Abstract
Protein utilization and requirements in critical illness are much researched and debated topics. The enhanced turnover and catabolism of protein in the setting of critical illness is well described and multifactorial in nature. The need to preserve lean body mass and enhance nitrogen retention in this state to improve immunologic function and reduce morbidity is well described. Debates as to the optimum amount of protein to provide in such states still exist, and a significant amount of research has contributed to our understanding of not only how much protein to supply to these patients, but how best to do so. Small peptide formulations, intact protein formulations, branched chain amino acids, and specialty formulas all exist, and their benefits, drawbacks, and potential uses have been investigated. Specific amino acid therapy has become part of the concept of immunonutrition, or the modification and enhancement of the immune response with specific nutrients. In this article, we describe the changes in outcomes demonstrated through the provision of protein, both as a macronutrient and as specific amino acids.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The metabolic response to stress has been well characterized. There is an immediate inflammatory response to the stressed state that occurs in the first hours following the insult to the host. It can last anywhere from hours to days. This initial response is followed by a longer, immunosuppressive phase that occurs from 48 h to 72 h after the insult and can last several days to weeks. The degree to which this peak and valley response occurs is dependent on the degree of stress sustained by the host. The attendant morbidity seen with these deviations from the homeostatic baseline increases proportionally to the level of response.
In the stressed state, the body undergoes various physiologic and metabolic changes. A hypermetabolic state ensues after a stress response, leading to insulin resistance and hyperglycemia. There is increased oxidative stress at the cellular level and systemic activation of various inflammatory processes that lead to complex immunologic changes. There is a poor adaptation to starvation, and accelerated turnover of energy stores [1]. All macronutrients are affected by this process, however, protein catabolism is increased in the stressed state disproportionately more [2••].
Protein Use in Critical Illness
Why is protein so important to the critically ill patient? Why do we focus so much on it? We know that negative energy balance in critical illness correlates to morbidity [3]. This negative outcome is seen most acutely with loss of lean body mass [2••]. Heightened rates of protein catabolism in the stressed state will lead to loss of lean body mass. Increased turnover of protein is seen after a stress response despite nutritional support that would be considered adequate for a non-stressed individual [2••]. There are many factors leading to this increased loss of protein, including mobilization of peripheral stores for gluconeogenesis, production of acute phase reactants, promotion of wound healing via production of cells like fibroblasts, and restoration of acid base balance in the kidney [2••]. Support of the immune system via maintenance of gut mucosal integrity is another important source of protein turnover and utilization [4]. Protein turnover is also increased by states such as starvation and prolonged immobilization, both of which are common during critical illness. This heightened and exaggerated catabolism of protein is disproportionate to the overall increase in metabolism as well; we know that provision of nonprotein calories in amounts sufficient to meet energy demands does little to preserve lean body mass and improve nitrogen sparing. In fact, protein requirements in critical illness can increase to 15–20% of total calories [5].
Another concept to consider when thinking about protein requirements in the critically ill is the idea of “conditionally essential” amino acids. Certain amino acids which are not considered essential in the nonstressed state become essential during critical illness because of increased requirements for that particular amino acid. For example, high amounts of tryptophan, phenylalanine, and tyrosine are seen in acute phase proteins, and the increased synthesis of these proteins requires proportionately higher need for these amino acids [6]. Similarly, glutamine, which is normally 50% of the body’s intracellular free amino acid pool (and is necessary as fuel for rapidly dividing cells, and as a nitrogen shuttle between visceral organs and muscle tissue) rapidly decreases in concentration in certain states and exceeds the cell’s ability to synthesize it [7, 8]. This alteration in substrate utilization can lead to breakdown of muscle tissue in order to supply these “conditionally essential” amino acids, further enhancing the loss of lean body mass.
Loss of lean body mass and negative nitrogen balance are seen most dramatically in the first 9–12 days following an insult, but continue to exceed the loss that would be expected based on the increase in resting energy expenditure in this patient population through the first 21 days [9]. In fact, 16% of total body protein is lost in that first 21-day period, 67% of which comes from muscle stores [9]. Loss of lean body mass in critical illness has been linked to increased rates of pneumonia, impaired wound healing, and prolonged rehabilitation, pressure ulcers, and even mortality [10].
Delivery of Protein in ICU: How Much?
Minimizing the loss of lean body mass and preserving positive nitrogen balance is obviously important in critical illness when one looks at the negative impacts of this catabolic state. The question that remains is how do we best achieve this goal? Every patient is different, and different states affect this catabolic state differently. For example, minor trauma or surgery has less of an effect on protein turnover than severe sepsis or burns. There are many calculations and methods to assess protein metabolism and nitrogen balance, including assessing nitrogen balance, measuring amino acids directly by sampling directly across tissue beds, measurement of tracers to assess protein degradation, and turnover of individual components, such as urea. Of these methods, nitrogen balance is the most widely used [2••].
Nitrogen balance is best assessed through the quantification of urine urea nitrogen.
- Nitrogen balance:
-
Nitrogen intake–Nitrogen output
- Nitrogen output (g/day):
-
urinary urea nitrogen (mg/100 mL) X urinary volume (L/day)/100 + 20% of urinary urea losses + 2 g [11]
This equation requires collection of a 24-h urine sample. In addition, this equation must be adjusted to account for losses from renal dysfunction, stool, ostomy, and fistula losses [1]. These losses, plus incomplete urine collections, can make this equation somewhat unreliable and cumbersome to use at the bedside. However, this can be a reliable tool to assess the adequacy of protein delivery.
Because of the discrepancies and difficulty assessing nitrogen balance, because there is a paucity of data to suggest that clinical benefits from reduction of net N losses through provision of protein-rich diets, and because there are some data available to suggest that provision of high amounts of protein may in fact be harmful, there is a significant amount of uncertainty about the optimum amount of protein to provide these patients [12]. Current guidelines from the American Society for Parenteral and Enteral Nutrition (ASPEN), the European Society for Parental and Enteral Nutrition (ESPEN), and the Society of Critical Care Medicine (SCCM) suggest the provision of 1.5–2.0 g protein/kg/day to patients with moderate to severe stress as a result of trauma, sepsis, or surgery [13••, 14]. Patients with severe sepsis or burns may require up to 2.5–3 g protein/kg/day [15]. Ongoing assessments of adequate protein delivery, such as urine urea nitrogen and documentation of wound healing, should be performed.
With all the discussion about the potential benefits of protein provision in critical illness, there is also the question of whether or not protein intake should be limited in certain disease states. There is some concern among practitioners about provision of protein to patients with chronic liver disease. The concern for hepatic encephalopathy in this patient subset prompts many to restrict dietary protein. As patients with cirrhosis are usually hypermetabolic to a degree, this practice can worsen protein calorie malnutrition that is already present in many of these patients and, in turn, worsen outcomes [16, 17]. Most of these patients can tolerate protein without exacerbation of hepatic encephalopathy; however, there is a subset of patients who may have worsening mental status that is refractory to medical management. Branched chain amino acids (BCAA) have a competitive action on amino acid transport across the blood brain barrier, and are a substrate for protein synthesis [18]. In this setting, BCAA may be considered to provide the necessary nitrogen intake and may not worsen hepatic encephalopathy [16, 17]. There is also some data to suggest that BCAA supplementation may decrease the frequency of cirrhosis related complications and improve nutritional status in chronic liver disease [19]. The cost associated with BCAA therapy, as well as the poor palatability, limits their use in standard clinical practice; however, they could be considered in select patients.
Another disease state in which protein provision is controversial is renal failure. The restriction of protein in these patients has been the topic of debate for many years. The results of clinical trials are varied, some claiming benefit and others claiming none [20–23]. The Modification of Diet in Renal Disease Study (MDRD) published long term follow up data on 255 patients with Stage 4 nondiabetic chronic kidney disease over 10 years. The results of the MDRD study showed that despite the findings of other small trials, provision of very low protein diet (0.28 g/kg/day) did not delay the progression to renal failure, and appeared to have an increased risk of death [24]. In light of these findings, the practice of limiting protein in patients with chronic kidney injury is not recommended in the ASPEN or SCCM guidelines [13••].
Delivery of Protein in ICU: What Form?
Further compounding the debate over how much protein to deliver in critical illness is the debate over what form of protein should be delivered. There is a significant amount of data emerging regarding whey-based formulas as compared to casein or soy based formulas. Whey has been demonstrated in preclinical studies to facilitate protein synthesis [25], reduce inflammation, increase anti-oxidant effects [26], and reduce gut-reperfusion injury [27]. Human data is lacking, however, and further investigation must be done to fully elucidate the optimum type of protein to supply.
Another area of interest revolves around small peptide formulations. There are studies to suggest that, at a physiologic level, peptide based formulations are easier to absorb across the gut lumen, result in less feeding intolerance, and cause increase in protein synthesis at the visceral level with resultant increases in nitrogen retention [28]. Preclinical studies have also demonstrated that glucagon is increased in greater amounts with peptide-based formulations, and that glucagon may have a positive trophic effect on the intestinal mucosa [29]. In animal models, research has found that peptide diets show higher levels of nitrogen retention, higher rates of weight gain, higher rates of tissue repair, and a positive trophic effect on small bowel mucosa when compared to free amino acid formulas [28, 30, 31]. While this has been well substantiated in animal models, there are not a great deal of level 1 data to support these claims in the clinical setting. A number of small trials, however, have demonstrated a decrease in intolerance as defined by diarrhea and better visceral protein levels as measured by prealbumin [32]. In addition, peptide formulations have shown promise in Crohn’s patients, acting to reverse growth failure in children and reduce steroid use [33, 34]. While more definitive data in this area are necessary, peptide formulations may have a role in the treatment of patients with malabsorption from inflammatory bowel conditions or critical illness.
Specific Amino Acid Delivery
A promising area on the horizon for protein delivery is the idea of specific amino acid delivery and the potential benefits of this practice. Specific amino acids, such as glutamine and arginine, which are discussed later in this review, are becoming an ever-increasing part so-called immunonutrition, the concept that specific therapeutic agents like amino acids, antioxidants, or fish oils, can have powerful therapeutic benefits. We know that certain amino acids exert pharmacologic activity when given during critical illness, and that these actions can have wide and varied clinical results.
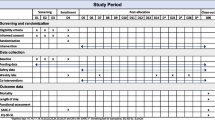
The amino acids that are the most promising as therapeutic targets are those that are conditionally essential, as discussed earlier. There is an overwhelming amount of data to support the claim that these immune modulating formulas impact outcomes (see Table 1). It is difficult, however, to know which portion of the formula is causing the clinical effect. Specialty formulas designed to enhance the immune system are costly, and many practitioners express concern that in the absence of hard data to support their use, we cannot rationalize the expense. However, ASPEN and SCCM both recommend the use of immune-modulating formulas containing arginine, glutamine, nucleic acids, and omega–3 fatty acids. Antioxidants are recommended for patients undergoing major elective surgery, trauma, burns, head and neck cancer, and critically ill patients on mechanical ventilation, with caution being exercised in those with severe sepsis [13••].
Glutamine
Glutamine is the most abundant free amino acid in the human body, making up more than 50% of the intracellular free amino acid pool. It has been studied in great detail over the past 15 years, and its effects and uses are wide and varied. Glutamine is an important fuel source for rapidly dividing cells, such as fibroblasts and reticuloendothelial cells, as well as the gut mucosa of the small bowel [2••]. In addition, it carries two nitrogen moieties per molecule, and serves as a shuttle for nitrogen between muscle tissue and visceral organs [1]. Glutamine obviously plays an important role in cell homeostasis and organ metabolism. Because of these functions, glutamine stores rapidly deplete and decreased circulating concentrations are seen in exercise, sepsis, and trauma [35]. When the circulating concentration of glutamine exceeds the body’s ability to synthesize de novo glutamine, atrophy of intestinal mucosa, impairment of immune function, and decreased protein synthesis are seen [36]. Decreased levels of plasma glutamine have also been shown to be correlated with increased mortality [37].
There are many proposed mechanisms by which glutamine acts on and supports the immune system. Glutamine exhibits a direct antioxidant effect and reduces oxidative stress on cells by attenuating the inducible nitric oxide synthase (iNOS) pathway in sepsis. It also acts directly on the tissue by preserving mitochondrial function and acting as a substrate for adenosine triphosphate (ATP) synthesis. In addition, it attenuates cytokine expression [36]. But perhaps the most important manner in which glutamine exerts its actions on the immune system is by upregulation of heat shock proteins. Heat shock proteins function to refold misfolded proteins coming off the endoplasmic reticulum, help eliminate irreversibly damaged proteins by marking them for apoptosis, stimulate the innate immune system, and attenuate proinflammatory cytokines [38]. Heat shock proteins are induced by a stress response, and this induction is enhanced by glutamine administration, heightening their response [39, 40]. The proposed mechanism through which this occurs is via attenuation of the inflammatory response by binding and inhibiting NF-ΚΒ, thus limiting IL-6 and TNF-α, which occurs as a proinflammatory response to injury/sepsis [41].
Glutamine supplementation in critical illness has been shown in the clinical setting to have decreases in mortality, length of stay, and infectious morbidity. Interestingly, however, there are some data to suggest that there is no effect to glutamine supplementation. These studies are very heterogeneous with respect to patient population, route of glutamine administration, and amount of glutamine administration [40]. It seems that high doses given via a parenteral route demonstrate greater effect than low doses given by the enteral route. It is recommended to give high-dose oral glutamine at levels >0.2–0.3 g/kg/day (or roughly, 20–40 g/day). There is more data for intravenous glutamine than for glutamine administered orally, however high oral doses seem to be efficacious [40].
Arginine
Arginine is considered a nonessential amino acid under normal physiologic conditions. L-Arginine is available to the host from endogenous synthesis via citrulline conversion in kidney, from endogenous protein breakdown, and from dietary protein sources [42]. Arginine plays an active role in cell growth and proliferation, wound healing, immune function and regulation, and waste ammonia disposal through the urea cycle [2••]. Arginine also helps regulate vascular endothelial vasodilatation through the nitrogen oxygen synthase (NOS) pathway and the generation of nitric oxide (NO) [43]. NO is also a potent intracellular signaling molecule influencing virtually every mammalian cell type and is involved in the cytotoxicity of activated macrophages [42]. De novo synthesis, as well as dietary supplementation of arginine is diminished in critical illness, making it a conditionally essential amino acid.
In critical illness, the cellular demand for arginine is increased. This is related to the upregulation of arginase-1, which is reported in trauma and surgery [44]. In addition, plasma arginine levels diminish rapidly in trauma, critical illness, and sepsis [45]. When arginase pathways are upregulated, there is a resultant decrease in substrate availability for the opposing NOS pathway, thereby downregulating NO synthesis [42]. It is believed this inhibition of the NOS pathway is secondary to increased circulating levels of asymmetric dimethylarginine (ADMA), which may have a direct inhibitory effect on the NOS pathway [46, 47]. ADMA is then converted to citrulline, which is then use to synthesize arginine [42]. The question is whether this downregulation of the NOS pathway and resultant decrease in the levels of circulating NO is the source of the vasoconstriction and end-organ malperfusion seen in sepsis, or if this downregulation is an adaptive strategy the body undergoes to prevent hypotension after critical illness [48•].
This question is the source of much controversy in the topic of arginine supplementation. Is the increased activity of arginase-1 involved in the increased levels of ADMA purely a mechanism by which to increase de novo synthesis of arginine in times of need? Does supplementation of arginine fuel the NOS pathway in preference to the arginase-1 pathway? In hemodynamically unstable critically ill patients, there was growing concern that the vasodilatation related to increased NO could worsen systemic hypotension [49]. As arginine is a common constituent of many immune-enhancing formulas utilized in the critically ill patient, this concept led to growing concern about immunonutrition use in septic patients.
Making generalized statements about amino acid metabolism in critical care is extremely difficult because the critically ill population is not a homogeneous group. Making any generalized statements about the toxicity or benefits of any dietary supplement, let alone an amino acid with the metabolic complexity of arginine, is not advisable as no study of these individual supplements can effectively be done in a clinical setting. Although theoretical concern is understood, both animal and human data are available to support arguments for and against the use of arginine [50, 51]. In light of this conflicting data, safety issues remain. Currently ASPEN recommends against the use of arginine-containing formulas in the hemodynamically unstable patient, regardless of the nature of the insult [13••]. Further research as to the safety and efficacy of arginine in sepsis is needed.
In hemodynamically stable patients, the optimal dose of arginine to be delivered has yet to be determined. It seems that the 15 g to 30 g of enteral supplemental arginine is safe and appears to meet the needs of the patient [52]. This is the amount that is commonly received at goal rates with immune-modulating formulas.
Amino Acids on the Horizon
In addition to arginine and glutamine, there are many other promising amino acid targets that are the fuel for ongoing research. Citrulline is one such amino acid. Citrulline is utilized in the de novo synthesis of arginine and is produced through conversion of ADMA, as previously discussed [47]. Studies demonstrate that citrulline availability is closely linked with arginine availability [50, 52]. Provision of citrulline may provide for de novo synthesis of arginine, thereby reducing the amounts of circulating ADMA and its deleterious effects.
Choline is another essential amino acid that is necessary for cell membrane structure. Choline is not a part of many parenteral nutritional formulations (PN), and patients on longterm PN have impaired choline synthesis [2••]. There is some evidence to support that this choline deficiency plays a role in the hepatic impairment seen in patients on longterm PN. Enteral repletion of choline to prevent or treat PN-induced hepatic failure is currently under research and shows a lot of promise [53].
Conclusions
Is it fact or fantasy that we can improve outcomes in our critically ill patients through the appropriate and timely supplementation of protein and by specifically targeting certain amino acids for immune modulation? By review of the current data and promising glimpses at the future of nutritional support, we can conclude that this is a fact. We can change outcomes for the better. It is therefore important to remember:
-
Supply adequate protein calories for the degree of metabolic insult. Namely, 1.5–2.0 g protein/kg/day for moderate to severe stress, and 2.5–3.0 g protein/kg/day for severe sepsis or burns.
-
Provision of more protein than these recommendations is not helpful. Enough is enough.
-
Protein restriction is rarely indicated, and can potentially exacerbate already severe malnutrition in the state of critical illness.
-
Glutamine is beneficial in the setting of critical illness. Glutamine supplementation has been demonstrated reliably to reduce inflammation, reduce infectious risks, and improve outcomes.
-
Arginine is also recommended for immune support in appropriate patient populations, namely surgical or trauma patients and some medical patients. Use caution in sepsis because of safety concerns.
-
There is little support for the use of branched chain amino acids routinely in hepatic encephalopathy, although they may play a role in the treatment of select patients who are refractory to maximized medical management.
-
The use of peptide-based formulations remains an area of ongoing research, although there are some trends to favor their use in the management of patients with inflammatory bowel disease and malabsorption related to critical illness. There is some evidence to support reduction in diarrhea, retention of nitrogen, and reduction of steroid use in Crohn’s disease, specifically.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Lin E, Calvano SE, Lowry SF. Systemic response to injury and metabolic support. In: Brunicardi FC, Anderson DK, et al., editors. Schwartz’s principles of surgery. New York: McGraw-Hill; 2005. p. 3–41.
•• Young LS, Kearns LR, Schoepfel SL. Protein. In: Gottschlich MM, editor. The A.S.P.E.N. Nutrition Support Curriculum. Cincinatti: A.S.P.E.N.; 2007. p. 71–87 This reference is exceedingly important as it provides a practical guide and approach to the care of the adult patient requiring nutritional support.
Villet S, Chiolero RL, Bollmann MD, et al. Negative impact of hypocaloric feeding and energy balance on critical outcome in ICU patients. Clin Nutr. 2005;24:502–9.
Jabbar A, Wei-Kuo C, McClave SA, et al. Gut immunology and the differential response to feeding and starvation. Nutr Clin Pract. 2003;18:461–82.
Shaw JH, Wildborne M, Wolfe RR. Whole body protein kinetics in severely septic patients. The response to glucose infusion and total parenteral nutrition. Ann Surg. 1987;205:288–94.
Reeds PJ. Dispensible and indispensible amino acids for humans. J Nutr. 2000;130:1835S–40.
Griffiths RD, Allen KD, Andrews FJ, et al. Infection, multiple organ failure, and survival in the intensive care unit: influence of glutamine-supplemented parenteral nutrition on acquired infection. Nutrition. 2002;18:546–52.
Alpers DH. Glutamine: do the data support the cause for glutamine supplementation in humans? Gastroenterology. 2006;130:S106–16.
Monk DN, Plank LD, Franch-Arcas G, et al. Sequential changes in the metabolic response in critically injured patients during the first 25 days after blunt trauma. Ann Surg. 1996;223(4):395–405.
Martindale RG, Zhou M. Nutrition and metabolism. In Physiologic Basis of Surgery. 2008.
Wilmore DW. Metabolic management of the critically ill. New York: Plenum; 1977. p. 193.
Stroud M. Protein and the critically ill; do we know what to give? Proc Nutr Soc. 2007;66:378–83.
•• McClave SA, Martindale RG, Vanek VW, et al. A.S.P.E.N. Board of Directors; American College of Critical Care Medicine; Society of Critical Care Medicine: Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (ASPEN). JPEN 2009;33:277–316. This reference is of importance as it is the reference of most practitioners in the nutritional support of the critically ill in America. The entire guideline is found online at the ASPEN website.
Kreymann KG, Berger MM, Deutz NE, et al. ESPEN (European Society for Parenteral and Enteral Nutrition): ESPEN guidelines on enteral nutrition: intensive care. Clin Nutr. 2006;25:210–33.
Jacobs DG, Jacobs DO, Kudsk KA, et al. Practice management guidelines for nutrition support of the trauma patient. J Trauma. 2004;57:660–79.
Chadalavada R, Sappati BRS, Maxwell J, et al. Nutrition in hepatic encephalopathy. Nutr Clin Pract. 2010;25(3):257–64.
Marchesini G, Bianchi G, Rossi B, et al. Nutritional treatment with branched-chain amino acids in advanced liver cirrhosis. J Gastroenterol. 2000;35 Suppl 12:7–12.
Bianchi G, Marzocchi R, Agostini F, et al. Update on branched-chain amino acid supplementation in liver diseases. Curr Opin Gastroenterol. 2005;21(2):197–200.
Charlton M. Branched chain amino acid enriched supplements as therapy for liver disease. J Nutr. 2006;136(1 Suppl):295S–8.
Garneata L, Mircescu G. Nutritional intervention in uremia—myth or reality? J Ren Nutr. 2010;20(5 Suppl):S31–4.
Levey AS, Greene T, Sarnak MJ, et al. Effect of dietary protein restriction on the progression of kidney disease: long-term follow up of the MDRD Study. Am J Kidney Dis. 2006;48(6):879–88.
Mircescu G, Garneata L, Stancu SH, et al. Effects of a supplemented hypoproteic diet in chronic kidney disease. J Ren Nutr. 2007;17(3):179–88.
Aparicio M, Chauveau P, Combe C. Low protein diets and outcome of renal patients. J Nephrol. 2001;14(6):433–9.
Menon V, Kopple JD, Wang X, et al. Effect of a very low-protein diet on outcomes: long-term follow up of the MDRD Study. Am J Kidney Dis. 2009;53(2):208–17.
Ha E, Zemel MB. Functional properties of whey, whey components, and essential amino acids: mechanisms underlying health benefits for active people (review). J Nutr Biochem. 2003;14(5):251–8.
De Aguilar-Nascimento JE, Prado Silveira BR, Dock-Nascimento DB. Early enteral nutrition with whey protein or casein in elderly patients with acute ischemic stroke: a double-blind randomized trial. 2010;15:310–24.
Nakamura K, Ogawa S, Dariki K, et al. A new immune modulating diet enriched with whey-based hydrolyzed peptide, fermented milk, and isomaltulose attenuates gut ischemia-reperfusion injury in mice. Clin Nutr 2011;Epub Jan 29, 2011.
Poullain MG, Cezard JP, Roger L, et al. Effect of whey proteins, their oligopeptide hydrosylates and free amino acid mixtures on growth and nitrogen retention in fed and starved rats. JPEN. 1989;13:382–6.
Rerat A, Nunes CS, Mendy FG, et al. Amino acid absorption and production of pancreatic hormones in non-anaesthetized pigs after duodenal infusions of a milk enzymatic hydrosylate or free amino acids. Br J Nutr. 1988;60:121–36.
Birke H, Thoiacus-Ussing O, Hessov I. Trophic effect of dietary peptides on mucosa in the rat bowel. J Parent Ent Nutr. 1990;14(Suppl):2. Abstract.
Zaloga GP, Ward KA, Prielipp RC. Effect of enteral diets on whole body and gut growth in unstressed rats. J Parent Enteral Nutr. 1991;15:42–7.
Meredith JW, Ditesheim JA, Zaloga GP, et al. Visceral protein levels in trauma patients are greater with peptide diet than with intact protein diet. J Trauma. 1990;30(7):825–9.
Polk DB, Hattner JT, Kerner JA. Improved growth and disease activity after intermittent administration of a defined formula diet in children with Crohn’s disease. J Parent Enteral Nutr. 1992;16:499–504.
Hartman C, Eliakim R, Shamir R. Nutritional status and nutritional therapy in inflammatory bowel diseases. World J Gastroenterol. 2009;15(21):2570–8.
Oudemans-van Straaten HM, Bosman RJ, Treskes M, et al. Plasma glutamine depletion and patient outcome in acute ICU admissions. Inten Care Med. 2001;27:84–90.
Wischmeyer PE. Glutamine: role in gut protection in critical illness. Curr Op Clin Nutr. 2006;9:607–12.
Novak F, Heyland DK, Avenell A, et al. Glutamine supplementation in serious illness: a systematic review of the evidence. Crit Care Med. 2002;30:2022–9.
Macario AJL, Conway de Macario E. Sick chaperones, cellular stress and disease. NEJM. 2005;353:1489–501.
Oliveira GP, Dias CM, Rocco PR. Understanding the mechanisms of glutamine action in critically ill patients. An Acad Bras Cienc. 2010;82(2):417–30.
Kelly D, Wischmeyer PE. Role of L-glutamine in critical illness: new insights. Curr Opin Clin Nutr Metab Care. 2003;6(2):217–22.
Singleton KD, Beckey VE, Wischmeyer PE. Glutamine prevents activation of nfkappab and stress kinase pathways, attenuates inflammatory cytokine release, and prevents acute respiratory distress syndrome (ARDS) following sepsis. Shock. 2005;24(6):583–9.
Zhou M, Martindale RG. Arginine in the critical care setting. Jour Nutr. 2007;137:1687S–92.
Albina JE, Mills CD, Henry Jr WL, et al. Regulation of macrophage physiology by L-arginine: role of the oxidative L-arginine deaminase pathway. J Immunol. 1989;143:3641–6.
Morris SM. Recent advances in arginine metabolism. Curr Opin Clin Nutr Metab Care. 2004;7:45–51.
Chiarla C, Giovannini I, Siegel JH. Plasma arginine correlations in trauma and sepsis. Amino Acids. 2006;30:81–6.
Arrigoni F, Ahmetaj B, Leiper J. The biology and therapeutic potential of the DDAH/AMDA pathway. Curr Pharm Des. 2010;16(37):4089–102.
Pope AJ, Karrupiah K, Xia Y, et al. Role of dimethylarginine dimethylaminohydrolases in the regulation of nitric oxide production. J Biol Chem. 2009;284(51):36338–47.
• Fortin CF, McDonald PP, Fulop T, et al. Sepsis, leukocytosis, and nitric oxide (NO): An intricate affair. Shock 2010;33(4):344–52. This paper is of importance as it clearly delineates the role of NO in sepsis and how arginine is involved. It makes the arginine argument clear.
Suchner U, Heyland DK, Peter K. Immune-modulatory actions of arginine in the critically ill. Brit Jour Nutr. 2002;87 Suppl 1:S121–32.
Kao CC, Bandi V, Guntupalli KK, et al. Arginine, citrulline and nitric oxide metabolism in sepsis. Clin Sci (Lond). 2009;117(1):23–30.
Luiking YC, Poeze M, Ramsay G, Deutz NE. Reduced citrulline production in sepsis is related to diminished de novo arginine and nitric oxide production. Am J Clin Nutr. 2009;89(1):142–52.
Pan M, Choudry HA, Epler MJ, et al. Arginine transport in catabolic disease states. Jour Nutr. 2004;134:2826S–9. discussion 2853S.
Chawla RK, Berry CJ, Kutner MH, et al. Plasma concentration of transulfuration pathway products during nasoenteral and intravenous hyperalimentation of malnourished patients. Am J Clin Nutr. 1985;42:577–84.
Braga M, Gianotti L, Giovanni R, et al. Perioperative immunonutrition in patients undergoing cancer surgery. Arch Surg. 1999;134:428–33.
Senkal M, Zumtobel V, Karl-Heinz B, et al. Outcome and cost-effectiveness of perioperative enteral immunonutrition in patients undergoing elective upper gastrointestinal tract surgery. Arch Surg. 1999;134:1309–16.
Snyderman CH, Kachman K, Molseed L, et al. Reduced postoperative infections with an immune-enhancing nutritional supplement. Laryng. 1999;109(6):915–21.
Riso S, Aluffi P, Brugnanai M, et al. Postoperative enteral immunonutrition in head and neck cancer patients. Eur J Clin Nutr. 2005;59:145–7.
Tepaske R, Velthuis H, Oudemans-van Straaten HM, et al. Effect of preoperative oral immune-enhancing nutritional supplement on patients at high risk of infection after cardiac surgery: a randomized placebo-controlled trial. Lancet. 2001;358:696–701.
Gianotti L, Braga M, Nespoli L, et al. A randomized controlled trial preoperative oral supplementation with a specialized diet in patients with gastrointestinal cancer. Gastroenterology. 2002;122:1763–70.
Braga M, Gianotti L, Nespoli L, et al. Nutritional approach in malnourished surgical patients: a prospective randomized study. Arch Surg. 2002;137:174–80.
Giger U, Buchler M, Farhadi J, et al. Preoperative immunonutrition suppresses perioperative inflammatory response in patients with major abdominal surgery—a randomized controlled pilot study. Ann Surg Onc. 2007;14(10):2798–806.
Klek S, Kulig J, Sierzega M, et al. The impact of immunostimulating nutrition on infectious complications after upper gastrointestinal surgery: a prospective randomized clinical trial. Arch Surg. 2008;248(2):212–20.
Fukuda T, Seto Y, Hiki N, et al. Can immune-enhancing nutrients reduce postoperative complications in patients undergoing esophageal surgery? Dis Esophagus. 2008;21(8):708–11.
Helminen H, Raitanen M, Kellosalo J. Immunonutrition in elective gastrointestinal surgery patients. Scand J Surg. 2007;96(1):46–50.
Ryan A, Power D, Reynolds J. Immunonutrition in upper gastrointestinal surgery. Arch Surg. 2009;249(6):1062–3.
Okamoto Y, Keiichi O, Kunihiko I, et al. Attenuation of the systemic inflammatory response and infectious complications after gastrectomy with preoperative oral arginine and omega 3 fatty acids supplemented immunonutrition. WJS. 2009;33(9):1815–21.
Disclosure
S.A. McClave: Received honoraria from Nettle Pharmaceuticals and Abbott Pharmaceuticals, and worked as a consultant for Kimberly Clark and Covidien Pharmaceuticals; C.M. Lawson; K.R. Miller; and V.L. Smith reported no potential conflicts of interest relevant to this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lawson, C.M., Miller, K.R., Smith, V.L. et al. Appropriate Protein and Specific Amino Acid Delivery Can Improve Patient Outcome: Fact or Fantasy?. Curr Gastroenterol Rep 13, 380–387 (2011). https://doi.org/10.1007/s11894-011-0201-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11894-011-0201-0