Abstract
The relationship between law enforcement and those with mental illness is severely strained and possibly even broken. But who caused this rift in the relationship? Is law enforcement to blame? Are those with a mental illness to blame? Or, does the issue stem from a bigger problem of deinstitutionalization and negative stigmas that society has against both mentioned populations? The purpose of this study was to dive deeper into the relationship between law enforcement officers and those with mental illness to seek the root cause of the disconnect, as well as what can be done to bridge the gap. Previous research has focused on the law enforcement perspective, focusing on what training (if any) they have for dealing with citizens with mental illnesses as well as how those in law enforcement perceive people with mental illnesses while on the job. These perceptions are yet another possible explanation of the disconnect and could potentially be part of the solution to help mend the break between law enforcement and those suffering from a mental illness. The present study sought to examine the effects that CIT training has on the response outcomes when law enforcement officers respond to those with mental illness. These response outcomes, when ranked by severity, can help to explain the importance of CIT training and its effectiveness, especially when compared to the previous studies data pool of officer perspectives. The results of this study are compelling and create an effortless opening for conversation on a topic that is difficult for many to talk about.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Mental illness, a complex and multifaceted phenomenon, prompts a critical inquiry into its definition and the role of law enforcement in addressing it. This empirical study sought to explore the capacity of law enforcement agencies to identify and assist individuals afflicted by mental illness, and the resources available for this purpose. In the context of contemporary society, it is imperative to address the burgeoning mental health crisis, particularly in the realm of interactions between law enforcement agencies and individuals with mental health conditions. This crisis underscores a substantial gap between the support individuals with mental illness require and what they currently have access to, necessitating the intervention of law enforcement officers. Regrettably, these individuals, who lack medical expertise or specialized training in mental health, often find themselves assuming the unexpected role of street corner psychiatrists.
The American Psychiatric Association (APA 2018) defines mental illness as a constellation of changes in emotions, thought processes, and behaviors, encompassing a broad spectrum of conditions, from less severe to extremely debilitating. Furthermore, mental illness, as delineated by the APA (2018), can lead to distress and impairment in various aspects of an individual’s life, including social relationships, familial dynamics, employment, and academic performance.
The prevalence of mental illness in contemporary society is a pressing concern. According to The National Alliance on Mental Illness (NAMI 2021), an estimated one in five adults and one in six youth grapples with mental health challenges annually, impacting over 20% of adults and 15% of children in the USA. NAMI (2021) also revealed that suicide ranks as the second leading cause of death among individuals aged 10 to 34. The deleterious effects of mental illness on individuals’ daily functioning often necessitate law enforcement intervention. This reality highlights the frequency with which law enforcement is summoned to respond to individuals in distress. When individuals are in imminent danger of harming themselves, the recourse frequently entails reaching out to law enforcement, as hospitals or medical professionals are not typically the first responders available to address such crises.
Law enforcement agencies are currently under intense scrutiny, obligated to conduct themselves in accordance with the expectations of the public, an ever-evolving and challenging standard. In this complex landscape, law enforcement personnel frequently encounter individuals of all age groups experiencing mental health crises. A change in an individual’s mental status can precipitate disturbances that pose risks to themselves or others, thereby compelling law enforcement to intervene. Additionally, law enforcement officers often respond to calls to ensure the safety of the firefighters, paramedics, counselors, or case managers who are assisting individuals with mental illness. These scenarios consistently place law enforcement officers in direct contact with individuals affected by a diverse array of mental health conditions, raising the pertinent question: are law enforcement officers adequately trained to safely engage with individuals suffering from mental illness? This study aims to address this critical question and provide insights into the challenges and potential solutions concerning this pressing societal issue.
Deinstitutionalization: a Historical Perspective
Deinstitutionalization, initiated in 1963 under President John F. Kennedy, was born from his personal experience with his sister, Rosemary. Her tragic experience, marked by birth complications leading to mental delays, was compounded by the stigma surrounding mental health at the time. The Kennedy family’s response to this challenge was to manage Rosemary’s condition discreetly, ultimately leading to a traumatic lobotomy, which left her incapacitated (Lenz 2017). The turning point came when Rosemary was discovered, nearly two decades later, upon her father’s passing. President Kennedy, by then in office, used his position to propose a national community mental health program, which was initially intended to span approximately 20 years (Mechanic and Rochefort 1990). However, the program’s timeline accelerated, partly due to President Kennedy’s assassination, with the allocated funds diverted to the Vietnam War (Slate 2017). This redirection had profound implications for mental health care in the USA.
The Unintended Consequences of Deinstitutionalization
Deinstitutionalization, often misunderstood, triggered a mass exodus from mental health institutions, driven by advancements in psychopharmacology, notably drugs like thorazine, which enabled previously non-functional individuals to participate in society (French 1987; Krieg 2001). However, it is crucial to acknowledge that mental health institutions served as not just treatment centers but also homes for many individuals who had no other place to stay or support systems to care for them (French 1987). The consequences of deinstitutionalization were far-reaching. In 1955, at the onset of this movement, there were approximately 559,000 residents in mental health institutions across the USA (Slate 2017). By 2017, this number had dwindled to an estimated 35,000, a staggering 94% reduction. These individuals were released without adequate resources and support, often left homeless and without consistent access to essential medications.
Challenges in Community Care Alternatives
The transition from institutional care to community-based alternatives posed significant challenges. Mechanic and Rochefort (1990) noted that these community care alternatives were often highly inadequate, leaving individuals with mental illness without the essential services they previously received while residing in institutions. This shift in approach raises parallels with the challenges faced by the prison system when reintegrating individuals into society without adequate resources and support.
Stigmas Surrounding Mental Illness and Law Enforcement
In today’s society, mental illness and law enforcement are often burdened with stigmas, partly fueled by the expansive reach of modern media. Morgan et al. (2022) highlighted how news media wrongly portray individuals with mental illness as intrinsically dangerous. Despite these stigmatizing portrayals, many individuals with mental illnesses have never exhibited violence. Negative stigmas comprise three key elements: stereotyped beliefs, emotional reactions, and behaviors. These stigmas often result in prejudiced assumptions about the dangerousness of those with mental illness, evoking emotions such as fear and anxiety. Corresponding behaviors may involve discrimination or avoidance (Morgan et al. 2022). Stigmas also permeate the law enforcement sector. Lockwood et al. (2021) revealed that officers tend to arrest individuals with mental illness more frequently and perceive them as more threatening, often experiencing fear and uncertainty when interacting with them. The limited prevalence of extreme mental illness leads to unfamiliarity, fostering misrepresentation and miscommunication. This lack of direct exposure to severe mental illness contributes to the proliferation of exaggerated, unfounded fears and misconceptions (Morgan et al. 2022). Addressing negative stigmas requires more balanced media representation. News outlets and social media platforms should shift their focus from rare and extreme incidents to reduce misperceptions. It is vital to minimize selective sharing of images and videos that may provide only partial truths, which perpetuate inaccuracies and reinforce negative stigmas (Morgan et al. 2022). Society’s collective effort can work toward minimizing these detrimental stigmas, enhancing overall understanding and safety.
How Law Enforcement Officers Assess Mental Illness
Law enforcement officers, without specialized medical training, often find themselves in situations involving individuals with mental illness. These encounters result from the fact that officers are frequently the first responders to crises involving mental illness (Goldberg et al. 2019). Despite department-regulated training, it is clear that officers are not fully equipped to handle the complexities of mental illness, hence the moniker “street corner psychiatrists.” Law enforcement agencies report that up to 15% of their annual service calls involve individuals with altered mental states (powerdms.com, 2020). This frequent exposure places officers in situations where they must assess individuals with mental illness, even though they may not possess the expertise to make accurate assessments. Furthermore, the overlap in signs and symptoms between mental illness and substance abuse poses challenges. Officers may misinterpret situations and provide inadequate responses, potentially leading to wrongful assessments, causing unnecessary stress, fear of law enforcement, and disruptions to individuals’ lives (Bohrman et al. 2018).
Department Policies and Procedures
Diverse local police departments across the USA operate with varying policies and procedures, affecting how they handle interactions with individuals with mental illness. The roots of this diversity can be traced back to deinstitutionalization, which placed the responsibility on law enforcement officers to address mental health issues (Reyes 2014). This disparity in procedures complicates efforts to standardize training and education. Training for law enforcement officers faces significant challenges, especially when considering the myriad diagnosable mental illnesses and the large number of individuals suffering from these conditions (Laan et al. 2013). Conventional police response tactics often prove ineffective and unsafe for individuals with mental illness (Laan et al. 2013). The lack of training and the perception that handling mental illness is not within their job description further exacerbate the situation. This creates a problematic cycle, especially when media coverage perpetuates the issues, worsening the relationship between law enforcement and individuals with mental illness. Overall, addressing the shortcomings in how law enforcement officers assess mental illness requires a multi-faceted approach, encompassing standardized training and improved understanding among officers, policymakers, and the public.
CIT Training
CIT training is the most common and well-known training for law enforcement in regard to mental illness. CIT—crisis intervention team—was first developed in 1988 and consists of a 40-h training course for law enforcement employees. CIT, as stated by Kubiak et al. (2017), also known as the Memphis Model, attempts to improve interactions with citizens who have a mental illness. However, according to Zelle et al. (2022), less than 17% of law enforcement jurisdictions have any CIT trained officers. If we have a model that has proven success readily available for law enforcement, why have less than 17% taken advantage of it?
CIT training has 3 elements: ongoing elements, operational elements, and sustaining elements. Dempsey (2017) stated that ongoing elements focus on the partnership between law enforcement and mental health advocacy. This takes into consideration how the two can work hand in hand to provide the best outcome for citizens who suffer from mental illness. It also considers what policies and procedures are best equipped to benefit all parties involved and keep everyone as safe as possible. The next element, according to Dempsey (2017), focuses on who needs CIT training and the curriculum that goes along with it. The CIT training is needed by police officers and dispatchers. Police officers obviously need the training because they are in the field face to face with the mentally ill citizens but why are dispatchers included? Dispatchers are included because they are technically the first person on every call. They may not be in the field but they are responsible for gathering as much information as possible to ensure the safety of the responding officers. CIT training is important for dispatchers to have so that while taking the call they can ask pertinent questions like what kind of mental illness does the person have or what things may set off the mentally ill person. Having just those two answers already puts responding officers at an advantage while on scene for safety and for success in handling the call. The final element of CIT, according to Dempsey (2017), focuses on in-service training, recognition, and outreach. This element allows law enforcement to keep up to date training on new discoveries and procedures being implemented. The sustaining element also considers that whenever an officer or dispatcher successfully uses CIT training and helps a person with mental illness, they deserve to be recognized for their efforts. If you do not recognize people for the good work they do and make them feel valued, they may not bother to put forth the effort. In this case, that potential lack of effort could be harmful to all parties involved.
CIT does not just sound good on paper, but there has been proven success from law enforcement employees who applied it. Kubiak et al. (2017) stated that CIT-trained officers who came into contact with those with mental illness were able to reduce jail time and had more success with severely mental ill citizens getting the needed help at the hospital. Jail time is sometimes the only option police have for citizens with mental illness but that does not make it a good option. Kubiak et al. (2017) also mentioned that CIT-trained officers reported having more confidence when dealing with mentally ill citizens. That confidence can go a long way, especially when considering officer and citizen safety. If officers feel more equipped to handle the situation, they will be able to utilize resources that are non-lethal and hopefully less forceful as well. This confidence and ability to avoid confrontation as much as possible further shows why CIT training is so important to law enforcement employees as well as those people with mental illness. The goal of a police department, as stated by Dempsey (2017), is to provide humane, cooperative, compassionate, and effect law enforcement to people within their community. CIT training allows for that goal to be met more easily and successfully.
Interactions Between Law Enforcement and Citizens with Mental Illness
Law enforcement officers have frequent interactions with individuals suffering from mental illness. Wood et al. (2017) reported that 90% of patrol officers encounter people with mental illness at least six times a month. The prevalence of these encounters, accounting for approximately 10% of all police interactions, raises challenges due to their time-consuming nature (Lipson et al. 2010).
Causes of Interactions
Various factors contribute to these interactions. Citizens with mental illness may request police assistance, either for legitimate reasons or simply to share their concerns. These interactions can also occur when a person’s behavior raises suspicion among others, or when family members or caretakers seek help in managing the individual. Many such interactions are for minor offenses, often non-violent, further complicating the assessment and response process (Wood et al. 2017).
Building Rapport and Breaking Stigmas
Establishing trust during these interactions is crucial. Law enforcement officers who can effectively communicate and calm individuals with mental illness can build trust, potentially benefiting future encounters (Frederick et al. 2018). This trust can challenge the negative stigmas associated with people with mental illness as dangerous, impulsive, or irrational.
Response Options for Law Enforcement
Law enforcement officers have various response options when dealing with individuals suffering from mental illness. According to Akins et al. (2016), these options include detaining and transporting the individual to a mental health facility, making an arrest, or resolving the situation informally. The choice of response remains a challenge, given the lack of consistent approaches in both law and medicine (Matthews 1970). Civil commitment to a hospital is not always straightforward. Commitment may occur voluntarily, with the individual’s consent, or involuntarily when specific criteria are met. Commitment balances community safety and the individual’s care requirements, which often involve room for interpretation (Makin et al. 2018). The result is that some individuals may end up in jail due to the strict criteria for civil commitment. Jail is often inappropriately overused as a response option. A significant portion of inmates in state prisons and local jails require mental health treatment (Constantine et al. 2012). However, this raises the question of whether alternatives, such as hospitals, outreach programs, or group homes, might be more suitable for some individuals. The phenomenon of “criminalization of the mentally ill” occurs when individuals with mental illness, even for minor crimes, are disproportionately arrested (Lamb and Weinberger 2001).The presence of “frequent fliers,” individuals who repeatedly interact with law enforcement, can be a considerable challenge. These contacts, while relatively small in number, consume significant resources and become frustrating for officers (Akins et al. 2016). Use of force, particularly its impact on interactions between law enforcement and individuals with mental illness, is a critical issue. These situations can be challenging and sometimes result in the application of force (Zelle et al. 2022). Law enforcement officers are more likely to use force when dealing with symptomatic individuals, such as those experiencing psychotic episodes, suicidal thoughts, or homicidal tendencies (Agee et al. 2019).
Differences in Use of Force and Its Causes
Differences exist in the use of force between interactions with individuals with and without mental illness. Factors contributing to this discrepancy include a reduced ability of individuals with mental illness to understand or comply with officers’ commands and a varied physiological response to pain. Drug or alcohol use, often combined with psychotropic medications, further complicates the issue, increasing the risk of injury (Rossler and Terrill 2017). Law enforcement officers require increased training and awareness to appropriately address these differences and minimize the need for extreme use of force.
Laws Related to Mental Illness
Joey’s Law
Like any other issue in today’s society, there are laws to protect people with mental illness, one of which is Joey’s Law. Joey’s Law allows people who suffer from a mental illness to have special identification, like a license plate decal, to alert approaching law enforcement of any disabilities (Lockwood et al. 2021). The idea behind this identification system is to alert approaching officers that there may be some mental health issues that could complicate or change the desired plan of response. It could also be a seat belt cover listing what mental illness the person suffers from and what triggers a response from them, like flashing lights or the sound of the siren. Giving law enforcement that advantage of foresight on how to successfully help the person with mental illness can be the difference between all parties leaving safely or someone potentially getting hurt because they did not have all the needed information. The idea behind this voluntary option for PwMI could potentially be beneficial; however, it does come with concerns as well. A mental health diagnosis, just like medical diagnosis, is often considered a very private matter. This privacy concern may lead to not as many PwMI taking advantage of the opportunity due to fear of being stigmatized before an interaction with LEO even begins.
O’Connor Standard
Another beneficial law is the O’Connor standard. The O’Connor standard states that to civilly confine a person, law enforcement must be able to prove that the person suffers from a mental illness and is a potential danger to themselves (Makin et al. 2018). This means that law enforcement cannot force a person to go to the hospital or other treatment facility without proof they have a mental illness and will potentially harm themselves if left in the public. This standard makes the job of law enforcement officers very hard because if the person cannot be left in society but does not reach the criteria of a civil commitment, then where can they go? The simple answer to that is they end up incarcerated because that becomes the safest place for them. How ironic that jail, a place known for its unfriendliness and potential danger, becomes a safe place for people suffering from mental illness.
Not Guilty by Reason of Insanity
The most well-known legal term regarding mental illness is perhaps not guilty by reason of insanity. NGRI is the term heard in crime fighting tv shows and read about in dramatized books about extreme crimes. Notice how it is not guilty by reason of insanity, rather than innocent by reason of insanity. That is because the defendant with the mental illness could have undeniably committed the crimes in question, but it does not mean that mentally they understood what they were doing or that they truly intended to do it. So, they are not guilty of intending to do the crime, or understanding the crime, and yet they still did it meaning that they are not innocent either. Due to media dramatizing everything, it would seem that everyone goes for the insanity plea; however, it is actually a very rare occurrence. Lawinfo.com (2021) found that only 1% of all court cases have a defense strategy that tries to plead insanity, and of that 1%, it is only successful roughly 26% of the time. A local yet unsuccessful example of the insanity plea is the Cleveland Strangler. He killed multiple women but could not prove that he did not know right versus wrong at trial so he was found guilty instead and received the death penalty. These three examples of legal terms specifically pertaining to those with mental illness demonstrate how law enforcement and those with a mental illness have been intertwined for some time now. Enough interactions to warrant needing specific laws and regulations set in place to help to bridge the gap of misunderstandings and attempt to keep everyone as safe as possible while abiding by the law.
Conclusion
There is still an abundance of unknowns when it comes to the relationship between law enforcement and people with mental illness. A main contributor to the disconnect between the two is the mass exodus of those with mental illness from designated institutions. When something like deinstitutionalization is allowed to occur, the stakeholders involved need to be considered and allowed time to prepare to ensure the safety and well-being of all who will be affected. In this case, the stakeholders were not given time to prepare and the act of deinstitutionalization turned law enforcement officers into street corner psychiatrists. These officers were not properly trained or prepared to handle such situations. There are laws set into place and some training available for law enforcement to try and ease the difficulties that have arisen but they are not without their faults. There is still plenty of room for improvements when it comes to law enforcement handling people with mental illness, and this need must be brought to light to get the attention it so desperately deserves.
Study
The mental health crisis in the USA is an ever growing and never-ending problem. As stated previously, the act of deinstitutionalization has forced those with mental illness out onto the streets with no assistance or protection in place to help them. Being on the streets with a lack of shelter, medical attention, and means to get by turns into an increased number of interactions with law enforcement. Consideration needs to be conveyed to the topic of mental health in regard to law enforcement response options and training. New law and regulations are a must in order to narrow the gap between what law enforcement thinks they know about metal illness and what they should know. This starts by examining what training is obligatory to adequately respond to people who are in the midst of a mental health crisis.
The purpose of this research study was to examine the call for service outcomes and determine if officers having CIT training positively affects which outcome was utilized. The data for this study comes from a Midwestern police department calls for service data for the year 2022. All information is public record and no names or personal information was included for the people with mental illness that required police response. This study examined if a CIT officer was on scene, if the officers have had prior dealings with the person who has the mental illness, and if the caller told dispatch the person needing assistance was suffering from some sort of mental illness episode. That data will then be examined to see what effects they have on call outcomes and officers using force. The possible call outcomes are arrest, mental health outreach, pink slip, or left as is and deemed okay. This study attempted to bring light to any benefits that CIT training may have in an attempt to ensure the safety of all involved in these difficult situations.
Empirical Questions
-
1.
What is the impact of CIT training for law enforcement officers on the possible outcome(s) of calls for service when dealing with PwMI?
-
(a)
Outcomes: arrest and taken to jail, pink slipped and taken to the hospital, provided with an outreach from a mental health professional, or deemed ok and left as is
-
(a)
-
2.
What impact does CIT training have on the use of force by law enforcement officers when responding to PwMI?
-
(a)
Force: use of firearm, use of taser, use of pepper spray, use of baton, or utilizing physical take down techniques
-
(a)
Hypotheses
-
1.
CIT training for law enforcement officers and prior knowledge of the PwMI has no effect on the call for service outcome or use of force.
-
2.
CIT training for law enforcement officers and prior knowledge of the PwMI improves call for service outcomes (outreach) and reduces use of force
-
3.
CIT training and prior knowledge of the PwMI hinders call for service outcomes (arrest) and increases use of force
Methodology
Design
The design for this study was a main factor comparison. This is a 2 × 2 × 2, between, non-repeated study. The independent variables are CIT training, prior dealings with the PwMI, and if the caller informed dispatch of the possible MI. For the CIT training variable, the officer who responded to the call for service either has or has not completed the required 40-h training to become CIT certified. The prior dealings with the PwMI variable required a notation to have been put on the PwMI in the computer system stating that they have some form of MI. The final variable regarding the caller informing dispatch of the MI requires it to be notated in the call for service as being stated during the phone call. The dependent variables are the response outcome and if force was used against the PwMI. The possible response outcomes for this study are the PwMI being taken to jail, the PwMI being provided with a mental health outreach from a mental health specialist, the PwMI being pink slipped and taken to the hospital for a psychiatric hold, or being deemed in an acceptable state of mind and left as is. For the use of force variable, this can include the law enforcement officer using a firearm, a taser, a baton, pepper spray, or physical takedown techniques against the PwMI. The statistical tests used for this study included a t-test and chi-square test. These tests are based on the individual scores determined from questions on the worksheets for each call for service involving a PwMI.
Materials
The materials for this research project include the agency consent form from the previous study, the incident reports for all calls involving a PwMI, worksheets for each incident report, binders to keep all reports and worksheets in, and the SPSS software for the statistical analysis to be completed.
Participants
This study was based on archival data from a Midwestern police department. The data was collected from calls for service incident reports involving a PwMI. All identifying information was removed from the incident report print outs due to confidentiality and the protection of the PwMI. The archival data included 993 calls for service that involved a PwMI from Jan 1 at 0000 h to June 30, 2022, at 2359 h.
Procedure
All calls for service were sifted through to determine if they involved a PwMI. These calls were chosen based on if the narrative stated an involved party had a mental illness, if there was a previous notation stating someone involved had a mental illness, or if the call type was listed as psychiatric situation or suicidal attempt/investigation. Once it was determined which calls for service met the parameters of the study, all identifying information was removed and the calls for service were printed. After all of the archival data had been collected, a data worksheet was completed for each incident report. The worksheet included questions regarding if a CIT officer was on scene, if any force was used against the PwMI, what the outcome of the call was, and more. Once completed, the incident reports and worksheets were put into binders until ready for statistical analysis.
Data Analysis
Once all archival data was collected and printed for analysis, a data worksheet for each incident report was filled out for easier viewing. After a data worksheet was completed for each incident involving a PwMI, the data was then transferred to numeric values and entered into an SPSS spreadsheet. The SPSS spreadsheet included the following data columns: incident number, month of incident, PwMI gender, PwMI age, PwMI race, if a weapon was present, the type of weapon present, if a CIT trained officer was on scene, if the mental illness was known due to the caller notifying the dispatcher, if the police had had prior dealings with the PwMI, use of force by the officer, the outcome of the call, and the arrest reason if applicable.
When all data sets were determined to be of optimal size through SPSS, the descriptive statistics were graphed (Table 1). Once the descriptive statistics were completed, chi-square tests were completed as well. For the chi-square, independent chi-square was run though SPSS based on the original data set at an alpha level of 0.05.
Results
Descriptive Statistics
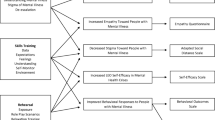
The descriptive statistics of all 6 independent variable data sets were run first. It was found that of the 994 incidents included in the data set, 459 had an officer who was CIT-trained on scene and 535 did not have an officer who was CIT-trained on scene. For the variable of MI known, meaning that the caller told the dispatcher before officers were on scene, 560 of the incidents were known and 434 of the incidents the MI was not known. For the final independent variable of the officers having prior notation of the subjects MI, 527 incidents had the prior notation and 467 of the incidents did not (Fig. 1).
Significant Finding 1
Out of the three chi-square tests that were run for this data set, all were found to be statistically significant. The first of which being CIT training v outcomes. This was found at a chi-square value of 21.257 with a significance level of < 0.001**. This significant finding indicates that the presence or lack thereof for CIT training impacts the outcome responses that the officers chose to utilize. When examining just the incidents with CIT-trained officers compared to the outcome options, 5.4% of the calls resulted in an arrest, 2.4% of the calls resulted in an outreach with a mental health professional being suggested or completed, 34.6% of the calls resulted in a mental health pink-slip, and 57.5% of the calls resulted in the PwMI being deemed okay and left as is. This suggests that CIT training helps to minimize arrest rates when compared to the utilization of pink-slipping the PwMI to get mental health treatment as well as deeming them as okay as they are.
When examining just the incidents without CIT-trained officers compared to the outcome options, 2.2% of the calls resulted in an arrest, 2.1% of the calls resulted in an outreach with a mental health professional being suggested or completed, 25% of the calls resulted in a mental health pink-slip, and 70.7% of the calls resulted in the PwMI being deemed okay and left as is. This also suggests that no CIT training helps to minimize arrest rates when compared to the utilization of pink-slipping the PwMI to get mental health treatment and deeming them as okay as they are.
Now, when comparing arrests rates between CIT-trained officers and non-CIT-trained officers, it is 67.6% compared to 32.4%. This suggests that CIT-trained officers make approximately 30% more arrests of PwMI than non-CIT-trained officers do. When comparing the outreach rates between CIT-trained officers and non-CIT-trained officers, it is equal at 50% each. When considering the utilization of pink-slipping, the PwMI between CIT-trained officers and non-CIT-trained officers is 54.3% compared to 45.7%. This suggests that CIT-trained officers pink-slip PwMI approximately 10% more than non-CIT-trained officers. When examining the final outcome of deemed okay and left as is between CIT-trained officers and non-CIT-trained officers, it is 41.1% compared to 58.9%. This suggests that CIT-trained officers are able to better determine what is best for the PwMI instead of leaving them as is with no other intervention like mental health professionals in an outreach or hospital setting (Tables 2 and 3 and Fig. 2).
Significant Finding 2
The next significant chi-square test was MI known v outcome. This was found at a chi-square value of 122.495 with a significance level of < 0.001**. This significant finding indicates that the presence or lack thereof for the caller advising dispatch of the PwMI before officers respond impacts the outcome responses that the officers chose to utilize. When examining just the incidents with MI known compared to the outcome options 1.4% of the calls resulted in an arrest, 3.4% of the calls resulted in an outreach with a mental health professional being suggested or completed, 42.1% of the calls resulted in a mental health pink-slip, and 53% of the calls resulted in the PwMI being deemed okay and left as is. This suggests that knowing about the mental illness helps to increase the PwMI being deemed okay and pink-slipped while reducing the PwMI being arrested.
When examining just the incidents without the MI being known compared to the outcome options 6.7% of the calls resulted in an arrest, 0.7% of the calls resulted in an outreach with a mental health professional being suggested or completed, 13.1% of the calls resulted in a mental health pink-slip, and 79.5% of the calls resulted in the PwMI being deemed okay and left as is. This suggests that not being told the subject is suffering from a mental illness increases the outcome of being deemed okay and left as is instead of providing PwMI with mental health professionals in an outreach or medical setting.
Now, when comparing arrest rates between MI known and MI not known, it is 21.6% compared to 78.4%. This suggests that if the officers are not told about the MI by the caller, they will make an arrest approximately 50% more than if they had known. When comparing the outreach rates between MI known and MI not known, it is 86.4% and 13.6%. This suggests that the MI known than the officers are approximately 70% more likely to request an outreach than if the MI was not known. When considering the utilization of pink-slipping the PwMI between MI known and MI not known, it is 80.5% compared to 19.5%. This suggests that if the MI is known the chance of the person being pink-slipped increases by approximately 60%. When examining the final outcome of deemed okay and left as is between MI known and MI not known, it is 46.3% and 53.7%. This is the closest comparison that was found suggesting that the MI being known does not greatly affect if the officers deem the person to be okay and left as is (Tables 4 and 5 and Fig. 3).
Significant Finding 3
The final significant chi-square test was prior v outcome. This was found at a chi-square value of 80.181 with a significance level of < 0.001**. This significant finding indicates that the presence or lack thereof for officer having notated prior dealings with the PwMI impacts the outcome responses that the officers chose to utilize. When examining just the incidents with prior notation of officers dealing with the PwMI compared to the outcome options, 6.1% of the calls resulted in an arrest, 1.9% of the calls resulted in an outreach with a mental health professional being suggested or completed, 18.2% of the calls resulted in a mental health pink-slip, and 73.8% of the calls resulted in the PwMI being deemed okay and left as is. This suggests that the officers having prior interactions and notations of the PwMI increase the likelihood of the PwMI being deemed okay and left as is while also reducing arrest rates and treatment options. When examining just the incidents without the prior notations compared to the outcome options, 1.1% of the calls resulted in an arrest, 2.6% of the calls resulted in an outreach with a mental health professional being suggested or completed, 42.2% of the calls resulted in a mental health pink-slip, and 54.2% of the calls resulted in the PwMI being deemed okay and left as is. This suggests that no prior dealings and notations also have a high deemed okay rate but are almost just as likely to pink-slip the PwMI. Now, when comparing arrest rates between prior interactions and notations and no prior interactions and notations, it is 86.5% compared to 13.5%. This suggests that prior interactions and notation significantly increase the arrest rate of the PwMI by approximately 70%. When comparing the outreach rates between prior interactions and notations and no prior interactions and notations, it is 45.5% compared to 54.5%. This suggests that prior interactions and notations only slightly differ the outreach outcome in favor of the latter. When considering the utilization of pink-slipping the PwMI between prior interactions and notations and no prior interactions and notations, it is 32.8% and 67.2%. This suggests that the lack of prior interactions and notations increases the likelihood of the PwMI being pink-slipped by roughly 30%. When examining the final outcome of deemed okay and left as is between prior interactions and notations and no prior interactions and notations, it is 60.6% compared to 39.4%. This proposes that if the officers have had prior interactions and notations with the PwMI, they are more likely to deem them as okay due to their state by roughly 30% (Tables 6 and 7 and Fig. 4).
Discussion
The purpose of this study was an attempt to discover how CIT training for law enforcement officers affects the outcomes of the calls for service in which they respond to involving PwMI. This study was consequent of a personal curiosity due to being a police dispatcher and not feeling as if there is nearly enough training when it comes to dealing with people who are suffering from a mental illness. As mentioned previously, the majority of personal confidence in doing so comes from schooling in the criminal justice and psychology fields outside of the police department. Those who are suffering from mental illness deserve the best treatment they can get. However, when the respondent is a law enforcement employee who is not equip to handle the situation nor wants to handle the situation, where does that leave people who are suffering from mental illness? This study is an attempt to stress the importance of training among law enforcement officers and improve the relationship they currently have with PwMI.
Findings
This study had statistical significance; some findings were unanticipated. For instance, when looking at the chi-square test for CIT training v outcome, it was found that the CIT-trained officers had a higher arrest rate than the non-CIT-trained officers. It was hypothesized that CIT training would help to lower the arrests rates which was determined not to be the case. Another surprising finding from the same test was that the CIT-trained officers and non-CIT-trained officers both utilized the outreach option at 50% suggesting that training does not affect it. The outreach option also had the smallest individual percentages of 2.4% for CIT-trained and 2.1% for non-CIT-trained. When considering the chi-square test for MI known v outcomes, there were no astonishing findings that were not to be expected. The chi-square test for prior v outcomes had one surprising finding. The prior interactions and notations had a higher arrest rate than the no prior interactions and arrest rates. Based on the hypothesis, it was thought that prior interactions would minimize the arrest rates due to a report that would be suspected to have formed. The final unanticipated finding was that there was no significance found when running a chi-square test for weapons v outcomes. It was hypothesized that the presence of a weapon would significantly affect the arrest rate when compared to mental health treatments and being deemed okay and left as is; however, that was found to not be the case.
Limitations
Like any research study, there are bound to be limitations. One of which for this study was that due to COVID, many training opportunities have been lost over the past few years. Due to restrictions in travel as well as contact with others, it is possible that more officers would have been fortunate enough to receive CIT training; however, they were unable to due to trainings being postponed and canceled. Another limitation is that each incident that was included in the data set was documented by multiple different people. There are set guidelines that dispatchers are supposed to follow; however, there are still minor variations in documentation that could have affected the data set, specifically the variable of if the MI was known due to what the caller said or not. A third possible limitation of this study is that if the officers did not run the PwMI on scene, meaning did not add the PwMI identifying information to the incident form, then the prior interactions and notations would not have populated which could have affected that variables’ data set. Another thing to consider as a possible limitation to this study is that officers, whether CIT-trained or not, are the ones determining if a notation is put on a subject judging them to have some form of MI. This unprofessional assessment could be deeming people who do not have a MI as having one which in turn could alter the data set.
Data Availability
Data is available upon request.
References
Agee ER, Zelle H, Kelley S, Moore SJ (2019) Marshaling administrative data to study the prevalence of mental illness in assault on law enforcement cases. Behav Sci Law 37(6):636–649. https://doi.org/10.1002/bsl.2437
Akins S, Burkhardt BC, Lanfear C (2016) Law enforcement response to “frequent fliers.” Crim Justice Policy Rev 27(1):97–114. https://doi.org/10.1177/0887403414559268
American Psychiatric Association (2018) What is mental illness?. American Psychiatric Association. Retrieved January 31, 2022 from https://www.psychiatry.org/patients-families/what-is-mental-illness
Bohrman C, Blank Wilson A, Watson A, Draine J (2018) How police officers assess for mental illnesses. Victims & Offenders 13(8):1077–1092. https://doi.org/10.1080/15564886.2018.1504844
Constantine RJ, Robst J, Andel R, Teague G (2012) The impact of mental health services on arrests of offenders with a serious mental illness. Law Hum Behav 36(3):170–176. https://doi.org/10.1037/h0093952
Dempsey C (2017) Beating mental illness: crisis intervention team training and law enforcement response trends. Southern California Interdisciplinary Law Journal 26(2):323–340
Frederick T, O’Connor C, Koziarski J (2018) Police interactions with people perceived to have a mental health problem: a critical review of frames, terminology, and definitions. Victims & Offenders 13(8):1037–1054. https://doi.org/10.1080/15564886.2018.1512024
French L (1987) Victimization of the mentally ill: an unintended consequence of deinstitutionalization. Soc Work 32(6):502–505. https://doi.org/10.1093/sw/32.6.502
Goldberg V, White C, Weisburd D (2019) Perspectives of people with mental health problems at hot spots: attitudes and perceptions of safety, crime, and the police. Behav Sci Law 37(6):650–664. https://doi.org/10.1002/bsl.2440
Krieg RG (2001) An interdisciplinary look at the deinstitutionalization of the mentally ill. Social Science Journal 38(3):367. https://doi.org/10.1016/S0362-3319(01)00136-7
Kubiak S, Comartin E, Milanovic E, Bybee D, Tillander E, Rabaut C, Bisson H, Dunn LM, Bouchard MJ, Hill T, Schneider S (2017) Countywide implementation of crisis intervention teams: multiple methods, measures and sustained outcomes. Behav Sci Law 35(5–6):456–469. https://doi.org/10.1002/bsl.2305
Laan JM, Ingram RV, Glidden MD (2013) Law enforcement training on mental disorders and autism spectrum disorders in the southeastern United States. Journal of Global Intelligence & Policy 6(10):51–67
Lamb HR, Weinberger LE (2001) Persons with severe mental illness in jails and prisons: a review. New Dir Ment Health Serv 90:29–49. https://doi.org/10.1002/yd.23320019005
LawInfo (2021) How do you prove not guilty by reason of insanity? LawInfo. Retrieved March 17, 2022 from https://www.lawinfo.com/resources/criminal-defense/not-guilty-by-reason-of-insanity.html
Lenz L (2017) The secret lobotomy of Rosemary Kennedy. Marie Claire Magazine. Retrieved April 18, 2022 from https://www.marieclaire.com/celebrity/a26261/secret-lobotomy-rosemary-kennedy/
Lipson G, Turner J, Kasper R (2010) A strategic approach to police interactions involving persons with mental illness. Journal of Police Crisis Negotiations 10(1/2):30–38. https://doi.org/10.1080/15332581003757297
Lockwood A, Lizarraga V, Kochanowski S, Mann B (2021) Stigma of mental illness: an exploration of rural law enforcement attitudes toward mental health in the heartland. J Police Crim Psychol 36(2):204–210. https://doi.org/10.1007/s11896-020-09392-0
Makin DA, Bernat FP, Lyons JA (2018) Who decides civil commitments? A statewide analysis of initial hold requests. Victims & Offenders 13(8):1171–1192. https://doi.org/10.1080/15564886.2018.1509037
Matthews AR Jr (1970) Observations on police policy and procedures for emergency detention of the mentally ill. Journal of Criminal Law, Criminology & Police Science 61(2):283–295. https://doi.org/10.2307/1142223
Mechanic D, Rochefort DA (1990) Deinstitutionalization: an appraisal of reform. Ann Rev Sociol 16(1):301–327. https://doi.org/10.1146/annurev.so.16.080190.00150
Morgan AJ, Ross AM, Wake A, Jorm AF, Kashihara J, Reavley NJ (2022) Stigmatizing and mitigating elements of a TV news report on violent crime and severe mental illness: an experiment. Stigma and Health. https://doi.org/10.1037/sah0000358
National Alliance on Mental Illness (2021) Mental health by the numbers. NAMI. Retrieved January 31, 2022 from https://www.nami.org/mhstats
PowerDMS (2020) Policing the mentally ill. PowerDMS. Retrieved January 31, 2022 from https://www.powerdms.com/policy-learning-center/policing-the-mentally-ill
Reyes G (2014) Mental illness and law enforcement: current procedures and practices. College of St. Elizabeth Journal of the Behavioral Sciences 1–7
Rossler MT, Terrill W (2017) Mental illness, police use of force, and citizen injury. Police Q 20(2):189–212. https://doi.org/10.1177/1098611116681480
Slate RN (2017) Deinstitutionalization, criminalization of mental illness, and the principle of therapeutic jurisprudence. Southern California Interdisciplinary Law Journal 26(2):341–356
Wood JD, Watson AC, Fulambarker AJ (2017) The “Gray Zone” of police work during mental health encounters. Police Q 20(1):81–105. https://doi.org/10.1177/1098611116658875
Zelle H, Kelley S, Agee ER, & Siebert WL (2022) Police use of force standards and mental health crises in the United States: identifying research and policymaking targets. International Journal of Law and Psychiatry 80. https://doi.org/10.1016/j.ijlp.2021.101750
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Boddy, K., Athaide-Victor, E., Law, FM. et al. CIT Training Among Law Enforcement: Does It Work?. J Police Crim Psych (2024). https://doi.org/10.1007/s11896-024-09660-3
Accepted:
Published:
DOI: https://doi.org/10.1007/s11896-024-09660-3