Abstract
Purpose of Review
Obesity has grown at an alarming rate in children and adolescents. Concurrently, consumption on sugar-sweetened beverages (SSBs) also rose significantly. This review provides an overview of obesity and type 2 diabetes mellitus (T2DM) related to SSBs and current policies restricting SSBs in schools, school-based interventions, and taxation on reducing SSB intake and obesity. We also discuss challenges of and future steps for these initiatives.
Recent Findings
Clinical and epidemiological studies suggest a strong association between SSB intake and obesity and T2DM. School food policies have been initiated at federal, state, and local levels. School-based interventions have shown positive effects on SSB intake and obesity reduction. Taxation on SSBs is promising in combating obesity and in generating revenue. Challenges towards compliance and implementation of the policies and programs exist.
Summary
The relationship between SSB and obesity and T2DM is a complex problem which requires comprehensive solutions. Continued efforts in restricting SSBs in schools are needed. Intervention programs should be tailored to age, gender, language, and culture and involve participation from families and local communities. Taxation can reduce SSB consumption by direct economic incentive, earmarking revenues to support healthy foods, and sending negative message. However, a higher tax rate may be necessary to have a measurable effect on weight.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of obesity tripled for children and adolescents in the USA in recent three decades [1]. Metabolic complications of obesity, such as type 2 diabetes mellitus (T2DM), are also emerging as serious health risks for children. One factor that may contribute rising obesity and T2DM is the steep rise in sugar-sweetened beverage (SSB) intake [2]. US children consume nearly twice as many calories from SSBs—beverages containing added caloric sweeteners, such as sodas, fruit drinks, spot drinks, and energy drinks [3] than they did 30 years ago, and now, SSBs is the single largest category of caloric intake in children [2]. With growing evidence linking SSBs to obesity and T2DM in children and adolescents, there is sufficient rationale to explore means of limiting SSB availability and accessibility, including school food policies, school-based intervention programs, and taxation to combat the epidemic. In this review, we outline health risks that are associated with SSB consumption, efforts to curb SSB consumption, obesity and T2DM, and the likely effectiveness of these efforts, especially among children and adolescents. We also discuss challenges of implementing the policies and programs and suggest future steps.
The Increased Obesity and SSB Consumption in Children and Adolescents
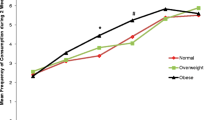
There is mounting evidence that the increase consumption of SSBs over time is related to the increased obesity levels among children and adolescent in the USA. During the past three decades, there has been a marked increase in the prevalence of obesity in US children and adolescents, with the prevalence rate tripled since 1980 [1]. Today, 19.6% of children aged 6–11 years and 18.1% of adolescents aged 12–19 years are obese [1]. The increased consumption of SSBs is parallel to the rising obesity rates [3]. Indeed, children are now consuming nearly twice as many calories from SSBs than they did 30 years ago [2]. By 1999–2004, children aged 2–18 years obtained more than 10% of their energy from SSBs, which is 175 kcal/day. Boys aged 13–18 years consume the most SSBs of all age and gender groups (an average of 357 kcal per day) [4] and that those at most risk of obesity, including African-Americans, Mexican Americans, and lower education and income populations, have the highest intake of SSBs [5]. Consumption patterns of the youngest children—toddlers to preschoolers are of particular concerns. Almost half (44%) of toddlers 1.5 to 2 years old consume a SSB on any given day [6]. That proportion rises to 70% of 2- to 5-year-olds consuming a SSB on a typical day [4].
Mechanisms Explaining the Relationship Between SSBs and Obesity and T2DM
Current evidence regarding SSBs’ effects on obesity and its common complication, T2DM, has pointed at the long-term public health consequences, given that these conditions early in life are likely antecedents to adult diseases. Scientists have proposed potential mechanisms for links between SSBs and obesity and T2DM. SSBs contribute to weight gain due to their high added sugar content, low satiety, and potential incomplete compensation for total energy leading to increased energy intake [7, 8]. In addition, because of their high amounts of rapidly absorbable carbohydrates such as various forms of sugar and high-fructose corn syrup, the primary sweeteners used in SSBs, and high quantities consumed, SSBs may increase T2DM. SSB-related risk of T2DM is independent from obesity. SSBs contribute to high dietary glycemic load which leads to inflammation, insulin resistance, and impaired Beta-cell function [8, 9].
Current Evidence of SSBs and Obesity and T2DM Among Children and Adolescents
Researchers have presented numerous epidemiological findings about the relationship between SSBs and obesity or T2DM in children and adolescents. Dubois et al. found that in over 2000 children age 2.5 years old followed for 3 years, regular consumers of SSBs between meals had a 2.4-fold greater odds of being overweight compared to non-consumers (P < 0.05) [10]. A prospective study involving middle-school students over the course of two academic years showed that the risk of becoming obese increased by 60% for every additional serving of SSB per day [11]. In a recent meta-analysis [12], a significant positive association between SSB intake and weight gain (0.08; 95% CI 0.03–0.13 kg) was reported. This result was supported by an earlier meta-analysis [13] and a systematic review [14]. Importantly, studies suggest that greater SSB consumption in childhood or adolescence predicted weight gain into adulthood [15, 16]. Obese children are more likely to become obese adults [17], further increasing their risks for higher rates of T2DM, heart diseases, and some cancers later in life. A recent large cohort study found that a child with obesity faces a 4-fold greater risk of being diagnosed with T2DM by age 25 than a counterpart who is normal weight [18•]. Another well-powered meta-analysis also found that individuals in the highest quantile of SSB intake (most often 1–2 servings/day) had a 26% greater risk of developing T2DM than those in the lowest quantile (none or < 1 serving/month). This suggests the independent effect of SSB intake on T2DM in addition to weight gain [8].
Efforts to Curb SSB Consumption–School Food Policies, School-Based Intervention Programs, and Taxation on SSBs
School Food Policies
The substantial increase in SSBs among children and adolescents and its strong relationship with obesity related diseases urge initiatives to limit and restrict the availability and accessibility of SSBs. Schools are an ideal venue to institute healthier beverages because they are responsible for administering at least one third of a child’s food intake during the school day, and they can function as educational and role models for healthier food choices [19]. Policies assuring healthy food choices in schools have been an area of long-standing interest [20]. Competitive foods in school environment have placed negative impact on children’s eating behaviors and weight outcomes [20]. Competitive foods are defined as foods and drinks sold from vending machines, school stores, and à la carte cafeteria lines other than meals from federally funded school meal programs in public schools [21]. The most common types of food offered in these venues are soft drinks, juices, juice drinks, chips, desserts, and candies, which are poor in nutrition but energy-dense [21].
Because of the increase in penetration of these competitive foods, federal, many states, and local governments have increased efforts to place limits on access to competitive foods including SSBs in schools. As part of the Child Nutrition and WIC Reauthorization Act of 2004, Congress required that school districts participating in the National School Lunch Program (NSLP), a federally assisted meal program operating in public and non-profit private schools and residential child care institution that provide balanced, low-cost, or free lunches to school children [22], develop wellness policies that addressed the nutritional quality of all foods available in schools, not just U.S. Drug and Administration (USDA) meals [23]. The Healthy, Hunger-Free Kids Act of 2010 gives the USDA authority to update standards for all foods and beverages served and sold in schools, including those sold in vending machines, school stores, and a à la carte items [23]. In February, 2013, the USDA released the proposed rules that would govern competitive foods [24]. The final rule should follow as a guide the standards for competitive foods set by the Institute of Medicine (IOM), which recommend limits on fat, sugar, calories, and serving sizes, as well as the most recent Dietary Guidelines for Americans [25]. In 2013, the Smart Snacks in School Standards were also established with the aim of decreasing competitive foods and beverages available at schools [26]. The standards apply to all competitive foods sold in students during the school day on all areas of the school campus, in all schools that participate in the NSLP and School Breakfast program (SBP) [26].
Many states update nutrition guidelines for foods and beverages that are provided in schools. According to a report from Trust for America’s Health, a non-profit, non-partisan organization conducting science-based public health research [27], 19 states set nutritional standards for school lunches, breakfasts, and snacks that are stricter than existing USDA requirements in 2009. Twenty-seven states have nutritional standards for competitive foods sold à la carte, in vending machines, in school stores, or in school bake sales. Twenty-nine states limit when and where competitive foods menu be sold beyond federal requirements [27].
At local level, school districts are seen as having the opportunity to institute more comprehensive policies than states. In 2003, elementary schools in Alaska and all schools in California implemented bans to soft drinks [20]. Several large school systems such as those in Philadelphia and Chicago have also placed restrictions on access to vending machines [28]. From the beginning of 2003, San Francisco Unified School District (SFUSD) developed district-wide nutrition policies that extend beyond the state Childhood Obesity Prevention Act, requiring elimination of foods not meeting the food minimal nutrition value, a federal nutrition standard that bans the sale of products such as artificially sweetened foods and foods that provide less than 5% of the recommended dietary intake of each of eight specified nutrients per serving [29].
School-Based Intervention Programs
School-based intervention programs have been shown to yield positive results in preventing and reducing obesity [30]. School is an ideal setting for programs targeting health dietary behaviors since children spend a major part of their day in school [31]. Systematic reviews on the effectiveness of school-based nutrition and fitness programs showed that school-based interventions are effective in increasing healthy behaviors [32,33,34], discouraging purchases and consumption of unhealthy foods [33, 34, 35•] and reducing caloric intakes and BMI [33, 34]. Coordinated Approach to Child Health (CATCH) is a successful example of school health promotion program that focused on supporting positive environmental influences to increase physical activity and improve healthy eating [36]. A 3-year follow-up study showed that students receiving CATCH intervention maintained a diet considerably lower in total fat and saturated fat and participated in more vigorous physical activities [34]. These findings reinforce the expectation that participation in a program like CATCH could contribute to better cardiovascular health as students mature [34]. Another innovative school program to improve cardiovascular health and lower the prevalence of obesity among students is Planet Health [36]. This 21-month interdisciplinary curriculum stressed the importance of decreasing television viewing, which contributes to obesity through both the sedentary act of television watching and exposure of viewers to relentless broadcast encouragement to consume high-calorie, high-fat, nutrient-poor foods [37]. The intervention showed a significant decrease in prevalence of obesity, an increase in fruit and vegetable consumption and less of an increased in daily calories consumed among girls participating in Planet Health [33]. Additional analyses also found that girls in this program were less likely to report weight control behavior disorders [38] or early menarche [39]. With respects to SSBs specially, evidence-based school wellness interventions have contributed to a decreased SSB intake among students in elementary, middle, and high schools [31]. Successful intervention programs often include a combination of educational, environmental and parental involvement strategies [40,41,42,43,44,45,46]. Some also stressed the importance of peer influence and peer or family support in behavioral change and weight management [41, 43, 45]. Innovative technologies, such as web-based lessons, were also used in intervention [44]. Components of these programs highlighted the sugar content of SSBs, addressed portion sizes and healthier alternatives to SSBs, and educated on reading nutrition labels and planning meals [40,41,42,43,44,45,46]. Table 1 provides a summary of school-based interventions that have significant impact on reducing SSBs in recent 10 years. We listed program name, location, year of publication, participants, sample size, program key features, behavioral theory used, and critical intervention components.
Taxation
Given the success in other public health areas such as tobacco, implementing a SSB tax to regulate conduct and improve health is now being seriously considered [47]. The economic downturn also makes taxation an attractive source of revenue [48]. The IOM states that the introduction of a tax to discourage the consumption of food products that are low in nutritional value like soft and energy drinks is a very promoting strategy for governments [49].
High profile taxes on SSBs have been introduced at the federal and state levels [50]. At the federal level, the SWEET Act was proposed in 2014 to place an excise tax on SSBs in proportion to the amount of sugar that they contain and designates that funds from that tax go “to the prevention, treatment, and research of diet-related health conditions” [51]. It is thought that the passing of this bill would serve as an alert to the consumer that is built into the price tag, instead of printed on the side of the cigarette package [48].
One way many states have tried to impact the obesity epidemic is by taxing junk foods [52]. In 2007, 34 states taxed soda sold in grocery stores and 39 states taxed soda sold through vending machines at mean rates of 3.4 and 4.0%, respectively [53]. In December 2008, former Gov. David Paterson of New York proposed an 18% “obesity tax” on SSBs. Although the proposal failed in legislation, it received national media attention [54•]. Also in 2008, Maine enacted legislation that would have taxed soft drinks at a rate of 0.42 per gallon of bottled or powered-based soft drinks and $4 per gallon of soft drink syrup [20]. In November 2016, Cook County, IL, which includes Chicago, was the largest jurisdiction in the USA to enact tax SSBs [55]. The tax imposed was at the rate of $0.01 per ounce on the retail sale of all SSBs in the County. However, both Maine and Cook County’s proposals encountered political opposition. Maine’s beverage tax was repealed in November 2008, and Cook County in October 2017 [20, 55].
Many believe the combination of taxing SSBs, while subsidizing healthy beverages has the potential to reduce obesity in children and adolescents [20, 56, 57]. Even though the current evidence of the relationship between SSB tax and weight outcomes is not strong due to the very low tax rates, findings in the literature suggest potential behavioral and health benefits of implementing such tax [57]. Systematic reviews have found that food taxes strongly influence consumption and indicated that imposing substantial taxes on energy dense foods is promising to improve health outcomes [58]. Additionally, economic modeling has been used to predict potential impact of taxes on SSB consumption [57]. Studies found that a 10% increase in price would lead to a decreased consumption to 7 to 17% among less frequent consumers and the highest consumers, respectively [59].
Beyond health benefits, taxation of SSB would also generate significant revenue, which is hoped to have impact on government actions and could be targeted towards obesity prevention and health promotion activities [56]. Further, taxation of SSB would also signify recognition by government of the serious health risks that associated with SSB consumption. A strong message acknowledging health risk of SSB can be sent by taxation [57].
Challenges
Although efforts to restrict children from accessing SSBs have received support from some politicians and health advocates, challenges towards compliance and implementation of the policies and programs exist [19, 60]. For example, despite the Congress’ requirement that school districts participating in the NSLP develop wellness policies to address nutritional quality of foods in schools, the content of the policies was left to local discretion—schools could restrict less nutritious competitive foods or not. Similarly, there were no requirements to assess compliance with any policies established [60]. Additionally, the restrictions are usually not easy to be implemented in high schools because of logistic difficulties, including many students obtaining meals off campus [19]. In addition, concern about losing revenues generated by the sale of these items, particularly in support of high school sports and other programs, led to lobbying and other negative influences, such as protests and letter writing, by school districts and the food industry [19].
Some also critique that the benefits of the school food policies can be limited by the type and amount of drinks that substitute SSBs [52]. If a child offsets her sodas by consuming other high calories beverages such as sports drinks, she may not receive benefits from the SSB restriction policies. Many beverages such as fruit juice and reduced fat milk, even though presumably more nutritious, would have a similar number of calories per serving as SSBs [56]. Furthermore, there is a concern that restrictions of SSBs in school during the school day could redirect the place and time of SSB purchase, therefore diminishing the benefits of reducing consumption and weight [61]. Finally, SSB’s contribution to children’s and adolescent’s total calories in food items acquired at school is smaller than at home [4]. Because of these countervailing factors, current evidence of the impact of the school policies such as implementing vending machine ban to reduce SSB consumption seems weak [62, 63]. Full evidence, however, should not be a barrier for action. Any action with respect to policies to address obesity will require monitoring and evaluation of intended and unintended consequences [57]. Because of the complexity of the food environment, more innovative and rigorous research is needed to assess the policies’ impact in the long run.
Limitations for current school-based interventions exist too. Many programs apply same intervention strategies to both girls and boys [64]. However, research suggests that girls and boys may not respond comparably to a given intervention. Girls may respond better to educational components grounded based upon social learning, while boys may be more influenced by structural and environmental components facilitating improved diet intake [64]. Furthermore, many programs targeted younger youth aged 7–10 years old. Older youth should also be desirable for future programs since studies found positive outcomes in older groups [65]. These positive outcomes are possibly due to older children’s increased control over food choices and leisure activities, greater concerns about weight and appearance, and peer-group mediated changes in behavior [64]. Additionally, many studies stressed the importance of cultural considerations to the success of programs [66, 67]. Factors such as language, lifestyle, and beliefs are potential barriers for minority populations who are at higher risk of obesity [68]. Apart from gender, age, and cultural factors, duration of intervention, quality of education or diet programs, the adherence rate of schoolchildren to those interventions, and involvement of school teachers, staffs, and families [69, 70] can determine the success of a program and should be considered in design and implementation of an intervention program. Further, at present, there is insufficient evidence to provide strong guidance as to the cost-effectiveness of the school-based intervention programs due to limited number of published studies as well as methodological concerns that limit the validity of and comparability between those identified [64].
Taxation on SSBs also faces strong challenges. First of all, there is the opposition from the beverage industry. Fear for sale declines, the beverage industry has created Americans against Food Taxes, just like the tobacco industry fought policy changes by creating front groups with names that suggested community involvements [56]. Opponents also argue that the direct effect of taxation on weight outcomes is less conclusive; therefore, the benefit of SSB taxation is questionable [57]. The lack of strong evidence of SSB taxation and weight is due to past studies considered relatively small variations in tax rates that applied to a limited set of SSBs (i.e., mainly sodas). Powell and Chaloupk [71] suggested that substantial tax increases will be necessary to have potent effects. In fact, Andreyev et al. [59] estimated that a tax increase at 20% of current prices would reduce consumption by between 16 and 20%, which would translate into a reduction of 36–45 kcal in youth, assuming that they have average intake of 225 kcal [4]. Moreover, previous studies have found that youth who are overweight and from low-SES background are particularly sensitive to food prices, suggesting that high SSB taxes may generate greater impact on these high-risk groups [72]. Therefore, to expect a significant impact of SSB taxation on weight outcome, a tax with higher rates that apply to a broader range of SSBs should be considered.
Future Steps
School districts and states should be encouraged to strengthen efforts to update their own nutritional guidelines for competitive products and continue restricting unhealthy items including SSBs within and outside schools. Adding healthier competitive foods and beverages would not lead to loss in revenues [73]. In fact, as reported in previous studies, it increases participation in the NSLP and attract new revenue [19, 74]. Also, offering healthier foods in competitive food venues could help to reinforce practices encouraged by school-based nutrition education [75].
With regard to school-based interventions, programs are recommended to be tailored according to age, gender, language, and culture [76]. Well-designed evaluation tools that include both short- and long-term assessments, valid analysis of behavioral and weight outcomes, and a discussion of cost-effectiveness analysis should all be taken into account. Intervention component that involve participation from teachers, parents, and a broader local community should also be given increased attention [32].
The broader benefits of taxation on SSBs must be recognized despite the insufficient evidence demonstrating its direct link with obesity reduction. SSB taxes may be particularly useful in reducing obesity if they are used as one aspect of a larger, more comprehensive policy approach that aims to redirect consumers away from caloric sweeteners and towards more healthful alternatives such as water or food without added sweeteners [77]. Researchers suggest dedicating at least half of the revenue generated from a SSB tax to programs that support health promotion initiatives and further transform the food environment to a milieu that promotes health food and beverage choices [57]. This could include promoting sale and consumption of healthier products, such as through subsidizing fruit and vegetables or investing in health school universal meal or snack programs [57].
Conclusions
SSBs and its relationship with obesity and T2DM is a complex problem, which requires comprehensive solutions that address different levels of the environment [35]. Besides initiatives discussed above, other prominent strategies in reducing SSB intake and obesity and T2DM include family-based ones, such as parents/children education [35]; community-based ones, such as zoning to restrict fast food outlets that provide a large volume of SSBs [78]; food industry-based ones, such as calorie labeling and value sizing [79]; and broad, societal ones, such as regulating SSB advertising and marketing [80]. A collective effort and timely action is necessary to combat the obesity epidemic. If we do nothing to address the issue, one in three children today will develop T2DM in their lifetime; for children of color, the risk is one in two [54]. By reducing SSB intake and crafting a healthier food environment, we can help children to achieve and maintain healthy weight.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999-2010. JAMA. 2012;307(5):483–90.
Popkin BM. Patterns of beverage use across the lifecycle. Physiol Behav. 2010;100(1):4–9.
Johnson RK, Appel LJ, Brands M, Howard BV, Lefevre M, Lustig RH, et al. Dietary sugars intake and cardiovascular health: a scientific statement from the American Heart Association. Circulation. 2009;120(11):1011–20.
Wang YC, Bleich SN, Gortmaker SL. Increasing caloric contribution from sugar-sweetened beverages and 100% fruit juices among US children and adolescents, 1988-2004. Pediatrics. 2008;121(6):e1604–14.
Bleich SN, Wang YC, Wang Y, Gortmaker SL. Increasing consumption of sugar-sweetened beverages among US adults: 1988-1994 to 1999-2004. Am J Clin Nutr. 2009;89(1):372–81.
Fox MK, Pac S, Devaney B, Jankowski L. Feeding infants and toddlers study: what foods are infants and toddlers eating? J Am Diet Assoc. 2004;104(1 Suppl 1):s22–30.
DiMeglio DP, Mattes RD. Liquid versus solid carbohydrate: effects on food intake and body weight. Int J Obes Relat Metab Disord. 2000;24(6):794–800.
Malik VS, Popkin BM, Bray GA, Després J-P, Willett WC, Hu FB. Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes. A Meta-Analysis. 2010;33(11):2477–83.
Schulze MB, Liu S, Rimm EB, Manson JE, Willett WC, Hu FB. Glycemic index, glycemic load, and dietary fiber intake and incidence of type 2 diabetes in younger and middle-aged women. Am J Clin Nutr. 2004;80(2):348–56.
Dubois L, Farmer A, Girard M, Peterson K. Regular sugar-sweetened beverage consumption between meals increases risk of overweight among preschool-aged children. J Am Diet Assoc. 2007;107(6):924–34. discussion 34-5
Ludwig DS, Peterson KE, Gortmaker SL. Relation between consumption of sugar-sweetened drinks and childhood obesity: a prospective, observational analysis. Lancet. 2001;357(9255):505–8.
Malik VS, Willett WC, Hu FB. Sugar-sweetened beverages and BMI in children and adolescents: reanalyses of a meta-analysis. Am J Clin Nutr. 2009;89(1):438–9. author reply 9-40
Vartanian LR, Schwartz MB, Brownell KD. Effects of soft drink consumption on nutrition and health: a systematic review and meta-analysis. Am J Public Health. 2007;97(4):667–75.
Olsen NJ, Heitmann BL. Intake of calorically sweetened beverages and obesity. Obes Rev. 2009;10(1):68–75.
Nissinen K, Mikkila V, Mannisto S, Lahti-Koski M, Rasanen L, Viikari J, et al. Sweets and sugar-sweetened soft drink intake in childhood in relation to adult BMI and overweight. The Cardiovascular Risk in Young Finns Study. Public Health Nutr. 2009;12(11):2018–26.
Viner RM, Cole TJ. Who changes body mass between adolescence and adulthood? Factors predicting change in BMI between 16 year and 30 years in the 1970 British Birth Cohort. Int J Obes. 2006;30(9):1368–74.
Freedman DS, Khan LK, Serdula MK, Dietz WH, Srinivasan SR, Berenson GS. The relation of childhood BMI to adult adiposity: the Bogalusa Heart Study. Pediatrics. 2005;115(1):22–7.
• Abbasi A, Juszczyk D, van Jaarsveld CHM, Gulliford MC. Body mass index and incident type 1 and type 2 diabetes in children and young adults: a retrospective cohort study. J Endoc Soc. 2017;1(5):524–37. A new study adds evidence that children with obesity face a significantly higher odds of having type 2 diabetes later in life.
Wojcicki JM, Heyman MB. Healthier choices and increased participation in a middle school lunch program: effects of nutrition policy changes in San Francisco. Am J Public Health. 2006;96(9):1542–7.
Fletcher JM, Frisvold D, Tefft N. Taxing soft drinks and restricting access to vending machines to curb child obesity. Health Aff (Millwood). 2010;29(5):1059–66.
U.S. General Accounting Office. School meal programs: competitive foods are available in many schools; actions taken to restrict them differ by state and locality. Washington, D.C.: U.S. 2004.
U.S. Department of Agriculture, Food and Nutrition Service. National School Lunch Program (NSLP). Cited Feberary 20, 2018. Available at https://www.fns.usda.gov/nslp/national-school-lunch-program-nslp
“S. 2507 —108th Congress: Child Nutrition and WIC Reauthorization Act of 2004.” www.GovTrack.us. 2004. Cited February 2, 2018. Available at https://www.govtrack.us/congress/bills/108/s2507
Chriqui JF, Resnick, E, Schneider L, et al. School district wellness policies: evaluating progress and potential for improving children’s health five years after the federal mandate. School years 2006–07 through 2010-11. Chicago, IL: Bridging the Gap, Health Policy Center, Institute for Health Research and Policy, University of Illinois at Chicago; 2013.
Institute of Medicine. Nutrition standards for foods in schools: leading the way toward healthier youth. Washington, DC: The National Academies Press; 2007.
U.S. Department of Agriculture, Office of Communications, Agriculture Secretary Vilsack highlights new “smart snacks in school” standards; will ensure school vending machines, snack bars include healthy choices; 2013. Cited Feberary 2, 2018. Available at https://www.usda.gov/media/press-releases/2013/06/27/agriculture-secretary-vilsack-highlights-new-smart-snacks-school
Jeffrey Levi SV, Richardson L, St. Laurent R, Segal LM. F as in fat: how obesity policies are failing in America. In: Trust for America's health; 2009.
Story M, Kaphingst KM, French S. The role of schools in obesity prevention. Futur Child. 2006;16(1):109–42.
San Francisco Unified School District. SFUSD Student Nutrition and Physical Fitness Plan Time: Revised. In: District SFUS, editor. San Francisco 2003.
Veugelers PJ, Fitzgerald AL. Effectiveness of school programs in preventing childhood obesity: a multilevel comparison. Am J Public Health. 2005;95(3):432–5.
Tipton JA. Reducing sugar-sweetened beverage intake among students: school-based programs and policies that work. NASN Sch Nurse. 2016;31(2):102–10.
Budd GM, Volpe SL. School-based obesity prevention: research, challenges, and recommendations. J Sch Health. 2006;76(10):485–95.
Gortmaker SL, Peterson K, Wiecha J, Sobol AM, Dixit S, Fox MK, et al. Reducing obesity via a school-based interdisciplinary intervention among youth: Planet Health. Arch Pediatr Adolesc Med. 1999;153(4):409–18.
Nader PR, Stone EJ, Lytle LA, Perry CL, Osganian SK, Kelder S, et al. Three-year maintenance of improved diet and physical activity: the CATCH cohort. Child and Adolescent Trial for Cardiovascular Health. Arch Pediatr Adolesc Med. 1999;153(7):695–704.
• Zhang Q, Liu S, Liu R, Xue H, Wang Y. Food policy approaches to obesity prevention: an international perspective. Curr Obes Rep. 2014;3(2):171–82. This paper provides a comprehensive overview of the recent obesity prevention-related food policies worldwide.
Franks A, Kelder SH, Dino GA, Horn KA, Gortmaker SL, Wiecha JL, et al. School-based programs: lessons learned from CATCH, Planet Health, and Not-On-Tobacco. Prev Chronic Dis. 2007;4(2):A33.
Epstein LH, Paluch RA, Consalvi A, Riordan K, Scholl T. Effects of manipulating sedentary behavior on physical activity and food intake. J Pediatr. 2002;140(3):334–9.
Austin SB, Field AE, Wiecha J, Peterson KE, Gortmaker SL. The impact of a school-based obesity prevention trial on disordered weight-control behaviors in early adolescent girls. Arch Pediatr Adolesc Med. 2005;159(3):225–30.
Chavarro JE, Peterson KE, Sobol AM, Wiecha JL, Gortmaker SL. Effects of a school-based obesity-prevention intervention on menarche (United States). Cancer Causes Control. 2005;16(10):1245–52.
Bjelland M, Bergh IH, Grydeland M, Klepp KI, Andersen LF, Anderssen SA, et al. Changes in adolescents' intake of sugar-sweetened beverages and sedentary behaviour: results at 8 month mid-way assessment of the HEIA study—a comprehensive, multi-component school-based randomized trial. Int J Behav Nutr Phys Act. 2011;8:63.
Burrows T, Warren JM, Baur LA, Collins CE. Impact of a child obesity intervention on dietary intake and behaviors. Int J Obes. 2008;32(10):1481–8.
Collins CE, Dewar DL, Schumacher TL, Finn T, Morgan PJ, Lubans DR. 12 month changes in dietary intake of adolescent girls attending schools in low-income communities following the NEAT Girls cluster randomized controlled trial. Appetite. 2014;73:147–55.
Cunha DB, de Souza Bda S, Pereira RA, Sichieri R. Effectiveness of a randomized school-based intervention involving families and teachers to prevent excessive weight gain among adolescents in Brazil. PLoS One. 2013;8(2):e57498.
Ezendam NP, Brug J, Oenema A. Evaluation of the web-based computer-tailored FATaintPHAT intervention to promote energy balance among adolescents: results from a school cluster randomized trial. Arch Pediatr Adolesc Med. 2012;166(3):248–55.
Lo E, Coles R, Humbert ML, Polowski J, Henry CJ, Whiting SJ. Beverage intake improvement by high school students in Saskatchewan, Canada. Nutr Res. 2008;28(3):144–50.
Sichieri R, Paula Trotte A, de Souza RA, Veiga GV. School randomised trial on prevention of excessive weight gain by discouraging students from drinking sodas. Public Health Nutr. 2009;12(2):197–202.
Powell LM, Chriqui J, Chaloupka FJ. Associations between state-level soda taxes and adolescent body mass index. J Adolesc Health. 2009;45(3 Suppl):S57–63.
Pomeranz JL. Advanced policy options to regulate sugar-sweetened beverages to support public health. J Public Health Policy. 2012;33(1):75–88.
Institute of Medicine. Local government actions to prevent childhood obesity. Washington, DC: The National Academies Press; 2009.
Sturm R, Powell LM, Chriqui JF, Chaloupka FJ. Soda taxes, soft drink consumption, and children's body mass index. Health Aff (Millwood). 2010;29(5):1052–8.
“H.R.5279 – 113th Congress: SWEET Act (2013-2014)”. Cited February 2, 2018. Available at https://www.congress.gov/bill/113th-congress/house-bill/5279
Levy DT, Friend KB, Wang YC. A review of the literature on policies directed at the youth consumption of sugar sweetened beverages. Adv Nutr. 2011;2(2):182S–200S.
Chriqui JF, Eidson SS, Bates H, Kowalczyk S, Chaloupka FJ. State sales tax rates for soft drinks and snacks sold through grocery stores and vending machines, 2007. J Public Health Policy. 2008;29(2):226–49.
• Maa J. Taxing soda: strategies for dealing with the obesity and diabetes epidemic. Perspect Biol Med. 2016;59(4):448–64. This study describes the historical and scientific framework of policy on SSBs and lessons learned from implementing these efforts.
Cook County Government. Sweetened beverage tax. Cited February 20, 2018. Available at https://www.cookcountyil.gov/service/sweetened-beverage-tax
Brownell KD, Farley T, Willett WC, Popkin BM, Chaloupka FJ, Thompson JW, et al. The public health and economic benefits of taxing sugar-sweetened beverages. N Engl J Med. 2009;361(16):1599–605.
Buhler S, Raine KD, Arango M, Pellerin S, Neary NE. Building a strategy for obesity prevention one piece at a time: the case of sugar-sweetened beverage taxation. Can J Diabetes. 2013;37(2):97–102.
Thow AM, Jan S, Leeder S, Swinburn B. The effect of fiscal policy on diet, obesity and chronic disease: a systematic review. Bull World Health Organ. 2010;88(8):609–14.
Andreyeva T, Long MW, Brownell KD. The impact of food prices on consumption: a systematic review of research on the price elasticity of demand for food. Am J Public Health. 2010;100(2):216–22.
Joanne F. Guthrie CN, K Ralston, M Prell, and M Ollinger. Nutrition standards for competitive foods in schools: implications for foodservice revenues, EIB-114. In: U.S. Department of Agriculture ERS, editor. 2013.
Taber DR, Chriqui JF, Powell LM, Chaloupka FJ. Banning all sugar-sweetened beverages in middle schools: reduction of in-school access and purchasing but not overall consumption. Arch Pediatr Adolesc Med. 2012;166(3):256–62.
Fernandes MM. The effect of soft drink availability in elementary schools on consumption. J Am Diet Assoc. 2008;108(9):1445–52.
Forshee RA, Storey ML, Ginevan ME. A risk analysis model of the relationship between beverage consumption from school vending machines and risk of adolescent overweight. Risk Anal. 2005;25(5):1121–35.
Kropski JA, Keckley PH, Jensen GL. School-based obesity prevention programs: an evidence-based review. Obesity. 2008;16(5):1009–18.
Sallis JF, McKenzie TL, Conway TL, Elder JP, Prochaska JJ, Brown M, et al. Environmental interventions for eating and physical activity: a randomized controlled trial in middle schools. Am J Prev Med. 2003;24(3):209–17.
Cyril S, Nicholson JM, Agho K, Polonsky M, Renzaho AM. Barriers and facilitators to childhood obesity prevention among culturally and linguistically diverse (CALD) communities in Victoria, Australia. Aust N Z J Public Health. 2017;41(3):287–93.
Ickes MJ, McMullen J, Haider T, Sharma M. Global school-based childhood obesity interventions: a review. Int J Environ Res Public Health. 2014;11(9):8940–61.
Economos CD, Hyatt RR, Goldberg JP, Must A, Naumova EN, Collins JJ, et al. A community intervention reduces BMI z-score in children: Shape Up Somerville first year results. Obesity (Silver Spring). 2007;15(5):1325–36.
Mahmood S, Perveen T, Dino A, Ibrahim F, Mehraj J. Effectiveness of school-based intervention programs in reducing prevalence of overweight. Indian J Community Med. 2014;39(2):87–93.
Silveira JA, Taddei JA, Guerra PH, Nobre MR. Effectiveness of school-based nutrition education interventions to prevent and reduce excessive weight gain in children and adolescents: a systematic review. J Pediatr. 2011;87(5):382–92.
Powell LM, Chaloupka FJ. Food prices and obesity: evidence and policy implications for taxes and subsidies. Milbank Q. 2009;87(1):229–57.
Sturm R, Datar A. Food prices and weight gain during elementary school: 5-year update. Public Health. 2008;122(11):1140–3.
French SA, Story M, Fulkerson JA, Hannan P. An environmental intervention to promote lower-fat food choices in secondary schools: outcomes of the TACOS Study. Am J Public Health. 2004;94(9):1507–12.
Wharton CM, Long M, Schwartz MB. Changing nutrition standards in schools: the emerging impact on school revenue. J Sch Health. 2008;78(5):245–51.
Johnston LD, O’Malley PM, Terry-McElrath YM, Colabianchi N. School policies and practices to improve health and prevent obesity: National Secondary School Survey results: school years 2006–07 through 2010–11: Ann Arbor, MI, Bridging the Gap Program, Survey Research Center; 2013.
Hatfield DP, Chomitz VR. Increasing children’s physical activity during the school day. Curr Obes Rep. 2015;4(2):147–56.
Fletcher J, Frisvold D, Tefft N. Substitution patterns can limit the effects of sugar-sweetened beverage taxes on obesity. Prev Chronic Dis. 2013;10:E18.
Julie Samia Mair MWP, SP Teret. The use of zoning to restrict fast food outlets: a potential strategy to combat obesity. Center for law and the public’s health at Johns Hopkins and Georgetown Universities; 2005.
U.S. Food and Drug Administration. Menu and vending machines labeling requirements. 2010. Cited Feberary 2, 2018. Available at https://www.fda.gov/Food/GuidanceRegulation/GuidanceDocumentsRegulatoryInformation/LabelingNutrition/ucm217762.htm
Harris JL, Graff SK. Protecting young people from junk food advertising: implications of psychological research for First Amendment law. Am J Public Health. 2012;102(2):214–22.
Funding
Dr. Eduardo J. Simoes reports grants from NIH/NIDDK. This publication was partially funded by Grant Number 1P30DK092950 from the NIDDK, and its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIDDK.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Yilin Yoshida and Eduardo J. Simoes declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by either of the authors.
Additional information
This article is part of the Topical Collection on Economics and Policy in Diabetes
Rights and permissions
About this article
Cite this article
Yoshida, Y., Simoes, E.J. Sugar-Sweetened Beverage, Obesity, and Type 2 Diabetes in Children and Adolescents: Policies, Taxation, and Programs. Curr Diab Rep 18, 31 (2018). https://doi.org/10.1007/s11892-018-1004-6
Published:
DOI: https://doi.org/10.1007/s11892-018-1004-6