Abstract
The prevalence of heart failure (HF) and its subtype, HF with preserved ejection fraction (HFpEF), is on the rise due to aging of the population. HFpEF is convergence of several pathophysiological processes, which are not yet clearly identified. HFpEF is usually seen in association with systemic diseases, such as diabetes, hypertension, atrial fibrillation, sleep apnea, renal and pulmonary disease. The proportion of HF patients with HFpEF varies by patient demographics, study settings (cohort vs. clinical trial, outpatient clinics vs. hospitalised patients) and cut points used to define preserved function. There is an expanding body of literature about prevalence and prognostic significance of both cardiovascular and non-cardiovascular comorbidities in HFpEF patients. Current therapeutic approaches are targeted towards alleviating the symptoms, treating the associated comorbid conditions, and reducing recurrent hospital admissions. There is lack of evidence-based therapies that show a reduction in the mortality amongst HFpEF patients; however, an improvement in exercise tolerance and quality of life is seen with few interventions. In this review, we highlight the epidemiology and current treatment options for HFpEF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Heart failure (HF) is a complex clinical syndrome where structural or functional abnormalities of the heart compromise its ability to fill with or eject sufficient blood to meet the metabolic requirements of the body [1]. HF results in a classic array of clinical signs and symptoms arising due to circulatory insufficiency during normal exertion as well as pulmonary or systemic venous congestion [2]. It affects about 2 % of adult population in the developed nations, and nearly 500,000 new cases are diagnosed each year in the USA [3]. The prevalence of HF increases with age, from 1 % amongst people less than 50 years to as much as 13 % amongst octogenarians and older [4••]. Its subtype, heart failure with preserved ejection fraction (HFpEF), has been observed to become more common with aging, and it is expected that this number is only going to increase as projected by the increase in life expectancy and by the population growth projections. It is estimated that HFpEF constitutes nearly half of the HF patients [5]. In comparison with the heart failure with reduced ejection fraction (HFrEF), the overall prognosis of HFpEF patients is similar to those of HFrEF with a higher degree of repeat hospitalizations in the former group. This points towards the existence of critical gaps in our understanding of the molecular pathways involved in the disease process and potential interventional targets [6••]. Further, while more than half of the deaths amongst HFpEF patients are attributed to cardiovascular causes (30 % of all being sudden), about one-third deaths have non-cardiovascular causes [7••]. Due to its complexity and lack of successful therapeutic targets thus far, there is a need for research oriented towards healthy aging and prevention of HFpEF through early control of its risk factors. In this review, we discuss the epidemiology and therapeutic options for HFpEF and contrast them with HFrEF.
Diagnosis and Classification
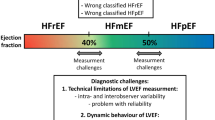
The diagnosis and classification of HFpEF remain challenging. There are several criteria to define HF and they have poor concordance [8] and majority of them do not include biomarkers or echocardiographic data [9•]. Historically, systolic HF or HFrEF has been the focus of both clinical studies and trials and its most common risk factors remain atherosclerosis and the ensuing ischemic insult to the myocardium. However, with recent epidemiologic studies showing a rise in the proportion of HF patients with apparently preserved ejection fraction [10••], the HFpEF has increasingly gained wider recognition. Although both HFpEF or HF with normal ejection fraction (HFnEF) have been used interchangeably, the term preserved ejection fraction may not be completely normal but only relatively so [11••], thus, the term HFpEF is more appropriate. Diastolic dysfunction constitutes the mainstay pathophysiological finding in HFpEF patients, and, thus, for this reason, diastolic heart failure was used to define the same syndrome. Recently, there has been a movement away from using this terminology owing to the fact that some degree of systolic dysfunction may also coexist in these patients [5], and the diastolic dysfunction in HFpEF patients may not be higher than age-matched sedentary controls and is not the target for intervention [12]. Further, an improved classification using echocardiographic measures and biomarkers may be needed to differentiate it from other entities such as non-cardiac dyspnea, valvular heart disease, or pericardial diseases [12–14]. Several cutoff values, prominently either greater than 40 or 50 %, have been used to define a preserved EF. Moreover, categorization of HFpEF using an EF cut point is not stable over time. During the follow-up of many years, EF declined on average by 5.8 % per 5 years and at least two fifths of HFpEF patients had reduced EF at some point during a mean follow-up of 3 years and vice versa [15•].
Lastly, according to the AHA guidelines, recovered EF is defined as a rise in the EF to greater than 40 % in a patient who previously had reduced ejection fraction [11••]. A recent study reported that approximately 70 % of patients diagnosed with HFpEF had reduced ejection fraction in the past and that the diagnosis of HFpEF in these patients is thus erroneous [16]. Also, it has been suggested that the patients with recovered ejection fraction significantly differ from the patients with HFpEF or HFrEF in terms of baseline characteristics as well as long-term prognosis [16, 17]. This might have an important bearing on the actual prevalence as well as important prognostic factors in patients presently being diagnosed as having HFpEF.
Two major criteria for diagnosing HFpEF have been proposed. First criteria by Vasan et al. suggested a triad of (1) signs and symptoms of congestive HF, (2) LVEF >50 % measured within 72 h of presentation and (3) diastolic dysfunction as evidenced by cardiac catheterization as necessary condition [18]. This criterion has practical limitations as demonstration of preserved EF within 72 h may not be feasible in clinical practice and the need of cardiac catheterization to demonstrate diastolic dysfunction has been questioned [19]. The more recent diagnostic criteria by the European Society of Cardiology suggested three conditions: (1) clinical evidence of congestive HF, (2) presence of normal or near normal LV systolic function and (3) establishment of LV diastolic dysfunction using either of the three methods, plasma natriuretic peptide levels or Doppler echocardiography or cardiac catheterisation [20].
Prevalence and Incidence
The prevalence of HFpEF amongst patients hospitalised for HF varies widely from 32 to 52 % (Fig. 1). This wide variation is primarily attributed to the different cutoff values of normal EF in different studies [21], though study population and settings are contributory too. The issue of missing EF is not often addressed in the registries, and these patients are more likely to have preserved EF and the proportion of HFpEF patients using an EF of ≥40 % as benchmark may be close to 50 % [22••, 23]. Clinical trials may have slightly selective samples and are not included in above estimates. Data from the Atherosclerosis Risk in Communities (ARIC) study suggest that around 850,000 cases of new heart failure are diagnosed every year in the USA of which half may have HFpEF [24]. In the general adult population of a developed country, the prevalence of HFpEF may be around 1.1 % [25]. Moreover, the prevalence has increased almost linearly over the last few decades. The relative proportion of patients with HFpEF in a large study in Olmsted County, mostly Caucasians, showed an increase during the 15-year period, from 38 % in 1987 to 54 % in 2001 [10••] In addition, the prevalence has been found to vary with age and gender. A large community-based study found that the prevalence of HFpEF increased from 0 % in males and 1 % in females in the age group of 25–49 years to 4–6 % in males and 8–10 % in females above 80 years, indicating an obvious rise in the prevalence with increasing age but additionally a higher prevalence amongst females as compared to age-matched males [26•].
Similar to the prevalence, the incidence of HFpEF increases with age, from 20 per 1000 persons in a 60–65-year age group to 80 per 1000 persons who are above 85 years of age [27]. The Framingham Heart Study reported temporal trends in the incidence of HF over a period of 50 years, from 1950 to 1999, which have remained relatively constant amongst males and have declined in females [28•]. However, more studies are required to delineate the incidence rates and temporal trends of HFpEF.
Demographics and Risk Factors
Large population-based studies have described the demographic factors in patients with HFpEF. Patients with HFpEF as compared to HFrEF patients are usually older and are more commonly females [29, 30]. Though the association of HFpEF with any particular ethnicity has not been clearly established, however, a small cohort study amongst the HF patients showed that the South Asians were more likely to have preserved EF as compared to the Whites [31]. In addition, it has been shown that ethnicity may influence the disease course and final outcome in the patients with HFpEF. In the above context, a study comprising HFpEF patients suggested that African Americans may have higher 5-year mortality than whites [32].
Table 1 summarises the various comorbidities seen in patients with HFpEF. Hypertension (60–80 %), ischemic heart disease (35–70 %), diabetes (20–45 %) and atrial fibrillation (15–40 %) are the common comorbidities (Fig. 2). Lifestyle issues such as obesity and cigarette smoking are common too. Worse outcomes are seen in patients with chronic obstructive lung disease (31 %) and renal insufficiency (26 %) [22••]. Comorbid conditions especially renal insufficiency and atrial fibrillation may be less common in randomised controlled trials than hospital-based registries due to exclusion criteria.
Traditional risk factors such as hypertension, diabetes mellitus and ischemic heart disease have been associated with a higher incidence of HFpEF [51–53]. Effects of hypertension on myocardial elasticity, vasculature and micro vessel may contribute to poor LV compliance and are risk factors for ischemic heart disease and arrhythmia such as AF which is usually seen in patients with HFpEF. Hypertension may be the strongest and most prevalent modifiable risk factor to prevent HFpEF. Diabetes mellitus and insulin resistance have been implicated in adverse cell signalling, myocardial apoptosis, fibrosis and changes in vasculature, thus contributing to HFpEF [54]. Myocardial ischemia facilitates the upregulation and activation of the fibroblasts in the cardiac wall that lead to fibrosis of the wall and hence reduced diastolic filling of the ventricles [55, 56]. It has been proposed that to define HFpEF appropriately, ischemia should be excluded as a cause or contributor. Lastly, arrhythmias such as atrial fibrillation (AF) are common and may have important influence on exercise capacity and decompensation [57]. Though echocardiographic focus has been on LV diastology using tissue Doppler, the presence of pulmonary hypertension and right ventricular dysfunction (RVD) is frequent and is associated with poor outcome in HFpEF patients [58•].
Hospitalisation
Hospitalisation marks as an important landmark in the natural disease course of HF as these patients are likely to be predisposed to a higher risk than the outpatient HF patients [59]. It serves as a harbinger of future increased risk of re-hospitalizations, morbidity and mortality [60]. Amongst the overall HF patients, the total hospitalizations, length of stay in the hospital as well as the in-hospital mortality have shown a constant decline over the last decade [61]. Nevertheless, the rates of subsequent readmission and post-discharge mortality have remained high [62].
Based on the large HFpEF trials, it can be inferred that the patients with HFpEF have lower hospitalisation rates than those with HFrEF [63•]; however, in a community-based cohort with similar NYHA class, HFpEF has higher rates of re-hospitalisation [10••]. Furthermore, HFrEF patients have nearly 1 % absolute higher in-hospital mortality rate than HFpEF patients [22••, 23]. The mean length of stay in the hospital (approximately 5–6 days) may not differ between HFpEF and HFrEF [22••, 23]. The rates of re-hospitalisation and post-discharge mortality amongst the patients with HFpEF have been estimated as 30 and 10 %, respectively, at 2–3 months post-discharge follow-up [23].
Mortality
HFpEF patients have a considerable annual mortality rate, ranging from 10 to 30 % [64]. Two large population-based studies followed the disease course of the HF patients after discharge from the hospital. In the Olmsted County HF cohort, mortality rates in HFpEF (29 %) were only slightly better than HFrEF (32 %). The Canadian EFFECT study found similar 30-day and 1-year survival rates by EF subgroups [6••]. Furthermore, during the study period of 15 years, although the post-discharge mortality rates declined for the patients with HFrEF, they remained nearly constant for the patients with HFpEF [10••]. These large cohort studies suggested that the mortality rates in HFpEF are nearly comparable to those with HFrEF. On the other hand, one of the largest recent meta-analysis compared the mortality rates in the two sub-groups of HF patients and found that HFpEF had 50 % lower hazards of mortality when compared to HFrEF [65••, 66]. The above differences may be partially attributed to selection bias in trials and need evaluation by population- or patient-based registries.
The causes of death in the HF patients can broadly be attributed to the cardiovascular and non-cardiovascular causes. The cardiovascular causes of death include pump failure, myocardial infarction, sudden cardiac death and cerebrovascular accidents while the non-cardiovascular deaths occur due to renal failure, chronic obstructive pulmonary disease, respiratory failure, cancer and infections [35]. It is established that when compared to HFrEF, the patients with HFpEF are older and accordingly have a higher burden of comorbid diseases [6••]. This offers an explanation for the higher prevalence of non-cardiovascular deaths in HFpEF [67]. The cause-specific mortality estimates show that the non-cardiovascular causes of death constitute nearly 30 to 50 % of all deaths in HFpEF patients while only 15–18 % in HFrEF patients [7••, 35]. Of note, the clinical trials report a lower proportion of non-cardiovascular deaths than do most of the population-based studies, owing to the fact that healthier subjects with lesser comorbid diseases are recruited in the trials [68].
Several studies have analysed the factors predicting mortality in the HF patients. Amongst all HF patients, low systolic blood pressure and elevated renal function tests (serum creatinine and blood urea nitrogen) at the time of presentation have been shown to be the most important predictors of mortality. While another study found that tachycardia increases the hazards of mortality in patients with HFpEF but not in HFrEF [22••]. In addition, greater patient age and lesser haemoglobin levels increase the likelihood of cardiovascular-related deaths in patients with HFpEF [35]. In yet another large clinical trial, it was reported that log N-terminal pro-B type natriuretic peptide, diabetes mellitus and prior hospitalisation were the important factors predicting mortality as well as future hospitalizations [69].
Treatment
The focus of the current treatment has been to alleviate acute symptoms and to control proximal risk factors as therapeutic trials focused on HFpEF patients have been mostly negative in terms of survival benefits. The treatment recommendations from the American Heart Association have set four goals in the management of these patients: (a) control of hypertension, (b) control of heart rate especially in the patients with atrial fibrillation, (c) control of pulmonary and peripheral edema and (d) prevention of myocardial ischemia [11••]. Table 2 summarises the major clinical trials that have evaluated the efficacy of various therapeutic drugs in patients with HFpEF.
Control of Hypertension
An optimal anti-hypertensive that improves the survival in the patients with HFpEF remains unclear. Drugs effective for HFrEF have been tried amongst HFpEF patients. Activation of renin-angiotensin-aldosterone axis contributes to sodium and water retention, hypertension and ventricular remodelling. Inhibition of this axis using angiotensin-converting enzyme inhibitors (ACEi) and aldosterone receptor blockers (ARBs) has been efficacious in controlling hypertension and has shown to significantly improve the survival in patients with HFrEF [81]. Based on these observations, several clinical trials have tested the efficacy of ACEi and ARBs in the patients with HFpEF. The three large clinical trials, PEP-CHF, CHARM-Preserved and I-PRESERVE, have investigated the roles of perindopril, an ACEi, and candesartan and irbesartan, ARBs, respectively, on mortality and hospitalisations in the patients with HFpEF [39, 41, 43]. None of these trials have observed any reduction in mortality. However, perindopril and candesartan were observed to reduce the rates of hospitalisation. A small study on 21 subjects evaluated the effect of enalapril on exercise capacity and observed an improvement in exercise time [71].
The negative ionotropic and chronotropic effects of β-blockers result in the control of hypertension and confer a survival advantage in the patients with HFrEF [82]. SENIORS study is the largest study to evaluate the efficacy of nebivolol in the management of HFpEF. It reported that there was no difference in either mortality- or cardiovascular-related hospitalisation between the study group and the placebo group [75]. However, another smaller study on 158 patients found significant reduction in mortality in patients with HFpEF taking propranolol [72].
Control of Heart Rate
Chronic diastolic dysfunction or underlying common pathophysiologic processes may predispose to supraventricular tachyarrhythmia [83]. Tachycardia in a patient with HFpEF may further reduce the LV filling in a heart that has poor diastolic function to begin with. Moreover, it can precipitate ischemia by increasing the myocardial oxygen demand. There are only a few trials that have evaluated an effective drug to control the heart rate in patients with HFpEF. A small study that investigated the effect of verapamil reported an increase in the peak filling rates and improved exercise capacity in patients with HFpEF [70]. In spite of known negative chronotropic effects of β-blockers, their efficacy in controlling tachycardia in HFpEF is yet to be studied.
Control of Edema
Diuretics form the mainstay of treatment in patients with pulmonary or peripheral edema [84]. The Hong Kong Diastolic Heart Failure study compared the use of diuretics alone versus diuretics with ACEi/ARBs. It reported that treatment with diuretics significantly improved the quality of life and alleviated the congestive symptoms in patients with HFpEF. The addition of ACEi/ARBs added a little further improvement in the quality of life. However, they led to a significant reduction in the plasma levels of natriuretic peptide [42]. A large study evaluating spironolactone observed a decrease in cardiovascular-related hospitalisations in HFpEF, though no reduction in mortality was evident [45].
Prevention of Ischemia
Myocardial ischemia has classically been treated by coronary revascularisation procedures. However, ranolazine is a newer anti-ischemic drug that improves the coronary blood flow preferentially in the ischemic areas of the heart. It has been observed to improve the diastolic tone and oxygen handling during ischemia [85]. Studies evaluating the effect of ranolazine in HF patients have reported an improvement in the diastolic function [85].
Other Therapeutic Agents
The effect of digoxin was evaluated by DIG-PEF, a large randomised trial. Although digoxin was observed to alleviate the symptoms, however, no benefit in terms of mortality or hospitalisation was observed [40].
Tehrani et al. evaluated the effect of statins in the patients with HFpEF and found surprisingly significant reduction in mortality. Further studies on larger number of subjects are needed to validate the role of statins in mortality reduction [76].
Non-pharmacological Therapy
Exercise training has clearly been shown to benefit cardiorespiratory health in patients with HFrEF. Recent studies have addressed the effects of exercise training in patients with HFpEF. Though the effects on HF-related mortality and hospitalisations were not studied, these reports evaluated the improvement in the quality of life, exercise tolerance and left ventricular EF [86, 87]. A 16-week randomised trial studied the effects of supervised exercise training in patients with HFpEF and observed that the peak exercise oxygen uptake was significantly improved in the exercise cohort as compared to the controls. In addition, exercise time and 6-min walk distance also showed an improvement [86]. Although other similar trials have replicated the effect of exercise training on the quality of life, however, a significant improvement in the left ventricular EF has not been shown [86, 87].
Prevention
In view of a lack of effective therapies that can improve the survival in patients with HFpEF, prevention remains the best approach to reduce its burden. As discussed above, hypertension antedates the development of HFpEF in nearly 90 % of the cases and it confers a two- to threefold increased risk of developing HFpEF [51]. Therefore, risk modification to prevent hypertension in the first place as well as controlling it in the early stages once it develops would be an essential step towards the prevention of HFpEF. Stringent control of hypertension in order to maintain the blood pressure within normal range is required. Supporting this argument, HYVET trial observed a dramatic 64 % reduction in the development of HF and 21 % reduction in mortality, subsequent to controlling hypertension [1].
As noted above, insulin resistance leads to an array of metabolic aberrations in cardiac myocytes contributing towards the pathogenesis of HFpEF. So treating the insulin resistance might as well target the prevention of HFpEF. Finally, the prevention of ischemia by newer drugs such as ranolazine, a fatty acid oxidation inhibitor that improves the coronary blood flow preferentially in the ischemic areas [88], might go a long way in the prevention of HFpEF.
Finally, recent studies have shown that lower levels of cardiorespiratory fitness in mid-life are associated with a greater risk of heart failure, particularly in older age [89]. This seems to be mediated through a greater degree diastolic dysfunction amongst low-fit individuals [90•]. Taken together, these findings suggest that improving cardiorespiratory fitness amongst low-fit sedentary individuals by exercise training could represent a novel preventive approach against HFpEF. Further clinical trials are needed to evaluate the efficacy of exercise training in preventing HFpEF amongst low-fit at-risk individuals.
There are several ongoing trials registered on trials.gov that examine nitric oxide precursors as an active intervention to improve exercise tolerance and haemodynamics in HFpEF patients. Whether renal sympathetic denervation provides benefit to HFpEF patients with poorly controlled hypertension remains an active area of research. Agents that modify myocardial energy substrate such as perhexiline are also being studied currently.
Existing Gaps
Several gaps exist in our current understanding of HFpEF, its accurate diagnosis and effective treatment. First, the incidence and temporal risk factors of HFpEF remain less clear. Whether the prevalence of diastolic dysfunction as currently measured is higher in HFpEF patients than controls remains unclear. Whether right ventricular structural and functional measures, as well as pulmonary pressures, would improve HFpEF sub-classification needs consideration. Secondly, there is a need for a validated and a sensitive diagnostic criterion that defines a clear cutoff value for “preserved EF”. Finally and most importantly, we lack definitive therapies for the treatment of HFpEF. The classic drugs that have improved the survival of patients with HFrEF have failed to reduce the mortality in HFpEF [23]. Future research should be directed towards the fundamental understanding of the molecular basis of the disease.
Conclusion
HFpEF constitutes about 50 % of all HF patients. Its prevalence increases with age, and it is more commonly seen in females. It has a higher burden of cardiovascular and non-cardiovascular comorbid conditions. The diagnosis of this complex syndrome remains challenging in view of the absence of any sensitive set of diagnostic criteria. Current treatment is targeted towards alleviating the symptoms and treating the associated comorbid conditions, and there is no evidence-based therapy showing a reduction in the mortality of these patients. Therefore, prevention via the early modification of risk factors may remain the best approach in reducing its burden. Further studies are needed that aid in a better understanding of this complex syndrome and to design therapeutic strategies that will improve the outcome in these patients.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Hunt SA, Abraham WT, Chin MH, Feldman AM, Francis GS, Ganiats TG, et al. Focused update incorporated into the ACC/AHA 2005 guidelines for the diagnosis and management of heart failure in adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the International Society for Heart and Lung Transplantation. Circulation. 2009;119:391–479.
Jessup M, Brozena S. Heart failure. N Engl J Med. 2003;348:2007–18.
Hunt SA, Baker DW, Chin MH, Cinquegrani MP, Feldman AM, Francis GS, et al. ACC/AHA guidelines for the evaluation and management of chronic heart failure in the adult: executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to revise the 1995 Guidelines for the Evaluation and Management of Heart Failure). J Am Coll Cardiol. 2001;38:2101–13.
Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, et al. Heart disease and stroke statistics—2014 update: a report from the American Heart Association. Circulation. 2014;129(3):e28–292. This AHA document highlights the statistics for HF epidemic in the US.
McMurray JJ, Adamopoulos S, Anker SD, Auricchio A, Böhm M, Dickstein K, et al. ESC Committee for Practice Guidelines. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2012;33:1787–847.
Bhatia RS, Tu JV, Lee DS, Austin PC, Fang J, Haouzi A, et al. Outcome of heart failure with preserved ejection in a population-based study. N Engl J Med. 2006;355:260–9. This study reported similar one year mortality in patients with newly diagnosed HFpEF and HFrEF.
Zile MR, Gaasch WH, Anand IS, Haass M, Little WC, Miller AB, et al. Mode of death in patients with heart failure and a preserved ejection fraction: results from the Irbesartan in Heart Failure with Preserved Ejection Fraction Study (I-Preserve) trial. Circulation. 2010;121:1393–405. This study reports the causes of death among HFpEF patients enrolled in a large trial.
Rosamond WD, Chang PP, Baggett C, Johnson A, Bertoni AG, Shahar E, et al. Classification of heart failure in the atherosclerosis risk in communities (ARIC) study: a comparison of diagnostic criteria. Circ Heart Fail. 2012;5(2):152–9.
Loehr LR, Agarwal SK, Baggett C, Wruck LM, Chang PP, Solomon SD, et al. Classification of acute decompensated heart failure: an automated algorithm compared with a physician reviewer panel: the Atherosclerosis Risk in Communities study. Circ Heart Fail. 2013;6(4):719–26. This study implements and compares a novel heart failure classification consensus scheme that includes biomarkers and echocardiographic parameters.
Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med. 2006;355:251–9. This study reported an increase in prevalence from 1987–2001 without any improvement in mortality rates in a US community with predominantly white patients.
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey Jr DE, Drazner MH, et al. ACCF/AHA guideline for the management of heart failure: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013;128(16):1810–52. This AHA/ACC guideline highlights the management options and algorithms for HF patients.
Maurer MS, Hummel SL. Heart failure with a preserved ejection fraction: what is in a name? J Am Coll Cardiol. 2011;58(3):275–7.
Bishu K, Deswal A, Chen HH, LeWinter MM, Lewis GD, Semigran MJ, et al. Biomarkers in acutely decompensated heart failure with preserved or reduced ejection fraction. Am Heart J. 2012;164(5):763–70.
Penicka M, Vanderheyden M, Bartunek J. Diagnosis of heart failure with preserved ejection fraction: role of clinical Doppler echocardiography. Heart. 2014;100(1):68–76.
Dunlay SM, Roger VL, Weston SA, Jiang R, Redfield MM. Longitudinal changes in ejection fraction in heart failure patients with preserved and reduced ejection fraction. Circ Heart Fail. 2012;5(6):720–6. This study reports changes in EF based status among HFpEF and HFrEF patients over time.
Punnoose LR, Givertz MM, Lewis EF, Pratibhu P, Stevenson LW, Desai AS. Heart failure with recovered ejection fraction: a distinct clinical entity. J Card Fail. 2011;17:527–32.
Basuray A, French B, Ky B, Vorovich E, Olt C, Sweitzer NK, et al. Heart failure with recovered ejection fraction: clinical description, biomarkers, and outcomes. Circulation. 2014;129(23):2380–7. This study reports the prevalence of HF with recovered EF and distinguishes it from HFpEF and HFrEF.
Vasan RS, Levy D. Defining diastolic heart failure: a call for standardized diagnostic criteria. Circulation. 2000;101:2118–21.
Zile MR, Baicu CF, Gaasch WH. Diastolic heart failure—abnormalities in active relaxation and passive stiffness of the left ventricle. N Engl J Med. 2004;350:1953–9.
Paulus WJ, Tschope C, Sanderson JE, Rusconi C, Flachskampf FA, Rademakers FE, et al. How to diagnose diastolic heart failure: a consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the Heart Failure and echocardiography Associations of the European Society of Cardiology. Eur Heart J. 2007;28:2539–50.
Vasan RS, Benjamin EJ, Levy D. Prevalence, clinical features and prognosis of diastolic heart failure: an epidemiologic perspective. J Am Coll Cardiol. 1995;26:1565–74.
Yancy CW, Lopatin M, Stevenson LW, De Marco T, Fonarow GC. Clinical presentation, management, and in-hospital outcomes of patients admitted with acute decompensated heart failure with preserved systolic function: a report from the Acute Decompensated Heart Failure National Registry (ADHERE) database. J Am Coll Cardiol. 2006;47(1):76–84. A descriptive paper from largest registry of hospitalized HFpEF patients.
Fonarow GC, Stough WG, Abraham WT, Albert NM, Gheorghiade M, Greenberg BH, et al. Characteristics, treatments, and outcomes of patients with preserved systolic function hospitalized for heart failure: a report from the OPTIMIZE-HF Registry. J Am Coll Cardiol. 2007;50(8):768–77.
Chang PP, Chambless LE, Shahar E, Bertoni AG, Russell SD, Ni H, et al. Incidence and survival of hospitalized acute decompensated heart failure in four US communities (from the Atherosclerosis Risk in Communities Study). Am J Cardiol. 2014;113(3):504–10.
Owan TE, Redfield MM. Epidemiology of diastolic heart failure. Prog Cardiovasc Dis. 2005;47:320–32.
Ceia F, Fonseca C, Mota T, Morais H, Matias F, de Sousa A, et al. Prevalence of chronic heart failure in Southwestern Europe: the EPICA study. Eur J Heart Fail. 2002;4:531–9. This study reports the prevalence of HFpEF in Portuguese reporting a higher prevalence than HFrEF.
Curtis LH, Whellan DJ, Hammill BG, Hernandez AF, Anstrom KJ, Shea AM, et al. Incidence and prevalence of heart failure in elderly persons, 1994–2003. Arch Intern Med. 2008;168(4):418–24.
Levy D, Kenchaiah S, Larson MG, Benjamin EJ, Kupka MJ, Ho KK, et al. Long-term trends in the incidence of and survival with heart failure. N Engl J Med. 2002;347:1397–402. This paper from Framingham cohort study reports a decrease in HF mortality since 1950, and a simultaneous decline in HF incidence among women but not among men.
Senni M, Tribouilloy CM, Rodeheffer RJ, Jacobsen SJ, Evans JM, Bailey KR, et al. Congestive heart failure in the community: a study of all incident cases in Olmsted County, Minnesota, in 1991. Circulation. 1998;98:2282–9.
Yip GW, Ho PP, Woo KS, Sanderson JE. Comparison of frequencies of left ventricular systolic and diastolic heart failure in Chinese living in Hong Kong. Am J Cardiol. 1999;84:563–7.
Sharp A, Tapp R, Francis DP, McG Thom SA, Hughes AD, Stanton AV, et al. Ethnicity and left ventricular diastolic function in hypertension an ASCOT (Anglo-Scandinavian Cardiac Outcomes Trial) substudy. J Am Coll Cardiol. 2008;52:1015–21.
East MA, Peterson ED, Shaw LK, Gattis WA, O’Connor CM. Racial difference in the outcomes of patients with diastolic heart failure. Am Heart J. 2004;148:151–6. This study reports poorer survival among black patients with HFpEF than whites.
MacCarthy PA, Kearney MT, Nolan J, Lee AJ, Prescott RJ, Shah AM, et al. Prognosis in heart failure with preserved left ventricular systolic function: prospective cohort study. BMJ. 2003;327:78–9.
Klapholz M, Maurer M, Lowe AM, Messineo F, Meisner JS, Mitchell J, et al. Hospitalization for heart failure in the presence of a normal left ventricular ejection fraction: results of the New York Heart Failure Registry. J Am Coll Cardiol. 2004;43:1432–8.
Hamaguchi S, Kinugawa S, Sobirin MA, Goto D, Tsuchihashi-Makaya M, Yamada S, et al. Mode of death in patients with heart failure and reduced vs. preserved ejection fraction: report from the registry of hospitalized heart failure patients. Circ J. 2012;76(7):1662–9.
Steinberg BA, Zhao X, Heidenreich PA, Peterson ED, Bhatt DL, Cannon CP, et al. Trends in patients hospitalized with heart failure and preserved left ventricular ejection fraction: prevalence, therapies, and outcomes. Circulation. 2012;126(1):65–75. Study discussing in detail the hospitalization and in-hospital mortality in patients of Heart failure with Preserved ejection fraction.
West R, Liang L, Fonarow GC, Kociol R, Mills RM, O’Connor CM, et al. Characterization of heart failure patients with preserved ejection fraction: a comparison between ADHERE-US registry and ADHERE-International registry. Eur J Heart Fail. 2011;13(9):945–52.
Senni M, Gavazzi A, Oliva F, Mortara A, Urso R, Pozzoli M, et al. In-hospital and 1-year outcomes of acute heart failure patients according to presentation (de novo vs. worsening) and ejection fraction. Results from IN-HF Outcome Registry. Int J Cardiol. 2014;173(2):163–9.
Yusuf S, Pfeffer MA, Swedberg K, Granger CB, Held P, McMurray JJ, et al. Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction: the CHARM-Preserved Trial. Lancet. 2003;362:777–81.
Ahmed A, Rich MW, Fleg JL, Zile MR, Young JB, Kitzman DW, et al. Effects of digoxin on morbidity and mortality in diastolic heart failure; the ancillary digitalis investigation group trial. Circulation. 2006;114:266–70.
Cleland JG, Tendera M, Adamus J, Freemantle N, Polonski L, Taylor J. The perindopril in elderly people with chronic heart failure (PEP-CHF) study. Eur Heart J. 2006;27:2338–45.
Yip GWK, Wang M, Wang T, Chan S, Fung JW, Yeung L, et al. The Hong Kong diastolic heart failure study: a randomized controlled trial of diuretics, irbesartan and ramipril on quality of life, exercise capacity, left ventricular global and regional function in heart failure with a normal ejection. Heart. 2008;94:573–80.
Massie BM, Carson PE, McMurray JJ, Komajda M, McKelvie R, Zile MR, et al. Irbesartan in patients with heart failure and preserved ejection fraction. N Engl J Med. 2008;359:2456–67.
van Veldhuisen DJ, Cohen-Solal A, Böhm M, Anker SD, Babalis D, Roughton M, et al. SENIORS Investigators. Beta-blockade with nebivolol in elderly heart failure patients with impaired and preserved left ventricular ejection fraction: data from SENIORS (Study of Effects of Nebivolol Intervention on Outcomes and Rehospitalization in Seniors With Heart Failure). J Am Coll Cardiol. 2009;53(23):2150–8.
Pitt B, Pfeffer MA, Assmann SF, Boineau R, Anand IS, Claggett B, et al. Spironolactone for heart failure with preserved ejection fraction. N Engl J Med. 2014;370(15):1383–92.
Bursi F, Weston SA, Redfield MM, Jacobsen SJ, Pakhomov S, Nkomo VT, et al. Systolic and diastolic heart failure in the community. JAMA. 2006;296:2209–16.
Lee DS, Gona P, Vasan RS, Larson MG, Benjamin EJ, Wang TJ, et al. Relation of disease pathogenesis and risk factors to heart failure with preserved or reduced ejection fraction: insights from the Framingham Heart Study of the national heart, lung, and blood institute. Circulation. 2009;119:3070–7.
Brouwers FP, de Boer RA, van der Harst P, Voors AA, Gansevoort RT, Bakker SJ, et al. Incidence and epidemiology of new onset heart failure with preserved vs. reduced ejection fraction in a community-based cohort: 11-year follow-up of PREVEND. Eur Heart J. 2013;34(19):1424–31.
Adabag S, Smith LG, Anand IS, Berger AK, Luepker RV. Sudden cardiac death in heart failure patients with preserved ejection fraction. J Card Fail. 2012;18(10):749–54.
Chun S, Tu JV, Wijeysundera HC, Austin PC, Wang X, Levy D, et al. Lifetime analysis of hospitalizations and survival of patients newly admitted with heart failure. Circ Heart Fail. 2012;5(4):414–21.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo Jr JL, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 Report. JAMA. 2003;289:2560–72.
Choudhury L, Gheorghiade M, Bonow RO. Coronary artery disease in patients with heart failure and preserved systolic function. Am J Cardiol. 2002;89:719–22.
Levy D, Larson MG, Vasan RS, Kannel WB, Ho KK. The progression from hypertension to congestive heart failure. JAMA. 1996;275:1557–62.
van Heerebeek L, Hamdani N, Handoko ML, Falcao-Pires I, Musters RJ, Kupreishvili K, et al. Diastolic stiffness of the failing diabetic heart: importance of fibrosis, advanced glycation end products, and myocyte resting tension. Circulation. 2008;117:43–51.
He KL, Dickstein M, Sabbah HN, Yi GH, Gu A, Maurer M, et al. Mechanisms of heart failure with well-preserved ejection fraction in dogs following limited coronary microembolization. Cardiovasc Res. 2004;64:72–83.
Asanuma T, Uranishi A, Masuda K, Ishikura F, Beppu S, Nakatani S. Assessment of myocardial ischemic memory using persistence of post-systolic thickening after recovery from ischemia. JACC Cardiovasc Imaging. 2009;2:1253–61.
Zakeri R, Borlaug BA, McNulty SE, Mohammed SF, Lewis GD, Semigran MJ, et al. Impact of atrial fibrillation on exercise capacity in heart failure with preserved ejection fraction: a RELAX trial ancillary study. Circ Heart Fail. 2014;7(1):123–30.
Melenovsky V, Hwang SJ, Lin G, Redfield MM, Borlaug BA. Right heart dysfunction in heart failure with preserved ejection fraction. Eur Heart J. 2014 May 29. This study examines the role and association of right ventricular dysfunction in HFpEF patients.
Vaduganathan M, Fonarow GC. Epidemiology of hospitalised heart failure: differences and similarities between patients with reduced versus preserved ejection fraction. Heart Fail Clin. 2013;9(3):271–6.
Ahmed A, Allman RM, Fonarow GC, Love TE, Zannad F, Dell’italia LJ, et al. Incident heart failure hospitalization and subsequent mortality in chronic heart failure: a propensity-matched study. J Card Fail. 2008;14(3):211–8.
Bueno H, Ross JS, Wang Y, Chen J, Vidán MT, Normand SL, et al. Trends in length of stay and short-term outcomes among Medicare patients hospitalized for heart failure, 1993–2006. JAMA. 2010;303(21):2141–7.
Ross JS, Chen J, Lin Z, Bueno H, Curtis JP, Keenan PS, et al. Recent national trends in readmission rates after heart failure hospitalization. Circ Heart Fail. 2010;3(1):97–103.
Campbell RT, Jhund PS, Castagno D, Hawkins NM, Petrie MC, McMurray JJ. What have we learned about patients with heart failure and preserved ejection fraction from DIG-PEF, CHARM-preserved, and I-PRESERVE? J Am Coll Cardiol. 2012;60(23):2349–56. This editorial compares outcomes for patients enrolled in few clinical trials among HFpEF patients.
Chan MM, Lam CS. How do patients with heart failure with preserved ejection fraction die? Eur J Heart Fail. 2013;15:604–13.
Somaratne JB, Berry C, McMurray JJ, Poppe KK, Doughty RN, Whalley GA. The prognostic significance of heart failure with preserved left ventricular ejection fraction: a literature-based meta-analysis. Eur J Heart Fail. 2009;11:855–62. This meta-analysis reported lower mortality rate among HFpEF patients than HFrEF.
Meta-analysis Global Group in Chronic Heart Failure (MAGGIC). The survival of patients with heart failure with preserved or reduced left ventricular ejection fraction: an individual patient data meta-analysis. Eur Heart J. 2012;33(14):1750–7.
Henkel DM, Redfield MM, Weston SA, Gerber Y, Roger VL. Death in heart failure: a community perspective. Circ Heart Fail. 2008;1:91–7.
Lam CS, Donal E, Kraigher-Krainer E, Vasan RS. Epidemiology and clinical course of heart failure with preserved ejection fraction. Eur J Heart Fail. 2011;13(1):18–28.
Komajda M, Carson PE, Hetzel S, McKelvie R, McMurray JJ, Ptaszynska A, et al. Factors associated with outcome in heart failure with preserved ejection fraction: findings from the Irbesartan in heart failure with preserved ejection fraction study (I-PRESERVE). Circ Heart Fail. 2011;4:27–35.
Setaro JF, Zaret BL, Schulman DS, Black HR, Soufer R. Usefulness of verapamil for congestive heart failure associated with abnormal left ventricular diastolic filling and normal left ventricular systolic performance. Am J Cardiol. 1990;66(12):981–6.
Aronow WS, Kronzon I. Effect of enalapril on congestive heart failure treated with diuretics in elderly patients with prior myocardial infarction and normal left ventricular ejection fraction. Am J Cardiol. 1993;71(7):602–4.
Aronow WS, Ahn C, Kronzon I. Effect of propranolol versus no propranolol on total mortality plus nonfatal myocardial infarction in older patients with prior myocardial infarction, congestive heart failure, and left ventricular ejection fraction > or =40 % treated with diuretics plus angiotensin-converting enzyme inhibitors. Am J Cardiol. 1997;80(2):207–9.
Nodari S, Metra M, Dei CL. Beta-blocker treatment of patients with diastolic heart failure and arterial hypertension. A prospective, randomized, comparison of the long-term effects of atenolol vs. nebivolol. Eur J Heart Fail. 2003;5(5):621–7.
Takeda Y, Fukutomi T, Suzuki S, Yamamoto K, Ogata M, Kondo H, et al. Effects of carvedilol on plasma B-type natriuretic peptide concentration and symptoms in patients with heart failure and preserved ejection fraction. Am J Cardiol. 2004;94(4):448–53.
Flather MD, Shibata MC, Coats AJ, Van Veldhuisen DJ, Parkhomenko A, Borbola J, et al. Randomized trial to determine the effect of nebivolol on mortality and cardiovascular hospital admission in elderly patients with heart failure (SENIORS). Eur Heart J. 2005;26:215–25.
Tehrani F, Morrissey R, Phan A, Chien C, Schwarz ER. Statin therapy in patients with diastolic heart failure. Clin Cardiol. 2010;35:e1–5.
Solomon SD, Zile M, Pieske B, Voors A, Shah A, Kraigher-Krainer E, et al. The angiotensin receptor neprilysin inhibitor LCZ696 in heart failure with preserved ejection fraction: a phase 2 double-blind randomised controlled trial. Lancet. 2012;380(9851):1387–95.
Edelmann F, Wachter R, Schmidt AG, Kraigher-Krainer E, Colantonio C, Kamke W, et al. Effect of spironolactone on diastolic function and exercise capacity in patients with heart failure with preserved ejection fraction: the Aldo-DHF randomized controlled trial. JAMA. 2013;309(8):781–91.
Yamamoto K, Origasa H, Hori M. J-DHF Investigators. Effects of carvedilol on heart failure with preserved ejection fraction: the Japanese Diastolic Heart Failure Study (J-DHF). Eur J Heart Fail. 2013;15(1):110–8.
Maier LS, Layug B, Karwatowska-Prokopczuk E, Belardinelli L, Lee S, Sander J, et al. RAnoLazIne for the treatment of diastolic heart failure in patients with preserved ejection fraction: the RALI-DHF proof-of-concept study. JACC Heart Fail. 2013;1(2):115–22.
Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. The SOLVD Investigators. N Engl J Med. 1991; 325(5):293–302.
Effect of metoprolol CR/XL in chronic heart failure: Metoprolol CR/XL Randomised Intervention Trial in Congestive Heart Failure (MERIT-HF). Lancet. 1999;353(9169):2001–7.
Cuspidi C, Meani S, Fusi V, Valerio C, Catini E, Sala C, et al. Prevalence and correlates of left atrial enlargement in essential hypertension: role of ventricular geometry and the metabolic syndrome: the Evaluation of Target Organ Damage in Hypertension study. J Hypertens. 2005;23:875–82.
Sica DA, Gehr TWB, Frishman WH. Use of diuretics in the treatment of heart failure in the elderly. Clin Geriatr Med. 2007;23:107–21.
Maier LS. New treatment options for late Na current, arrhythmias, and diastolic dysfunction. Curr Heart Fail Rep. 2012;9:183–91.
Kitzman DW, Brubaker PH, Morgan TM, Stewart KP, Little WC. Exercise training in older patients with heart failure and preserved ejection fraction: a randomized, controlled, single-blind trial. Circ Heart Fail. 2010;3:659–67.
Kitzman DW, Brubaker PH, Herrington DM, Morgan TM, Stewart KP, Hundley WG, et al. Effect of endurance exercise training on endothelial function and arterial stiffness in older patients with heart failure and preserved ejection fraction: a randomized, controlled, single-blind trial. J Am Coll Cardiol. 2013;62:584–92.
Stone HP, Chaitman BR, Stocke K, Sano J, DeVault A, Koch GG. The anti-ischemic action of ranolazine in stable ischemic heart disease. J Am Coll Cardiol. 2010;56:934–442.
Berry JD, Pandey A, Gao A, Leonard D, Farzaneh-Far R, Ayers C, et al. Physical fitness and risk for heart failure and coronary artery disease. Circ Heart Fail. 2013;6(4):627–34.
Brinker SK, Pandey A, Ayers CR, Barlow CE, DeFina LF, Willis BL, et al. Association of cardiorespiratory fitness with left ventricular remodeling and diastolic function: the cooper center longitudinal study. JACC Heart Fail. 2014;2(3):238–46. This study shows poorer diastolic and other structural measures among participants with lower fitness level.
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
Abhinav Dhingra, Aayushi Garg, Simrat Kaur, Saurav Chopra, Jaspreet Singh Batra, Ambarish Pandey, Antoine H. Chaanine and Sunil K. Agarwal declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dhingra, A., Garg, A., Kaur, S. et al. Epidemiology of Heart Failure with Preserved Ejection Fraction. Curr Heart Fail Rep 11, 354–365 (2014). https://doi.org/10.1007/s11897-014-0223-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11897-014-0223-7