Abstract
Purpose of Review
Hyperglycemia occurs frequently in hospitalized patients with stroke and peripheral vascular disease (PVD). Guidelines for inpatient glycemic management are not well established for this patient population. We will review the clinical impact of hyperglycemia in this acute setting and review the evidence for glycemic control.
Recent Findings
Hyperglycemia in acute stroke is associated with poor short and long-term outcomes, and perioperative hyperglycemia in those undergoing revascularization for PVD is linked to increased post-surgical complications. Studies evaluating tight glucose control do not demonstrate improvement in clinical outcomes, although the risk for hypoglycemia increases substantially. Additional studies are needed to evaluate tight glucose goals relative to our current standard of care and the role of permissive hyperglycemia.
Summary
Given the limited data to guide glycemic management in these patient populations, it is recommended that general guidelines for inpatient glycemic control be followed. Special considerations should be made to address factors that may impact glucose management, including neurological deficits and clinical changes that occur in the postoperative state.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
While glucose management in hospitalized patients with coronary artery disease requiring surgical intervention has been extensively studied, relatively less attention has been devoted to understanding the role of inpatient glycemic management for non-cardiac cardiovascular disease (CVD) [1]. In this article, we review the literature regarding the prevalence, associated outcomes, and management of hyperglycemia in hospitalized patients with acute stroke and peripheral vascular disease (PVD). For the latter, we focus on surgical outcomes and perioperative management, since the focus of PVD management in the hospital is largely surgical. Given the limited evidence on this topic, we highlight areas of uncertainty and unique management considerations for this patient population.
Stroke
Background
Hyperglycemia occurs frequently in the setting of stroke. It is estimated that the risk for ischemic stroke is two- to threefold higher in men and two- to fivefold higher in women with diabetes compared to those without diabetes [2]. Furthermore, in those with ischemic stroke, it is estimated that the prevalence of recognized diabetes is 30%, while 17% have occult diabetes and 20% have impaired glucose metabolism [3]. Many patients without a history of diabetes may also experience acute hyperglycemia in the setting of this neurologic stressor. Shimoyama et al. evaluated 375 patients with acute ischemic stroke and found that of 143 patients who presented with hyperglycemia, only 40.6% had a diagnosis of diabetes [4].
Outcomes
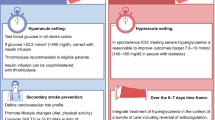
As reviewed in Table 1, hyperglycemia during stroke has been linked to worse clinical outcomes including greater infarct expansion, increased hemorrhagic conversion, more severe neurological deficits, and increased mortality. There is also evidence that acute hyperglycemia is more detrimental than chronic hyperglycemia. This finding has been demonstrated in other inpatient populations [13,14,15,16,17]. In addition to poor short-term outcomes, patients with hyperglycemia in the setting of acute stroke may have worse long-term outcomes. It is important to emphasize that hyperglycemia does not necessarily have a causal relationship with stroke outcomes and may simply be a marker of disease severity. Although we will focus mainly on the impact of acute hyperglycemia on clinical outcomes, it is important to note that the degree of chronic hyperglycemia, measured by A1c on admission, has also been associated with stroke severity and functional outcomes [18].
Short-Term Outcomes
In patients with acute stroke, Pulsinelli et al. found that stroke-related deficits were more severe in those with an admission glucose value more than 120 mg/dl [5]. Evidence from both animal and human studies suggests that hyperglycemia may be toxic to the ischemic brain; in the ischemic penumbra, anaerobic metabolism of glucose leads to lactic acidosis, resulting in mitochondrial dysfunction and a worsening cycle of acidosis from increasing anaerobic metabolism [19]. Parsons et al., who performed MRI/MR spectroscopy to assess tissue lactate accumulation in acute stroke patients, showed that higher acute blood glucose levels were associated with greater lactate production. The authors also noted that acute hyperglycemia was correlated with reduced salvage of potentially viable tissue, greater final infarct size, and worse functional outcome [6]. These findings have been confirmed in numerous studies [20,21,22].
Hyperglycemia in acute stroke has also been associated with increased risk for hemorrhagic transformation. The National Institute of Neurological Disorders and Stroke Recombinant Tissue Plasminogen Activator Stroke (NINDS rt-PA) Trial showed that the odds of symptomatic ICH increased by 1.75 per 100 mg/dl of admission blood glucose regardless of rt-PA treatment [7]. The Safe Implementation of Treatments in Stroke International Stroke Thrombolysis Registry (SITS-ISTR) found that blood glucose levels greater than 180 mg/dl were independently associated with higher risk of intracerebral hemorrhage (OR 2.86) [8].
Hyperglycemia is thought to have direct effects on vasculature causing endothelial dysfunction. In animal models, products of anaerobic metabolism and free radicals may disrupt the blood-brain barrier causing increased permeability resulting in cerebral edema [23]. It is unclear whether this process also occurs in humans, but disruption of the blood-brain barrier may be a mechanism for hemorrhagic transformation in hyperglycemic stroke patients. In addition to neurologic deficits, a large prospective study found that rates of hospital complications, including infection and venous thrombosis, were higher in patients with diabetes and acute stroke [23].
Neurological Recovery
Hyperglycemia has been linked to reduced neurological recovery following acute stroke. The Copenhagen Stroke study evaluated clinical outcomes during rehabilitation after acute stroke and found that patients with diabetes recovered more slowly despite having similar stroke severity scores [9]. In another study, when patients with mean admission glucose of greater than 160 mg/dl were compared to those with a mean glucose of 144 mg/dl or less, the former had less functional improvement following stroke. Interestingly, every 100 mg/dl increase in admission glucose was associated with a 24% reduction in odds of neurological improvement [10]. In a prospective study, Pulsinelli et al. found that in patients (with and without diabetes) with an admission glucose > 120 mg/dl, only 43% were able to return to work compared with 76% of those with glucose levels below this threshold [5].
Mortality and CVD Events
The large-scale prospective SITS-ISTR study of > 16,000 patients found that blood glucose was independently associated with mortality. Blood glucose greater than 120 mg/dl was associated with a 24% increase in odds for mortality at 3 months [8]. Williams et al. found that hyperglycemia, defined as admission glucose of 130 mg/dl, was an independent predictor of short- and long-term mortality. Hyperglycemia independently increased the risk for death at 30 days (HR 1.87, p ≤ 0.01), 1 year (HR 1.75, p ≤ 0.01), and 6 years after stroke (HR 1.41, p ≤ 0.01) [11]. Post-stroke glycemic variability is also associated with poor cardiovascular outcomes. Yoon et al. evaluated 674 acute stroke patients with diabetes and found that a high coefficient of variability in glucose values was associated with a greater risk of the composite of nonfatal stroke, nonfatal myocardial infarction (MI), and cardiovascular death [24].
New-Onset Hyperglycemia
Although most patients with pre-existing diabetes will experience hyperglycemia in the setting of acute stroke, so do many patients without diabetes. Allport et al. used continuous glucose monitoring (CGM) to characterize glucose trends in 59 patients with acute stroke, of whom 23 had no prior history of diabetes. In this group with a mean glycated hemoglobin (A1C) of 5.6%, 50% experienced hyperglycemia [25].
New-onset hyperglycemia in acute stroke is likely a function of several adaptive processes that occur in the setting of acute stress and severe illness. These physiologic changes include an increase in counter-regulatory hormones that result in increased hepatic glucose production and decreased peripheral glucose uptake [26]. In critical illness, high levels of cytokines, including tumor necrosis factor, alpha, and interleukin also increase blood glucose [26]. Hyperglycemia during stress is typically transient, but Allport et al. found that at 48–88 h post stroke, 27% of patients without diabetes and 78% of patients with diabetes still remained hyperglycemic [25].
In the acute stroke population, several studies have found that acute hyperglycemia is a better prognostic indicator than chronic hyperglycemia. Baird et al. found that mean glucose throughout the hospitalization better correlated with infarct volume and neurologic outcomes than admission A1C [3]. Shimoyama et al. found that degree of hyperglycemia correlated with infarct size in those without diabetes. This finding was found in patients with a diagnosis of diabetes [4]. Capes et al. performed a meta-analysis of 26 studies and found that the relative risk of in-hospital or 30-day mortality associated with admission glucose level of 108 to 144 mg/dl was 3.07 (95% CI, 2.50 to 3.79) in patients without diabetes and 1.30 (95% CI, 0.49 to 3.43) in patients with diabetes compared to lower glucose levels [12]. Levetan et al. [27] and Umpierrez et al. [28] both found that in-hospital mortality was increased, and functional outcomes were reduced in patients with new-onset hyperglycemia when compared to euglycemic patients or those with diabetes [29].
Hypoglycemia
Hypoglycemia, which often occurs in the setting of correcting hyperglycemia, is also associated with deleterious effects on the ischemic brain. Acute episodes of hypoglycemia have been associated with increased cerebral infarct size and ischemic damage in animal models of stroke [30]. Hypoglycemia aggravates brain injury after ischemic stroke by activating cell death pathways through stimulation of neuroinflammatory signaling cascades. A large outpatient prospective cohort study of 96,000 participants found that hypoglycemia was associated with an approximately twofold increased hazard ratio for intracerebral hemorrhage [31]. In light of these concerns, it is perhaps even more critical that hypoglycemia be avoided in acute stroke patients compared to general inpatients.
Although it is well known that hypoglycemia is associated with adverse neurological consequences [32] —ranging from altered mental status to seizure or coma—there are surprisingly very few studies quantifying the prevalence of hypoglycemic-related neurological complications following acute stroke in the hospital setting. Considering that approximately 5–20% of patients with acute stroke may develop a poststroke seizure [33], there is concern that hypoglycemia after acute stroke may further increase susceptibility for seizures [32]. In a study of general hospitalized patients of over 4000 admissions, severe hypoglycemia was associated with a risk of death as high as 8.2% and increased length of stay [34]. Both spontaneous and insulin-related hypoglycemia are associated with increased mortality in the general hospital population [35].
Acute Management of Hyperglycemia
Target Blood Glucose in Acute Stroke
There have been several randomized controlled trials (RCTs) exploring whether correcting hyperglycemia improves stroke outcomes. A Cochrane systematic review and meta-analysis evaluated 11 RCTs involving 1583 participants, of whom 791 were treated with tight glycemic control (blood glucose 72 to 135 mg/dl) and 792 were treated with placebo, loose, or no control in the first 24 h after stroke symptom onset [36]. The results of this meta-analysis showed that there was no difference between the treatment and control groups in outcomes of death, dependency, or final neurological deficit [36]. Of note, the mean blood glucose in the intervention and control groups were 121 and 132 mg/dl, respectively. Although these mean glucose values are statistically different, they both fall within the range specified for tight glucose control, thus making the results of this study less informative. Bruno et al., Johnston et al., and Kreisel et al. evaluated tight glucose control for longer periods of time (i.e., 3–5 days) and found no significant difference in mortality or functional outcomes [3]. In these three studies, the differences in blood glucose between the intervention and control groups were 133 versus 190 mg/dl, 111 versus 151 mg/dl, and 116 versus 144 mg/dl respectively.
In the Cochrane review mentioned above, despite a mean difference of glucose of only 11 mg/dl, the rate of symptomatic hypoglycemia was higher in patients subjected to tight glycemic control (OR 14.6), with a number need to harm of 9 [36]. In the SELESTIAL Trial, 76% of patients treated with intravenous (IV) insulin with strict goals experienced hypoglycemia [20]. There is currently an on-going large multicenter, RCT of 14,000 participants, The Stroke Hyperglycemia Insulin Network Effort (SHINE) Trial, which is evaluating the safety and efficacy of a glucose target of 80–130 mg/dl versus standard therapy [37]. The primary outcome is the Modified Rankin Scale for Neurologic Disability at 3 months. This study is still recruiting and results are expected in 2020 [38].
Although evidence suggests that tight glucose control (72 to 135 mg/dl) is more harmful than beneficial, there is little evidence to support what degree of glycemic control provides the most benefit. The joint guidelines of the American Heart Association and American Stroke Association on acute stroke management make a moderate strength of recommendation for a glucose target range of 140–180 mg/dl. They note that this recommendation is based on a relatively low quality of evidence [39]. Neurological expert opinion also has emphasized the avoidance of glucose less than 80 mg/dl [3]. Joint inpatient guidelines from the American Diabetes Association, the American Association of Clinical Endocrinologists, and the Endocrine Society, do not comment on specific glucose targets for those with acute stroke. These guidelines generally recommend a target blood glucose level of 140 mg/dl before meals and less than 180 mg/dl post-prandially in non-critically ill patients [40, 41].
Inpatient Management of Hyperglycemia
Inpatient hyperglycemia management recommendations in stroke patients are largely based on general recommendations for all acutely ill patients in the inpatient setting, as stroke-specific guidelines are lacking.
Subcutaneous Insulin Regimens
In the non-ICU hospital setting, a subcutaneous insulin regimen is recommended for patients with persistent hyperglycemia and for all insulin deficient patients (type 1 diabetes, or long-standing type 2 diabetes). At our institution, we consider two or more blood glucose readings ≥ 180 mg/dl as indication of persistent hyperglycemia. Many patients with type 2 diabetes treated at home with non-insulin antihyperglycemic medications may require insulin in the setting of stress-induced hyperglycemia.
Scheduled insulin regimens consisting of both basal and nutritional insulin are typically required to adequately control blood glucose levels [40]. For patients with mild hyperglycemia and no prior history of diabetes, it may be reasonable to start with a correctional insulin regimen alone. We typically recommend initiation of a basal-bolus insulin regimen in such patients once daily correctional insulin requirements exceed 10 units.
There are several well-described methods for estimating total daily insulin requirements: (a) weight-based estimate, which takes into account factors affecting insulin sensitivity (e.g., body weight) and hypoglycemic risk factors (e.g., reduced renal function, advanced liver disease) [41]; (b) adjustment of home insulin doses; (c) appraisal of previous 24-h insulin requirements (correctional insulin or insulin infusion rates). Once an estimate of TTD is calculated, this dose is distributed based on the nutritional status of the patient. Correctional insulin scales should be prescribed according to the patient’s estimated total daily dose to reflect their insulin sensitivity, as inappropriately high/aggressive correctional insulin scales could contribute to hypoglycemia, and inappropriately low scales will be insufficient.
Insulin Drips
Although subcutaneous insulin is usually adequate in management of inpatient hyperglycemia, there are circumstances in which IV insulin infusion is more appropriate. Patients presenting with acute stroke and evidence of diabetic ketoacidosis or hyperosmolar hyperglycemic state clearly require IV insulin. IV insulin should also be used for critically ill patients, those with difficult to control hyperglycemia and patients with ischemic stroke treated with thrombolytic therapy, given the increased risk for hemorrhagic transformation with uncontrolled hyperglycemia in the first 24–48 h [3]. Patients managed on an insulin drip will require frequent glucose monitoring, and the insulin drip should be titrated to maintain a blood glucose between 140 and 180 mg/dl based on recommendations for the general inpatient population [40]. Once glucose levels are well controlled and the patient is eating regular meals or transferred to lower intensity care, the patient should be transitioned to a subcutaneous insulin regimen [40].
Non-Insulin Anti-Hyperglycemic Agents
Non-insulin agents are typically inappropriate in most hospitalized patients who are admitted with serious illness, and these agents should be discontinued on admission [40]. Each class of oral hypoglycemic agents have restrictions that potentially limit their use in hospitalized patients, especially in the setting of fluctuating renal function, unstable hemodynamics, and frequent nutritional status changes. There is an on-going clinical trial exploring the use of the GLP-1 agonist, exenatide, in acute stroke [42]. Animal studies have shown that GLP-1 can act directly on the brain and reduce cerebral hyperglycemia, which may decrease oxidative stress and neuronal cell apoptosis [42]. A small pilot study of 11 patients with acute stroke showed that exenatide improved glucose control without symptomatic hypoglycemia. There were no serious adverse effects but most patients experienced mild nausea or vomiting [43]. Further studies will need to be done to clarify the potential role of GLP-1 agonist in stroke patients with hyperglycemia.
Special Considerations in Stroke Patients
Although the overall approach of inpatient hyperglycemia management in stroke patients mirrors that of the general hospital population, there are several situations that deserve special consideration in stroke patients.
Dysphagia is estimated to occur in 25–50% of stroke patients [44]. Food modifications to accommodate swallowing impairments include pureed or soft diets that are typically high in both fats and carbohydrates (e.g., mashed potatoes and gravy). High dietary fat in combination with carbohydrates may exacerbate and prolong post-prandial hyperglycemia in insulin deficient patients [45]. Alternative food choices, such as pureed vegetables, may be needed to improve glycemic control, and enlisting the help of the hospital nutrition team is advised. Patients with dysphagia do not always complete their meals or may eat small amounts slowly throughout the day instead of eating discrete meals. This may introduce a challenge due to mismatch in timing of the peak insulin effect and carbohydrate absorption. In this situation, it may be beneficial to administer nutritional insulin after verification that at least 50% of the carbohydrates of the meal have been consumed. Lastly, it will be important to ensure that the patient remains well hydrated to avoid renal insufficiency and subsequently increased hypoglycemia risk resulting from reduce insulin clearance. Dehydration can occur quickly if the patient is unable to consume thin liquids, and free water is not provided via an alternative method.
Cognitive and communication impairments may compromise the patient’s ability to report hypoglycemic symptoms. Careful attention should be made to identify trends in blood glucose levels that may be an indicator of future hypoglycemia [46]. Hemiparesis, ataxia, and visual impairment may complicate diabetes management upon discharge. For patients with impaired hand motor function, occupational therapy tailored to glucose monitoring and insulin administration will be important. Insulin pens should be considered on discharge over insulin administered through syringes. Insulin pens are also helpful for patients with visual impairments, as the doses can be easily measured by counting clicks. Talking glucose monitors are also helpful for home blood glucose monitoring in visually impaired patients. In patients with neurological deficits, it is important that discharge plans address barriers to diabetes self-management and that appropriate caregiver training is provided for a safe transition out of the hospital.
Peripheral Vascular Disease
Background
Peripheral vascular disease (PVD) occurs in patients with and without diabetes, but those with diabetes tend to have more severe disease. It is estimated that in those with PVD, 20–30% have diabetes. The true prevalence of PVD in those with diabetes is unknown but the United Kingdom Prospective Diabetes Study (UKPDS) found that 1.2% of patients with type 2 diabetes had PVD at the time of diabetes diagnosis. In those without PVD at diagnosis, there was a 28% increased risk of PVD at 6-year follow-up with each 1% increase in A1C [47]. The Framingham study showed that diabetes conferred a 3.5-fold and 8.6-fold increased risk in men and women, respectively, for PVD [48] [49]. Diabetes-related PVD risk is attributed to endothelial dysfunction, vascular smooth muscle cell dysregulation, inflammation, impaired function, and coagulation abnormalities, which in combination, result in accelerated proatherogenic changes [47].
In addition to the long-term impact of hyperglycemia on the progression and severity of PVD, studies have also found that in the inpatient setting, perioperative hyperglycemia is associated with negative outcomes. As with acute stroke, there is not strong evidence for selection of optimal glucose targets in the perioperative period.
Hyperglycemia and Surgical Outcomes
As summarized in Table 2, there have been several studies examining the impact of both chronic and acute hyperglycemia on outcomes after vascular surgery. Poorly controlled diabetes at baseline is a major risk factor for post-operative complications. Arya et al. found that each 1% rise in A1C above 6.0% was associated with a 25% higher risk of amputation and a 105% increased risk of a major adverse limb event [56]. Feringa et al. found that patients with impaired glucose regulation or diabetes were at higher risk for ischemia, troponin release, 30-day cardiac events, and long-term cardiac events. Patients with A1C > 7% were at 2.8-fold increased risk for ischemia, 5.3-fold increased risk for troponinemia, and 5.3-fold increased risk of 30-day cardiac event [58].
Short-term hyperglycemia, specifically in the pre-operative period, has also been associated with adverse post-operative outcomes. McGirt et al. demonstrated that increasing operative day glucose was associated with increased perioperative stroke, MI, and death after carotid endarterectomy. Patients at highest risk were those with an operative day glucose greater than 200 mg/dl: OR 2.8 for perioperative stroke or transient ischemic attack, OR 4.3 for MI, and OR 3.3 for death within 30 days [50]. In patients undergoing infrainguinal bypass surgery, Malmstedt et al. showed that perioperative hyperglycemia, determined by 48 h area under the curve for blood glucose after surgery, was associated with a 13.4-fold increase of surgical wound complications at 30 days [52]. Perioperative hyperglycemia has also been reported to increase odds of inpatient mortality, length of stay greater than 10 days, and risk of infection [54•, 59]. Ramos et al. found that risk of infection increased by 30% for every 40 mg/dl above a perioperative blood glucose of 110 mg/dl in patients undergoing general and vascular surgery [60].
Perioperative Glycemic Management
There are limited studies evaluating optimal glucose targets in patients undergoing surgery for PVD, and most evidence is extrapolated from the general surgical literature. A randomized controlled trial of 236 participants undergoing vascular surgery (of whom approximately half had diabetes) evaluated outcomes of continuous perioperative insulin infusion with a target of 100–150 mg/dl versus intermittent insulin bolus for blood glucose > 150 mg/dl. They found a significant reduction in risk for their composite endpoint of all-cause mortality, MI, and acute congestive heart failure (p = 0.01). Interestingly, there was no difference in their secondary endpoints, which included hyperglycemia (defined as a blood glucose > 150 mg/dl) or hypoglycemia, so it is unclear whether the outcomes observed were related to the intervention [57].
A Cochrane review from 2012 evaluated outcomes of intensive versus conventional glycemic control on 1403 patients undergoing surgery and found that there was no significant difference in all-cause mortality, infectious complications, cardiovascular events, or renal failure; however, there was a 6.9-fold increased risk of hypoglycemic episodes [61]. A pooled blood glucose mean for the intervention and control group could not be calculated in this meta-analysis due to heterogeneity. Among included studies, the mean blood glucose in the intensive group ranged from 99 to 203 mg/dl, although most means were less than 152 mg/dl. The mean blood glucose in the conventional group ranged from 163 to 243 mg/dl, with most means falling between 160 and 178 mg/dl. The mean difference between the intensive and control group ranged from − 31 to − 13 mg/dl. Another systematic review found that moderate perioperative glucose control with a goal of 150–200 mg/dl was associated with reduced risk of post-operative mortality and stroke when compared with a liberal target of > 200 mg/dl [62]. No additional benefit was observed in those with blood glucose less than 150 mg/dl.
The 2018 Standards of Medical Care in Diabetes recommend a target glucose of 80–180 mg/dl in the perioperative period. Metformin and other non-insulin glucose-lowering medications should be held the morning of surgery. For insulin-requiring patients, dose reductions in basal insulin are typically recommended while NPO to minimize hypoglycemia risk. Patients receiving NPH should be given a half dose the day of surgery, while those on long-acting basal analogs or insulin pumps should have a 20–40% reduction in their basal dose or rate [63, 64••]. Short-acting insulin is typically held as the patient will be fasting, unless correctional insulin is required for hyperglycemia [64••]. A useful web-based tool developed by the University of California San Francisco Medical Center provides specific pre-operative dose adjustment recommendations for glucose-lowering medications [65].
Given the lack of evidence for specific guidelines, glucose management in the perioperative period mirrors recommendations of the general inpatient populations (see Inpatient Management of Hyperglycemia in stroke section above). Special consideration should be made to recognize factors that may impact glycemic management including stress hyperglycemia, changes in nutritional status post-operatively, fluctuating renal status in the setting of fluid shifts or blood loss intraoperatively, and inconspicuous symptoms of hypoglycemia in the setting of altered mental status from anesthesia or pain medications. Immobilization, which often occurs in the inpatient setting, especially in those with amputation or lower extremity procedures, can result in worsening hyperglycemia in those with diabetes. These factors should be considered when determining the antihyperglycemic regimen in the hospital as well as at discharge as dose adjustments may be required. In preparation for transition to the outpatient setting, one should also consider possible adjuvant therapies that may impact glucose control. Hyperbaric oxygen therapy, which can be used as an adjuvant therapy for non-healing foot ulcers, has uncommonly been associated with hypoglycemia [66]. Although the exact mechanism is unknown, some studies have shown an increase activity in insulin receptor sites and upregulation of PPAR-γ in skeletal muscle resulting in increased insulin sensitivity. [67] If this occurs, one should consider permissive hyperglycemia during these sessions. Given the complexity of diabetes management in those with active complications of PVD and diabetes, it is recommended that outpatient follow-up occur within a multidisciplinary diabetic foot or limb salvage clinic whenever possible [68].
Conclusions
Hyperglycemia occurs frequently in the setting of stroke and peripheral vascular disease and has been associated with poor clinical outcomes. However, tight glycemic control (e.g., 70–110 mg/dl) does not appear to be justified given the increased risk of hypoglycemia and lack of evidence of clinical benefit. Since the completion of many of these studies, there has been a shift in our standard of care to less extreme inpatient glycemic targets; therefore, additional studies are needed to evaluate whether moderately strict blood glucose goals (e.g., 110–140 mg/dl) or conversely permissive hyperglycemia (e.g., 180–200 mg/dl) would be of benefit to this patient population.
At this time, inpatient hyperglycemia guidelines tailored specifically to acute stroke and perioperative management in PVD are lacking. It is recommended that providers follow general inpatient hyperglycemia management guidelines, keeping in mind that both these populations may have unique factors that should be considered during inpatient management and at hospital discharge.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major Importance
Galindo RJ, Fayfman M. Perioperative management of hyperglycemia and diabetes in cardiac surgery patients. Endocrinol Metab Clin North Am. 2018;47:203–22. https://doi.org/10.1016/J.ECL.2017.10.005.
Heyboer M, Sharma D, Santiago W, McCulloch N, McCulloch N. Hyperbaric oxygen therapy: side effects defined and quantified. Adv Wound Care. 2017;6:210–24. https://doi.org/10.1089/wound.2016.0718.
Baker L, Juneja R, Bruno A. Management of hyperglycemia in acute ischemic stroke. Curr Treat Options Neurol. 2011;13:616–28. https://doi.org/10.1007/s11940-011-0143-8.
Shimoyama T, Kimura K, Uemura J, Saji N, Shibazaki K. Elevated glucose level adversely affects infarct volume growth and neurological deterioration in non-diabetic stroke patients, but not diabetic stroke patients. Eur J Neurol. 2014;21:402–10. https://doi.org/10.1111/ene.12280.
Pulsinelli WA, Levy DE, Sigsbee B, Scherer P, Plum F. Increased damage after ischemic stroke in patients with hyperglycemia with or without established diabetes mellitus. Am J Med. 1983;74:540–4. https://doi.org/10.1016/0002-9343(83)91007-0.
Parsons MW, Barber PA, Desmond PM, Baird TA, Darby DG, Byrnes G, et al. Acute hyperglycemia adversely affects stroke outcome: a magnetic resonance imaging and spectroscopy study. Ann Neurol. 2002;52:20–8. https://doi.org/10.1002/ana.10241.
Bruno A, Levine SR, Frankel MR, Brott TG, Lin Y, Tilley BC, et al. Admission glucose level and clinical outcomes in the NINDS rt-PA Stroke Trial. Neurol Am Acad Neurol. 2002;59:669–74. https://doi.org/10.1212/WNL.59.5.669.
Ahmed N, Dávalos A, Eriksson N, Ford GA, Glahn J, Hennerici M, et al. Association of admission blood glucose and outcome in patients treated with intravenous thrombolysis: results from the Safe Implementation of Treatments in Stroke International Stroke Thrombolysis Register (SITS-ISTR). Arch Neurol. 2010;67:1123–30. https://doi.org/10.1001/archneurol.2010.210.
Jørgensen H, Nakayama H, Raaschou HO, Olsen TS. Stroke in patients with diabetes. The Copenhagen Stroke Study. Stroke American Heart Association. Inc. 1994;25:1977–84. https://doi.org/10.1161/01.STR.25.10.1977.
Golden SH, Hill-Briggs F, Williams K, Stolka K, Mayer RS. Management of diabetes during acute stroke and inpatient stroke rehabilitation. Arch Phys Med Rehabil. 2005;86:2377–84. https://doi.org/10.1016/J.APMR.2005.07.306.
Williams LS, Rotich J, Qi R, Fineberg N, Espay A, Bruno A, et al. Effects of admission hyperglycemia on mortality and costs in acute ischemic stroke. Neurol Am Acad Neurol. 2002;59:67–71. https://doi.org/10.1212/WNL.59.1.67.
Capes SE, Hunt D, Malmberg K, Pathak P, Gerstein HC. Stress hyperglycemia and prognosis of stroke in nondiabetic and diabetic patients: a systematic overview. Stroke. 2001;32:2426–32.
Goyal N, Kaur R, Sud A, Ghorpade N, Gupta M. Non diabetic and stress induced hyperglycemia [SIH] in orthopaedic practice what do we know so far? J Clin Diagn Res. 2014;8:LH01–3. https://doi.org/10.7860/JCDR/2014/10027.5022.
Kerby JD, Griffin RL, MacLennan P, Rue LW. Stress-induced hyperglycemia, not diabetic hyperglycemia, is associated with higher mortality in trauma. Ann Surg. 2012;256:446–52. https://doi.org/10.1097/SLA.0b013e3182654549.
Rau C-S, Wu S-C, Chen Y-C, Chien P-C, Hsieh H-Y, Kuo P-J, et al. Higher mortality in trauma patients is associated with stress-induced hyperglycemia, but not diabetic hyperglycemia: a cross-sectional analysis based on a propensity-score matching approach. Int J Environ Res Public Health. 2017;14:1161. https://doi.org/10.3390/ijerph14101161.
Sleiman I, Morandi A, Sabatini T, Ranhoff A, Ricci A, Rozzini R, et al. Hyperglycemia as a predictor of in-hospital mortality in elderly patients without diabetes mellitus admitted to a sub-intensive care unit. J Am Geriatr Soc. 2008;56:1106–10. https://doi.org/10.1111/j.1532-5415.2008.01729.x.
Lazaros G, Tsiachris D, Vlachopoulos C, Chrysohoou C, Milkas A, Papageorgiou N, et al. Distinct association of admission hyperglycemia with one-year adverse outcome in diabetic and non-diabetic patients with acute ST-elevation myocardial infarction. Hell J Cardiol. 54:119–25.
Hjalmarsson C, Manhem K, Bokemark L, Andersson B. The role of prestroke glycemic control on severity and outcome of acute ischemic stroke. Stroke Res Treat. 2014;2014:694569–6. https://doi.org/10.1155/2014/694569.
Olsen TS. Blood glucose in acute stroke. Expert Rev Neurother. 2009;9:409–19. https://doi.org/10.1586/14737175.9.3.409.
Laird E. Blood glucose monitoring and management in acute stroke care. Nurs Stand. 2014;28:52–6. https://doi.org/10.7748/ns2014.01.28.19.52.e8163.
Kagansky N, Levy S, Knobler H. The role of hyperglycemia in acute stroke. Arch Neurol. 2001;58:1209–12. https://doi.org/10.1001/archneur.58.8.1209.
Alvarez-Sabín J, Molina CA, Montaner J, Arenillas JF, Huertas R, Ribo M, et al. Effects of admission hyperglycemia on stroke outcome in reperfused tissue plasminogen activator–treated patients. Stroke. 2003;34:1235–41. https://doi.org/10.1161/01.STR.0000068406.30514.31.
Quinn TJ, Lees KR. Hyperglycaemia in acute stroke—to treat or not to treat. Cerebrovasc Dis. 2009;27(Suppl 1):148–55. https://doi.org/10.1159/000200453.
Yoon J-E, Sunwoo J-S, Kim JS, Roh H, Ahn M-Y, Woo H-Y, et al. Poststroke glycemic variability increased recurrent cardiovascular events in diabetic patients. J Diabetes Complicat. 2017;31:390–4. https://doi.org/10.1016/J.JDIACOMP.2016.11.014.
Allport L, Baird T, Butcher K, Macgregor L, Prosser J, Colman P, et al. Frequency and temporal profile of poststroke hyperglycemia using continuous glucose monitoring. Diabetes Care. 2006;29:1839–44. https://doi.org/10.2337/dc06-0204.
Paolino AS, Garner KM. Effects of hyperglycemia on neurologic outcome in stroke patients. J Neurosci Nurs. 2005;37:130–5. https://doi.org/10.1161/hs1001.096194.
Levetan CS, Passaro M, Jablonski K, Kass M, Ratner RE. Unrecognized diabetes among hospitalized patients. Diabetes Care. 1998;21:246–9. https://doi.org/10.2337/DIACARE.21.2.246.
Umpierrez GE, Isaacs SD, Bazargan N, You X, Thaler LM, Kitabchi AE. Hyperglycemia: an independent marker of in-hospital mortality in patients with undiagnosed diabetes. J Clin Endocrinol Metab. 2002;87:978–82. https://doi.org/10.1210/jcem.87.3.8341.
Levetan CS. Effect of hyperglycemia on stroke outcomes. Endocr Pract. 2004;10:34–9. https://doi.org/10.4158/EP.10.S2.34.
Klingbeil KD, Koch S, Dave KR. Potential link between post-acute ischemic stroke exposure to hypoglycemia and hemorrhagic transformation. Int J Stroke. 2017;0:174749301774379. https://doi.org/10.1177/1747493017743797.
Jin C, Li G, Rexrode KM, Gurol ME, Yuan X, Hui Y, et al. Prospective study of fasting blood glucose and intracerebral hemorrhagic risk. Stroke. 2018;49:27–33. https://doi.org/10.1161/STROKEAHA.117.019189.
Brutsaert E, Carey M, Zonszein J. The clinical impact of inpatient hypoglycemia. J Diabetes Complicat. 2014;28:565–72. https://doi.org/10.1016/J.JDIACOMP.2014.03.002.
Silverman IE, Restrepo L, Mathews GC. Poststroke Seizures. Arch Neurol. 2002;59:195–201. https://doi.org/10.1001/archneur.59.2.195.
Turchin A, Matheny ME, Shubina M, Scanlon JV, Greenwood B, Pendergrass ML. Hypoglycemia and clinical outcomes in patients with diabetes hospitalized in the general ward. Diabetes Care. 2009;32:1153–7. https://doi.org/10.2337/dc08-2127.
Akirov A, Grossman A, Shochat T, Shimon I. Mortality among hospitalized patients with hypoglycemia: insulin related and noninsulin related. J Clin Endocrinol Metab. 2017;102:416–24. https://doi.org/10.1210/jc.2016-2653.
Bellolio MF, Gilmore RM, Ganti L. Insulin for glycaemic control in acute ischaemic stroke. Cochrane Database Syst Rev. 2014; https://doi.org/10.1002/14651858.CD005346.pub4.
Bruno A, Durkalski VL, Hall CE, Juneja R, Barsan WG, Janis S, et al. The Stroke Hyperglycemia Insulin Network Effort (SHINE) trial protocol: a randomized, blinded, efficacy trial of standard vs. intensive hyperglycemia management in acute stroke. Int J Stroke. 2014;9:246–51. https://doi.org/10.1111/ijs.12045.
Johnston K. Stroke Hyperglycemia Insulin Network Effort (SHINE) Trial (SHINE) [Internet]. U.S Natl. Libr. Med. 2017. Doi: https://clinicaltrials.gov/ct2/show/NCT01369069
Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. 2018 Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018;49:eXXX–X. https://doi.org/10.1161/STR.0000000000000158.
Moghissi ES, Korytkowski MT, DiNardo M, Einhorn D, Hellman R, Hirsch IB, et al. American Association of Clinical Endocrinologists and American Diabetes Association consensus statement on inpatient glycemic control. Diabetes Care. 2009:1119–31. https://doi.org/10.2337/dc09-9029.
Umpierrez GE, Hellman R, Korytkowski MT, Kosiborod M, Maynard GA, Montori VM, et al. Management of hyperglycemia in hospitalized patients in non-critical care setting: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2012;97:16–38. https://doi.org/10.1210/jcem.97.1.zeg16a.
McGrath RT, Hocking SL, Priglinger M, Day S, Herkes GK, Krause M, et al. Rationale and design of Short-Term EXenatide therapy in Acute ischaemic Stroke (STEXAS): a randomised, open-label, parallel-group study. BMJ Open. 2016;6:e008203. https://doi.org/10.1136/bmjopen-2015-008203.
Daly SC, Chemmanam T, Loh P-S, Gilligan A, Dear AE, Simpson RW, et al. Exenatide in Acute Ischemic Stroke. Int J Stroke. 2013;8:E44. https://doi.org/10.1111/ijs.12073.
Singh S, Hamdy S. Dysphagia in stroke patients. Postgrad Med J. 2006;82:383–91. https://doi.org/10.1136/pgmj.2005.043281.
Wolpert HA, Atakov-Castillo A, Smith SA, Steil GM. Dietary fat acutely increases glucose concentrations and insulin requirements in patients with type 1 diabetes: implications for carbohydrate-based bolus dose calculation and intensive diabetes management. Diabetes Care. 2013;36:810–6. https://doi.org/10.2337/dc12-0092.
Mathioudakis N, Everett E, Golden SH. Prevention and management of insulin-associated hyoglycemia in hospitalized patients. Endocr Pract. 2016;22:959–69. https://doi.org/10.4158/EP151119.OR.
Huysman F, Mathieu C. Diabetes and peripheral vascular disease. Acta Chir Belg. 2009;109:587–94. https://doi.org/10.1080/00015458.2009.11680493.
Kannel WB, McGee DL. Update on some epidemiologic features of intermittent claudication: the Framingham Study. J Am Geriatr Soc. 1985;33:13–8.
Jude EB, Eleftheriadou I, Tentolouris N. Peripheral arterial disease in diabetes—a review. Diabet Med. 2010;27:4–14. https://doi.org/10.1111/j.1464-5491.2009.02866.x.
McGirt MJ, Woodworth GF, Brooke BS, Coon AL, Jain S, Buck D, et al. Hyperglycemia independently increases the risk of perioperative stroke, myocardial infarction, and death after carotid endarterectomy. Neurosurgery. 2006;58:1066–73. https://doi.org/10.1227/01.NEU.0000215887.59922.36.
Davies MG, Saad WE. Impact of elevated perioperative fasting blood glucose on carotid artery stenting outcomes. Ann Vasc Surg. 2014;28:1885–91. https://doi.org/10.1016/J.AVSG.2014.07.001.
Malmstedt J, Wahlberg E, Jörneskog G, Swedenborg J. Influence of perioperative blood glucose levels on outcome after infrainguinal bypass surgery in patients with diabetes. Br J Surg. 2006;93:1360–7. https://doi.org/10.1002/bjs.5466.
Steely AM, Smith L, Callas PW, Nathan MH, Lahiri JE, Stanley AC, et al. Prospective study of postoperative glycemic control with a standardized insulin infusion protocol after infrainguinal bypass and open abdominal aortic aneurysm repair. Ann Vasc Surg. 2017;44:211–20. https://doi.org/10.1016/j.avsg.2017.04.020.
• Vogel TR, Smith JB, Kruse RL. The association of postoperative glycemic control and lower extremity procedure outcomes. J Vasc Surg. 2017;66:1123–32. https://doi.org/10.1016/J.JVS.2017.01.053. This study highlights the range of complications that has been associated with post-operative hyperglycemia and odds of these complications after lower extremity vascular surgery.
Nayak RK, Kirketerp-Møller K. Preoperative blood glucose and prognosis in diabetic patients undergoing lower extremity amputation. Dan Med J. 2016;63
Arya S, Binney ZO, Khakharia A, Long CA, Brewster LP, Wilson PW, et al. High hemoglobin A1c associated with increased adverse limb events in peripheral arterial disease patients undergoing revascularization. J Vasc Surg. 2018;67:217–228.e1. https://doi.org/10.1016/j.jvs.2017.06.101.
Subramaniam B, Panzica PJ, Novack V, Mahmood F, Matyal R, Mitchell JD, et al. Continuous perioperative insulin infusion decreases major cardiovascular events in patients undergoing vascular surgery. Anesthesiology. 2009;110:970–7. https://doi.org/10.1097/ALN.0b013e3181a1005b.
Feringa HHH, Vidakovic R, Karagiannis SE, Dunkelgrun M, Elhendy A, Boersma E, et al. Impaired glucose regulation, elevated glycated haemoglobin and cardiac ischaemic events in vascular surgery patients. Diabet Med. 2008;25:314–9. https://doi.org/10.1111/j.1464-5491.2007.02352.x.
Vriesendorp TM, Morélis QJ, DeVries JH, Legemate DA, Hoekstra JBL. Early post-operative glucose levels are an independent risk factor for infection after peripheral vascular surgery. A retrospective study. Eur J Vasc Endovasc Surg. 2004;28:520–5. https://doi.org/10.1016/J.EJVS.2004.08.006.
Ramos M, Khalpey Z, Lipsitz S, Steinberg J, Panizales MT, Zinner M, et al. Relationship of perioperative hyperglycemia and postoperative infections in patients who undergo general and vascular surgery. Trans Meet Am Surg Assoc. 2008;126:228–34. https://doi.org/10.1097/SLA.0b013e31818990d1.
Buchleitner AM, Martínez-Alonso M, Hernández M, Solà I, Mauricio D. Perioperative glycaemic control for diabetic patients undergoing surgery. Cochrane Database Syst Rev. 2012; https://doi.org/10.1002/14651858.CD007315.pub2.
Sathya B, Davis R, Taveira T, Whitlatch H, Wu W-C. Intensity of peri-operative glycemic control and postoperative outcomes in patients with diabetes: a meta-analysis. Diabetes Res Clin Pract. 2013;102:8–15. https://doi.org/10.1016/J.DIABRES.2013.05.003.
American Diabetes Association AD. 14. Diabetes Care in the Hospital:Standards of Medical Care in Diabetes-2018. Diabetes Care. 2018;41:S144–51. https://doi.org/10.2337/dc18-S014.
•• Duggan EW, Carlson K, Umpierrez GE. Perioperative Hyperglycemia Management. Anesthesiology. 2017;126:547–60. https://doi.org/10.1097/ALN.0000000000001515. This comprehensive review paper thoroughly describes the impact of surgical stress on glycemic control and articulates in detail how to manage hyperglycemia preoperatively and post-operatively.
Hirsch J, Rushakoff R, Robinowitz D, Rouine-Rap K, Windham H. UCSF Diabetes Pre-Op Managment [Internet]. 2017. Doi: http://ucsfprod.logicnets.com/UCSF/packages/DiabetesPreOp_20170417/logicnets.lns?_session=54B6BE07F2F011
Jokinen-Gordon H, Barry RC, Watson B, Covington DS. A retrospective analysis of adverse events in hyperbaric oxygen therapy (2012-2015). Adv Skin Wound Care. 2017;30:125–9. https://doi.org/10.1097/01.ASW.0000508712.86959.c9.
Nwafor TS, Collins N. Managing low blood glucose levels in patients undergoing hyperbaric oxygen therapy. Ostomy Wound Manage. 2014;60:12–5.
Everett E, Mathioudakis N. Update on management of diabetic foot ulcers. Ann N Y Acad Sci. 2018;1411:153–65. https://doi.org/10.1111/nyas.13569.
Funding
This study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). EE is supported by the Clinical Research and Epidemiology in Diabetes and Endocrinology Training grant (T32 DK062707). NM is supported by NIDDK K23DK111986-01.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Estelle Everett and Nestoras Mathioudakis declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Hospital Management of Diabetes
Rights and permissions
About this article
Cite this article
Everett, E., Mathioudakis, N. Inpatient Glycemic Management of Non-cardiac CVD: Focus on Stroke and PVD. Curr Diab Rep 18, 49 (2018). https://doi.org/10.1007/s11892-018-1026-0
Published:
DOI: https://doi.org/10.1007/s11892-018-1026-0