Abstract
Purpose of Review
The purpose is to make aware of the existence of the rare and exclusive small intestine (SI) diseases, namely cryptogenic multifocal ulcerating stenosing enteropathy (CMUSE) or chronic non-specific multiple ulcers of the small intestine (CNSU) and non-granulomatous ulcerating jejunoileitis (NGUJI). The article will elucidate their epidemiology, pathogenesis, clinical features, diagnosis, differentiating features and management.
Recent Findings
Recent papers have published the clinical features and diagnostic criteria of CMUSE/CNSU and NGUJI. CNSU/CMUSE is caused by gene mutations involved in the prostaglandin pathways. Although capsule endoscopy can detect these lesions, it carries a risk of retention. TNF antagonists and azathioprine have shown response in few cases.
Summary
CMUSE/CNSU and NGUJI are uncommon diseases that cause relapsing SI obstruction and bleed due to short-segment strictures and multiple shallow ulcers. This article focuses on current knowledge and novel insights regarding their pathogenesis, genetics, clinical features, diagnostic criteria and management. Multicentric clinical and genetic studies are the need of the hour.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The small intestine (SI) is known as the dark area of the gut. However, with the advent of better SI imaging, in the form of balloon enteroscopy (BE) and wireless capsule enteroscopy (CE), it has led to the diagnosis of various new diseases and clinical entities, which were not described before. The traditional diseases of the small intestine are the infective conditions (most prominent being tuberculosis), inflammatory conditions (Crohn’s disease or Behcet’s disease), malignant conditions (lymphoma/immunoproliferative small intestinal disease (IPSID)) or drug-induced (nonsteroidal anti-inflammatory drugs (NSAID)) enteropathy.
But in the last five decades, few distinct disease conditions, which cause idiopathic superficial ulcerations and stenosis of the SI, have been recognised and evaluated. These diseases, which almost exclusively affect the SI, are described as “Chronic nonspecific multiple ulcers of the small intestine (CNSU)”, “Cryptogenic multifocal ulcerous stenosing enteritis (CMUSE)”, “neuromuscular and vascular hamartoma (NMVH)”, “Chronic Enteropathy Associated With SLCO2A1 Gene (CEAS)” and “Non-granulomatous ulcerating jejuno-ileitis (NGUJI)”. The majority of these conditions present with obscure gastrointestinal (GI) bleed or intermittent small bowel obstruction. Bleed is due to shallow ulcer formation while obstructive symptoms are due to stenosis of the small bowel segments. The small bowel is involved for short segments with completely normal intervening mucosa. Some of these patients may present with features of malabsorption. Most of the conditions are either underdiagnosed or misdiagnosed. These patients have a prolonged clinical course, and the symptoms may persist for several years and decades, even after undergoing multiple surgeries. Each of the conditions will be described in detail subsequently. Clinical acumen and knowledge about these relatively unknown conditions will increase awareness, which will lead to better diagnosis and management of such cases.
CMUSE/NVMH and CNSU/CEAS
History and Epidemiology
The condition “Cryptogenic plurifocal ulcerative stenosing enteritis” was first described in France by Debray and his group in 1964 [1]. After an extensive review of the literature, it was seen that probably sixty cases have been reported worldwide. Most of the reported cases are segregated in France and Japan. This is probably because Perlemuter et al. and Matsumoto et al., who are considered the pioneers on these rather rare disease entities, are from France and Japan, respectively [2•, 3•]. In an exhaustive study spanning over three decades (1965–1995), Perlemuter et al. reported twelve patients with CMUSE who were hospitalised in France [2•]. Similarly, Matsumoto et al. in their research paper followed up fifteen cases from Japan for four decades (1965–2005) [3•]. These authors provided a thorough review of the literature and tried to explain the pathogenesis of CMUSE and also laid down the clinical and diagnostic criteria. The doctors from Japan, nevertheless, consider the term CNSU rather than CMUSE [3•]. In fact, they say that CMUSE and CNSU are slightly different clinical entities and need to be differentiated. Approximately 200 patients have been diagnosed with CNSU in Japan since its introduction by Matsumoto and his team. In recent research papers, these Japanese investigators have tried to establish the genetic basis of the disease condition by using next-generation sequencing [4••]. They found that mutations in the SLCO2A1 gene “solute carrier organic anion transporter family, member 2A1 gene, encoding a prostaglandin transporter”, which is transmitted in an autosomal recessive fashion, can lead to this condition [4••]. After this significant discovery, the Japanese doctors prefer the term “chronic enteropathy associated with the SLCO2A1 gene (CEAS)” instead of CNSU [5••]. Thus, the cases of CNSU and/or CEAS are considered to be autosomal recessive, and these are exclusively reported from Japan. A multicentric study from Japan identified 31 patients with CNSU, out of which 21 were positive for the SLCO2A1 gene mutation [5••]. Only one case of CEAS was recently described outside Japan [6].
Considerable interest has been growing in other countries as well. There were random case reports from authors, from the 1960s and 1970s, who have referred to similar disease conditions as “Stenosing small-bowel ulceration”, “Nonspecific stenosing ulceration of the small bowel” and “Chronic Stenosing Enteropathy” [7,8,9]. However, these early case reports are sporadic and difficult to evaluate as there were diagnostic limitations in those early days. Kohoutová and his team described in detail about three cases of CMUSE from a single tertiary centre at the Czech Republic. These cases were diagnosed between 1990 and 2010 and were followed up for more than a decade [10••]. In Korea, Chang et al. did a retrospective evaluation of 48 cases who had undergone double-balloon enteroscopy [BE] and found two cases of CMUSE [11]. More recently, Hwang et al. reviewed the medical records from 2000 to 2015 of seven centres of South Korea. Twenty patients, who fulfilled the diagnostic criteria of CMUSE, were described in their study [12••].
One case of refractory CMUSE has been published recently from India who was on follow-up for the past 30 years [13]. A few cases have been published from China as well [14, 15]. There is a case report from Thailand where CMUSE is described in a 10-year-old girl child who presented with a 7-year history of iron deficiency anaemia and protein-losing enteropathy [16]. Thus, the term CMUSE is slowly being recognised worldwide [17].
Few authors in the early part of the 1980s published case reports of unknown SI ulcerations and strictures and named it as “neuromuscular and vascular hamartoma (NMVH)”. This is because they found a marked proliferation of smooth muscle and nerve fibres [18]. There are few other case reports of NMVH in the same decade [19]. However, Setaffy et al. in an exhaustive review argued that these NMVH and CMUSE are two sides of the same coin, and these are different terms to explain the same disease entity [20•]. The pathological features, such as small superficial multifocal ulcers and strictures confined to the SI, non-specific inflammation confined only to the mucosa and submucosa, few vascular changes, and a chronic relapsing clinical course, were similar in the two disease entities.
Pathogenesis and Genetic Contribution
The pathogenesis of these small bowel ulcerations and stenosis is not clearly understood. This is because of the rare occurrence of the disease condition. Hence, the nomenclature “cryptogenic” is added as a prefix. In the early description of the disease, Perlemuter et al. postulated that probably there is an autoimmune mechanism at play, and an aberrant vasculitis may be the predominant pathogenic mechanism [2•]. They illustrate that a type of “atypical vasculitis” can lead to ulcer formation and stenosis. They demonstrate complement c2 deficiency in one of his patients with CMUSE and try to clarify the vasculitis theory [21]. However, other experts in the field have vehemently opposed this hypothesis [10••]. C2 deficiency is usually associated with systemic inflammation like “systemic lupus erythematosus (SLE)”, but here CMUSE/CNSU is characterised by the absence of systemic inflammation. The histology of the resected segments of the intestine or the endoscopy tissues also does not show any features suggestive of vasculitis [10••, 13]. Again, authors argue that if vasculitis is a cause of the ulcer, then it should be included under GI vasculitis such as “Churg-Strauss syndrome”, SLE, “Buerger’s disease” and “Wegener’s granulomatosis” rather than using the CMUSE/CNSU nomenclature [10••]. Furthermore, vasculitis does not explain the cause of fibrosis or stenosis in these patients.
Another school of thought is either activation of fibrogenic interleukins which leads to overstimulation of fibroblasts or defective degradation of collagen fibres [10••]. This leads to excessive fibrous tissue formation which causes strictures. However, this hypothesis fails to explain the cause of shallow ulcers and the absence of inflammatory activity.
Significant development has been done recently, where there has been an attempt to decode the genetic basis of the disease, which can lead to an explanation in the pathogenesis and pave treatment options. The genetic basis of the disease was initially suspected by a few indirect pieces of evidence. First, there are reports of family history and of segregation of CNSU cases in parents with consanguineous marriage [22, 23]. Second, the occurrence of this rare disease has been described in a couple of siblings [24, 25]. Brooke et al. first described CMUSE in a pair of siblings. When gene analysis was done, it was seen that both the siblings had “PLA2G4A” gene mutations [24]. However, in the other CMUSE siblings, reported by Zhang et al., they did not find any PLA2G4A gene mutation [25]. The third indirect evidence comes from a case report by Fraile et al., who have shown that CMUSE can occur in a patient suffering from “X-linked recessive reticulate pigmentary disorder” [26].
PLA2G4A Gene
CMUSE is now believed to be an “autosomal recessive” disease caused by mutations in the PLA2G4A gene [24, 27, 28]. The detection of “PLA2G4A gene” mutation in CMUSE patients has led to the prostaglandin and arachidonic acid hypothesis of the disease [24, 25]. The “PLA2G4A” gene encodes “cytoplasmic phospholipase A2-α” (cPLA2α), which catalyses the release of arachidonic acid from membrane phospholipids. This is likely to have reduced production of eicosanoids like prostaglandins (PGE2) and thromboxane A2. As prostaglandins are very important for the mucosal integrity of the gut, it is damaged which leads to superficial and multiple ulcer formations. There is some criticism of this theory. First, why only exclusive small bowel is involved; second, what causes fibrogenesis; and third, there are case reports of CMUSE who have normal PLA2G4A gene [5••]. The explanation is that CMUSE is a multifactorial disease, and probably some other gene or host factors may also be involved in its pathogenesis.
SLCO2A1 Gene
CNSU is a term that is exclusively described in Japan [3•, 6]. Recently, Umeno et al. looked at the genetic profile of five CNSU patients [4••]. His group identified mutations in the “solute carrier organic anion transporter family, member 2A1” (SLCO2A1) gene, encoding a “prostaglandin transporter” by whole exome sequencing. This mutation was present in four out of the five studies of CNSU patients (80%). Based on this promising result, a team of Japanese gastroenterologists who were experts in the field of small bowel enteritis sat together and formed a “CEAS ATLAS”. This group decided that the term “CNSU” is too “ambiguous”, and the term CEAS “Chronic enteropathy associated with SLCO2A1 gene mutation” was coined [5••]. This CEAS ATLAS group did a multicentric nation-wise study in Japan and identified 31 patients with CNSU, and when the genetic analysis was done, 70% of the patients had the SLCO2A1 gene mutation [5••]. In another recent study from Japan, it was shown that CEAS is genetically different from Crohn’s disease [29•]. A multicentric study on a paediatric population where out of 4 patients with CNSU, 2 were positive for the gene mutation [30]. Only one case of CEAS/CNSU, which is not from Japan, has recently been described from Korea [6].
Umeno et al. in their landmark paper also tried to explain the pathogenesis of this obscure disease from the genetic point of view [4••]. The SLCO2A1 gene encodes a prostaglandin transporter that mediates the uptake and clearance of prostaglandins. Furthermore, they showed that the SLCO2A1 mutations found in the patients caused functional impairment of “prostaglandin E2 (PGE2)” within cells. As PGE2 is known to protect the mucosa of SI against inflammatory damage, its functional impairment may lead to ulcer formation. It can also trigger a fibrogenic activity resulting in short-segment strictures. However, the exact mechanism of how the PGE2 causes ulcers and strictures and why only some demarcated areas of SI are affected is still not elucidated.
There is another rare autosomal recessive disease which is caused by the same SLCO2A1 gene mutation. This is described as “primary hypertrophic osteoarthropathy [PHO]”, where patients present with digital clubbing, periostosis and/or pachydermia [31, 32]. Even clubbing and thickened skin have been noticed in a few cases of CEAS. Thus, the Japanese team (CEAS Atlas) is quite convinced that CNSU/CEAS is a distinct autosomal recessive disease where gene mutation plays a major role in the pathogenesis [5••].
Umeno et al. also tried to bring out similarities in the pathogenesis of CMUSE, CEAS and NSAID enteropathy [4••]. This team is of the opinion that impaired prostaglandin function is the primary mechanism behind all the three disease entities and should be grouped under a “Prostaglandin associated enteropathy” [4••, 5••].
Clinical Features and Diagnostics Issues
The majority of these patients have a prolonged and protracted clinical course. These patients never fail to amaze the clinicians as most of the patients show intermittent episodes of ileus and/or GI bleed with intervening periods of normalcy which may run into decades [3•, 13]. The superficial ulcers present in the SI, especially in the jejunum and ileum are the cause of obscure GI bleed or iron deficiency anaemia. Short-segment stenosis or strictures cause intermittent obstructive symptoms most commonly manifested as pain. These ulcers and strictures are notorious to recur even after medical and surgical treatment.
Most of these patients would have undergone several diagnostic procedures, and the final diagnosis is based on collaborating all the clinical, endoscopic and histological features and ruling out other common causes of small bowel ulcerations and obstruction. The colon and stomach are classically spared in this disease. The inflammatory markers such as erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) are negative. Multiple small, shallow, superficial ulcers that may be circular or oval may be noticed during balloon enteroscopy (BE) and wireless capsule endoscopy (CE). Histology of these ulcers shows the involvement of only the mucosa or submucosa with non-specific ulcerations (hence the name CNSU). Granulomas are conspicuous by their absence. Stenosed segments are multiple, ultrashort with long intervening mucosa.
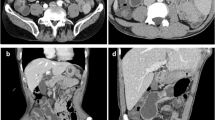
Small bowel evaluation should begin with abdominal computed tomography (CT) or CT enteroclysis followed by balloon enteroscopy. Both CE and BE are excellent diagnostic modalities to evaluate the small lesions of the SI [33,33,34,36]. While CT scan may miss some superficial ulcerations, wireless CE is the best non-invasive imaging modality to diagnose CMUSE or CNSU. Nevertheless, based on previous experiences, CE should either be contraindicated or should be used with utmost caution in a patient with suspected CMUSE as there is a high probability of capsule retention [37••]. Tao et al. have shown that around 60% of the patients have CE retention which required either surgical or endoscopic intervention [37••].
BE, on the other hand, can evaluate the superficial ulcers and stricturous segments [35, 36]. The additional advantage of obtaining histology samples makes it as the investigation of choice to assess these rare cases of small bowel ulcers and strictures. The technical issues and invasive nature of the procedure are the drawbacks associated with BE.
We need to exclude Crohn’s disease, NSAIDS enteropathy and NGUJI before we can stamp these disease entities as CMUSE or CNSU. Crohn’s disease involving the SI is very similar in presentation. However, features of systemic inflammation (inflammatory markers are classically negative), granulomas, transmural involvement in histology, fistulae and fissures and colon or esophageal or gastric involvement rule out CMUSE/CNSU and make Crohn’s disease the more likely diagnosis [23]. The superficial ulcers and short-segment strictures also closely resemble NSAIDS enteropathy or diaphragm disease [38,38,39,41]. Umeno et al. have shown that NSAIDS enteropathy and CMUSE/CNSU share the similar pathogenesis of impaired prostaglandin function. In fact, the ulcers and stenosed segments/diaphragms very closely resemble those of CMUSE/CNSU [39, 40]. Thus, a careful drug history (although some can present without any drug history as well) is a must before diagnosing CMUSE. Another differential diagnosis is NGUJI, which will be discussed subsequently. NGUJI presents with malabsorption syndrome (MAS) rather than GI bleed and is usually associated with partial or complete villous atrophy and is mostly present in adult-onset celiac disease (Table 1).
The diagnostic criteria for CMUSE/CNSU were based on previous studies [2•, 3•, 12••, 37••]:
- 1.
Unexplained small bowel strictures
- 2.
Superficial ulcer in the mucosa and submucosa
- 3.
Chronic or relapsing ulcerative stenosis and abdominal pain
- 4.
No signs of systemic inflammation
- 5.
Persistent and occult blood loss from the gastrointestinal (GI) tract except during bowel rest or postoperative period
Nevertheless, on careful analysis, these diagnostic criteria appear fallacious. The criteria are mostly based on clinical features. It cannot rule out diseases such as Crohn’s and NSAIDs enteropathy. The criteria do not stress on the endoscopic images, or the histopathological features. With the recent discovery on genetics, gene mutation should be a major diagnostic criterion. Based on the research articles on CMUSE/CNSU and CEAS, all the important diagnostic features (which include clinical data, genetic analysis, endoscopic images, histological reports) are summarized in Table 2.
Treatment
It is always difficult to treat a disease whose pathogenesis is unclear. As initially CMUSE was believed to be an “autoimmune disease” or a case of “atypical vasculitis”, treatment with steroids has been tried in almost all the reported cases [10••, 17]. The CEAS ATLAS team from Japan believes that CMUSE has a favourable response to steroid therapy while CNSU/CEAS cases do not show any response. However, on careful scrutiny, it is seen that corticosteroid therapy in the majority of cases of CMUSE has shown either mixed or disappointing results [13, 14]. The few patients, who respond to it, have a recurrence in the later course of life. Immunomodulators like 5-aminosalicylic acid (5ASA) and thiopurines have been also tried, but these drugs also do not show any promising results [23]. However, recently, an adolescent with CEAS was treated successfully with high-dose steroids and maintained successfully with azathioprine [42]. De Schepper et al. reported that anti-TNF therapy with infliximab induced remission in one patient with CMUSE [43•]. However, with the lack of robust clinical data or absence of long-term follow-up of the above-described case, infliximab cannot be recommended routinely in cases of CMUSE or CNSU.
Enteral and parental nutrition along with iron supplementation is given to most of the patients. Patients should be educated to take a non-residual diet and medium-chain triglycerides [10••, 13]. We had a good experience in treating a patient with CMUSE who had recurrent episodes of small bowel bleed despite multiple surgeries. This patient responded to hormonal therapy containing ethinyl estradiol and norethisterone [13]. This is probably because angioectasias were noted in the histological specimens of the ulcerated lesions.
Most of these patients undergo surgeries for their obstructive symptoms. However, after a symptom-free period of few years, recurrence occurs invariably, and these patients are likely to undergo multiple surgeries [10••, 13, 23].
Once the genetic basis of the disease is established, the pathogenesis can be elucidated and molecular or gene therapy can be targeted accordingly. A mutation in the gene involving PGE2 has been identified; prostaglandin therapy in form of misoprostol can be tried. However, multicentric clinical trials are required to evaluate the response of misoprostol/anti-TNF therapy/sex hormones in this rare disease. At present, treating CMUSE/CEAS can be extremely frustrating.
NGUJI: an Ulcerating Disease Associated With Celiac Disease?
During the 1960s, when CMUSE was first described, Jeffries and his team reported a similar syndrome affecting the SI. This syndrome was termed as “chronic ulcerative non-granulomatous jejunitis” that was characterised by chronic diarrhoea, weight loss and clinical features of malabsorption which were due to “multiple jejunoileal ulcerations, associated with total or subtotal villous atrophy” [44•].
Modigliani et al. tried to establish the relationship with refractory celiac disease (RCD) with these idiopathic small bowel ulcerations [45]. The authors believe that the spectrum of RCD includes ulcerative jejunoileitis and enteropathy-associated T cell lymphoma (EATL) [46].
NGUJI is an extremely rare condition. So far, a handful of cases, mostly on adult patients with RCD, have been reported in the literature [44•, 45, 46, 47,47,48,49,50,52]. Only one case of ulcerative jejunoileitis has been reported in a child with RCD [51].
Most prominent clinical features include small bowel diarrhoea and features of malabsorption. GI bleeds and episodes of ileus, which are the predominant features of CMUSE/CNSU, are rarely seen in NGUJI. The proximal SI especially jejunum and proximal ileum are commonly involved. Small bowel imaging studies are required for the diagnosis of NGUJI. Barium swallow studies and CT enteroclysis show non-specific findings. CE can beautifully demonstrate not only the ulcers but also the associated villous atrophy [52, 54]. Unlike CMUSE, no cases of capsule retention have been described. BE has the additional advantage of procuring histological samples, which shows superficial ulcers, villous atrophy and proliferation of intraepithelial mononuclear cells. Serology may be positive for celiac disease (CD).
As NGUJI is most commonly associated with CD, gluten-free diet (GFD) is tried in this disease. However, even after strict GFD, patients do not show the necessary improvement. This is probably because the disease is associated with refractory CD which does not respond to GFD. Corticosteroid and immunosuppressant therapy shows a good response. There are case reports where thiopurines and TNF antagonists have shown good response [49, 55].
The diagnostic criteria are given by Jeffries et al., way back summarises NGUJI which are [44•]:
- 1.
Typical clinical presentation with abdominal pain, diarrhoea and malabsorption
- 2.
The presence of villous atrophy, ulceration and mononuclear cell infiltrate in jejunal biopsy specimens
- 3.
Failure to induce a clinical remission on a gluten-free diet
CMUSE, NVHM, CNSU, CEAS and NGUJI: Same Disease, Different Names?
The differences and similarities of CNSU/CEAS, CMUSE and NGUJI are given in Table 2. Although the Japanese endoscopists [5••, 23] strongly believe that CMUSE and CNSU/CEAS are different entities, yet the scare shreds of evidence suggest that they actually belong to the same spectrum. After the dramatic discovery of SLCO2A1 gene mutation, the name CNSU was changed by the Japanese endoscopists to CEAS. Umeno et al. suggest that CNSU/CEAS is different from CMUSE and NSAID enteropathy, and gene analysis can differentiate the above conditions [4••, 23]. They argue that the male predominance, response to steroid therapy, and predominant involvement of the jejunum are found in CMUSE which are uncommon in CEAS. However, on a careful review of literature, males and females are equally affected, and both jejunum and ileum are affected in CMUSE. Further, a large number of cases need to be reviewed before the gender ratio and common site of involvement can be quoted. Response to steroid therapy is disappointing even in cases of CMUSE [13, 15]. The basic clinical presentation of the recurrent and prolonged clinical course of exclusive yet pleurifocal SI involvement in the form of shallow discrete ulcers and strictures is similar in both the disease condition. Hence, probably these descriptions (CNSU, CEAS, CMUSE) represent the same disease condition, and more studies especially focussing on the genetic basis can clarify. One problem with CEAS nomenclature is that how to deal with the 30% of cases that fulfil the clinical criteria for CMUSE/ CNSU, yet do not have the gene mutation [4••, 5••]. Alas, none of the reported patients with CMUSE received a genetic test for SLCO2A1 gene mutation. Hence, it is difficult to say whether CNSU/CEAS and CMUSE are different genetically. Multicentric and multinational genetic studies on this unknown disease entity are required.
As already discussed, Setaffy et al. have clarified that NVHM and CMUSE are essentially the same disease entity with similar clinical and pathological features.
NGUJI is a cause of recurrent SI ulcerations associated with villous atrophy. NGUJI, widely believed to be a type of refractory CD, appears to be different from CMUSE or CNSU. This is because the jejunum and proximal ileum are affected in a continuous manner in a celiac background. Malabsorption and chronic diarrhoea are the predominant clinical presentation. Short-segment SI stenosis is absent. The ulcers described are continuous without any skip lesions. Hence, NGUJI appears to be a disease entity different from CMUSE/CNSU.
Conclusion
Evolution of small intestine imaging especially in the form of wireless capsule endoscopy and balloon enteroscopy has opened a Pandora box of new diseases that exclusively affect the small intestine. These diseases are distinct from the inflammatory, infective or drug-induced conditions, traditionally described before, in relation to the small bowel. They are characterised by multiple superficial and sharply demarcated ulcers and multifocal short-segment stenosis. These small bowel ailments, although rare, cannot be ignored as the patients suffer for many years. However, the physician awareness about CMUSE/CNSU and NGUJI is very low. Several multicentric and multinational studies are required to evaluate these disease conditions along with the gene mutation studies. Standard textbooks and gastrointestinal (GI) societies should recognise these conditions and formulate guidelines, so that awareness can increase, and more patients can be diagnosed and treated in a systemic manner.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Debray C, Besancon F, Hardouin JP, Martin E, Marche C, Khoury K. Cryptogenetic plurifocal ulcerative stenosing enteritis. Arch Mal Appar Dig Mal Nutr. 1964;53:193–206.
• Perlemuter G, Guillevin L, Legman P, Weiss L, Couturier D, Chaussade S. Cryptogenetic multifocal ulcerous stenosing enteritis: an atypical type of vasculitis or a disease mimicking vasculitis. Gut. 2001;48:333–8. Initial paper which gives a comprehensive review and also tries to explain the pathogenesis of CMUSE.
• Matsumoto T, Iida M, Matsui T, Yao T. Chronic nonspecific multiple ulcers of the small intestine: a proposal of the entity from Japanese gastroenterologists to Western enteroscopists. Gastrointest Endosc. 2007;66(3 Suppl):S99–S107. The term CNSU is coined in Japan.
•• Umeno J, Hisamatsu T, Esaki M, Hirano A, Kubokura N, Asano K, et al. A hereditary enteropathy caused by mutations in the SLCO2A1 gene, encoding a prostaglandin transporter. PLoS Genet. 2015;11(11):e1005581. Landmark paper where the genetic basis of the disease is identified and the term CEAS is coined.
•• Hosoe N, Ohmiya N, Hirai F, Umeno J, Esaki M, Yamagami H, et al. Chronic enteropathy associated with SLCO2A1 gene [CEAS]—characterisation of an enteric disorder to be considered in the differential diagnosis of Crohn’s disease. J Crohn’s Colitis. 2017;11(10):1277–81. https://doi.org/10.1093/ecco-jcc/jjx068. Large multicentric study from Japan, where 20 patients of CEAS are described. Validates that CNSU are autosomal recessive and occur due to mutation in the SLCO2A1 gene.
Sun X, Hosoe N, Miyanaga R, Kimura K, Mizuno S, Takabayashi K, et al. A male Korean who was diagnosed with chronic enteropathy associated with SLCO2A1 (CEAS): case report with literature review. BMJ Open Gastroenterol. 2018;5:e000223. https://doi.org/10.1136/bmjgast-2018-000223.
Hopkins JE, Deaver JM. Stenosing small-bowel ulceration. Pa Med. 1966;69(8):35–9.
Lindholmer B, Nyman E, Raef L. Nonspecific stenosing ulceration of the small bowel: a preliminary report. Acta Chir Scand. 1964;128:310–1.
Rocha A, Artigas V. Stenosing ulcerous disease of the jejuno-ileum. Arch Mal Appar Dig Mal Nutr. 1959;48:1230–6 (French).
•• Kohoutová D, Bures J, Tycová V, Bártová J, Tachecí I, Rejchrt S, et al. Severe cryptogenic multifocal ulcerous stenosing enteritis. A report of three cases and review of the literature. Acta Medica (Hradec Kralove). 2010;53(53):25–9. Comprehensive review paper on CMUSE.
Chang DK, Kim JJ, Choi H, Eun CS, Han DS, Byeon JS, et al. Double balloon endoscopy in small intestinal Crohn’s disease and other inflammatory diseases such as cryptogenic multifocal ulcerous stenosing enteritis (CMUSE). Gastrointest Endosc. 2007;66(3):S96–8.
•• Hwang J, Kim JS, Kim AY, Lim JS, Kim SH, Kim MJ, et al. Cryptogenic multifocal ulcerous stenosing enteritis: radiologic features and clinical behavior. World J Gastroenterol. 2017;23:4615–23. https://doi.org/10.3748/wjg.v23.i25.4615. Recent large case series on CMUSE patients.
Singh A, Sahu MK, Panigrahi MK, Misra D. Cryptogenic multifocal ulcerous Stenosing enteritis (CMUSE): a tale of three decades. ACG Case Rep J. 2017;4:e44.
Kim CW, Yu CS, Yoon YS, Yoon SN, Lim SB, Kim JC, et al. Steroid-refractory cryptogenic multifocal ulcerous stenosing enteritis. Am J Surg. 2011;202:e48–51.
Yang Y, Zhao L, Zhang Y. A steroid-resistant cryptogenic multifocal ulcerous stenosing enteritis. Niger J Clin Pract. 2018;21:678–80.
Kijmassuwan T, Tanpowpong P, Molagool S, Treepongkaruna S. A rare cause of multiple small bowel ulcers and strictures in a 10-year-old child. Turk J Gastroenterol. 2018;29:112–5.
Freeman HJ. Multifocal stenosing ulceration of the small intestine. World J Gastroenterol. 2009;15(39):4883–5. https://doi.org/10.3748/wjg.15.4883.
Fernando SS, McGovern VJ. Neuromuscular and vascular hamartoma of small bowel. Gut. 1982;23:1008–12.
Smith CE, Filipe MI, Owen WJ. Neuromuscular and vascular hamartoma of small bowel presenting as inflammatory bowel disease. Gut. 1986;27:964–9.
• Setaffy L, Osuna MJ, Plieschnegger W, et al. Cryptogenic multifocal ulcerous stenosing enteritis (CMUSE), and neuromuscular and vascular hamartoma (NMVH): two sides of the same coin? Endoscopy. 2015;47:345–8. Elucidated that CMUSE and NMVH are similar diseases.
Perlemuter GA, Chaussade ST, Soubrane OL, Degoy AN, Louvel AN, Barbet PI, et al. Multifocal stenosing ulcerations of the small intestine revealing vasculitis associated with C2 deficiency. Gastroenterology. 1996;110(5):1628–32.
Matsumoto T, Kubokura N, Matsui T, Iida M, Yao T. Chronic nonspecific multiple ulcer of the small intestine segregates in offspring from consanguinity. J Crohns Colitis. 2011;5:559–65.
Esaki M, Umeno J, Kitazono T, Matsumoto T. Clinicopathologic features of chronic nonspecific multiple ulcers of the small intestine. Clin J Gastroenterol. 2015;8:57–62.
Brooke MA, Longhurst HJ, Plagnol V, Kirkby NS, Mitchell JA, Rüschendorf F, et al. Cryptogenic multifocal ulcerating stenosing enteritis associated with homozygous deletion mutations in cytosolic phospholipase A2-α. Gut. 2014;63:96–104. https://doi.org/10.1136/gutjnl-2012-303581.
Zhang Y, Huang L, Liu R, Wang M, Jiang Z, Zhou W, et al. Case report of a pair of siblings with cryptogenic multifocal ulcerating stenosing enteritis: a rare disease easily to be misdiagnosed as Crohn disease. Medicine. 2017;96(32).
Fraile G, Norman F, Reguero ME, Defargues V, Redondo C. Cryptogenic multifocal ulcerous stenosing enteritis (CMUSE) in a man with a diagnosis of X-linked reticulate pigmentary disorder(PDR). Scand J Gastroenterol. 2008;43:506–10.
Adler DH, Cogan JD, Phillips JA 3rd, Schnetz-Boutaud N, Milne GL, Iverson T, et al. Inherited human cPLA(2alpha) deficiency is associated with impaired eicosanoid biosynthesis, small intestinal ulceration, and platelet dysfunction. J Clin Invest. 2008;118:2121–31. https://doi.org/10.1172/JCI30473.
Umeno J, Matsumoto T, Hirano A, Fuyuno Y, Esaki M. Genetic analysis is helpful for the diagnosis of small bowel ulceration. World J Gastroenterol. 2018;24(28):3198–200 Available from: http://www.wjgnet.com/1007-9327/full/v24/i28/3198.htm. https://doi.org/10.3748/wjg.v24.i28.3198.
• Umeno J, Esaki M, Hirano A, Fuyuno Y, Ohmiya N, Yasukawa S, et al. Clinical features of chronic enteropathy associated with SLCO2A1 gene: a new entity clinically distinct from Crohn’s disease. J Gastroenterol. 2018;53(8):907–15. Recent multicentric genetic study.
Uchida K, Nakajima A, Ushijima K, Ida S, Seki Y, Kakuta F, et al. Pediatric-onset chronic nonspecific multiple ulcers of small intestine: a nationwide survey and genetic study in Japan. J Pediatr Gastroenterol Nutr. 2017;64(4):565–8.
Niizeki H, Shiohama A, Sasaki T, Seki A, Kabashima K, Otsuka A, et al. The complete type of pachydermoperiostosis: a novel nonsense mutation p. E141* of the SLCO2A1 gene. J Dermatol Sci. 2014;75(3):193–5.
Zhang Z, Xia W, He J, Zhang Z, Ke Y, Yue H, et al. Exome sequencing identifies SLCO2A1 mutations as a cause of primary hypertrophic osteoarthropathy. Am J Hum Genet. 2012 Jan 13;90(1):125–32.
Iddan G, Meron G, Glukhovsky A, Swain P. Wireless capsule endoscopy. Nature. 2000;405(6785):417.
Yamamoto H, Sekine Y, Sato Y, Higashizawa T, Miyata T, Iino S, et al. Total enteroscopy with a nonsurgical steerable double-balloon method. Gastrointest Endosc. 2001;53(2):216–20.
May A, Nachbar L, Wardak A, Yamamoto H, Ell C. Double-balloon enteroscopy: preliminary experience in patients with obscure gastrointestinal bleeding or chronic abdominal pain. Endoscopy. 2003;35(12):985–91.
Tsukahara H, Kumagai H, Yano T, Maisawa SI. A 4-year-old girl with chronic nonspecific multiple ulcers of the small intestine diagnosed by double-balloon endoscopy. Clin J Gastroenterol. 2014;7(2):144–7.
•• Tao EW, Zou TH, Wang YF, Tang JT, Chen YX, Gao QY. Case report of cryptogenic multifocal ulcerous stenosing enteritis (CMUSE): a rare disease may contribute to endoscopy-capsule retention in the small intestine. BMC Gastroenterol. 2019;19(1):49. Recent paper which suggests capsule endoscopy should be used with caution in CMSE/CNSU patients.
Chung SH, Jo Y, Ryu SR, Ahn SB, Son BK, Kim SH, et al. Diaphragm disease compared with cryptogenic multifocal ulcerous stenosing enteritis. World J Gastroenterol: WJG. 2011;17(23):2873–6.
Santolaria S, Cabezali R, Ortego J, Castiella T, Salinas JC, Lanas A. Diaphragm disease of the small bowel: a case without apparent nonsteroidal anti-inflammatory drug use. J Clin Gastroenterol. 2001;32:344–6.
Matsumoto T, Nakamura S, Esaki M, Yada S, Koga H, Yao T, et al. Endoscopic features of chronic nonspecific multiple ulcers of the small intestine: comparison with nonsteroidal anti-inflammatory drug-induced enteropathy. Dig Dis Sci. 2006;51(8):1357–63.
Matsumoto T, Iida M, Matsui T, Yao T, Watanabe H, Okabe H. Non-specific multiple ulcers of the small intestine unrelated to non-steroidal anti-inflammatory drugs. J Clin Pathol. 2004;57(11):1145–50.
Eda K, Mizuochi T, Takaki Y, Ushijima K, Umeno J, Yamashita Y. Successful azathioprine treatment in an adolescent with chronic enteropathy associated with SLCO2A1 gene: A case report. Medicine. 2018;97(41).
• De Schepper H, Macken E, Van Marck V, Spinhoven M, Pelckmans P, Moreels T. Infliximab induces remission in cryptogenic multifocal ulcerous stenosing enteritis: First case. World J Gastroenterol. 2013;19(10):1661. Promising paper which shows TNF antagonist may be helpful in CMUSE patients.
• Jeffries GH, Steinberg H, Sleisenger MH. Chronic ulcerative (non granulomatous) jejunitis. Am J Med. 1968;44:47–59. NGUJI was first described and the diagnostic criteria are laid down.
Modigliani R, Poitras P, Galian A, Messing B, Guyet-Rousset P, Libeskind M, et al. Chronic non-specific ulcerative duodenojejunoileitis: report of four cases. Gut. 1979;20(4):318–28.
Enns R, Lay T, Bridges R. Use of azathioprine for nongranulomatous ulcerative jejunoileitis. Can J Gastroenterol. 1997;11:503–6.
Freeman M, Cho SR. Nongranulomatous ulcerative jejunoileitis. Am J Gastroenterol. 1984;79:446–9.
Saxon A, Stevens RH, Ashman RF, Parker NH. Dual immune defects in nongranulomatous ulcerative jejunoileitis with hypogammaglobulinemia. Clin Immunol Immunopathol. 1977;8:272–9.
Corlin RF, Pops MA. Nongranulomatous ulcerative jejunoileitis with hypogammaglobulinemia. Clinical remission after treatment with -globulin. Gastroenterology. 1972;62:473–8.
Seven G, Assaad A, Biehl T, Kozarek RA. Use of anti tumor necrosis factor-alpha monoclonal antibody for ulcerative jejunoileitis. World J Gastroenterol: WJG. 2012;18(36):5135.
Sigman T, Nguyen VH, Costea F, Sant’Anna A, Seidman EG. Ulcerative jejunitis in a child with celiac disease. BMC Gastroenterol. 2014;14(1):29.
Moon H, Kim YS, Chung YJ, Kim KA, Kim KM, Park MJ, et al. Three cases of chronic nongranulomatous ulcerative jejunoileitis. Korean J Gastroenterol. 1999;34(3):399–405.
Kim HH, Kim YS, Ok KS, Ryu SH, Lee JH, Moon JS, et al. Chronic non-granulomatous ulcerative jejunoileitis assessed by wireless capsule endoscopy. Korean J Gastroenterol. 2010;56(6):382–6.
LePane CA, Barkin JS, Parra J, Simon T. Ulcerative jejunoileitis: a complication of celiac sprue simulating Crohn’s disease diagnosed with capsule endoscopy (PillCam). Dig Dis Sci. 2007;52:698–701.
Enns R, Lay T, Bridges R. Use of axathioprine for nongranulomatous ulcerative jejunoileitis. Can J Gastroenterol Hepatol. 1997;11(6):503–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The author declares that there is no conflict of interest.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the author have been previously published and complied with all applicable ethical standards.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Small Intestine
Rights and permissions
About this article
Cite this article
Singh, A. Cryptogenic Multifocal Ulcerating Stenosing Enteropathy(CMUSE) and/or Chronic Non-specific Multiple Ulcers of the Small Intestine(CNSU) and Non-granulomatous Ulcerating Jejunoileitis (NGUJI). Curr Gastroenterol Rep 21, 53 (2019). https://doi.org/10.1007/s11894-019-0721-6
Published:
DOI: https://doi.org/10.1007/s11894-019-0721-6