Abstract
Preeclampsia is diagnosed in women presenting with new onset hypertension accompanied by proteinuria or other signs of severe organ dysfunction in the second half of pregnancy. Preeclampsia risk is increased 2- to 4-fold among women with type 1 or type 2 diabetes. The limited number of pregnant women with preexisting diabetes and the difficulties associated with diagnosing preeclampsia in women with proteinuria prior to pregnancy are significant barriers to research in this high-risk population. Gestational diabetes mellitus (GDM) also increases preeclampsia risk, although it is unclear whether these two conditions share a common pathophysiological pathway. Nondiabetic women who have had preeclampsia are more likely to develop type 2 diabetes later in life. Among women with type 1 diabetes, a history of preeclampsia is associated with an increased risk of retinopathy and nephropathy. More research examining the pathophysiology, treatment, and the long-term health implications of preeclampsia among women with preexisting and gestational diabetes is needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Preeclampsia is a leading cause of maternal [1] and fetal [2] morbidity and mortality. In developed countries, this syndrome affects 2–7 % of pregnancies in nondiabetic women [3, 4]. Type 1 diabetes, type 2 diabetes, and gestational diabetes further increase preeclampsia risk. Preeclampsia is diagnosed in women presenting with new onset hypertension and proteinuria during the second half of pregnancy [5••]. New guidelines from the American College of Obstetrics and Gynecology (ACOG) indicate that preeclampsia can also be diagnosed in the absence of proteinuria in hypertensive women with pulmonary edema, progressive renal insufficiency, impaired liver function, thrombocytopenia, or new onset cerebral or visual disturbances [5••]. Delivery is the only known cure for preeclampsia, and effective prevention strategies are lacking. Preeclampsia also has long-term health implications. The American Heart Association recently recognized preeclampsia as a risk factor for future cardiovascular disease [6•] and stroke [7•] in women.
The pathophysiology of preeclampsia remains elusive. Current theories suggest that the clinical features of this syndrome are caused by systemic maternal endothelial dysfunction resulting from a combination of preexisting maternal risk factors and abnormal placental development [8]. Maternal risk factors include prepregnancy obesity, advanced maternal age, black race, and chronic hypertension and other cardiovascular risk factors [8]. These maternal characteristics may contribute to oxidative stress, inflammation, and vascular dysfunction, all of which have been implicated in the etiology of preeclampsia [8]. At the placental level, failed adaptation of the uterine spiral arteries may cause hypoxia [8], repeated ischemia-reperfusion injury [9], or high velocity blood flow in the intervillous space [10]. The damaged placenta is believed to release one or more factors into the maternal circulation that contribute to vascular dysfunction [8]. Possible candidates for this placental factor include the antiangiogenic proteins soluble fms-like tyrosine kinase 1 (sFlt-1) and soluble endoglin (sEng) [11, 12]. sFlt-1 lowers the bioavailability of vascular endothelial growth factor (VEGF) and placental growth factor (PGF) by binding these proangiogenic ligands as a nonsignaling decoy [13]. sEng inhibits binding of transforming growth factor β1 to endoglin, preventing endothelial nitric oxide synthase activation and subsequent vasodilation [12]. Thus, excessive sFlt-1 and sEng may impair pregnancy-induced adaptation in maternal placental bed vessels and contribute to systemic maternal endothelial dysfunction in some women with preeclampsia [13].
Insulin resistance has also been hypothesized to contribute to the pathophysiology of preeclampsia. Compared to women who have normotensive pregnancies, women who develop preeclampsia are more insulin resistant prior to pregnancy [14], in the first and second trimesters [15], and years after pregnancy [16]. This effect is partially explained by the fact that many preeclampsia risk factors are also associated with insulin resistance, including obesity, advanced maternal age, non-white race, chronic hypertension, diabetes, and gestational diabetes [15, 14]. However, insulin resistance at 22–26 weeks gestation was a significant independent predictor of preeclampsia after adjustment for these common risk factors, suggesting an independent effect [15].
This review examines the relationship between preeclampsia and diabetes, focusing on new research in three key areas. The first section describes the unique challenges of studying preeclampsia in women with diabetes and reviews recent studies examining preeclampsia pathophysiology in women with type 1 or type 2 diabetes. The second section examines the relationship between gestational diabetes and preeclampsia, along with the possibility of a shared pathophysiological pathway for these two conditions. The third section focuses on long-term risk of diabetes and diabetic complications in women with a history of preeclampsia.
Preeclampsia in Women with Type 1 or Type 2 Diabetes
Preexisting diabetes is a risk factor for preeclampsia. In comparison to the relatively low incidence of preeclampsia in nondiabetic women (2–7 %) [3, 4], preeclampsia is diagnosed in 15–20 % of pregnancies in women with type 1 diabetes [17–19] and 10–14 % of pregnancies in women with type 2 diabetes [20, 19]. Obesity is a shared risk factor for both preeclampsia and type 2 diabetes; however, the greater preeclampsia risk among women with type 2 diabetes persists even when women are matched for BMI [21]. In a population-based study of deliveries in Washington state, preexisting diabetes was a risk factor for both early onset (diagnosis before 34 weeks gestation; hazard ratio (HR) 1.87, 95 % confidence interval (CI) 1.60–2.81) and late onset (HR 2.46, 95 % CI 2.32–2.61) preeclampsia [22]. Known risk factors for preeclampsia among women with type 1 and type 2 diabetes include nulliparity, advanced maternal age, previous preeclampsia, hypertension, a longer duration of diabetes, microalbuminuria, nephropathy and retinopathy, and poor glycemic control [23••, 24, 25].
Preeclampsia research in women with type 1 and type 2 diabetes is complicated by two factors. First, multicenter studies and recruitment for an extended time period are often required to obtain a sufficient number of preeclamptic women with diabetes. Many investigators address this challenge by pooling women with type 1 and type 2 diabetes or by combining women with diabetes with other high-risk groups (i.e., chronic hypertension, multifetal gestation, preeclampsia in a previous pregnancy, etc.). Recent guidelines for the standardization of preeclampsia study design strongly discourage this approach, as preeclampsia pathophysiology may differ among high-risk groups [26••].
The second problem is the lack of standardized criteria for preeclampsia diagnosis in women who have proteinuria prior to conception, which is common in women with diabetes. The diagnosis of preeclampsia is straightforward in a subset of patients who develop the most severe forms of preeclampsia, such as the convulsive form, eclampsia, or HELLP syndrome (hemolysis, elevated liver enzymes, low platelets). For other patients, a variety of modified criteria are used. These include worsening proteinuria and/or other signs of organ dysfunction, such as a serum aminotransferase concentration of ≥70 U per liter, thrombocytopenia, or hypertension with severe headaches or epigastric pain [27, 28]. These diverse criteria make comparisons between studies difficult. In addition, worsening proteinuria during pregnancy is common in women with diabetic nephropathy [29] due to increases in the glomerular filtration rate [30]. Studies are needed to determine whether the recently expanded ACOG criteria for diagnosing preeclampsia in pregnant women who do not have proteinuria [5••] also have diagnostic utility among women with preexisting proteinuria. Despite these challenges, recent studies examining the pathophysiology of preeclampsia in women with type 1 diabetes have focused on the potential roles of angiogenic imbalance and haptoglobin phenotype.
Angiogenic Imbalance
Antiangiogenic factors and preeclampsia risk have been extensively examined. However, many studies have excluded women with diabetes or combined women from different high-risk populations. Studies examining the relationship between antiangiogenic (sFlt-1, sEng) and proangiogenic (PGF) factors and preeclampsia in women with preexisting diabetes have yielded conflicting results. The largest study examined plasma angiogenic factors at 26 weeks gestation among 540 women with type 1 diabetes [31••]. Compared to women who did not develop preeclampsia, women who later developed preeclampsia (n = 94) had higher plasma sFlt-1 and sEng and lower PGF [31••]. The addition of sFlt-1/PGF slightly improved the performance of predictive models based on traditional preeclampsia risk factors [31••].
Smaller longitudinal studies have examined these markers in women with type 1 diabetes who did not have microalbuminuria in early pregnancy [32], women with preexisting diabetes that required insulin [33], and a mixed group of women with type 1 or type 2 diabetes [34]. sFlt-1, sEng, and PGF prior to 25 weeks gestation did not differ between diabetic women who developed preeclampsia and those who did not [34, 32, 33]. After 25 weeks gestation, results were conflicting. Whereas some studies reported lower PGF [34, 32], higher sFlt-1 [32], or higher sEng [33] among women who developed preeclampsia, others found no differences in PGF [33], sFlt-1 [34, 33], or sEng [32]. In addition to the small sample sizes and varying inclusion criteria, differences in sample type and processing may also contribute to the heterogeneity of results. Angiogenic markers were measured in plasma [31••], serum [33, 32], or both [34], and few details regarding sample processing were provided. Angiogenic factors released from platelets and other blood components during sample processing can dramatically increase measured concentrations [35•]. The collection of samples with cell activation inhibitors has been shown to reduce maternal serum PGF by 29 % and sFlt-1 by 20 % [35•]. Larger studies with appropriate sample processing techniques are needed. Additional studies of angiogenic factors in relation to preeclampsia risk among women with type 2 diabetes would be beneficial, as most studies focused on type 1 diabetes.
Haptoglobin
Haptoglobin (Hp) is an antioxidant [36] and proangiogenic [37] protein best known for its ability to bind free hemoglobin following hemolysis. Hp has three common, genetically determined phenotypes (1-1, 2-1, 2-2) [38]. Hp 1-1 is the strongest antioxidant [36], whereas Hp 2-2 is the most angiogenic [37].
Several factors suggested that Hp phenotype could potentially be important in preeclampsia. First, oxidative stress and angiogenic imbalance are important pathophysiological processes in preeclampsia [11, 39]; therefore, it is reasonable to think that Hp phenotype might influence preeclampsia risk. Second, cardiovascular event risk is doubled in Hp 2-2 individuals with diabetes, compared to Hp 1-1 and 2-1 individuals with diabetes [40–42]. Additionally, Hp phenotype influences responsiveness to antioxidant vitamins in individuals with diabetes. Daily vitamin E supplementation eliminates the increased cardiovascular disease risk seen in Hp 2-2 individuals with type 2 diabetes, but has no effect in Hp 2-1 or 1-1 individuals with diabetes [43, 42, 44]. In contrast, vitamin C combined with vitamin E may be beneficial or harmful depending on phenotype [41]. These findings are of particular interest to preeclampsia researchers. Oxidative stress is associated with preeclampsia [11, 39] and the antioxidant vitamins C and E lowered preeclampsia incidence by 60 % among high-risk women in a small randomized controlled trial (RCT) [45]. Unfortunately, subsequent RCTs in high- [46–50] and low-risk [51] women and women with type 1 diabetes [28] were negative. These disparate results are likely due to low power in the small trial. However, differences could also be explained by the greater diversity of patients in multicenter trials masking a subset of responsive women.
Small case-control studies of nondiabetic women have reported that preeclampsia risk was increased, [52], decreased [53, 54], or not different [55] in women with the stronger antioxidant Hp 1-1 phenotype. The heterogeneity of results may have been due to differences in the populations studied. However, the small sample sizes and lack of consistent findings suggest that type II error may have been a factor. To address these issues, Weissgerber et al. conducted secondary analyses of two larger RCTs of daily vitamin C and E supplementation to prevent preeclampsia. The first examined low-risk primiparous women [51], while the second enrolled women with type 1 diabetes [28]. Hp phenotype was not associated with preeclampsia risk in either trial [56•, 57]. Furthermore, the authors found no evidence that vitamins C and E prevented preeclampsia in women of any Hp phenotype [56•, 57]. Despite proven effects in other disease states, it appears that Hp phenotype does not play a significant role in preeclampsia risk or responsiveness to antioxidant vitamin supplementation to prevent preeclampsia.
Preeclampsia and Gestational Diabetes
Gestational diabetes mellitus (GDM) is defined as hyperglycemia that is first diagnosed during pregnancy. The American Diabetes Association (ADA) recommends using either the traditional two-step approach or a newer one-step approach to screen for GDM at 24–28 weeks gestation. For the two-step approach, women who fail a 50-g glucose challenge test complete a second diagnostic 75-g oral glucose tolerance test to confirm the diagnosis [58]. The newer one-step approach is based on a single 75-g oral glucose tolerance test and was developed by the International Association of Diabetes and Pregnancy Study Groups (IADPSG), which includes the ADA. GDM is diagnosed if fasting (≥92 mg/dl) and 1-h (≥180 mg/dl) or 2-h (≥153 mg/dl) glucose values exceed established cut points [58].
The prevalence of GDM ranges from 2 to 10 % of all pregnancies in developed countries [59]; however, those rates are expected to rise drastically with the adoption of the less restrictive IADPSG diagnostic criteria [60]. GDM is associated with birth complications, including macrosomia and operative delivery. Long-term health risks associated with GDM include an increased risk of type 2 diabetes for both the woman and her child [61–63].
GDM and preeclampsia share many risk factors, including advanced maternal age, nulliparity, multifetal pregnancies, non-white race/ethnicity, and prepregnancy obesity [64, 65••]. GDM is often listed as a risk factor for the development of preeclampsia; however, previous research on the co-occurrence of the two conditions has often been underpowered and/or failed to account for shared risk factors such as obesity. To address these issues, a retrospective investigation of 647,392 pregnancies in the German Perinatal Quality Registry examined the relation between GDM and preeclampsia while controlling for common risk factors. The authors found that the odds of preeclampsia were increased among women with GDM (adjusted odds ratio (aOR) 1.29, 95 % CI 1.19–1.41), even after controlling for age, nationality, job status, smoking, parity, multifetal pregnancy, prepregnancy weight status, and gestational weight gain [65••]. These results concur with other birth registry studies in Canada and Sweden, confirming that GDM is an independent risk factor for preeclampsia [66, 67].
One study sought to identify the most salient clinical risk factors for preeclampsia among women with GDM [68]. First trimester obesity (defined as BMI ≥27 kg/m2; aOR 10.4, 95 % CI 5.3–20.8), GDM diagnosis prior to 20 weeks gestation (aOR 8.0, 95 % CI 4.3–14.9), and poor glycemic control (aOR 8.4, 95 % CI 5.6–15.4) were the most significant risk factors for preeclampsia [68]. Among these, maternal obesity may be the most modifiable risk factor, although new results also identify excessive gestational weight gain as an independent modifiable risk factor for preeclampsia. A study of 2037 women with GDM assessed the effects of prepregnancy weight status, gestational weight gain, and third trimester glycemic control (via glycated hemoglobin or HbA1c) on the risk of pregnancy-induced hypertension (including preeclampsia and new onset hypertension after 20 weeks gestation) [69•]. The authors found that poor glycemic control (aOR 2.5, 95 % CI 1.1–5.7) and prepregnancy obesity (aOR 8.9, 95 % CI 5.0–16.0) were associated with increased risk of pregnancy-induced hypertension, but excessive gestational weight gain also increased risk (aOR 1.9, 95 % CI 1.1–3.4) [69•]. The prevalence of pregnancy-induced hypertension was highest among obese women who gained excessive weight (41 %). In another study specific to preeclampsia, excessive gestational weight gain was associated with nonsignificantly increased odds of preeclampsia (aOR 1.4, 95 % CI 0.6–3.1) compared to appropriate weight gain; however, when weight gain was expressed continuously, every 1 lb/week increase in weight gain after GDM diagnosis was associated with a 1.8-fold increased odds of preeclampsia [70]. Taken together, these results indicate that while excess gestational weight gain may increase preeclampsia risk among women with GDM, preexisting obesity confers a greater risk.
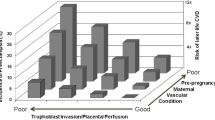
It is unclear whether a common etiologic pathway underlies both GDM and preeclampsia. When compared to women with healthy pregnancies, researchers have identified many maladaptations to pregnancy that are present in both preeclampsia and GDM. These include endothelial dysfunction (e.g., lower flow-mediated dilation) [71, 72], angiogenic imbalance (e.g., high sFlt-1 and/or low PGF) [71, 73], increased oxidative stress (e.g., low total antioxidant status, high free radicals) [74], and dyslipidemia (e.g., increased triglycerides) [75, 76]. However, it is difficult to know whether abnormalities in these biomarkers result from a common etiology or are responses to different underlying disease processes in women with preeclampsia and GDM. For example, Wen et al. [77•] postulate that prepregnancy susceptibility to cardiovascular disease sets the stage for preeclampsia. Poor placentation leads to systemic endothelial dysfunction and inflammation, which is reflected by the biomarkers stated above. In contrast, they argue that GDM has prepregnancy origins in beta cell dysfunction that is only unmasked by the progressive insulin resistance of pregnancy [77•]. The resulting hyperglycemia causes endothelial damage and inflammation, as captured by the above biomarkers [77•]. In fact, others have postulated that insulin resistance during pregnancy could be the common trigger leading to GDM and/or preeclampsia in predisposed women [78]. At present, none of these theories have been adequately tested.
One way to assess whether GDM and preeclampsia share a common etiology would be to determine whether interventions to treat GDM also reduce preeclampsia risk. A randomized control trial of treatment (nutritional counseling, diet therapy, and insulin if needed) vs. no treatment among almost 1000 women with mild GDM found that treatment was associated with 55 % reduced risk of preeclampsia (relative risk (RR) 0.46, 95 % CI 0.22–0.97) [79]. However, other trials have failed to find significant effects [80, 81]. A recent meta-analysis of 10 GDM treatment trials (of which only 3 examined preeclampsia rates) found no association between GDM treatment and preeclampsia (RR = 1.14, 95 % CI 0.24–5.45) [82••]. The wide confidence intervals of the studies included in the meta-analysis demonstrate that additional adequately powered studies are needed to determine whether GDM treatment lowers preeclampsia risk.
The Risk of Diabetes After a Preeclamptic Pregnancy
While preeclampsia is now recognized as a risk factor for cardiovascular disease [6•] and stroke [7•], the relationship between preeclampsia and future diabetes has received less attention. A classic study by Chesley reported an increased risk of late onset diabetes among women with a history of eclampsia [83]. This severe form of preeclampsia causes seizures and leads to very high rates of maternal and fetal morbidity and mortality. Recent studies suggest that preeclampsia is also a risk factor for future diabetes (Table 1) [84•, 85–88]. This effect is evident even when women who had preeclampsia with gestational diabetes are excluded [84•, 85]. However, preeclampsia is a modest predictor of future diabetes when compared to gestational diabetes (Table 1). When considering both pregnancy conditions, the risk of developing diabetes is moderately increased in women who had preeclampsia (without gestational diabetes), greatly elevated in women who had gestational diabetes (without preeclampsia), and highest in women who had both preeclampsia and gestational diabetes [84•, 85]. A registry study of 226,832 women in Norway showed that only 0.5 % of women without GDM or preeclampsia had received a prescription to treat diabetes within 5 years of birth, while 2 % of women with preeclampsia had received such a prescription, 19 % of women with GDM diagnoses were taking diabetes drugs, and over half (55 %) of women with both conditions had received a diabetes prescription [84•]. Feig and colleagues similarly reported that the number of women that would need to be followed for 5 years to detect one case of diabetes was 123 for preeclampsia, 68 for gestational diabetes, and 31 for preeclampsia and gestational diabetes [85].
Existing studies of long-term diabetes risk either did not distinguish between type 1 and type 2 diabetes [84•, 85, 87] or focused on type 2 diabetes [86]. Authors of the studies that pooled type 1 and 2 diabetes speculated that the increased risk that they observed was likely due to type 2 diabetes, as type 1 diabetes is usually diagnosed in childhood or adolescence. Only one study examined the risk of type 1 and type 2 diabetes separately [88]. Women who had preeclampsia were significantly more likely to be hospitalized for type 2 diabetes (aOR 2.0, 95 % CI 1.3–3.2), but not type 1 diabetes (aOR 1.8, 95 % CI 0.8–3.8), within 1 year of delivery [88]. Low power may have contributed to the absence of a significant effect for type 1 diabetes. The adjusted odds ratios for type 1 and type 2 diabetes were very similar (1.8 vs. 2.0), but fewer women were hospitalized for type 1 diabetes (n = 71 vs. 212 [88]). Regardless, the fact that 25 % of the women hospitalized for diagnosis of diabetes within 1 year of delivery had type 1 diabetes [88] questions the previous authors’ assumption that estimated effects of preeclampsia on a pooled “diabetes” variable predominantly reflect type 2 diabetes risk.
Additional studies of type 1 diabetes risk following a preeclamptic pregnancy are clearly warranted, and they should address three important limitations of the only study on type 1 diabetes to date [88]. First, the primary outcome of hospitalization for diabetes likely contributed to the high proportion of women with type 1 diabetes. Compared to type 2 diabetes, the more severe clinical features of type 1 diabetes may lead to higher hospitalization rates. Second, women were followed for 1 year after delivery. While some nondiabetic women may have developed diabetes during that time, others likely had preexisting diabetes that had never been diagnosed. Third, the study examined women who delivered in New York City [88]. Rates of diagnosis for type 1 diabetes may be different in other cohorts, as they likely depend on maternal age, length of follow-up, access to health care, and other factors.
Diabetic Complications in Women with Type 1 Diabetes After a Preeclamptic Pregnancy
Several studies suggest that women with preexisting type 1 diabetes who have had preeclampsia are more likely to develop diabetic complications later in life. Gordin and colleagues examined the risk of diabetic nephropathy, hypertension, and coronary heart disease among 203 Finnish women with type 1 diabetes [89]. After an average follow-up of 11 years, women who had preeclampsia were more likely to be taking antihypertensive medication than women who had normotensive pregnancies (50 vs. 10 %) [89]. They were also more likely to have coronary heart disease (12 vs. 2 %), myocardial infarction (7 vs. 0 %), and diabetic nephropathy (42 vs. 9 %) [89]. Preeclampsia and HbA1c during pregnancy were both independent predictors of diabetic nephropathy [89].
Two studies examined the relationship between preeclampsia and future retinopathy in women with type 1 diabetes. Sight-threatening deterioration of retinopathy was more common among Swedish women who had preeclampsia, compared to those who did not have preeclampsia (50 vs. 9 %), at 6 months postpartum [90]. A later study in the Finnish cohort that was described in the preceding paragraph examined the risk of severe diabetic retinopathy [91]. Compared to women who had normotensive pregnancies, women who had preeclampsia were more likely to develop severe diabetic retinopathy (hazard ratio 3.9, 95 % CI 1.3–11.3) after 16 years of follow-up [91]. Poor glycemic control likely contributed to this effect, as the strength of the association was attenuated after adjusting for HbA1c in pregnancy (hazard ratio 2.0, 95 % CI 0.6–6.8) [91].
Existing research suggests that preeclampsia is a risk factor for diabetic retinopathy and nephropathy among women with type 1 diabetes. Larger studies that can control for additional risk factors and examine the risk of other types of complications are needed. The mechanisms for increased rates of complications in women with a history of preeclampsia are not yet known. Women who develop preeclampsia may have more advanced disease and poorer glycemic control prior to pregnancy [23]. Genetic or environmental factors that contribute to preeclampsia could also increase the risk of diabetic complications later in life. Alternatively, preeclampsia may cause lasting damage that leads to diabetic complications years after pregnancy. If preeclampsia causes lasting damage, then new therapeutic targets for blood pressure, glycemic control, and other clinical indicators may be needed to prevent this damage in preeclamptic women with type 1 diabetes.
Conclusions
The high prevalence of preeclampsia among women with preexisting diabetes highlights the need for research examining predictive markers, pathophysiology, treatment, and the long-term health implications of preeclampsia in this population. However, multicenter studies and years of recruitment are often needed to obtain large cohorts of pregnant women with type 1 or type 2 diabetes. Standardized criteria for preeclampsia diagnosis in women who have proteinuria prior to pregnancy are urgently needed.
More research is also needed to examine the possibility that GDM and preeclampsia share a common etiologic pathway. Many maladaptations to pregnancy are common to both conditions, suggesting that their pathophysiology may overlap. However, studies to date have not had the power to compare biomarkers and risk factors among women with preeclampsia alone, GDM alone, and preeclampsia with GDM. A better understanding of the shared and separate pathophysiologies of these two conditions may help researchers and clinicians to optimize screening techniques and improve treatments for GDM and preeclampsia.
Large registry studies show that preeclampsia is a risk factor for diabetes later in life. Additional studies are needed to quantify the risks of type 1 vs. type 2 diabetes. Researchers should also determine whether any observed increase in the risk of type 1 diabetes reflects new onset disease or is due to preexisting disease that was never diagnosed. A few studies suggest that women with type 1 diabetes who have had preeclampsia are at increased risk for retinopathy and nephropathy later in life. These women may benefit from additional monitoring to prevent, detect, and treat diabetic complications after pregnancy. However, larger studies that can control for additional risk factors, and studies examining other types of complications, are needed. Given the increasing prevalence of type 2 diabetes in pregnant women [92], future studies should also examine the relationship between preeclampsia and diabetic complications in women with type 2 diabetes.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
World Health Organization. World Health Report: make every mother, and child count. Geneva: WHO 2005.
Altman D, Carroli G, Duley L, Farrell B, Moodley J, Neilson J, et al. Do women with pre-eclampsia, and their babies, benefit from magnesium sulphate? The Magpie Trial: a randomised placebo-controlled trial. Lancet. 2002;359(9321):1877–90.
Knuist M, Bonsel GJ, Zondervan HA, Treffers PE. Intensification of fetal and maternal surveillance in pregnant women with hypertensive disorders. Int J Gynaecol Obstet. 1998;61(2):127–33.
Hauth JC, Ewell MG, Levine RJ, Esterlitz JR, Sibai B, Curet LB, et al. Pregnancy outcomes in healthy nulliparas who developed hypertension. Calcium for Preeclampsia Prevention Study Group. Obstet Gynecol. 2000;95(1):24–8.
Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists’ Task Force on Hypertension in Pregnancy. Obstetrics and gynecology. 2013;122(5):1122-31. doi:10.1097/01.AOG.0000437382.03963.88. This paper outlines new ACOG criteria for the diagnosis of preeclampsia.
Mosca L, Benjamin EJ, Berra K, Bezanson JL, Dolor RJ, Lloyd-Jones DM, et al. Effectiveness-based guidelines for the prevention of cardiovascular disease in women—2011 update: a guideline from the American Heart Association. J Am Coll Cardiol. 2011;57(12):1404–23. doi:10.1016/j.jacc.2011.02.005. This American Heart Association guideline identifies preeclampsia as a major risk factor for future cardiovascular disease in women.
Bushnell C, McCullough LD, Awad IA, Chireau MV, Fedder WN, Furie KL, et al. Guidelines for the prevention of stroke in women: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45(5):1545–88. doi:10.1161/01.str.0000442009.06663.48. This American Heart Association guideline identifies preeclampsia as a risk factor for stroke years after pregnancy.
Roberts JM, Lain KY. Recent insights into the pathogenesis of pre-eclampsia. Placenta. 2002;23(5):359–72. doi:10.1053/plac.2002.0819.
Jauniaux E, Hempstock J, Greenwold N, Burton GJ. Trophoblastic oxidative stress in relation to temporal and regional differences in maternal placental blood flow in normal and abnormal early pregnancies. Am J Pathol. 2003;162(1):115–25. doi:10.1016/S0002-9440(10)63803-5.
Burton GJ, Woods AW, Jauniaux E, Kingdom JC. Rheological and physiological consequences of conversion of the maternal spiral arteries for uteroplacental blood flow during human pregnancy. Placenta. 2009;30(6):473–82. doi:10.1016/j.placenta.2009.02.009.
Maynard SE, Min JY, Merchan J, Lim KH, Li J, Mondal S, et al. Excess placental soluble fms-like tyrosine kinase 1 (sFlt1) may contribute to endothelial dysfunction, hypertension, and proteinuria in preeclampsia. J Clin Investig. 2003;111(5):649–58. doi:10.1172/JCI17189.
Venkatesha S, Toporsian M, Lam C, Hanai J, Mammoto T, Kim YM, et al. Soluble endoglin contributes to the pathogenesis of preeclampsia. Nat Med. 2006;12(6):642–9. doi:10.1038/nm1429.
Mutter WP, Karumanchi SA. Molecular mechanisms of preeclampsia. Microvasc Res. 2008;75(1):1–8. doi:10.1016/j.mvr.2007.04.009.
Valdes E, Sepulveda-Martinez A, Manukian B, Parra-Cordero M. Assessment of pregestational insulin resistance as a risk factor of preeclampsia. Gynecol Obstet Investig. 2014;77(2):111–6. doi:10.1159/000357944.
Hauth JC, Clifton RG, Roberts JM, Myatt L, Spong CY, Leveno KJ, et al. Maternal insulin resistance and preeclampsia. Am J Obstet Gynecol. 2011;204(4):327.e1–6.
Alsnes IV, Janszky I, Forman MR, Vatten LJ, Okland I. A population-based study of associations between preeclampsia and later cardiovascular risk factors. Am J Obstet Gynecol. 2014. doi:10.1016/j.ajog.2014.06.026.
Jensen DM, Damm P, Moelsted-Pedersen L, Ovesen P, Westergaard JG, Moeller M, et al. Outcomes in type 1 diabetic pregnancies: a nationwide, population-based study. Diabetes Care. 2004;27(12):2819–23.
Persson M, Norman M, Hanson U. Obstetric and perinatal outcomes in type 1 diabetic pregnancies: a large, population-based study. Diabetes Care. 2009;32(11):2005–9. doi:10.2337/dc09-0656.
Knight KM, Thornburg LL, Pressman EK. Pregnancy outcomes in type 2 diabetic patients as compared with type 1 diabetic patients and nondiabetic controls. J Reprod Med. 2012;57(9–10):397–404.
Groen B, Links TP, van den Berg PP, Hellinga M, Moerman S, Visser GH, et al. Similar adverse pregnancy outcome in native and nonnative Dutch women with pregestational type 2 diabetes: a multicentre retrospective study. ISRN Obstet Gynecol. 2013;2013:361435. doi:10.1155/2013/361435.
Knight KM, Pressman EK, Hackney DN, Thornburg LL. Perinatal outcomes in type 2 diabetic patients compared with non-diabetic patients matched by body mass index. J Matern Fetal Neonatal Med. 2012;25(6):611–5. doi:10.3109/14767058.2011.587059.
Lisonkova S, Joseph KS. Incidence of preeclampsia: risk factors and outcomes associated with early- versus late-onset disease. Am J Obstet Gynecol. 2013;209(6):544.e1–12.
Holmes VA, Young IS, Patterson CC, Pearson DW, Walker JD, Maresh MJ, et al. Optimal glycemic control, pre-eclampsia, and gestational hypertension in women with type 1 diabetes in the diabetes and pre-eclampsia intervention trial. Diabetes Care. 2011;34(8):1683–8. doi:10.2337/dc11-0244. This paper from a large randomized controlled trial of vitamin C and E to prevent preeclampsia in women with type 1 diabetes shows that poor glycemic control is an independent risk factor for preeclampsia.
Colatrella A, Loguercio V, Mattei L, Trappolini M, Festa C, Stoppo M, et al. Hypertension in diabetic pregnancy: impact and long-term outlook. Best Pract Res Clin Endocrinol Metab. 2010;24(4):635–51. doi:10.1016/j.beem.2010.05.003.
Ekbom P, Damm P, Feldt-Rasmussen B, Feldt-Rasmussen U, Molvig J, Mathiesen ER. Pregnancy outcome in type 1 diabetic women with microalbuminuria. Diabetes Care. 2001;24(10):1739–44.
Myatt L, Redman CW, Staff AC, Hansson S, Wilson ML, Laivuori H, et al. Strategy for standardization of preeclampsia research study design. Hypertension. 2014;63(6):1293–301. doi:10.1161/HYPERTENSIONAHA.113.02664. This guideline describes methods for standardizing and optimizing study design and data collection in preeclampsia studies.
Caritis S, Sibai B, Hauth J, Lindheimer MD, Klebanoff M, Thom E, et al. Low-dose aspirin to prevent preeclampsia in women at high risk. National Institute of Child Health and Human Development Network of Maternal-Fetal Medicine Units. N Engl J Med. 1998;338(11):701–5. doi:10.1056/NEJM199803123381101.
McCance DR, Holmes VA, Maresh MJ, Patterson CC, Walker JD, Pearson DW, et al. Vitamins C and E for prevention of pre-eclampsia in women with type 1 diabetes (DAPIT): a randomised placebo-controlled trial. Lancet. 2010;376(9737):259–66. doi:10.1016/S0140-6736(10)60630-7.
Reece EA, Leguizamon G, Homko C. Pregnancy performance and outcomes associated with diabetic nephropathy. Am J Perinatol. 1998;15(7):413–21. doi:10.1055/s-2007-993968.
Davison JM, Dunlop W. Renal hemodynamics and tubular function normal human pregnancy. Kidney Int. 1980;18(2):152–61.
Holmes VA, Young IS, Patterson CC, Maresh MJ, Pearson DW, Walker JD, et al. The role of angiogenic and antiangiogenic factors in the second trimester in the prediction of preeclampsia in pregnant women with type 1 diabetes. Diabetes Care. 2013;36(11):3671–7. doi:10.2337/dc13-0944. This secondary analysis of a randomized controlled trial is the largest study examining the potential value of sFlt-1, sEng and PGF to predict preeclampsia in women with type 1 diabetes.
Yu Y, Jenkins AJ, Nankervis AJ, Hanssen KF, Scholz H, Henriksen T, et al. Anti-angiogenic factors and pre-eclampsia in type 1 diabetic women. Diabetologia. 2009;52(1):160–8. doi:10.1007/s00125-008-1182-x.
Powers RW, Jeyabalan A, Clifton RG, Van Dorsten P, Hauth JC, Klebanoff MA, et al. Soluble fms-like tyrosine kinase 1 (sFlt1), endoglin and placental growth factor (PlGF) in preeclampsia among high risk pregnancies. PLoS One. 2010;5(10):e13263. doi:10.1371/journal.pone.0013263.
Cohen AL, Wenger JB, James-Todd T, Lamparello BM, Halprin E, Serdy S, et al. The association of circulating angiogenic factors and HbA1c with the risk of preeclampsia in women with preexisting diabetes. Hypertens Pregnancy. 2014;33(1):81–92.
Zamudio S, Kovalenko O, Echalar L, Torricos T, Al-Khan A, Alvarez M, et al. Evidence for extraplacental sources of circulating angiogenic growth effectors in human pregnancy. Placenta. 2013;34(12):1170–6. doi:10.1016/j.placenta.2013.09.016. This paper identifies methodological factors that influence measured concentrations of pro-angiogenic and anti-angiogenic factors. These factors must be accurately controlled to ensure the accuracy of study conclusions.
Levy AP, Asleh R, Blum S, Levy NS, Miller-Lotan R, Kalet-Litman S, et al. Haptoglobin: basic and clinical aspects. Antioxid Redox Signal. 2010;12(2):293–304. doi:10.1089/ars.2009.2793.
Cid MC, Grant DS, Hoffman GS, Auerbach R, Fauci AS, Kleinman HK. Identification of haptoglobin as an angiogenic factor in sera from patients with systemic vasculitis. J Clin Investig. 1993;91(3):977–85. doi:10.1172/JCI116319.
Langlois MR, Delanghe JR. Biological and clinical significance of haptoglobin polymorphism in humans. Clin Chem. 1996;42(10):1589–600.
Chappell LC, Seed PT, Briley A, Kelly FJ, Hunt BJ, Charnock-Jones DS, et al. A longitudinal study of biochemical variables in women at risk of preeclampsia. Am J Obstet Gynecol. 2002;187(1):127–36.
Blum S, Milman U, Shapira C, Miller-Lotan R, Bennett L, Kostenko M, et al. Dual therapy with statins and antioxidants is superior to statins alone in decreasing the risk of cardiovascular disease in a subgroup of middle-aged individuals with both diabetes mellitus and the haptoglobin 2-2 genotype. Arterioscler Thromb Vasc Biol. 2008;28(3):e18–20. doi:10.1161/ATVBAHA.107.159905.
Levy AP, Friedenberg P, Lotan R, Ouyang P, Tripputi M, Higginson L, et al. The effect of vitamin therapy on the progression of coronary artery atherosclerosis varies by haptoglobin type in postmenopausal women. Diabetes Care. 2004;27(4):925–30.
Levy AP, Gerstein HC, Miller-Lotan R, Ratner R, McQueen M, Lonn E, et al. The effect of vitamin E supplementation on cardiovascular risk in diabetic individuals with different haptoglobin phenotypes. Diabetes Care. 2004;27(11):2767.
Blum S, Vardi M, Levy NS, Miller-Lotan R, Levy AP. The effect of vitamin E supplementation on cardiovascular risk in diabetic individuals with different haptoglobin phenotypes. Atherosclerosis. 2010;211(1):25–7. doi:10.1016/j.atherosclerosis.2010.02.018.
Milman U, Blum S, Shapira C, Aronson D, Miller-Lotan R, Anbinder Y, et al. Vitamin E supplementation reduces cardiovascular events in a subgroup of middle-aged individuals with both type 2 diabetes mellitus and the haptoglobin 2-2 genotype: a prospective double-blinded clinical trial. Arterioscler Thromb Vasc Biol. 2008;28(2):341–7. doi:10.1161/ATVBAHA.107.153965.
Chappell LC, Seed PT, Briley AL, Kelly FJ, Lee R, Hunt BJ, et al. Effect of antioxidants on the occurrence of pre-eclampsia in women at increased risk: a randomised trial. Lancet. 1999;354(9181):810–6. doi:10.1016/S0140-6736(99)80010-5.
Beazley D, Ahokas R, Livingston J, Griggs M, Sibai BM. Vitamin C and E supplementation in women at high risk for preeclampsia: a double-blind, placebo-controlled trial. Am J Obstet Gynecol. 2005;192(2):520–1. doi:10.1016/j.ajog.2004.09.005.
Poston L, Briley AL, Seed PT, Kelly FJ, Shennan AH. Vitamin C and vitamin E in pregnant women at risk for pre-eclampsia (VIP Trial): randomised placebo-controlled trial. Lancet. 2006;367(9517):1145–54. doi:10.1016/S0140-6736(06)68433-X.
Spinnato 2nd JA, Freire S, Silva JL, Pinto E, Cunha Rudge MV, Martins-Costa S, et al. Antioxidant therapy to prevent preeclampsia: a randomized controlled trial. Obstet Gynecol. 2007;110(6):1311–8. doi:10.1097/01.AOG.0000289576.43441.1f.
Rumbold AR, Crowther CA, Haslam RR, Dekker GA, Robinson JS. Vitamins C and E and the risks of preeclampsia and perinatal complications. N Engl J Med. 2006;354(17):1796–806. doi:10.1056/NEJMoa054186.
Villar J, Purwar M, Merialdi M, Zavaleta N, Thi Nhu Ngoc N, Anthony J, et al. World Health Organisation multicentre randomised trial of supplementation with vitamins C and E among pregnant women at high risk for pre-eclampsia in populations of low nutritional status from developing countries. BJOG. 2009;116(6):780–8. doi:10.1111/j.1471-0528.2009.02158.x.
Roberts JM, Myatt L, Spong CY, Thom EA, Hauth JC, Leveno KJ, et al. Vitamins C and E to prevent complications of pregnancy-associated hypertension. N Engl J Med. 2010;362(14):1282–91. doi:10.1056/NEJMoa0908056.
Depypere HT, Langlois MR, Delanghe JR, Temmerman M, Dhont M. Haptoglobin polymorphism in patients with preeclampsia. Clin Chem Lab Med. 2006;44(8):924–8. doi:10.1515/CCLM.2006.182.
Sammour RN, Nakhoul FM, Levy AP, Miller-Lotan R, Nakhoul N, Awad HR, et al. Haptoglobin phenotype in women with preeclampsia. Endocrine. 2010;38(2):303–8. doi:10.1007/s12020-010-9392-7.
Weissgerber TL, Roberts JM, Jeyabalan A, Powers RW, Lee M, Datwyler SA, et al. Haptoglobin phenotype, angiogenic factors, and preeclampsia risk. Am J Obstet Gynecol. 2012;206(4):358.e10–18. doi:10.1016/j.ajog.2012.01.009.
Raijmakers MT, Roes EM, te Morsche RH, Steegers EA, Peters WH. Haptoglobin and its association with the HELLP syndrome. J Med Genet. 2003;40(3):214–6.
Weissgerber TL, Gandley RE, Roberts JM, Patterson CC, Holmes VA, Young IS, et al. Haptoglobin phenotype and preeclampsia incidence in women with type 1 diabetes supplemented with vitamins C and E. Br J Obstet Gynecol. 2013;120(10):1192–9. This secondary analysis of a randomized, controlled trial shows that Hp phenotype does not influence preeclampsia risk or the effectiveness of vitamin C and E supplementation in preventing preeclampsia in women with type 1 diabetes.
Weissgerber TL, Gandley RE, McGee PL, Spong CY, Myatt L, Leveno KJ, et al. Haptoglobin phenotype, preeclampsia risk and the efficacy of vitamin C and E supplementation to prevent preeclampsia in a racially diverse population. PLoS One. 2013;8(4):e60479. doi:10.1371/journal.pone.0060479.
American Diabetes Association. Standards of medical care in diabetes—2014. Diabetes Care. 2014;37 Suppl 1:S14–80. doi:10.2337/dc14-S014.
Jiwani A, Marseille E, Lohse N, Damm P, Hod M, Kahn JG. Gestational diabetes mellitus: results from a survey of country prevalence and practices. J Matern Fetal Neonatal Med. 2012;25(6):600–10. doi:10.3109/14767058.2011.587921.
Wendland EM, Torloni MR, Falavigna M, Trujillo J, Dode MA, Campos MA, et al. Gestational diabetes and pregnancy outcomes—a systematic review of the World Health Organization (WHO) and the International Association of Diabetes in Pregnancy Study Groups (IADPSG) diagnostic criteria. BMC Pregnancy Childbirth. 2012;12:23. doi:10.1186/1471-2393-12-23.
Bellamy L, Casas JP, Hingorani AD, Williams D. Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis. Lancet. 2009;373(9677):1773–9. doi:10.1016/S0140-6736(09)60731-5.
Catalano PM, Ehrenberg HM. The short- and long-term implications of maternal obesity on the mother and her offspring. BJOG. 2006;113(10):1126–33. doi:10.1111/j.1471-0528.2006.00989.x.
Ehrenberg HM, Mercer BM, Catalano PM. The influence of obesity and diabetes on the prevalence of macrosomia. Am J Obstet Gynecol. 2004;191(3):964–8. doi:10.1016/j.ajog.2004.05.052.
Mudd LM, Owe KM, Mottola MF, Pivarnik JM. Health benefits of physical activity during pregnancy: an international perspective. Med Sci Sports Exerc. 2013;45(2):268–77. doi:10.1249/MSS.0b013e31826cebcb.
Schneider S, Freerksen N, Rohrig S, Hoeft B, Maul H. Gestational diabetes and preeclampsia—similar risk factor profiles? Early Hum Dev. 2012;88(3):179–84. doi:10.1016/j.earlhumdev.2011.08.004. By using a perinatal health registry, this study was able to accurately describe prevalence rates for gestational diabetes, preeclampsia, and the co-occurrence of these two conditions within Germany. It also describes risk factors common to both conditions.
Nerenberg KA, Johnson JA, Leung B, Savu A, Ryan EA, Chik CL, et al. Risks of gestational diabetes and preeclampsia over the last decade in a cohort of Alberta women. J Obstet Gynaecol Can. 2013;35(11):986–94.
Ostlund I, Haglund B, Hanson U. Gestational diabetes and preeclampsia. Eur J Obstet Gynecol Reprod Biol. 2004;113(1):12–6. doi:10.1016/j.ejogrb.2003.07.001.
Phaloprakarn C, Tangjitgamol S. Risk assessment for preeclampsia in women with gestational diabetes mellitus. J Perinat Med. 2009;37(6):617–21. doi:10.1515/JPM.2009.108.
Barquiel B, Herranz L, Grande C, Castro-Dufourny I, Llaro M, Parra P, et al. Body weight, weight gain and hyperglycaemia are associated with hypertensive disorders of pregnancy in women with gestational diabetes. Diabetes Metab. 2014;40(3):204–10. doi:10.1016/j.diabet.2013.12.011. This study showed that while pre-pregnancy weight status was the strongest risk factor for preeclampsia, gestational weight gain and glycemic control were also independent risk factors.
Harper LM, Tita A, Biggio JR. The Institute of Medicine guidelines for gestational weight gain after a diagnosis of gestational diabetes and pregnancy outcomes. Am J Perinatol. 2014. doi:10.1055/s-0034-1383846.
Conti E, Zezza L, Ralli E, Caserta D, Musumeci MB, Moscarini M, et al. Growth factors in preeclampsia: a vascular disease model. A failed vasodilation and angiogenic challenge from pregnancy onwards? Cytokine Growth Factor Rev. 2013;24(5):411–25. doi:10.1016/j.cytogfr.2013.05.008.
de Resende Guimaraes MF, Brandao AH, de Lima Rezende CA, Cabral AC, Brum AP, Leite HV, et al. Assessment of endothelial function in pregnant women with preeclampsia and gestational diabetes mellitus by flow-mediated dilation of brachial artery. Arch Gynecol Obstet. 2014;290(3):441–7. doi:10.1007/s00404-014-3220-x.
Kane SC, Costa Fda S, Brennecke S. First trimester biomarkers in the prediction of later pregnancy complications. Biomed Res Int. 2014;2014:807196. doi:10.1155/2014/807196.
Karacay O, Sepici-Dincel A, Karcaaltincaba D, Sahin D, Yalvac S, Akyol M, et al. A quantitative evaluation of total antioxidant status and oxidative stress markers in preeclampsia and gestational diabetic patients in 24–36 weeks of gestation. Diabetes Res Clin Pract. 2010;89(3):231–8. doi:10.1016/j.diabres.2010.04.015.
Wiznitzer A, Mayer A, Novack V, Sheiner E, Gilutz H, Malhotra A, et al. Association of lipid levels during gestation with preeclampsia and gestational diabetes mellitus: a population-based study. Am J Obstet Gynecol. 2009;201(5):482.e1–8. doi:10.1016/j.ajog.2009.05.032.
Zhou J, Zhao X, Wang Z, Hu Y. Combination of lipids and uric acid in mid-second trimester can be used to predict adverse pregnancy outcomes. J Matern Fetal Neonatal Med. 2012;25(12):2633–8. doi:10.3109/14767058.2012.704447.
Wen SW, Xie RH, Tan H, Walker MC, Smith GN, Retnakaran R. Preeclampsia and gestational diabetes mellitus: pre-conception origins? Med Hypotheses. 2012;79(1):120–5. doi:10.1016/j.mehy.2012.04.019. This paper provides a review of hypothesized etiological pathways for preeclampsia and gestational diabetes and argues that both of these conditions have their origins in pre-pregnancy maternal health.
Mastrogiannis DS, Spiliopoulos M, Mulla W, Homko CJ. Insulin resistance: the possible link between gestational diabetes mellitus and hypertensive disorders of pregnancy. Curr Diab Rep. 2009;9(4):296–302.
Landon MB, Spong CY, Thom E, Carpenter MW, Ramin SM, Casey B, et al. A multicenter, randomized trial of treatment for mild gestational diabetes. N Engl J Med. 2009;361(14):1339–48. doi:10.1056/NEJMoa0902430.
Bevier WC, Fischer R, Jovanovic L. Treatment of women with an abnormal glucose challenge test (but a normal oral glucose tolerance test) decreases the prevalence of macrosomia. Am J Perinatol. 1999;16(6):269–75. doi:10.1055/s-2007-993871.
Deveer R, Deveer M, Akbaba E, Engin-Ustun Y, Aydogan P, Celikkaya H, et al. The effect of diet on pregnancy outcomes among pregnant with abnormal glucose challenge test. Eur Rev Med Pharmacol Sci. 2013;17(9):1258–61.
Poolsup N, Suksomboon N, Amin M. Effect of treatment of gestational diabetes mellitus: a systematic review and meta-analysis. PLoS One. 2014;9(3):e92485. doi:10.1371/journal.pone.0092485. This meta-analysis examines the effects of treating gestational diabetes on a range of pregnancy outcomes, including risk of diabetes. Results showed no effect on preeclampsia risk, although only three randomized trials have examined preeclampsia as a secondary outcome and the confidence intervals are extremely wide, indicating low power to detect a relationship.
Chesley LC. Remote prognosis after eclampsia. Perspect Nephrol Hypertens. 1976;5:31–40.
Engeland A, Bjorge T, Daltveit AK, Skurtveit S, Vangen S, Vollset SE, et al. Risk of diabetes after gestational diabetes and preeclampsia. A registry-based study of 230,000 women in Norway. Eur J Epidemiol. 2011;26(2):157–63. doi:10.1007/s10654-010-9527-4. Previous studies had very low power to examine future disease risk among women who developed both gestational diabetes and preeclampsia. Using a national birth registry, this study was able to more precisely estimate the risk of diabetes 5 years postpartum in relation to preeclampsia alone, gestational diabetes alone and both conditions combined.
Feig DS, Shah BR, Lipscombe LL, Wu CF, Ray JG, Lowe J, et al. Preeclampsia as a risk factor for diabetes: a population-based cohort study. PLoS Med. 2013;10(4):e1001425. doi:10.1371/journal.pmed.1001425.
Libby G, Murphy DJ, McEwan NF, Greene SA, Forsyth JS, Chien PW, et al. Pre-eclampsia and the later development of type 2 diabetes in mothers and their children: an intergenerational study from the Walker cohort. Diabetologia. 2007;50(3):523–30. doi:10.1007/s00125-006-0558-z.
Mannisto T, Mendola P, Vaarasmaki M, Jarvelin MR, Hartikainen AL, Pouta A, et al. Elevated blood pressure in pregnancy and subsequent chronic disease risk. Circulation. 2013;127(6):681–90. doi:10.1161/CIRCULATIONAHA.112.128751.
Savitz DA, Danilack VA, Elston B, Lipkind HS. Pregnancy-induced hypertension and diabetes and the risk of cardiovascular disease, stroke, and diabetes hospitalization in the year following delivery. Am J Epidemiol. 2014;180(1):41–4. doi:10.1093/aje/kwu118.
Gordin D, Hiilesmaa V, Fagerudd J, Ronnback M, Forsblom C, Kaaja R, et al. Pre-eclampsia but not pregnancy-induced hypertension is a risk factor for diabetic nephropathy in type 1 diabetic women. Diabetologia. 2007;50(3):516–22. doi:10.1007/s00125-006-0544-5.
Lovestam-Adrian M, Agardh CD, Aberg A, Agardh E. Pre-eclampsia is a potent risk factor for deterioration of retinopathy during pregnancy in type 1 diabetic patients. Diabetic Med. 1997;14(12):1059–65. doi:10.1002/(SICI)1096-9136(199712)14:12<1059::AID-DIA505>3.0.CO;2-8.
Gordin D, Kaaja R, Forsblom C, Hiilesmaa V, Teramo K, Groop PH. Pre-eclampsia and pregnancy-induced hypertension are associated with severe diabetic retinopathy in type 1 diabetes later in life. Acta Diabetol. 2013;50(5):781–7. doi:10.1007/s00592-012-0415-0.
Bell R, Bailey K, Cresswell T, Hawthorne G, Critchley J, Lewis-Barned N, et al. Trends in prevalence and outcomes of pregnancy in women with pre-existing type I and type II diabetes. BJOG. 2008;115(4):445–52. doi:10.1111/j.1471-0528.2007.01644.x.
Acknowledgments
Tracey L. Weissgerber and Lanay M. Mudd were supported by Building Interdisciplinary Careers in Women’s Health awards from the Office of Women’s Health Research (TLW: K12HD065987; LMM: K12HD065879-03).
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
Tracey L. Weissgerber and Lanay M. Mudd declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Diabetes and Pregnancy
Rights and permissions
About this article
Cite this article
Weissgerber, T.L., Mudd, L.M. Preeclampsia and Diabetes. Curr Diab Rep 15, 9 (2015). https://doi.org/10.1007/s11892-015-0579-4
Published:
DOI: https://doi.org/10.1007/s11892-015-0579-4