardiol. 2002;40(11):2044–52.
Freling HG, Willems TP, van Melle JP, van Slooten YJ, Bartelds B, Berger RM, et al. Effect of right ventricular outflow tract obstruction on right ventricular volumes and exercise capacity in patients with repaired tetralogy of fallot. Am J Cardiol. 2014;113(4):719–23.
Gao Y, Li H, He L, Zhang Y, Sun W, Li M, et al. Superior prognostic value of right ventricular free wall compared to global longitudinal strain in patients with repaired tetralogy of Fallot. Front Cardiovasc Med. 2022;9:996398.
Arroyo-Rodríguez C, Fritche-Salazar JF, Posada-Martínez EL, Arías-Godínez JA, Ortiz-León XA, Calvillo-Arguelles O, et al. Right ventricular free wall strain predicts functional capacity in patients with repaired tetralogy of Fallot. Int J Cardiovasc Imaging. 2020;36(4):595–604.
Friedberg MK, Fernandes FP, Roche SL, Grosse-Wortmann L, Manlhiot C, Fackoury C, et al. Impaired right and left ventricular diastolic myocardial mechanics and filling in asymptomatic children and adolescents after repair of tetralogy of Fallot. Eur Heart J Cardiovasc Imaging. 2012;13(11):905–13.
Mongeon FP, Ben Ali W, Khairy P, Bouhout I, Therrien J, Wald RM, et al. Pulmonary valve replacement for pulmonary regurgitation in adults with tetralogy of Fallot: a meta-analysis-a report for the Writing Committee of the 2019 Update of the Canadian Cardiovascular Society Guidelines for the Management of Adults With Congenital Heart Disease. Can J Cardiol. 2019;35(12):1772–83.
Panaioli E, Birritella L, Graziani F, Lillo R, Grandinetti M, Di Molfetta A, et al. Right ventricle-pulmonary artery coupling in repaired tetralogy of Fallot with pulmonary regurgitation: Clinical implications. Arch Cardiovasc Dis. 2022;115(2):67–77.
Frigiola A, Redington AN, Cullen S, Vogel M. Pulmonary regurgitation is an important determinant of right ventricular contractile dysfunction in patients with surgically repaired tetralogy of Fallot. Circulation. 2004;110(11)
Steinmetz M, Stümpfig T, Seehase M, Schuster A, Kowallick J, Müller M, et al. Impaired exercise tolerance in repaired tetralogy of Fallot is associated with impaired biventricular contractile reserve: an exercise-stress real-time cardiovascular magnetic resonance study. Circulation. Cardiovasc Imaging. 2021;14(8):e011823.
Bonello B, Kempny A, Uebing A, Li W, Kilner PJ, Diller GP, et al. Right atrial area and right ventricular outflow tract akinetic length predict sustained tachyarrhythmia in repaired tetralogy of Fallot. Int J Cardiol. 2013;168(4):3280–6.
Ghonim S, Voges I, Gatehouse PD, Keegan J, Gatzoulis MA, Kilner PJ, et al. Myocardial architecture, mechanics, and fibrosis in congenital heart disease. Front Cardiovasc Med. 2017;4:30.
Babu-Narayan SV, Kilner PJ, Li W, Moon JC, Goktekin O, Davlouros PA, et al. Ventricular fibrosis suggested by cardiovascular magnetic resonance in adults with repaired tetralogy of fallot and its relationship to adverse markers of clinical outcome. Circulation. 2006;113(3):405–13.
Ghonim S, Gatzoulis MA, Ernst S, Li W, Moon JC, Smith GC, et al. Predicting survival in repaired tetralogy of Fallot. JACC Cardiovasc Imaging. 2022;15(2):257–68. This is a novel risk stratification score in patients with tetralogy of Fallot based on non-invasive data.
Chen CA, Dusenbery SM, Valente AM, Powell AJ, Geva T. Myocardial ECV fraction assessed by CMR is associated with type of hemodynamic load and arrhythmia in repaired tetralogy of Fallot. JACC Cardiovasc Imaging. 2016;9(1):1–10.
Arvanitaki A, Gatzoulis MA, Opotowsky AR, Khairy P, Dimopoulos K, Diller GP, et al. Eisenmenger syndrome: JACC state-of-the-art review. J Am Coll Cardiol. 2022;79(12):1183–98.
Arvanitaki A, Giannakoulas G, Baumgartner H, Lammers AE. Eisenmenger syndrome: diagnosis, prognosis and clinical management. Heart. 2020;106(21):1638–45.
Dimopoulos K, Giannakoulas G, Wort SJ, Gatzoulis MA. Pulmonary arterial hypertension in adults with congenital heart disease: distinct differences from other causes of pulmonary arterial hypertension and management implications. Curr Opin Cardiol. 2008;23(6):545–54.
Diller GP, Korten MA, Bauer UM, Miera O, Tutarel O, Kaemmerer H, et al. Current therapy and outcome of Eisenmenger syndrome: data of the German National Register for congenital heart defects. Eur Heart J. 2016;37(18):1449–55.
Moceri P, Dimopoulos K, Liodakis E, Germanakis I, Kempny A, Diller GP, et al. Echocardiographic predictors of outcome in Eisenmenger syndrome. Circulation. 2012;126(12):1461–8.
Moceri P, Iriart X, Bouvier P, Baudouy D, Gibelin P, Saady R, et al. Speckle-tracking imaging in patients with Eisenmenger syndrome. Arch Cardiovasc Dis. 2016;109(2):104–12.
Lluri G, Aboulhosn J. The systemic right ventricle in adult congenital heart disease: why is it still such a challenge and is there any hope on the horizon? Curr Opin Cardiol. 2022;37(1):123–9.
Lewis MJ, Van Dissel A, Kochav J, DiLorenzo MP, Ginns J, Zemer-Wassercug N, et al. Cardiac MRI predictors of adverse outcomes in adults with a systemic right ventricle. ESC Heart Failure. 2022;9(2):834–41.
Woudstra OI, van Dissel AC, van der Bom T, de Bruin-Bon RHACM, van Melle JP, van Dijk APJ, et al. Myocardial deformation in the systemic right ventricle: strain imaging improves prediction of the failing heart. Can J Cardiol. 2020;36(9):1525–33. This article shows the significance of strain imaging in predicting systemic right ventricular failure.
Roest AA, Lamb HJ, van der Wall EE, Vliegen HW, van den Aardweg JG, Kunz P, et al. Cardiovascular response to physical exercise in adult patients after atrial correction for transposition of the great arteries assessed with magnetic resonance imaging. Heart. 2004;90(6):678–84.
Tay EL, Frogoudaki A, Inuzuka R, Giannakoulas G, Prapa M, Li W, et al. Exercise intolerance in patients with congenitally corrected transposition of the great arteries relates to right ventricular filling pressures. Int J Cardiol. 2011;147(2):219–23.
Dimopoulos K, Condliffe R, Tulloh RMR, Clift P, Alonso-Gonzalez R, Bedair R, et al. Echocardiographic screening for pulmonary hypertension in congenital heart disease: JACC review topic of the week. J Am Coll Cardiol. 2018;72(22):2778–88.
Alsaied T, Bokma JP, Engel ME, Kuijpers JM, Hanke SP, Zuhlke L, et al. Predicting long-term mortality after Fontan procedures: a risk score based on 6707 patients from 28 studies. Congenit Heart Dis. 2017;12(4):393–8.
Pundi KN, Johnson JN, Dearani JA, Pundi KN, Li Z, Hinck CA, et al. 40-year follow-up after the Fontan operation: long-term outcomes of 1,052 patients. J Am Coll Cardiol. 2015;66(15):1700.
Kim AS, Witzenburg CM, Conaway M, Vergales JE, Holmes JW, L’Ecuyer TJ, et al. Trajectory of right ventricular indices is an early predictor of outcomes in hypoplastic left heart syndrome. Congenit Heart Dis. 2019;14(6):1185–92.
Ghelani SJ, Lu M, Sleeper LA, Prakash A, Castellanos DA, Clair NS, et al. Longitudinal changes in ventricular size and function are associated with death and transplantation late after the Fontan operation. J Cardiovasc Magn Reson. 2022;24(1):1–8.
Boutsikou M, Tzifa A. Noninvasive imaging prior to percutaneous pulmonary valve implantation. Hellenic J Cardiol. 2022;67:59–65.
Timoteo AT, Branco LM, Rosa SA, Ramos R, Agapito AF, Sousa L, et al. Usefulness of right ventricular and right atrial two-dimensional speckle tracking strain to predict late arrhythmic events in adult patients with repaired Tetralogy of Fallot. Rev Port Cardiol. 2017;36(1):21–9.
Arvanitaki A, Ntiloudi D, Giannakoulas G, Dimopoulos K. Prediction models and scores in adult congenital heart disease. Curr Pharm Des. 2021;27(10):1232–44.
Jensen AS, Broberg CS, Rydman R, Diller G-P, Li W, Dimopoulos K, et al. Impaired Right, Left, or Biventricular function and resting oxygen saturation are associated with mortality in Eisenmenger syndrome. Circ Cardiovasc Imaging. 2015;8(12):e003596.
Kempny A, Dimopoulos K, Uebing A, Moceri P, Swan L, Gatzoulis MA, et al. Reference values for exercise limitations among adults with congenital heart disease. Relation to activities of daily life--single centre experience and review of published data. Eur Heart J. 2011;33(11):1386–96.
Diller GP, Giardini A, Dimopoulos K, Gargiulo G, Muller J, Derrick G, et al. Predictors of morbidity and mortality in contemporary Fontan patients: results from a multicenter study including cardiopulmonary exercise testing in 321 patients. Eur Heart J. 2010;31(24):3073–83.
Ntiloudi D, Gatzoulis MA, Arvanitaki A, Karvounis H, Giannakoulas G. Adult congenital heart disease: looking back, moving forward. Int J Cardiol Congenit Heart Dis. 2021;2:100076.
Zaragoza-Macias E, Zaidi AN, Dendukuri N, Marelli A. Medical therapy for systemic right ventricles: a systematic review (part 1) for the 2018 AHA/ACC Guideline for the Management of Adults with Congenital Heart Disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139(14):e801–13.
Zandstra TE, Nederend M, Jongbloed MRM, Kiès P, Vliegen HW, Bouma BJ, et al. Sacubitril/valsartan in the treatment of systemic right ventricular failure. Heart. 2021;107(21):1725–30.
Fusco F, Scognamiglio G, Merola A, Iannuzzi A, Palma M, Grimaldi N, et al. Safety and efficacy of sacubitril/valsartan in patients with a failing systemic right ventricle: a prospective single-center study. Circ Heart Fail. 2022;16(2):e009848.
Kosmidis D, Arvanitaki A, Giannakoulas G. Is there a role for renin–angiotensin–aldosterone system and neprilysin inhibition in the failing systemic right ventricle? Int J Cardiol Congenit Heart Dis. 2021;3:100119.
Appadurai V, Nicolae M, Aboulhosn J, Lluri G. The protocol and rationale for the efficacy and tolerability of sacubitril-valsartan in adult congenital heart disease patients with heart failure (ENTRUST ACHD HF) registry. Int J Cardiol Congenit Heart Dis. 2021;3:100096.
Humbert M, Kovacs G, Hoeper MM, Badagliacca R, Berger RMF, Brida M, et al. 2022 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Heart J. 2022;43(38):3618–731.
Arvanitaki A, Diller GP. The use of pulmonary arterial hypertension therapies in Eisenmenger syndrome. Expert Rev Cardiovasc Ther. 2021;27:1–9.
Sinning C, Huntgeburth M, Fukushima N, Tompkins R, Huh J, Tataneo S, et al. Treatment of advanced heart failure in adults with congenital heart disease: a narrative review and clinical cases. Cardiovasc Diagn Ther. 2022;12(5):727–43.
Kharbanda RK, Moore JP, Taverne YJHJ, Bramer WM, Bogers AJJC, de Groot NMS. Cardiac resynchronization therapy for the failing systemic right ventricle: a systematic review. Int J Cardiol. 2020;318:74–81.
Dellborg M, Eriksson P, Mandalenakis Z. ICD implantation for primary prevention in adult patients with a systemic right ventricle – the case in favor of implanting. Int J Cardiol Congenit Heart Dis. 2021;3:100129.
Diller GP, Arvanitaki A, Opotowsky AR, Jenkins K, Moons P, Kempny A, et al. Lifespan perspective on congenital heart disease research: JACC state-of-the-art review. J Am Coll Cardiol. 2021;77(17):2219–35. An extensive review directed to research oportunities in congenital heart disease that could improve every day clinical practice.
Khairy P. Ventricular arrhythmias and sudden cardiac death in adults with congenital heart disease. Heart. 2016;102(21):1703–9.
Engelings CC, Helm PC, Abdul-Khaliq H, Asfour B, Bauer UM, Baumgartner H, et al. Cause of death in adults with congenital heart disease-an analysis of the German National Register for Congenital Heart Defects. Int J Cardiol. 2016;211:31–6.
Villa CR, Lorts A, Kasten J, Chin C, Alsaied T, Tiao G, et al. Bridge to heart-liver transplantation with a ventricular assist device in the Fontan circulation. Circ Heart Fail. 2021;14(12):e008018.
Funding
AA was the recipient of the International Training and Research Fellowship EMAH Stiftung Karla Voellm, Krefeld, Germany, between 2020 and 2022.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Alexandra Arvanitaki declares no conflict of interest. Gerhard Diller declares no conflict of interest. George Giannakoulas declares lecture/consultant fees from Bayer HealthCare, Janssen, Ferrer, MSD, GSK, Elpen Pharmaceuticals, and Pfizer.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Arvanitaki, ., Diller, G. & Giannakoulas, G. The Right Heart in Congenital Heart Disease. Curr Heart Fail Rep 20, 471–483 (2023). https://doi.org/10.1007/s11897-023-00629-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11897-023-00629-7