Abstract
Purpose of Review
To review the role of cardiac troponin (cTn) for prognosis in acute and chronic heart failure, and for predicting heart failure; and to explore the association between troponin and response to heart failure therapies, with an eye toward a possible role for troponin in a personalized approach to heart failure management, beyond prognosis.
Recent Findings
A number of therapies, including the neprilysin inhibitor sacubitril/valsartan and sodium-glucose cotransporter-2 inhibitors, have recently been shown to improve outcomes in heart failure patients. Most studies suggest that these agents improve outcomes regardless of baseline cTn concentration, but have greater absolute benefit among patients with highest cTn and baseline risk.
Summary
Troponin is prognostic across the heart failure spectrum, but whether it can significantly help with heart failure prevention and with tailoring and guiding heart failure treatments and interventions remains unknown.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It is not surprising that cardiac troponin is prognostic in heart failure, since troponin is prognostic across a wide spectrum of clinical scenarios. This is true even though elevated cardiac troponin does not always reflect an acute thrombotic cardiovascular event.
With the highly sensitive assays available today, measurable concentrations of circulating cardiac troponin are now the norm in most individuals. This is especially true in heart failure patients, in whom troponin levels tend to be elevated compared to the general population. Multiple studies have consistently shown that among patients with both heart failure with reduced ejection fraction (HFrEF) and heart failure with preserved ejection fraction (HFpEF), and in both acute and chronic heart failure settings, higher concentrations of troponin are associated with a variety of worse outcomes [1, 2, 3, 4].
Whether there is a role for troponin in heart failure beyond prognostication is more uncertain. In the previous iteration of the ACC/AHA Guidelines for the Management of Heart Failure from 2013, cardiac troponin carried a Class IA recommendation for “Additive Risk Stratification” of both acute and ambulatory heart failure, with a recommendation that the measurement of troponin should be routine in patients presenting with acutely decompensated heart failure syndromes [5]. However, the most recent 2022 AHA/ACC Guidelines no longer formally recognize the role of “markers of myocardial injury,” instead noting that while they provide incremental prognostic information, they currently lack sufficient evidence of an incremental management benefit over natriuretic peptides [6•]. Despite this backpedal, there may yet be an important role for cardiac troponins in the future of heart failure management.
The higher concentrations of detectable cardiac troponin in heart failure patients can lead to confusion and clouding of the diagnosis of myocardial infarction; but they may also present an opportunity. Troponin concentrations may serve as a tool to help guide titration of emerging therapies, if serial values track with response to treatment and outcomes. In addition, an aspirational goal for the future of personalized medicine is to use biomarkers, including perhaps troponin, to help tailor therapies and interventions to selected patients who are most likely to benefit from them.
Here, we will briefly review the prognostic value of troponin in acute and chronic heart failure, as well as the value for predicting new heart failure both in patients with coronary artery disease and in the general population. Then, we explore how baseline troponin concentrations may predict a patient’s response to emerging and established heart failure therapies, and conversely, how such therapies affect serial troponin values and the implications this has for individualized selection and titration of therapies.
Troponin in Chronic Heart Failure
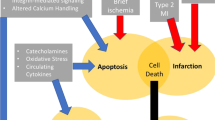
In patients with chronic heart failure, the association between elevated cardiac troponin and worse outcomes is well established and is thought to be primarily due to ongoing myocardial injury via various mechanisms. The leading cause is thought to be supply–demand mismatch, and is likely multifactorial with contribution from transmural pressures, microvascular disease, and endothelial dysfunction [7]. Latini et al. first presented this evidence in 2007 from Val-HeFT (Valsartan in Heart Failure Trial) [1]. Elevated cardiac troponin T (cTnT) was significantly associated with increased risk of death (adjusted hazard ratio [HR] 2.08 [95% confidence interval [CI]1.72–2.52]) and hospitalization (HR 1.55 [1.25–1.93]) as compared to undetectable troponin [1]. Later, a cohort analysis from CORONA (Controlled Rosuvastatin Multinational Trial in Heart Failure) revealed that in chronic heart failure patients with highly sensitive (hs)-cTnT concentrations over 14 ng/L, there was an increased risk of stroke, myocardial infarction (MI), and cardiovascular death (composite HR 1.89 [1.38–2.59]) [3]. Later investigators worked to delineate cut-offs to better establish this risk. For example, Aimo et al. studied 9289 patients with chronic heart failure in a meta-analysis of individual patient data from 10 cohort studies, and found that an hs-cTnT cut-off of 18 ng/L predicted higher rates of all-cause death (HR 2.28 [2.03–2.57]), cardiovascular death (HR 2.21 [1.92–2.54]), and cardiovascular hospitalization (HR 2.33 [2.07–2.63]) over 29 months [2]. These associations remained consistent even when adjusted for age, sex, etiology of heart failure (ischemic vs non-ischemic), left ventricular ejection fraction, kidney function, and natriuretic peptide level.
Troponin in Acute Heart Failure
Patient with acute heart failure exacerbations frequently present with troponin elevations. Many times, this is due to a type I acute MI which triggered the acute heart failure. However, even in the absence of an acute thrombotic event, mild troponin elevation in acute heart failure is common. Although many mechanisms have been posited, supply–demand mismatch is often implicated and can be due to subendocardial ischemia and/or increased transmural pressure, among other causes [7]. Even in the absence of a type I MI, troponin levels in the acute heart failure setting are predictive of outcomes. This was shown in an analysis of 67,924 patients from the ADHERE (Acute Decompensated Heart Failure National Registry) registry. Among patients admitted with a heart failure exacerbation, an elevated troponin (cTnI ≥ 1 mcg/L or cTnT ≥ 0.1 mcg/L) was associated with a significantly increased risk of in-hospital mortality (8.0% vs 2.7%) [8]. Over the years, many studies have further cemented this association between elevated troponin and adverse outcomes [4].
Troponin and the Risk of New-Onset Heart Failure in Patients with Stable Cardiovascular Disease
In patients with chronic, stable coronary artery disease (CAD), troponin concentrations can be useful as a prognostic tool to help assess the risk of developing heart failure, as was shown in an analysis of 3679 subjects with stable CAD and preserved left ventricular function from the biomarker substudy of the PEACE (Prevention of Events with Angiotensin Converting Enzyme Inhibition) Trial. Individuals with higher cTnT had increased risk of cardiovascular death (HR 2.78 [2.24–3.45] per unit increase in the natural log of cTn) and of heart failure (HR 2.77 [2.12–3.60]) after a median follow-up of 5.2 years. Of note, there was no significant association between cTnT and incident MI [9]. Similar associations were seen when the analyses were repeated years later with hs-cTnT and hs-cTnI [10].
Cardiac troponin fared well for prognostication in stable cardiovascular disease (CVD) patients when compared to various risk scores. One retrospective study compared risk stratification by troponins to risk scores such as PROCAM (Prospective Cardiovascular Münster) and Framingham [11]. Approximately 700 patients with a history of CAD, peripheral arterial disease, or transient ischemic attack/stroke who were followed for about 2 years found that hs-cTnT outperformed both the PROCAM and three Framingham subscores for predicting future cardiac events, with an area under the receiver-operator characteristic curve (AUC) of 0.661–0.836, which was significantly better than the risk scores (0.512–0.614) [11].
Troponin and New-Onset Heart Failure in the General Population
When a patient presents acutely with chest pain or anginal equivalent and develops an elevated cardiac troponin, ischemic heart disease is often the culprit. However, in the setting of an asymptomatic individual with a chronically elevated troponin, the implication is very different. A common theme in studies of the general population is that higher levels of cardiac troponin are more strongly associated with future risk of heart failure than with risk of ischemic heart disease (i.e., MI and/or need for coronary revascularization). Chronic elevations in cTn in the general population are associated with higher left ventricular mass and worse kidney function, as well as advanced age, all factors that relate to future heart failure risk [12].
A prospective cohort study of 4221 individuals over 65 years of age with no history of heart failure obtained cTnT levels at baseline and again at 2–3 years. After a median of 11.8 years of follow-up, subjects in the highest quintile of baseline troponin had an adjusted 2.5 × higher risk of new-onset heart failure compared to those in the lowest quintile (6.4 vs 1.6 per 100 person-years). Similarly, among individuals whose troponin increased by at least 50% over 2–3 years, there was a greater risk of new-onset heart failure (HR 1.61 [1.32–1.97]), while those who had a decrease of at least 50% had a lower risk (HR 0.73 [0.54–0.97]) compared to those whose troponin was more stable over time [13].
New-onset heart failure was also studied in 6814 subjects from the Multi-Ethnic Study of Atherosclerosis (MESA), ages 45–84 years, who had no known CVD at baseline. In this study, after approximately 12 years of follow-up, there was an increased risk of incident heart failure among participants with hs-cTnT in the highest quintile (≥ 8.81 ng/L) compared to those with undetectable hs-cTnT (HR 5.6 [3.0–10.7]). Furthermore, the study evaluated the association between baseline hs-cTnT and the presence of replacement fibrosis using late gadolinium enhancement [LGE] on cardiac magnetic resonance imaging [cMRI] 10 years later. Subjects with hs-cTnT in the highest quintile (≥ 7.42 ng/L) had a 2.4 × (1.2‒5.1) increased odds of LGE compared to those with undetectable troponin [14]. These findings suggest that hs-cTnT may represent a biomarker surrogate for early myocardial fibrosis.
Other studies have also aimed to explain the association between cTn and incident heart failure. One such study evaluated echocardiographic measures of left ventricular systolic and diastolic function among 4111 individuals without CVD from the ARIC (Atherosclerosis Risk in Communities) study [15]. The aim was to define the association between elevated cTnT and left ventricular dysfunction, and then quantify how much this association accounted for the risk that elevated troponins confers toward development of new-onset heart failure over approximately 4.5 years of follow-up. Patients with higher cTnT levels had greater left ventricular mass and worse diastolic function but not systolic function. Adjusting for this diastolic dysfunction reduced the association between elevated troponins and incident HFpEF by 41%, and incident HFrEF or heart failure with midrange ejection fraction (HFmrEF) by 17%. The authors concluded that elevated cTnT may serve as a marker for subclinical diastolic dysfunction, which in turn may predispose to incident heart failure.
Selecting Patients for Therapies and Tracking Treatment Response with Troponin
At this point, it has been well established that elevated cTn concentrations are associated with worse outcomes across the spectrum of heart failure. Evidence is also accumulating to reveal how established and emerging heart failure therapies alter troponin concentrations, and whether these changes correspond with meaningful differences in outcomes (Table 1). In addition, in some cases, baseline troponin concentrations may serve as a guide to selecting the patients most likely to benefit from a given therapy. In this era of multiple pathways for initiating and optimizing guideline directed medical therapy (GDMT), a readily available tool to help personalize therapy would be a welcome addition.
Below, we highlight the interplay between troponin and the more recent classes of GDMT medications, including the neprilysin inhibitor sacubitril/valsartan and sodium-glucose cotransporter-2 (SGLT2) inhibitors; as well as spironolactone.
Sacubitril/Valsartan in HFrEF
In the PARADIGM-HF (Prospective Comparison of ARNI with ACEI to Determine Impact on Global Mortality and Morbidity in Heart Failure) trial, 8399 patients with HFrEF were randomized to either sacubitril/valsartan or enalapril [16]. Subjects randomized to sacubitril/valsartan had lower rates of heart failure–related Emergency Department visits (HR 0.66 [0.52–0.85]) and of intensification of medical treatment for heart failure (HR 0.84 [0.74–0.94]) as well as 23% fewer hospitalizations, and an 18% lower need for intensive care. Within 4 weeks, there was a statistically significant, albeit small, reduction in hs-cTnT levels for patients in the sacubitril/valsartan group compared to the enalapril group, which was sustained at 8 months, suggesting less ongoing myocardial injury and possibly less wall stress.
The associations between sacubitril/valsartan and hs-cTnT trends were also analyzed in an exploratory analysis from the open-label, single-arm prospective study of 715 HFrEF patients followed for a year in PROVE-HF (Prospective Study of Biomarkers, Symptom Improvement and Ventricular Remodeling During Entresto Therapy for Heart Failure) [17•]. Within 1 month of initiating treatment, circulating hs-cTnT had already significantly decreased and remained lower over the course of the study. Over the full year, the average change in hs-cTnT was − 6.7%, and the magnitude of this change correlated with improvements in both baseline left ventricular ejection fraction and atrial volume index measurements. Notably, these same patterns were also found with N-terminal pro B-type natriuretic peptide (NT-proBNP), and the changes in hs-cTnT correlated with changes in NT-proBNP across all time points measured.
Neprilysin Inhibitors in HFpEF
Jhund et al. studied the trajectory of hs-cTnT in 298 patients with HFpEF from the Prospective Comparison of ARNI with ARB on Management of Heart Failure with Preserved Ejection Fraction (PARAMOUNT) trial [18]. Patients were assigned to either sacubitril/valsartan or valsartan alone and were followed for a period of 36 weeks. Although hs-cTnT levels decreased in both arms, the reduction was greater in the sacubitril/valsartan arm, measuring 12% at 12 weeks and 14% at 36 weeks. These findings again suggest less ongoing myocardial injury among patients randomized to sacubitril/valsartan.
The association between hs-cTnT and sacubitril/valsartan (compared to valsartan alone) was also evaluated within the Prospective Comparison of ARNI with ARB Global Outcomes in HF with Preserved Ejection Fraction (PARAGON-HF) trial [19•]. In this study of 1260 subjects with HFpEF, higher baseline hs-cTnT and hs-cTnT that increased over time were both independently associated with the composite outcome of cardiovascular death or heart failure hospitalization over a median 34-month follow-up. Furthermore, the subset of patients with hs-cTnT above the median at baseline appeared to derive the most benefit from sacubitril/valsartan therapy. Because patients with active ischemic heart disease were excluded from the PARAGON-HF trial, the authors speculated that this subgroup of HFpEF patients with higher baseline hs-cTnT may represent a group with ongoing myocardial injury, higher ventricular wall stress, or impaired microcirculation. They also found that hs-cTnT levels tracked with treatment arm: by 16 weeks, patients randomized to sacubitril/valsartan had hs-cTnT concentrations that were a significant 9% lower than those randomized to valsartan alone. Importantly, this reduction in hs-cTnT also tracked with improved outcomes. At 16 weeks, subjects with a decrease in their hs-cTnT to at or below the median of 17 ng/L had a lower risk of the composite outcome compared to those with persistently elevated concentrations. How sacubitril/valsartan leads to hs-cTnT reductions is speculative, but may be via neurohormonal modulation, reduced wall stress, and perhaps anti-fibrotic effects.
Sodium-Glucose Cotransporter-2 (SGLT2) Inhibitors in HFrEF
SGLT2 inhibitors, first introduced as treatments for diabetes but found to have important cardiometabolic benefits, are the latest class of medications shown to improve outcomes in heart failure and to become incorporated into the heart failure guidelines [6•]. The effect of the SGLT2 inhibitor dapagliflozin on hs-cTnT was evaluated among 2506 HFrEF patients from the Dapagliflozin and Prevention of Adverse Outcomes in Heart Failure (DAPA-HF) trial who were randomized to dapagliflozin or placebo and had measurements at both baseline and 1 year, with a median 18-month follow-up [20•]. The primary endpoint was a composite of worsening heart failure or cardiovascular death. Similar to patterns seen with sacubitril/valsartan, there was an increased risk of this primary endpoint with each increasing quartile of baseline troponin, as well as with larger serial increases in troponin levels. In contrast to findings with sacubitril/valsartan, dapagliflozin treatment was not associated with a downward trend in hs-TnT. Instead, hs-TnT had a general upward trend over the course of the year among all patients, though there was a small and non-significant 3% attenuation of this rise among patients randomized to the dapagliflozin arm. Dapagliflozin reduced the risk of the primary endpoint consistently, across all baseline troponin levels.
These findings are consistent with a prespecified biomarker substudy of DECLARE-TIMI 58 (Dapagliflozin Effect on Cardiovascular Events–Thrombolysis in Myocardial Infarction 58), in which diabetic patients were randomized to dapagliflozin or placebo and followed with serial cardiac biomarkers [21]. While only 10% of subjects in this trial had heart failure, all 14,565 had type 2 diabetes mellitus and either multiple risk factors or established atherosclerotic CVD. Each had baseline hs-cTnT measured and was followed over a median of 4 years for a composite end point of cardiovascular death or hospitalization for heart failure. Dapagliflozin consistently reduced the relative risk of the composite endpoint across all troponin quartiles (P-interaction non-significant), though the absolute risk reduction was higher for patients with baseline hs-cTnT above the median (1.8% vs 0.1%, P-interaction 0.03), due to their higher overall risk.
Another SGLT2 inhibitor, empagliflozin, was studied in EMPEROR-Reduced (Empagliflozin Outcome Trial in Patients with Chronic Heart Failure and a Reduced Ejection Fraction) and revealed similar patterns [22•]. In this, 3636 patients with HFrEF were randomized to placebo or empagliflozin and followed for a median of 16 months. When patients were stratified based upon baseline hs-cTnT, the combined risk of cardiovascular death and heart failure hospitalization increased with each higher quartile of hs-cTnT. However, benefits of empagliflozin for reducing events did not vary based upon baseline hs-cTnT; patients derived benefit within each quartile. There was a nominally significant greater effect of empagliflozin on the relative risk reduction of the primary endpoint among patients with lower levels of hs-cTnT; however, there was no difference in absolute risk reduction.
SGLT2 Inhibitors in HFpEF
The interplay between cardiac troponin and SGLT2 inhibitors has also been studied in the setting of HFpEF, and the pattern again was similar. A substudy from EMPEROR-Preserved (Empagliflozin Outcome Trial in Patients with Chronic Heart Failure with Preserved Ejection Fraction) evaluated hs-cTnT levels and outcomes in 5986 subjects who were randomized to empagliflozin versus placebo [23•]. There was a higher rate of cardiovascular death and heart failure hospitalizations among patients with baseline hs-cTnT in higher quartiles. In this study, empagliflozin reduced events evenly across all troponin quartiles, with comparable relative risk reductions, though the absolute risk reduction was highest for those patients with the highest baseline hs-cTnT (and risk). Troponin levels were not followed serially.
Spironolactone
In TOPCAT (the Treatment of Preserved Cardiac Function Heart Failure with an Aldosterone Antagonist Trial), there was a possible (albeit not statistically significant) reduction in heart failure hospitalizations for patients with HFpEF who were randomized to spironolactone vs placebo. Regional differences in baseline characteristics, study drug adherence, and outcomes were noted, and those enrolled in the Americas subregion derived significant benefit from spironolactone [24, 25]. Of the original 1767 patients in the study who were enrolled in this Americas subregion, 236 had baseline measurements of hs-cTnI, and 80% (n = 188) of those patients had subsequent paired troponin samples at 12 months. Once again, higher concentrations of baseline troponin were independently associated with increased risk of cardiovascular death and heart failure hospitalizations (HR for highest vs lowest quartile 4.85 [1.99–11.83], p = 0.001). However, the treatment effect of spironolactone did not vary by baseline troponin level (p = 0.94 for interaction) [24]. In a follow-up analysis, the TOPCAT investigators evaluated hs-cTnI along with other biomarkers, aiming to better characterize the underlying mechanism by which spironolactone benefits patients with HFpEF. This study included 204 of the original 1767 patients from the Americas subregion of TOPCAT, who had paired samples at baseline and at 12 months for various biomarkers in addition to hs-cTnI including BNP (B-type natriuretic peptide), NT-proBNP (N-terminal-pro-B-type natriuretic peptide), hs-CRP, uric acid, and urine protein-creatinine ratio. For troponin specifically, hs-cTnI levels increased over 12 months in the placebo group, while those randomized to spironolactone had no statistically significant change during that time [25]. Still, perhaps due to small sample size, spironolactone did not significantly affect the trend in hs-cTnI; furthermore, the 2018 study had found that change in troponin level was not significantly associated with the primary outcome [24]. In contrast, natriuretic peptides showed a significant reduction over time among patients randomized to spironolactone compared to placebo, suggesting that any clinical benefits observed in TOPCAT Americas may have been mediated by reduction in cardiac wall stress and/or filling pressures. However, given the small sample size, the TOPCAT biomarker substudy may have been underpowered to show some differences.
Summary and Future Directions
The prognostic value of cardiac troponin concentrations in patients with both acute and chronic heart failure is clear. In each scenario, elevated levels of troponin are associated with adverse events including death and worsening heart failure. Furthermore, in the case of patients with no history of heart failure, elevated levels of troponin are associated with incident heart failure.
A role for troponin in heart failure beyond prognostication, though, will depend upon how the evidence plays out in several key areas.
Predicting (and Preventing) Future Heart Failure
As discussed above, elevated troponin concentrations in the general population are associated with an increased risk for development of new-onset heart failure years later. Imaging studies have suggested that these early biochemical signals may correlate with subclinical myocardial fibrosis and early diastolic filling abnormalities. As such, hs-cTn may serve as a screening tool to help inform risk of heart failure. Partly in acknowledgement of this, the 2022 AHA/ACC Heart Failure Guidelines now recognize a role for troponin helping to differentiate Stage B (Pre-Heart Failure, with troponin persistently elevated) from Stage A (At Risk For Heart Failure, without cardiac biomarkers of injury) [6•].
Taking this a step further, the randomized STOP-HF trial (St Vincent’s Screening to Prevent Heart Failure), which evaluated a natriuretic peptide–based screening strategy to identify and intervene upon patients at risk for heart failure, found that the screening and subsequent early interventions reduced the composite endpoint of incident left ventricular dysfunction with or without new heart failure [26]. This suggests that with the proper interventions, and with the appropriate population targeted, mitigating the risk of heart failure is possible. This has yet to be confirmed on a large scale or integrated clinically, and much work to establish proper cutpoints, interventions, and target populations is still needed. Although this study involved screening with natriuretic peptides, one could envision a similar pathway forward for troponin.
Targeting and Guiding Therapy
Although troponin no longer receives a Class I indication in the AHA/ACC Heart Failure Guidelines for prognosis in heart failure, the book has been left open. Future investigation of “high-value methods to use biomarkers in the optimization of medical therapy” and of the “ability to use integrated systems biology models, including biomarkers… for diagnosis, prognosis, and targeting therapies” is specifically called out as a Future Direction [6•].
As reviewed above and outlined in the table, the bulk of evidence suggests that patients at higher baseline risk derive greater absolute benefit from therapy. Biomarkers including troponin can play an important role in identifying those high-risk patients. For some medical interventions, there may be a threshold within the disease progression at which the benefits of treatment begin to outweigh the costs and risks more meaningfully, and perhaps troponin and other markers can help to identify this “tipping point.” And although the medications reviewed here all tended to show the most absolute benefit within the highest risk patient subgroups, that is not always the case for interventions in heart failure. For example, the benefits of rosuvastatin among patients with ischemic heart failure may be most pronounced in lower risk patients [27]; irbesartan appeared to be most beneficial among HFpEF patients with lower natriuretic peptide concentrations [28]; and exercise training may be most beneficial among HFrEF patients with lower concentrations of biomarkers of cardiovascular risk [29].
Given the multitude of medication classes that are now available as part of GDMT, targeting therapies may be especially important in settings with limited resources. Identifying and targeting the patients who are most likely to benefit from therapy via biomarker-led risk stratification could help direct medical attention and resources more efficiently. Additionally, for interventions which are associated with a reduction (or at least a lack of rise) in troponin levels over time, troponin may help assess medication adherence, and may also help guide uptitration of medication doses. New technologies utilizing digital algorithms embedded in electronic medical records may also help with the process. Already in the works are digital algorithms, in some cases guided by artificial intelligence and informed in part by cardiac biomarkers, to help guide treating clinicians in heart failure diagnosis as well as medication initiation and titration.
Selection for Clinical Trials
After experience gained from TOPCAT, clinical trialists in heart failure have become more savvy about drafting inclusion criteria to ensure appropriate patient selection [30]. A large part of this evolution includes the use of cardiac biomarkers, with many trials now requiring a minimum cutpoint to meet inclusion criteria. In some cases, a maximum cutpoint exists as well. In this way, trials can ensure that the patient population they are enrolling is reasonably likely to have a diagnosis of heart failure and is at high enough (or low enough) baseline risk to accomplish the study goals. Though the role for biomarkers has most often been filled with natriuretic peptides, highly sensitive troponins may play a larger role going forward.
Conclusion
The role of troponin in heart failure is evolving. Troponin is prognostic across the heart failure spectrum, but the future of troponin in heart failure will hinge upon whether it can play a significant role in helping with heart failure prevention and with tailoring and guiding heart failure treatments and interventions. This is an evolving field—not only in the ongoing development of assays that are more sensitive and being brought to the point of care, but also in the ability to leverage digital technologies including artificial intelligence and integrated algorithms into patient care. There is no shortage of opportunities for future studies of troponin to explore and presumably expand upon their clinical utility in heart failure, beyond prognosis.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Latini R, Masson S, Anand IS, Missov E, Carlson M, Vago T, et al. Prognostic value of very low plasma concentrations of troponin T in patients with stable chronic heart failure. Circulation. 2007;116(11):1242–9.
Aimo A, Januzzi JL Jr, Vergaro G, Ripoli A, Latini R, Masson S, et al. Prognostic value of high-sensitivity troponin T in chronic heart failure: an individual patient data meta-analysis. Circulation. 2018;137(3):286–97.
Gravning J, Askevold ET, Nymo SH, Ueland T, Wikstrand J, McMurray JJ, et al. Prognostic effect of high-sensitive troponin T assessment in elderly patients with chronic heart failure: results from the CORONA trial. Circ Heart Fail. 2014;7(1):96–103.
Yousufuddin M, Abdalrhim AD, Wang Z, Murad MH. Cardiac troponin in patients hospitalized with acute decompensated heart failure: a systematic review and meta-analysis. J Hosp Med. 2016;11(6):446–54.
Yancy CW, Jessup M, Bozkurt B, Masoudi FA, Butler J, McBride PE et al. ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013.
• Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022;145(18):e895–e1032. These most recent US heart failure clinical practice guidelines provide updated recommendations regarding the use of troponin in heart failure.
Januzzi JL Jr, Filippatos G, Nieminen M, Gheorghiade M. Troponin elevation in patients with heart failure: on behalf of the third Universal Definition of Myocardial Infarction Global Task Force: Heart Failure Section. Eur Heart J. 2012;33(18):2265–71.
Peacock WFT, De Marco T, Fonarow GC, Diercks D, Wynne J, Apple FS, et al. Cardiac troponin and outcome in acute heart failure. N Engl J Med. 2008;358(20):2117–26.
Omland T, de Lemos JA, Sabatine MS, Christophi CA, Rice MM, Jablonski KA, et al. A sensitive cardiac troponin T assay in stable coronary artery disease. N Engl J Med. 2009;361(26):2538–47.
Omland T, Pfeffer MA, Solomon SD, de Lemos JA, Rosjo H, Saltyte Benth J, et al. Prognostic value of cardiac troponin I measured with a highly sensitive assay in patients with stable coronary artery disease. J Am Coll Cardiol. 2013;61(12):1240–9.
Biener M, Giannitsis E, Kuhner M, Zelniker T, Mueller-Hennessen M, Vafaie M, et al. Prognostic value of high-sensitivity cardiac troponin T compared with risk scores in stable cardiovascular disease. Am J Med. 2017;130(5):572–82.
de Lemos JA, Drazner MH, Omland T, Ayers CR, Khera A, Rohatgi A, et al. Association of troponin T detected with a highly sensitive assay and cardiac structure and mortality risk in the general population. JAMA. 2010;304(22):2503–12.
deFilippi CR, de Lemos JA, Christenson RH, Gottdiener JS, Kop WJ, Zhan M, et al. Association of serial measures of cardiac troponin T using a sensitive assay with incident heart failure and cardiovascular mortality in older adults. JAMA. 2010;304(22):2494–502.
Seliger SL, Hong SN, Christenson RH, Kronmal R, Daniels LB, Lima JAC, et al. High-sensitive cardiac troponin T as an early biochemical signature for clinical and subclinical heart failure: MESA (Multi-Ethnic Study of Atherosclerosis). Circulation. 2017;135(16):1494–505.
Myhre PL, Claggett B, Ballantyne CM, Selvin E, Rosjo H, Omland T, et al. Association between circulating troponin concentrations, left ventricular systolic and diastolic functions, and incident heart failure in older adults. JAMA Cardiol. 2019;i4(10):997–1006.
Packer M, McMurray JJ, Desai AS, Gong J, Lefkowitz MP, Rizkala AR, et al. Angiotensin receptor neprilysin inhibition compared with enalapril on the risk of clinical progression in surviving patients with heart failure. Circulation. 2015;131(1):54–61.
• Murphy SP, Prescott MF, Maisel AS, Butler J, Pina IL, Felker GM, et al. Association between angiotensin receptor-neprilysin inhibition, cardiovascular biomarkers, and cardiac remodeling in heart failure with reduced ejection fraction. Circ Heart Fail. 2021;14(6):e008410. Subanalysis showing the association and interaction between cardiac biomarkers and the effect of sacubitril/valsartan on outcomes in HFrEF patients.
Jhund PS, Claggett BL, Voors AA, Zile MR, Packer M, Pieske BM et al. Elevation in high-sensitivity troponin T in heart failure and preserved ejection fraction and influence of treatment with the angiotensin receptor neprilysin inhibitor LCZ696. Circ Heart Fail. 2014;7(6):953–9.
• Gori M, Senni M, Claggett B, Liu J, Maggioni AP, Zile M, et al. Integrating high-sensitivity troponin T and sacubitril/valsartan treatment in HFpEF: the PARAGON-HF trial. JACC Heart Fail. 2021;9(9):627–35. Subanalysis showing the association and interaction between cardiac troponin and the effect of sacubitril/valsartan on outcomes in HFpEF patients.
• Berg DD, Docherty KF, Sattar N, Jarolim P, Welsh P, Jhund PS et al. Serial assessment of high-sensitivity cardiac troponin and the effect of dapagliflozin in patients with heart failure with reduced ejection fraction: an analysis of the DAPA-HF trial. Circulation. 2022;145(3):158–69. Subanalysis showing the association and interaction between cardiac troponin and the effect of dapagliflozin on outcomes in HFrEF patients.
Zelniker TA, Morrow DA, Mosenzon O, Goodrich EL, Jarolim P, Murphy SA, et al. Relationship between baseline cardiac biomarkers and cardiovascular death or hospitalization for heart failure with and without sodium-glucose co-transporter 2 inhibitor therapy in DECLARE-TIMI 58. Eur J Heart Fail. 2021;23(6):1026–36.
• Packer M, Januzzi JL, Ferreira JP, Anker SD, Butler J, Filippatos G et al. Concentration-dependent clinical and prognostic importance of high-sensitivity cardiac troponin T in heart failure and a reduced ejection fraction and the influence of empagliflozin: the EMPEROR-Reduced trial. Eur J Heart Fail. 2021;23(9):1529–38. Subanalysis showing the association and interaction between cardiac troponin and the effect of empagliflozin on outcomes in HFrEF patients.
• Januzzi JL, Jr., Butler J, Zannad F, Filippatos G, Ferreira JP, Pocock SJ et al. Prognostic implications of N-terminal pro-B-type natriuretic peptide and high-sensitivity cardiac troponin T in EMPEROR-Preserved. JACC Heart Fail. 2022;10(7):512–24. Subanalysis showing the association and interaction between cardiac biomarkers and the effect of empagliflozin on outcomes in HFpEF patients.
Myhre PL, O’Meara E, Claggett BL, de Denus S, Jarolim P, Anand IS, et al. Cardiac troponin I and risk of cardiac events in patients with heart failure and preserved ejection fraction. Circ Heart Fail. 2018;11(11):e005312.
Myhre PL, Vaduganathan M, O’Meara E, Claggett BL, de Denus S, Jarolim P, et al. Mechanistic effects of spironolactone on cardiovascular and renal biomarkers in heart failure with preserved ejection fraction: a TOPCAT biorepository study. Circ Heart Fail. 2020;13(1):e006638.
Ledwidge M, Gallagher J, Conlon C, Tallon E, O’Connell E, Dawkins I, et al. Natriuretic peptide-based screening and collaborative care for heart failure: the STOP-HF randomized trial. JAMA. 2013;310(1):66–74.
Daniels LB, Barrett-Connor E. Can natriuretic peptides help identify heart failure patients for whom statins are beneficial? J Am Coll Cardiol. 2009;54(20):1860–1.
Anand IS, Rector TS, Cleland JG, Kuskowski M, McKelvie RS, Persson H, et al. Prognostic value of baseline plasma amino-terminal pro-brain natriuretic peptide and its interactions with irbesartan treatment effects in patients with heart failure and preserved ejection fraction: findings from the I-PRESERVE trial. Circ Heart Fail. 2011;4(5):569–77.
Felker GM, Fiuzat M, Thompson V, Shaw LK, Neely ML, Adams KF, et al. Soluble ST2 in ambulatory patients with heart failure: association with functional capacity and long-term outcomes. Circ Heart Fail. 2013;6(6):1172–9.
Januzzi JL Jr, Canty JM, Das S, DeFilippi CR, Gintant GA, Gutstein DE, et al. Gaining efficiency in clinical trials with cardiac biomarkers: JACC review topic of the week. J Am Coll Cardiol. 2021;77(15):1922–33.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
LBD has received consulting fees from Quidel, Roche Diagnostics, and Siemens; and has served on Clinical Endpoints Adjudication Committees for Abbott and Applied Therapeutics. DA declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Agdashian, D., Daniels, L.B. What Is the Clinical Utility of Cardiac Troponins in Heart Failure? Are They Modifiable Beyond Their Prognostic Value?. Curr Heart Fail Rep 20, 33–43 (2023). https://doi.org/10.1007/s11897-023-00588-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11897-023-00588-z