Abstract
Although the past few decades have yielded significant improvements in the management of cardiomyopathy, heart failure remains a leading cause of hospitalization as well as readmissions, both in the United States and worldwide. Accurate assessment of volume status in these patients is of great importance because it guides initial therapies and aids in determining suitability for discharge. However, this assessment can prove to be challenging and, therefore, must be based on multiple data points and techniques. This review examines the various modalities of volume assessment in the patient with decompensated heart failure.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
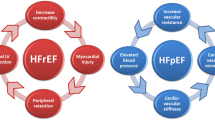
Heart failure (HF) affects over 5 million Americans, and decompensated HF (DHF) is the leading cause of hospitalizations among patients older than 65 years [1]. Nearly 90% of these admissions are due to symptoms of congestion [2]. Despite significant advancements in pharmacologic therapies, readmission rates remain high, approaching 50% at 6 months [3]. This is often related to inadequate decongestion during initial hospitalization and lack of an appropriate plan to maintain a normal volume state.
Volume assessment in HF can be difficult and there is no one reliable indicator. In this review, we examine the many techniques for volume assessment in the HF patient and how each can play a role in guiding type and duration of therapy.
Initial Assessment
A thorough history and physical can help decipher a patient’s volume status as well as give clues to the etiology of HF decompensation. However, the various components of the history and physical examination have a wide range of specificities and sensitivities in regard to accurately determining the presence of congestion (Table 1) [4–6]. As such, it is best to utilize them in combination in the context of the individual patient.
Historical Items
The medical history can help to confirm the presence of HF. A pooled analysis of 22 studies evaluating how best to conclude if HF was the cause of an emergency department visit with dyspnea as the presenting symptom revealed the most useful historical items to be a history of HF, myocardial infarction, or coronary disease (likelihood ratio [LR] 5.8, 3.1, and 1.8, respectively). Similarly, the absence of the above historical findings decreased the likelihood of HF (LR 0.45, 0.68, and 0.69, respectively) [6]. Therefore, a directed history can aid in determining if congestion is present.
Dyspnea is a common presenting symptom for patients with DHF [2], and registry data reveals that as many as 90% of hospitalized HF patients will have this complaint [7]. This often reflects pulmonary congestion due to an increase in pulmonary capillary wedge pressure (PCWP) as a result of left ventricular (LV) dysfunction generally related to volume overload. Dyspnea and its resolution are also used by clinical trials and the U.S. Food and Drug Administration as a key end point. Despite its high prevalence and importance, dyspnea is neither sensitive nor specific for DHF as it may be noncardiac in origin. Further complicating the matter is the purely subjective nature of this complaint and the lack of a standardized definition or measurement. Dyspnea challenges and severity scores, such as the Provocative Dyspnoea Assessment, which utilizes dynamic maneuvers and ambulation to more objectively define this symptom, have been proposed, but to date no trials have assessed their efficacy [8]. Nevertheless, assessment of dyspnea and an objective notation of its severity should be made on admission and monitored as a marker of response to treatment. This can be done by quantifying amount of activity, or change in position that brings on dyspnea.
Orthopnea is due to redistribution of blood to the thoracic compartment and pulmonary circulation while supine. In the Evaluation Study of Congestive Heart Failure and Pulmonary Artery Catheterization Effectiveness (ESCAPE) trial, orthopnea relieved by two or more pillows was independently associated with a PCWP of 28 mmHg or more [9]. Orthopnea often precedes a decompensation of HF, and in a hemodynamic analysis of HF patients, 91% of those with an elevated PCWP had orthopnea in the preceding week [10]. Additionally, persistent orthopnea despite medical therapy is associated with higher rates of rehospitalization [11].
Daily variations in body weight in patients with HF are likely to reflect changes in volume status, particularly the decompensated patient with increased sodium and water retention. Asking the patient their baseline or usual weight and assessing the degree of weight gain can be additional evidence in determining the amount of congestion and, therefore, efficacy of treatment.
Additionally, patient-specific factors should be elicited during the initial history. A patient’s congestion may manifest in a variety of ways, from lower extremity edema, to hand swelling and nausea. Asking the patient to identify their specific marker of congestion can be useful.
Physical Exam
Jugular venous pressure (JVP) reflects right atrial pressure (RAP) and, when assessed by experienced clinicians, estimation of JVP has a strong correlation to invasive measurement of central venous pressure [12]. RAP has been shown to be concordant with PCWP in patients with advanced HF [13] and, as such, can be utilized to estimate left-sided filling pressure. JVP of 12 mmHg (~16 cm H2O) or higher has been shown to accurately correlate with elevated PCWP on invasive monitoring [9]. Furthermore, in this analysis of data from the ESCAPE trial, after utilization of JVP, no data from the history and physical examination other than JVP provided additional information to detect a PCWP above 22 mmHg. This confirmed previous data revealing elevated JVP to be an independent predictor of a high PCWP (>18 mmHg), with a probability of 86% [4]. Furthermore, a prior review of 12 studies determined that an increased JVP is one of the best findings for detecting increased filling pressures [14]. Therefore, estimation of JVP is an important component of assessing the DHF patient.
The presence of edema can aid in the assessment of the HF patient. Edema is generally associated with a high RAP. When evaluating for peripheral edema, it is important to examine the lower extremities and the sacrum because edema may redistribute to this dependent area with bed rest. However, it is poorly sensitive and can be misleading, given volume redistribution during treatment. Nevertheless, an accurate and consistent examination of the lower extremities and sacrum can aid in determining effect and length of diuresis in the DHF patient.
The third heart sound (S3) coincides with rapid ventricular filling during early diastole; it is generally due to high left-sided pressure. While it is one of the more sensitive markers of elevated filling pressures [4, 5] some studies have noted poor specificities [10]. The auscultation of an S3 requires a careful examination and quiet surroundings, making it difficult to detect. The presence of an S3 should guide the clinician to suspect a congested patient.
The presence of rales is commonly associated with volume overload. Although Butman et al. [4] found the absence of rales on auscultation ruled out a measured PCWP above 18 mmHg, and others have determined its presence to have a positive predictive value of 87% in identifying patients with PCWP above 20 mmHg [5], this physical finding is best considered nonspecific because it may be due to other conditions. Despite the above data, it should still be regarded as insensitive because patients with high filling pressures may have clear lung fields.
Although rarely utilized, assessment of blood pressure in response to a Valsalva maneuver also has been shown to correspond to invasively measured filling pressure in stable patients [15] as well as those with clinical HF [16]. Therefore, the cardiovascular response to the Valsalva maneuver is a potentially useful addition to initial physical in determining the volume status of HF patients.
This can be accomplished by locking the sphygmomanometer 15 mmHg above the supine systolic pressure, at which point the patient is asked to strain typical of a Valsalva maneuver. A normal response is divided into four phases. In Phase 1, systolic blood pressure should immediately rise 30–40 mmHg caused by an acute increase in intrathoracic pressures, and as such, Korotkoff sounds will become audible once again. As strain continues and venous return decreases, the systolic pressure will drop below the baseline. Phase 2 is manifested by this disappearance of the Korotkoff sounds. Once the strain is released, Phase 3, there is a further drop in the systolic pressure due to an acute reduction of the intrathoracic pressure. In Phase 4, there is an overshoot of systolic pressures above the baseline due to increased venous return. In patients with HF, the initial three phases are normal, but Phase 4 is absent. In patients with more severe HF, the initial increase in systolic pressure remains through the entire strain period and returns to baseline after release in Phase 3, causing the so-called square wave pattern [15–18]. These differences in HF patients are due to maintenance of LV end-diastolic volume during strain such that stroke volume remains unchanged as preload is preserved, whereas in normal patients, both LV end-diastolic pressure and stroke volume significantly decrease. Therefore, in HF patients, despite a decrease in systemic venous return, left-sided filling remains adequate [17]. This can aid in differentiation of volume status, as it is an increase in central blood volume that drives the above mechanisms.
Laboratory and Radiographic Assessment
Natriuretic peptides (NPs), such as B-type natriuretic peptide (BNP) and N-terminal pro-BNP (NT-pro-BNP), are secreted from the ventricle in response to increased volume loading and wall stress. Although increased levels of NPs are nonspecific as they may be related to any form of cardiac stress and elevated in cases of sepsis, renal insufficiency, and active pulmonary conditions, they have been shown to be of utility in the diagnosis of DHF [19] as well as improving triage and reducing length of stay in patients presenting to the emergency department with dyspnea [20]. More precisely, a BNP of less than 100 pg/mL makes a diagnosis of HF very improbable (2%), while a level of 100–400 pg/mL correlates to a probable HF diagnosis (75%), and a level above 400 pg/mL makes a HF diagnosis very probable (95%) with a specificity exceeding 90% [21••]. When defining similar cut-points for NT-pro-BNP, a level below 300 pg/mL can rule out a diagnosis of HF with 99% sensitivity, while age-adjusted levels can confirm the diagnosis with an excellent overall sensitivity and good specificity, which, however, decreases with age (Table 2) [21••, 22]. However, one should keep in mind that these laboratory tests are not a complete surrogate for volume status and should be interpreted in the clinical context. This is of particular importance in the present era of rapid NP assessment.
Given the complex relationship between the cardiovascular and renal systems, which is further altered by the neurohormonal activation of HF, blood urea nitrogen (BUN) has been an area of increasing interest. A number of studies, including analysis of the Acute Decompensated Heart Failure National Registry (ADHERE) data, demonstrate that elevated levels of BUN are associated with worse outcomes in patients with HF in both the chronic and acute settings [23, 24]. This may be secondary to BUN acting as a surrogate marker of neurohormonal activation in HF [25]. However, as disproportionate elevations in BUN may also be a marker of dehydration, its use as a determinant of congestion is of less utility.
Creatinine, while it correlates to outcomes, is of limited utility as a marker of congestion. Furthermore, although renal dysfunction has been demonstrated to be an independent risk factor for adverse outcomes in HF patients, serum creatinine is not an accurate measure of renal function in this population. These limitations were underscored by a subanalysis from the ESCAPE trial that revealed baseline renal function is only weakly correlated with RAP, with no correlation found between worsening renal function and any invasively measured hemodynamic parameter [26]. Therefore, measurements of renal function are not a reliable measure of volume status by themselves. This is also important during treatment because loop diuretic administration may worsen measurements of renal function without reflecting a change in one’s volume status.
Similar to BUN, sodium levels reflect neurohormonal activation, and hyponatremia is an independent prognostic marker of increased mortality, prolonged hospital stays, and readmissions [27, 28]. In the absence of clear markers of overdiuresis and dehydration, it is of little utility in determining volume status. Hypernatremia is distinctly unusual in HF patients, and as such, offers little for volume assessment.
Chest Radiography
Imaging to evaluate for signs of pulmonary congestion can be a useful aid in determining volume status in the DHF patient and should be obtained routinely. Signs such as vascular redistribution and interstitial edema, while reasonably specific, are relatively insensitive (Table 1), and therefore must be interpreted appropriately.
Beyond vascular redistribution and interstitial edema, the chest radiography may hold additional information useful for patients with HF. Cardiac enlargement is associated with adverse outcomes, and cardiac size can be estimated from a chest film. One such method to assess cardiac enlargement is the cardiothoracic ratio (CTR), which relates the size of the heart as a proportion of the thoracic diameter. Many have suggested that CTR would correspond well to LV ejection fraction (LVEF), and therefore, may be a surrogate marker for systolic dysfunction. This was examined with data from the Digitalis Investigation Group, and a very weak negative correlation was seen between CTR and LVEF (r = −0.176) [29]. Furthermore, no reliable cut-point for CTR could be determined to differentiate between normal and non-normal LVEF. This confirms data from earlier, smaller studies. Therefore, CTR should not be used to determine if a patient’s symptoms are due to HF and is not of utility in volume assessment.
Congestion Scoring
It is clear that there are a number of determinants of volume status that can be utilized in the DHF patient, each with a range of diagnostic accuracies. As such, they should be interpreted within the entire clinical picture. It may be of some utility, however, to objectively score the degree of congestion present. The European Society of Cardiology (ESC) has recently proposed such a congestion scoring system (Table 3) [30••]. This system takes into account elements from the history and physical, as well as laboratory data and response to dynamic maneuvers, such as blood pressure response to Valsalva, to grade congestion from none to severe. In addition to aiding in the determination of volume status, this may help guide both the nature and length of therapy, as well as help determine appropriateness for discharge. Systems such as this should prove to be clinically useful; however, research to validate their efficacy and impact on important outcomes is necessary.
Objective Hemodynamic Assessment
Objective measures of filling pressures may be needed on occasion, particular when the clinical assessment presents a mixed picture. While the standard of any such assessment is invasive right heart catheterization (RHC), noninvasive techniques can be of great utility.
Echocardiography
A number of hemodynamic parameters have echocardiographic correlates that can be utilized in the assessment of the HF patient, with certain limitations (Table 4) [31•].
Utilization of inferior vena cava (IVC) diameter and its response to respirations have long been an echocardiographic technique to estimate RAP. In euvolemic patients, IVC diameter should measure 1.5–2.5 cm and decrease by more than 50% with inspiration. The lack of inspiratory IVC narrowing by over 50% predicts a RAP above 10 mmHg on invasive measurement with a sensitivity of 87% and specificity of 82% [32]. Greater amounts of IVC dilation with lack of an inspiratory response indicate increasing levels of RAP. It should be noted that these relationships are not well preserved in ventilated patients, but a small, collapsing IVC excludes elevated RAP [33].
Using tricuspid regurgitant velocities to estimate right ventricular systolic pressures and pulmonary pressures is a longstanding echocardiographic technique with excellent correlation to invasive hemodynamic measurements (r = 0.97) [34] and a great deal of normative data [35]. Similar Bernoulli principles have been applied to Doppler of the pulmonic valve to determine pulmonary artery diastolic pressures.
Using tissue Doppler, transmitral velocities (E/Ea) have been shown to correlate well with PCWP in patients with preserved as well as depressed LVEF (r = 0.87) with a E/Ea ratio above 10 predicting a PCWP above 15 mmHg with 97% sensitivity and 78% specificity [36].
Echocardiographic techniques also can be utilized to estimate pulmonary vascular resistance (PVR) in Woods units (WU) with excellent correlation (r = 0.93) with invasive measurements. This can be done by taking the ratio of peak tricuspid regurgitant velocity (VTR) in meters per second to the right ventricular outflow tract velocity-time integral (RVOT VTI) in centimeters and applying the following equation [37]:
For example, if VTR is measured to be 3.0 m per second and the RVOT VTI is calculated as 25 cm, then PVR = 10 (3.0/25) + 0.16 = 1.36WU.
Handheld Echocardiography
The utility of echocardiographic hemodynamic assessments are somewhat blunted by the expense, time, and limited portability of traditional imaging devices. This can be improved with the use of handheld echocardiography, a technology undergoing rapid development. The use of such handheld devices to evaluate IVC diameter, and thus estimate RAP, has been demonstrated to have greatly improved diagnostic accuracy compared to physical examination when performed by internal medicine residents [38]. Elevated RAP on handheld devices also has been shown to correlate with abnormal PCWP with diagnostic accuracy of 81% in patients with acute DHF [39]. This technique also can be utilized as an aid in discharge management because the use of hemodynamic parameters by handheld devices can predict readmissions for DHF [40], probably related to poor volume management. More advanced units with traditional as well as tissue Doppler technology have demonstrated that both IVC parameters and mitral E/E’ to have good diagnostic accuracy (80%) in estimating PCWP in patients referred for RHC due to symptoms of congestion, outperforming both JVP and a clinical congestion scoring system [41]. In all of the above studies, only minimal training was given to those operating the handheld devices. As this technology continues to improve and becomes more accessible and less expensive, it may prove to be a useful clinical aid in determining the volume status in DHF patients, but more experience is needed.
Invasive Hemodynamic Assessment
While the above techniques have clear utility in the hemodynamic assessment of HF patients, the standard of any such assessment is RHC. Even with direct measurement, sources of error and artifact exist and should be taken into consideration when obtaining or interpreting RHC data. Care must be taken when flushing the catheter and manifold to eliminate any bubbles because they may cause excessive dampening of the pressure wave form. Catheter tip motion also may produce variations in pressures, and similar superimposed waves may be caused by contact with the vessel wall. Error in pressure measurement due to an improper zero reference is common. Zeroing at the same level and maintenance of transducer and patient position are important for accurate pressure determinations. Pressures should be recorded at end-expiration when the pleural pressure surrounding the heart is closest to atmospheric pressure. Increases in positive end-expiratory pressure will likely increase pleural pressures as well and reduce the reliability of invasive measurements. This is usually manifested by a slight overestimation of pressures.
Cardiac output determinations, either with Fick’s principle or thermodilution, also have potential sources of error. This would include improper collection of the mixed venous blood sample or, in the case of thermodilution, fluctuations in the baseline temperature of blood and warming of injectate by the operator’s hands. It also should be noted that in the presence of tricuspid regurgitation, the thermodilution technique of determining cardiac output is inaccurate, with results that are lower than the actual value [42]. In either case, hemodynamics must be carefully measured and interpreted in the same fashion. Continuous invasive monitoring can be of utility in certain patients, and will be discussed below.
Treatment
Hemodynamic Profiles
As detailed above, a targeted history and physical examination is crucial to determining the degree of congestion. Furthermore, that information can be incorporated into the classic model first proposed by Stevenson [43], which allows for a bedside determination of the hemodynamic profile. Initial therapeutic strategies should be based upon this assessment and profile. This exercise will divide patients as to whether they are “wet” or “dry” based on evidence of congestion (eg, orthopnea, JVD, edema, and ascites), as well as whether they have signs of poor perfusion (eg, narrow pulse pressure, cold extremities, and poor mentation [ie, are they “warm” or “cold”]). Patients who are “wet and warm” will generally respond well to diuresis and afterload reduction. Patients who are “cold and wet,” however, may need inotropic therapy to enhance response to diuresis. This group of patients may benefit from a tailored therapeutic approach with invasive hemodynamic monitoring. Patients who are “cold and dry” are typically asymptomatic at rest, but have very poor exercise capacity and may need long-term inotropic support or more advanced mechanical and surgical therapies. Furthermore, not only are treatment strategies dependent on the hemodynamic assessment of the patient, these profiles can predict outcomes in HF [44], and care must be given to this evaluation, which is crucial to appropriate volume management.
As stated earlier, the treatment of DHF should be guided by a patient-specific hemodynamic assessment, whether done clinically alone or based on objective parameters. In general, however, most admissions for DHF are due to symptoms of congestion, and most of these patients will be “warm and wet.” While these patients usually respond well to diuresis and afterload reduction, the actual treatment strategies for accomplishing improvement of congestion can vary.
Re-establishment of Euvolemia
A complete discussion of how to improve volume status is beyond the scope of this paper; however, the mainstay of treatment of volume reduction in DHF patients is loop diuretics. The question of the best regimen has been an area of some debate. Recently, the Diuretic Optimization Strategies Evaluation (DOSE) trial examined bolus administration of furosemide to continuous infusion both in low (equivalent to oral) or high (2.5x oral) doses. No differences were noted between bolus and continuous delivery of the diuretic; however, within the continuous infusion group, those patients in the high-dose arm had greater weight loss, improved symptoms, and a more marked decrease in biomarkers of HF. This was at the cost of worse renal function, which normalized with time [45•].
An emerging method for decongestion is ultrafiltration. This was demonstrated to be a safe alternative to intravenous diuretics in the Ultrafiltration Versus Intravenous Diuretics for Patients Hospitalized for Acute Decompensated Heart Failure (UNLOAD) trial. Furthermore, ultrafiltration produced greater weight and net fluid loss when compared to traditional therapy. Interesting, it was also associated with significantly lower health care resource utilization at 90 days, possibly secondary to the benefits of reduced neurohormonal activation with less diuretic exposure [46].
Tailored Therapy
There has always been a desire to have a more patient-specific methodology in treating DHF. This has led to a concept of “tailored therapy,” which utilizes objective hemodynamic parameters obtained via invasive measurements as goals of therapy in individual patients. Earlier experiences with such an approach suggested that it was safe and provided greater reductions in filling pressures during initial hospitalization as well as greater freedom from congestion postdischarge [43]. More recently, this approach was re-examined to specifically address the question of tailored therapy with indwelling pulmonary artery catheters (PAC) during HF admissions in the ESCAPE trial. This strategy was not shown to provide benefit for survival or future hospitalizations when compared to clinical assessment alone [47]. It should be noted that highly skilled HF cardiologists performed the clinical assessment in the ESCAPE trial. This may have blunted any potential benefits derived from PAC use. In a subsequent trial of tailored therapy utilizing echocardiographic hemodynamic parameters, however, a lower rate of hospitalization and improvement in self-assessed symptoms were noted at 1 year [48]. These data suggest that while utilizing an indwelling PAC for extended periods of time to guide therapy may not be helpful, targeting of some objective measure of filling pressures and degree of congestion may be a useful adjunct to clinical assessment alone. This is particularly the case when there is no improvement or deterioration in a patient’s clinical picture while following a thoughtful treatment strategy based on a carefully derived hemodynamic profile. This scenario was further described in a recent study, in which RHC was performed in consecutive patients undergoing transplantation evaluation. A discordance between right- and left-sided filling pressures was seen in more than 1 in 3 patients [49]. In this subset of patients, obtaining objective hemodynamic data is often crucial to determining the most appropriate treatment strategy.
Duration of Treatment and Assessment of Discharge Appropriateness
Volume assessment and management are extremely important for proper management of the DHF patient. However, other reasons for admission such as ischemia or arrhythmia, or other etiologies of decompensation must be recognized and addressed. Furthermore, care should be taken to document improvement in physical findings of congestion, objective weight loss, and patient-reported symptoms. It should be noted that this assessment, in conjunction with an objective hemodynamic assessment, should drive therapy as opposed to changes in renal function or hemoconcentration. This point is underscored by the DOSE trial, which demonstrated benefits of more aggressive diuresis despite transient renal dysfunction, as well as a substudy of the ESCAPE trial, which revealed that while more aggressive therapy was associated with hemoconcentration and deterioration in renal function, it resulted in lower short-term mortality [50].
Additionally, there are certain prognostic markers that can predict future adverse events, including rehospitalization, that should be considered before discharge as described above. Most importantly this would include a decrease in NP levels by over 30% from admission, absolute BNP level lower than 350 pg/mL, or NT pro-BNP lower than 4000 pg/mL. Therefore, NPs should be a part of any discharge parameters.
Conclusions
The ability to accurately assess volume status in DHF patients is important in determining the degree of decompensation and the most appropriate treatment. Any assessment must include at minimum a targeted history and physical, chest radiography, and laboratory evaluation. Objective hemodynamic assessment, either by one-time RHC or echocardiography, can be of great utility in more clearly defining the clinical picture, especially when patients are not responding well, as well as helping to guide specifics of therapy. Both the initial assessment, as well as that performed to determine discharge appropriateness, must weigh multiple variables in the clinical context of the individual patient. In the future, more precise and novel biomarkers as well as improved and more portable ultrasound technology will likely play a role in optimizing volume assessment in HF patients.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Lloyd-Jones D, Adams RJ, Brown TM, et al. Heart disease and stroke statistics--2010 update: a report from the American Heart Association. Circulation. 121(7):e46–e215. doi:10.1161/CIRCULATIONAHA.109.192667.
Adams Jr KF, Fonarow GC, Emerman CL, et al. Characteristics and outcomes of patients hospitalized for heart failure in the United States: rationale, design, and preliminary observations from the first 100,000 cases in the Acute Decompensated Heart Failure National Registry (ADHERE). Am Heart J. 2005;149(2):209–16. doi:10.1016/j.ahj.2004.08.005.
Fonarow GC, Heywood JT, Heidenreich PA, et al. Temporal trends in clinical characteristics, treatments, and outcomes for heart failure hospitalizations, 2002 to 2004: findings from Acute Decompensated Heart Failure National Registry (ADHERE). Am Heart J. 2007;153(6):1021–8. doi:10.1016/j.ahj.2007.03.012.
Butman SM, Ewy GA, Standen JR, et al. Bedside cardiovascular examination in patients with severe chronic heart failure: importance of rest or inducible jugular venous distension. J Am Coll Cardiol. 1993;22(4):968–74.
Chakko S, Woska D, Martinez H, et al. Clinical, radiographic, and hemodynamic correlations in chronic congestive heart failure: conflicting results may lead to inappropriate care. Am J Med. 1991;90(3):353–9.
Wang CS, FitzGerald JM, Schulzer M, et al. Does this dyspneic patient in the emergency department have congestive heart failure? JAMA. 2005;294(15):1944–56. doi:10.1001/jama.294.15.1944.
Fonarow GC, Abraham WT, Albert NM, et al. Organized program to initiate lifesaving treatment in hospitalized patients with heart failure (OPTIMIZE-HF): rationale and design. Am Heart J. 2004;148(1):43–51. doi:10.1016/j.ahj.2004.03.004.
Pang PS, Cleland JG, Teerlink JR, et al. A proposal to standardize dyspnoea measurement in clinical trials of acute heart failure syndromes: the need for a uniform approach. Eur Heart J. 2008;29(6):816–24. doi:10.1093/eurheartj/ehn048.
Drazner MH, Hellkamp AS, Leier CV, et al. Value of clinician assessment of hemodynamics in advanced heart failure: the ESCAPE trial. Circ Heart Fail. 2008;1(3):170–7. doi:10.1161/CIRCHEARTFAILURE.108.769778.
Stevenson LW, Perloff JK. The limited reliability of physical signs for estimating hemodynamics in chronic heart failure. JAMA. 1989;261(6):884–8.
Beck da Silva L, Mielniczuk L, Laberge M, et al. Persistent orthopnea and the prognosis of patients in the heart failure clinic. Congest Heart Fail. 2004;10(4):177–80.
Vinayak AG, Levitt J, Gehlbach B, et al. Usefulness of the external jugular vein examination in detecting abnormal central venous pressure in critically ill patients. Arch Intern Med. 2006;166(19):2132–7. doi:10.1001/archinte.166.19.2132.
Drazner MH, Hamilton MA, Fonarow G, et al. Relationship between right and left-sided filling pressures in 1000 patients with advanced heart failure. J Heart Lung Transplant. 1999;18(11):1126–32.
Badgett RG, Lucey CR, Mulrow CD. Can the clinical examination diagnose left-sided heart failure in adults? JAMA. 1997;277(21):1712–9.
Weilenmann D, Rickli H, Follath F, et al. Noninvasive evaluation of pulmonary capillary wedge pressure by BP response to the Valsalva maneuver. Chest. 2002;122(1):140–5.
Felker GM, Cuculich PS, Gheorghiade M. The Valsalva maneuver: a bedside "biomarker" for heart failure. Am J Med. 2006;119(2):117–22. doi:10.1016/j.amjmed.2005.06.059.
Little WC, Barr WK, Crawford MH. Altered effect of the Valsalva maneuver on left ventricular volume in patients with cardiomyopathy. Circulation. 1985;71(2):227–33.
Zema MJ, Restivo B, Sos T, et al. Left ventricular dysfunction–bedside Valsalva manoeuvre. Br Heart J. 1980;44(5):560–9.
Worster A, Balion CM, Hill SA, et al. Diagnostic accuracy of BNP and NT-proBNP in patients presenting to acute care settings with dyspnea: a systematic review. Clin Biochem. 2008;41(4–5):250–9. doi:10.1016/j.clinbiochem.2007.08.008.
Lam LL, Cameron PA, Schneider HG, et al. Meta-analysis: effect of B-type natriuretic peptide testing on clinical outcomes in patients with acute dyspnea in the emergency setting. Ann Intern Med. 153(11):728–35. doi:10.1059/0003-4819-153-11-201012070-00006.
•• Maisel A, Mueller C, Adams Jr K, et al. State of the art: using natriuretic peptide levels in clinical practice. Eur J Heart Fail. 2008;10(9):824–39. doi:10.1016/j.ejheart.2008.07.014. This review provides guidelines on how to interpret natriuretic peptides in various inpatient and outpatient settings and how they may affect treatment strategies.
Januzzi Jr JL, Camargo CA, Anwaruddin S, et al. The N-terminal Pro-BNP investigation of dyspnea in the emergency department (PRIDE) study. Am J Cardiol. 2005;95(8):948–54. doi:10.1016/j.amjcard.2004.12.032.
Dries DL, Exner DV, Domanski MJ, et al. The prognostic implications of renal insufficiency in asymptomatic and symptomatic patients with left ventricular systolic dysfunction. J Am Coll Cardiol. 2000;35(3):681–9.
Fonarow GC, Adams Jr KF, Abraham WT, et al. Risk stratification for in-hospital mortality in acutely decompensated heart failure: classification and regression tree analysis. JAMA. 2005;293(5):572–80. doi:10.1001/jama.293.5.572.
Kazory A. Emergence of blood urea nitrogen as a biomarker of neurohormonal activation in heart failure. Am J Cardiol. 106(5):694–700. doi:10.1016/j.amjcard.2010.04.024.
Nohria A, Hasselblad V, Stebbins A, et al. Cardiorenal interactions: insights from the ESCAPE trial. J Am Coll Cardiol. 2008;51(13):1268–74. doi:10.1016/j.jacc.2007.08.072.
Gheorghiade M, Abraham WT, Albert NM, et al. Relationship between admission serum sodium concentration and clinical outcomes in patients hospitalized for heart failure: an analysis from the OPTIMIZE-HF registry. Eur Heart J. 2007;28(8):980–8. doi:10.1093/eurheartj/ehl542.
Klein L, O'Connor CM, Leimberger JD, et al. Lower serum sodium is associated with increased short-term mortality in hospitalized patients with worsening heart failure: results from the Outcomes of a Prospective Trial of Intravenous Milrinone for Exacerbations of Chronic Heart Failure (OPTIME-CHF) study. Circulation. 2005;111(19):2454–60. doi:10.1161/01.CIR.0000165065.82609.3D.
Philbin EF, Garg R, Danisa K, et al. The relationship between cardiothoracic ratio and left ventricular ejection fraction in congestive heart failure. Digitalis Investigation Group. Arch Intern Med. 1998;158(5):501–6.
•• Gheorghiade M, Follath F, Ponikowski P, et al. Assessing and grading congestion in acute heart failure: a scientific statement from the acute heart failure committee of the heart failure association of the European Society of Cardiology and endorsed by the European Society of Intensive Care Medicine. Eur J Heart Fail. 2010;12(5):423–33. doi:10.1093/eurjhf/hfq045. This article provides a detailed description of an objective congestion score, which may aid in the management of patients with heart failure.
• Abraham J, Abraham TP. The role of echocardiography in hemodynamic assessment in heart failure. Heart Fail Clin. 2009;5(2):191–208. doi:10.1016/j.hfc.2008.11.002. This review provides detailed information on the acquisition, interpretation, and supporting evidence of various echocardiographic measures of hemodynamics in heart failure.
Kircher BJ, Himelman RB, Schiller NB. Noninvasive estimation of right atrial pressure from the inspiratory collapse of the inferior vena cava. Am J Cardiol. 1990;66(4):493–6.
Lang RM, Bierig M, Devereux RB, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18(12):1440–63. doi:10.1016/j.echo.2005.10.005.
Berger M, Haimowitz A, Van Tosh A, et al. Quantitative assessment of pulmonary hypertension in patients with tricuspid regurgitation using continuous wave Doppler ultrasound. J Am Coll Cardiol. 1985;6(2):359–65.
McQuillan BM, Picard MH, Leavitt M, Weyman AE. Clinical correlates and reference intervals for pulmonary artery systolic pressure among echocardiographically normal subjects. Circulation. 2001;104(23):2797–802.
Nagueh SF, Middleton KJ, Kopelen HA, et al. Doppler tissue imaging: a noninvasive technique for evaluation of left ventricular relaxation and estimation of filling pressures. J Am Coll Cardiol. 1997;30(6):1527–33.
Abbas AE, Fortuin FD, Schiller NB, et al. A simple method for noninvasive estimation of pulmonary vascular resistance. J Am Coll Cardiol. 2003;41(6):1021–7.
Brennan JM, Blair JE, Goonewardena S, et al. A comparison by medicine residents of physical examination versus hand-carried ultrasound for estimation of right atrial pressure. Am J Cardiol. 2007;99(11):1614–6. doi:10.1016/j.amjcard.2007.01.037.
Blair JE, Brennan JM, Goonewardena SN, et al. Usefulness of hand-carried ultrasound to predict elevated left ventricular filling pressure. Am J Cardiol. 2009;103(2):246–7. doi:10.1016/j.amjcard.2008.08.061.
Goonewardena SN, Gemignani A, Ronan A, et al. Comparison of hand-carried ultrasound assessment of the inferior vena cava and N-terminal pro-brain natriuretic peptide for predicting readmission after hospitalization for acute decompensated heart failure. JACC Cardiovasc Imaging. 2008;1(5):595–601. doi:10.1016/j.jcmg.2008.06.005.
Goonewardena SN, Blair JE, Manuchehry A, et al. Use of hand carried ultrasound, B-type natriuretic peptide, and clinical assessment in identifying abnormal left ventricular filling pressures in patients referred for right heart catheterization. J Card Fail. 16(1):69–75. doi:10.1016/j.cardfail.2009.08.004.
Cigarroa RG, Lange RA, Williams RH, et al. Underestimation of cardiac output by thermodilution in patients with tricuspid regurgitation. Am J Med. 1989;86(4):417–20.
Stevenson LW. Tailored therapy to hemodynamic goals for advanced heart failure. Eur J Heart Fail. 1999;1(3):251–7.
Nohria A, Tsang SW, Fang JC, et al. Clinical assessment identifies hemodynamic profiles that predict outcomes in patients admitted with heart failure. J Am Coll Cardiol. 2003;41(10):1797–804.
• Felker GM, Lee KL, Bull DA, et al. Diuretic strategies in patients with acute decompensated heart failure. N Engl J Med. 364(9):797–805. doi:10.1056/NEJMoa1005419. This trial demonstrated that bolus and continuous infusion diuretic therapies were no different in regards to improvement in patient symptoms.
Costanzo MR, Guglin ME, Saltzberg MT, et al. Ultrafiltration versus intravenous diuretics for patients hospitalized for acute decompensated heart failure. J Am Coll Cardiol. 2007;49(6):675–83. doi:10.1016/j.jacc.2006.07.073.
Binanay C, Califf RM, Hasselblad V, et al. Evaluation study of congestive heart failure and pulmonary artery catheterization effectiveness: the ESCAPE trial. JAMA. 2005;294(13):1625–33. doi:10.1001/jama.294.13.1625.
Rohde LE, Palombini DV, Polanczyk CA, et al. A hemodynamically oriented echocardiography-based strategy in the treatment of congestive heart failure. J Card Fail. 2007;13(8):618–25. doi:10.1016/j.cardfail.2007.05.003.
Campbell P, Drazner MH, Kato M, et al. Mismatch of right- and left-sided filling pressures in chronic heart failure. J Card Fail. 17(7):561–8. doi:10.1016/j.cardfail.2011.02.013.
Testani JM, Chen J, McCauley BD, et al. Potential effects of aggressive decongestion during the treatment of decompensated heart failure on renal function and survival. Circulation. 122(3):265–72. doi:10.1161/CIRCULATIONAHA.109.933275.
Disclosures
No potential conflicts of interest relevant to this article were reported.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ahmed, M., Hill, J. A Rational Approach to Assess Volume Status in Patients with Decompensated Heart Failure. Curr Heart Fail Rep 9, 139–147 (2012). https://doi.org/10.1007/s11897-012-0084-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11897-012-0084-x