Abstract
Diabetic nephropathy, by far, is the most common cause of end stage renal disease in the US and many other countries. In type 1 diabetes, the natural history of diabetic nephropathy is tightly linked to evolution of classic lesions of the disease, namely glomerular basement membrane thickening, increased mesangial matrix, and reduced glomerular filtration surface density. These lesions progress in parallel and correlate with increased albumin excretion rate and reduced glomerular filtration rate across a wide range of renal function. In fact, the vast majority of the variances of albumin excretion and glomerular filtration rates can be explained by these glomerular lesions alone in type 1 diabetic patients. Although, classic lesions of diabetic nephropathy, indistinguishable from those of type 1 diabetes, also occur in type 2 diabetes, renal lesions are more heterogeneous in type 2 diabetic patients with some patients developing more advanced vascular or chronic tubulointerstitial lesions than diabetic glomerulopathy. More research biopsy longitudinal studies, especially in type 2 diabetic patients, are needed to better understand various pathways of renal injury in diabetic nephropathy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetic nephropathy is the leading cause of end-stage renal disease (ESRD) in the Western World. Type 2 (T2D) and, to a lesser extent, type 1 diabetes (T1D) combined account for >47 % of all new cases of ESRD in the United States [1]. The annual incidence of new cases of diabetes-related ESRD is steadily increasing in the United States, this despite overall improvements in managing hyperglycemia and hypertension and the availability of renin-angiotensin system blocking agents in the last decades [2].
Diabetic nephropathy results from a series of specific progressive renal pathological changes that start early in the course of diabetes, and progress during a long clinically silent period until features of clinical renal disease—including proteinuria, hypertension, and declining glomerular filtration rate (GFR)—become evident. Unfortunately, treatment initiated after the development of overt clinical nephropathy usually cannot arrest progression to ESRD. Thus, there is a need to identify predictors of diabetic nephropathy risk early in the course of diabetes in order to develop effective prevention strategies. This goal cannot be met without understanding the natural history of the disease.
This manuscript reviews evolution of classic diabetic nephropathy lesions, including glomerular basement membrane thickening, mesangial expansion, and reduced glomerular filtration surface density, as well as arteriolar hyalinosis, and tubulointerstitial chronic changes in relation to diabetes duration and renal function in an attempt to provide a comprehensive picture of the natural history of progression of this disease. We also provide an overview of podocyte injury and its role in evolution of segmental and eventually global glomerulosclerosis, as well as structural-functional relationships of diabetic nephropathy. At the end, we compare diabetic nephropathy lesions in patients with T1D vs T2D.
Glomerular Basement Membrane Thickening
The hallmark of diabetic nephropathy is accumulation of extracellular matrix within the glomerulus manifested by thickening of the glomerular basement membrane (GBM) and increase in the volume fraction of the glomerulus occupied by mesangium [Vv(Mes/glom)] (Fig. 1).
Classic lesions of diabetic nephropathy: a-c light microscopy (PAS stain) images of a a glomerulus from a nondiabetic patient with normal tight mesangium (arrowhead) and a normal arteriole (arrow) with no hyalinosis; b a glomerulus with diffuse mild to moderate mesangial expansion from a diabetic patient. The mesangial regions (arrowhead) are expanded predominantly due to matrix accumulation; c a glomerulus with advanced diabetic nephropathy, Kimmelstiel-Wilson nodules (asterisk) and prominent arteriolar hyalinosis (arrow). d-e Transmission electron micrographs from glomeruli with d normal structure, e mild to moderate diabetic nephropathy, and f advanced diabetic nephropathy. Note progressive glomerular basement membrane (spiral arrows) thickening and mesangial matrix (asterisks) accumulation from d to f. The squares show intact foot processes in (d) and progressive foot process effacement in (e) and f indicative of podocyte injury in diabetic nephropathy
GBM thickening is the earliest detectable glomerular structural change in diabetic patients (Fig. 1d–f) if carefully measured using unbiased stereological methods [3]. Thickening of the GBM can be detected as early as 1.5–2.5 years after the onset of T1D [3], although it should be noted that there is substantial overlap of GBM thickness values between patients with T1D and normoalbuminuria and nondiabetic subjects [4•]. This overlap is in part due to variability of the rate of progression of diabetic nephropathy lesions among the patients. Moreover, in the absence of knowledge about baseline (pre-diabetes) values of GBM thickness, a detection of change in this parameter due to diabetes may be challenging, a caveat that holds true for modest changes of most structural parameters discussed in this manuscript as well. In a study of identical diabetic twins, discordant for T1D, all diabetic twins had thicker GBM and greater Vv(Mes/glom) compared with their nondiabetic twins, while some of the values for the diabetic twins were still within the “normal range” [5]. Assuming that before the onset of T1D, diabetic, and nondiabetic twins had similar GBM thickness and Vv(Mes/glom) values, this study signifies the importance of longitudinal biopsies in detection of early progression of diabetic nephropathy lesions. Thickening of the GBM in diabetes is diffuse and quite uniform, although especially in advanced diabetic nephropathy, rare capillary loops with thin GBM can be seen, which are postulated to represent new capillary formation in the glomeruli [6]. Similarly, in the later stages of diabetic nephropathy, occasional irregularities in the GBM, consistent with remodeling are observable.
GBM is normally composed of 3 ultrastructurally distinct components of lamina rara externa (immediately underneath the foot processes), lamina densa (in the middle and more electron dense), and the lamina rara interna (subendothelial). GBM thickening in diabetic nephropathy is primarily due to expansion of lamina densa. Expansion of lamina rara interna, usually in a segmental distribution and less marked than lamina densa, becomes more noticeable in established diabetic nephropathy, and especially when accompanied by mesangiolysis.
Mesangial Expansion
The various lesions of diabetic nephropathy may evolve and progress at differing rates [4•, 7]. While GBM width tends to increase more or less linearly with increasing diabetes duration, Vv(Mes/glom), on average, changes little in the first 15 years and increases more rapidly thereafter, although it can sometimes be detected after only 4 to 5 years [8]. This may explain the association between greater GBM width at earlier stages of the disease and the later development of microalbuminuria, whereas Vv(Mes/glom) is a stronger correlate of albuminuria and declining GFR with longer diabetes duration [9•]. Progressive mesangial expansion is characterized by a greater increase in mesangial matrix than of mesangial cell fractional volume [8]. In early diabetic nephropathy, even when Vv(Mes/glom) is still within the normal range, fractional volume of the glomerulus occupied by mesangial matrix Vv(MM/glom) is often found increased [10].
Mesangial expansion can be diffuse, ie, more or less uniform within glomeruli or may be nodular (Kimmelstiel-Wilson nodules), characterized by round areas of marked mesangial expansion with palisading of mesangial nuclei around the periphery of the nodule often with extreme compression of the adjacent glomerular capillaries (Fig. 1c). Although, nodular mesangial expansion is usually a late finding and is typically concomitant with moderate to severe diffuse mesangial expansion, occasionally these nodules are found in biopsies with only mild diffuse mesangial expansion, suggesting that these 2 forms of diabetic mesangial change may, at least in part, have different pathogeneses. It is likely that mesangiolysis secondary to focal detachment of capillary wall from mesangial anchoring points to the GBM resulting in glomerular microaneurysms is a precursor to these Kimmelstiel-Wilson nodules [11].
Reduced Glomerular Filtration Surface Density
Mesangial expansion is associated with reduction of the available filtration surface per glomerulus [8]. Glomerular filtration surface per glomerulus, as one would expect, correlates nicely with GFR across a wide range from hyperfiltration to prominently reduced GFR values. This association has been recently confirmed in Japanese patients with T2D as well [12]. It should be noted that increased glomerular volume, at least to some extent, compensates for reduced glomerular filtration surface density. However, increased glomerular volume, in contrast to animal models of diabetic nephropathy, is a relatively late finding in humans with T1D [13, 14].
Nephron endowment, an important predictor of GFR, glomerular volume, and thus total glomerular filtration surface, can vary markedly among normal individuals and among patients with diabetes [15].
Podocyte Injury
Podocytes are essential components of the glomerular filtration barrier. Podocyte injury is often associated with foot process widening and albuminuria/proteinuria. Podocyte damage and loss can lead to segmental and global glomerulosclerosis [16].
Nephrin excretion in the urine (nephrinuria) can be detected in about 1/3 of normoalbuminuric diabetic patients, indicative of early podocyte injury in diabetic nephropathy even before the onset of microalbuminuria [17].
Foot process widening is detectable in the early stages of diabetic nephropathy, when patients are still normoalbuminuric [18] and becomes more severe with increasing albumin excretion rate (AER) [19]. Podocyte injury, if severe enough, leads to podocyte loss. Increased number of podocytes in the urine from patients with T2D and microalbuminuria or proteinuria confirms podocyte loss in diabetic nephropathy [20]. Since podocytes do not efficiently proliferate, podocyte loss can lead to reduced podocyte number in the glomeruli. White et al. reported an inverse relationship between AER and podocyte number density per glomerulus [Nv(Podo/glom)] in patients with T1D and proteinuria [16]. Interestingly, this study did not find a reduction in total podocyte number per glomerulus [N(Podo/glom)] in patients with T1D and proteinuria compared with nondiabetic control subjects. In contrast, Steffes et al. suggested that N(Podo/glom) reduces in patients with T1D and normoalbuminuria [21]. However, the methodologies used in these 2 studies were different, making any comparison questionable. Reduced N(Podo/glom) has also been shown in patients with T2D and proteinuria [22, 23]. A decrease in Nv(Podo/glom) can be consequent to increased glomerular volume, decrease in N(Podo/glom), or a combination of both factors. However, given that increased glomerular volume is not an early finding in diabetic nephropathy in T1D patients [14], reduced Nv(Podo/glom) due to increased glomerular volume cannot fully account for early changes in these podocyte parameters.
Podocyte injury can lead to GBM denudation [19, 24, 25] promoting synechiae formation between the glomerular tuft and Bowman’s capsule, an initial step in the development of segmental glomerulosclerosis. Tuft to Bowman’s capsule adhesions are frequently found at the glomerulotubular junction area, the so-called “tip lesion” in patients with T1D (Fig. 2) [26••, 27]. It has been postulated that podocytes are more vulnerable to mechanical injury due to shear stress at the tubular pole of the glomerular tuft [28]. Thus, a combination of podocyte and tubular epithelial cell injury at the glomerulotubular junction area, perhaps in part, secondary to proteinuria, may be responsible for emergence of these lesions in proteinuric diabetic patients. Segmental glomerulosclerosis (secondary type) either at the glomerulotubular junction or other regions of the glomerulus is a relatively late finding of nephropathy in patients with T1D. These lesions eventually lead to nephron loss either through progressive obstruction of glomerular tubular outlet (Fig. 2) and formation of atubular glomeruli, or evolving into globally sclerosed glomeruli, and in this way, ultimately contributing to the progression of GFR loss [26••].
A glomerulus with advanced diabetic nephropathy and a Kimmelstiel-Wilson nodule (white asterisk) shows adhesion of tuft to Bowman's capsule at the glomerulotubular junction (tip lesion, arrow) completely occluding the glomerular tubular outlet. The spiral arrow shows atrophic tubules. The white asterisk shows a globally sclerosed glomerulus with microaneurysm (Jones methenamine silver stain)
Tubular Basement Membrane Thickening
The tubular basement membrane (TBM) width is diffusely increased in diabetes, even among the patients with normoalbuminuria. TBM width in diabetic patients strongly correlates with GBM width and Vv(Mes/glom) but only weakly with the volume fraction of renal cortex that is interstitium [Vv(Int/cortex)] [5, 29]. The precision of the correlations of proximal TBM width with GBM width and with Vv(Mes/glom) are similar to that of Vv(Mes/glom) and GBM width to each other, indicating that these structural changes are occurring in diabetic patients roughly in parallel. Given that TBM and GBM thickening are both sensitive indicators of the severity of hyperglycemia, it is more likely that the TBM, GBM and mesangial structural abnormalities are primarily due to the metabolic derangement of the diabetic state leading to basement membrane extracellular matrix accumulation [29].
Tubulointerstitial Fibrosis
Interstitial fibrosis has been generally accepted as the best histologic correlate of GFR in glomerular diseases. A number of studies have suggested that GFR loss at the time of kidney biopsy correlates better with the morphometrically determined volume fraction of the cortical interstitium [Vv(Int/cortex)], regardless of the type of glomerular disease [30, 31]. However, when classic glomerular lesions of diabetic nephropathy are carefully assessed using precise morphometric methods in diabetic patients, the relationships between renal dysfunction and glomerular structural changes become stronger than Vv(Int/cortex)[26••] through most of the natural history of the disease from early stages to moderately advanced GFR loss. In fact, glomerular structural parameters alone can predict GFR much better than Vv(Int/cortex) across a wide range of GFR, from hyperfiltration to GFR values above chronic kidney disease stage IV (ie, to GFR levels of ~ 30–40 mL/min/1.73 m2) when already substantial cortical scarring is present in the kidney (see Structural – Functional Relationships of Diabetic Nephropathy below).
Of note, while in early stages of diabetic nephropathy in patients with T1D, interstitial fractional volume per cortex Vv(Int/cortex) is reduced, probably because of tubular enlargement without proportional interstitial expansion, early glomerular changes are already detectable [32].
Initially, interstitial expansion is primarily due to an increase in the cellular component. Further increase in Vv(Int/cortex) is largely due to the occurrence of true interstitial fibrosis, that is, an increase in the volume fraction of collagen fibrils within the interstitium [32].
Tubulointerstitial fibrosis in diabetic nephropathy, similar to other chronic kidney diseases, is associated with reduced peritubular capillaries, which perhaps through decreased delivery of oxygen and nutrients to interstitial and tubular epithelial cells, accentuates interstitial fibrosis through a vicious cycle.
Exudative and Vascular Lesions
Exudative lesions of diabetic nephropathy include arteriolar hyalinosis (Fig. 1c), hyaline caps (glomerular capillary subendothelial hyaline accumulation) and capsular drops (hyaline material accumulation underneath parietal epithelial cells). Concomitant hyalinosis of afferent and efferent arterioles is characteristic of, but not restricted to diabetic nephropathy. Arteriolar hyalinosis can be seen as early as 3 to 5 years following the onset of T1D [33]. Severe arteriolar hyalinosis correlates with global glomerulosclerosis in diabetic nephropathy [34]. Increased number of efferent arterioles can be seen in glomeruli with advanced diabetic nephropathy [35] (Fig. 3). Arteriosclerosis or intimal fibrosis is a common finding in biopsies with advanced diabetic nephropathy. While the contribution of arteriosclerosis to nephron loss may be less appreciated in biopsy specimens, study of autopsy nephrectomies showed that globally sclerosed glomeruli were distributed in a vascular branching pattern in patients with advanced diabetic nephropathy [36].
Structural–Functional Relationships of Diabetic Nephropathy
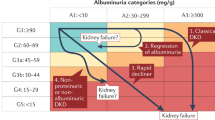
The natural history of diabetic nephropathy includes an initial long clinically silent period during which the patient remains normoalbuminuric with a normal or high GFR. Renal lesions that develop during this time may substantially overlap with normal values, but also may be as severe as those commonly seen in patients with microalbuminuria, and to a less extent, even in those with proteinuria. Once persistent microalbuminuria develops, glomerular lesions are overall worse than in patients with normoalbuminuria [4•]. Persistent microalbuminuria is associated with substantially increased risk for progression to proteinuria. GFR may remain preserved during microalbuminuria, but almost always progressively declines once proteinuria is established [26••]. On the other hand, patients with microalbuminuria and GFR decline are highly likely to progress to overt nephropathy, while those with preserved GFR may remain microalbuminuric or revert to normoalbuminuria [37].
Using simple linear regression analysis in patients with T1D and across a wide range of AER, from normoalbuminuria to proteinuria, Vv(Mes/glom) and GBM width directly and Sv(PGBM/glom) inversely correlate with AER. Among the classic glomerular structural parameters of diabetic nephropathy, Vv(Mes/glom), fractional volume of mesangial matrix per glomerulus [Vv(MM/glom)] and Sv(PGBM/glom) show the strongest relationships with GFR [4•]. Since glomerular structural parameters are remarkably inter-related [4•], multiple regression analysis more accurately describes individual and combined contribution of these structural parameters in renal function. In a small cohort of patients with T1D, using multiple regression analysis, Vv(Mes/glom), total glomerular filtration surface,, and GBM width as predictors explained about 67 % of GFR variance [26••], a relationship which was confirmed in a large cohort of patients with T1D as well (Najafian et al., unpublished data) . The addition of glomerulotubular junction abnormalities (GTJA) to this multiple regression model increased the GFR predictability to 75 % [26••], and a combination of glomerular structural parameters [Vv(Mes/glom), GBM width, and total glomerular filtration surface], GTJA, percentage of globally sclerosed glomeruli, and Vv(Int/cortex), explained 86 % of the GFR variance. Using multiple regression analyses, Vv(Mes/glom), total filtration surface, and GBM width explained 65 % of the observed AER variance with Vv(Mes/glom) and GBM width as independent predictor variables. Incorporation of GTJA increased the predictability of this multiple regression model to 72 % with Vv(Mes/glom) and GTJA as independent predictors. The addition of Vv(Int/cortex) did not substantially change this model [26••]. Taken together, these data suggest that, if carefully measured, glomerular structural changes alone can explain the vast majority of renal dysfunction in type 1 diabetic patients. Considering that the above mentioned relationships are obtained from averaging structural parameters in only 3 out of well over a million glomeruli, the T1D lesions among the glomeruli must be reasonably uniformly distributed.
The structural-functional relationship models of diabetic nephropathy mirror its clinical course and natural history, in that an initial slow progression of the disease is followed by an accelerated phase with rapid renal functional decline. In a relatively small number of patients with T1D, using piecewise linear regression (PLRA) analysis glomerular structural parameters alone [Vv(Mes/glom), GBM width, and total filtration surface] explained 95 % of the observed AER variability (with a model breakpoint in the microalbuminuria range), leaving almost no room for any other variable to improve the predictions [26••]. While, this smaller number of patients could lead to over-fitting of the models, evaluation of glomerular structural-functional relationships in a much larger cohort of patients with T1D yielded similar, albeit less strong, correlations (Najafian et al., unpublished data). In the same small cohort, PLRA explained 78 % of GFR variance by classic diabetic nephropathy glomerular structural parameters, with the model breakpoint at 110 mL/min. Adding GTJA to the model increased the predictability of the model by about 10 % and adding both GTJA and Vv(Int/cortex) increased the predictability by about 18 % [26••]. It is noteworthy that in the above PLRA models, the breakpoints where a steep change in the slope of relationships between glomerular structural parameters and renal function occurs, were in the microalbuminuric (52 μg/min) and normal GFR (110 mL/min/1.73 m2) ranges. These findings suggest that significant glomerular lesions are already in place (which set the stage for an accelerated phase of renal dysfunction), while patients are microalbuminuric and GFR is still relatively well preserved, albeit at lower than the initial hyperfiltration levels so common at earlier stages. In other words, microalbuminuria and GFR, especially using estimates from serum creatinine or Cystatin C, are not sensitive enough for monitoring early progression of diabetic nephropathy in patients with T1D. The structural-functional relationships of diabetic nephropathy are much stronger after these breakpoints, while in the initial phase (pre-breakpoint), perhaps the intrinsic inter-individual variability in renal structure masks these relationships.
Diabetic Nephropathy in Type 2 Diabetes
Albeit T2D is a much greater contributor to ESRD due to diabetes, the natural history of diabetic nephropathy in patients with T2D is, as yet, relatively poorly defined. The lack of precise knowledge about the onset of diabetes in majority of T2D, with the exception of the Pima Indian studies, is a clear challenge in studying the natural history of diabetic nephropathy in these patients. Classic lesions of diabetic nephropathy indistinguishable from those seen in patients with T1D, with GBM thickening, increased mesangial matrix and Kimmelstiel-Wilson nodules, may occur in patients with T2D as well [38]. Studies of Pima Indian patients with T2D who are regularly followed up with serial information about renal function and metabolic status have been valuable in understanding diabetic nephropathy in T2D [39]. However, given that the genetic background, relatively early age of onset and common environmental factors may be less heterogeneous in this cohort than the general population, one should be cautious in extrapolating the findings of these studies to all patients with T2D (see below). Pagtalunan et al. found that Pima Indian patients with T2D and microalbuminuria had greater glomerular and mesangial volume compared with those with less duration of diabetes; however, those values were not different from diabetes duration matched patients with normoalbuminuria [22].
The rate of GFR decline among Pima Indians with T2D is similar to that of white patients with T1D. The onset of T2D in Pima Indians is associated with hyperfiltration that persists until the development of persistent macroalbuminuria when GFR declines progressively afterward. A morphometric study of glomerular structural parameters in Pima Indian patients with T2D and micro- or macroalbuminuria suggested that reduced GFR in the macroalbuminuric subjects was associated with reduced glomerular ultrafiltration coefficient (Kf), although the estimated net pressure for ultrafiltration was actually higher in overt than in incipient nephropathy [40]. It was suggested that foot process widening, through reduction in filtration slit frequency, may have reduced the ultrafiltration capacity in patients with macroalbuminuria. On the other hand, GBM thickening would additionally contribute into GFR decline through reducing hydraulic permeability [40].
In the majority of white patients with T2D and microalbuminuria, glomeruli are essentially unremarkable by light microscopy and otherwise show mild GBM thickening and mesangial matrix accumulation, while the total filtration surface remains preserved as a result of glomerular hypertrophy. Similar findings occur in Pima Indian patients with long-standing T2D and normoalbuminuria, suggesting that these findings are a consequence of diabetes per se and are not necessarily related to albuminuria [40].
Overall, renal lesions are more heterogeneous in white patients with T2D compared with those with T1D. Different studies have suggested prevalence of nondiabetic lesions in patients with T2D and proteinuria may vary from 12 %–30 % [41]. However, selection bias caused by studying clinical, as opposed to research, biopsies may have significantly overestimated the true prevalence of nondiabetic lesions in patients with T2D [42]. In a study of research renal biopsies in a large cohort of patients with T2D and microalbuminuria or proteinuria, renal lesions were found to be heterogeneous [43]. In fact, classic diabetic nephropathy lesions, similar to those found in patients with T1D were found only in a minority subset of patients; while the majority had only mild or almost no diabetic glomerulopathy, and had normal or near normal renal biopsies (~1/3) or showed pronounced tubulointerstitial, arteriolar, and global glomerulosclerosis (~1/3) [43]. Overall, within the same range of AER, diabetic glomerulopathy lesions are milder in patients with T2D 2 compared with T1D. Using cluster analyses, we have found that about 1/3 of patients with T2D have distinctly greater AER relative to glomerulopathy lesions based on structural-functional relationships developed from patients with T1D (Fioretto et al., unpublished data). These findings suggest that diabetes may induce different patterns of renal injury in patients with T1D compared with T2D. Alternatively, aging, obesity, atherosclerosis, and systemic hypertension which are commonly present concomitant attributes of T2D could be at least partially responsible for the disproportionate tubulointerstitial, glomerulosclerotic, and vascular changes in these patients. The effect of various patterns of renal injury in patients with T2D on long term outcome and natural history of diabetic nephropathy remains to be unraveled.
Pathologic Classification of Diabetic Nephropathy
A uniform style of reporting pathologic changes of diabetic nephropathy is undoubtedly of clinical importance. A common reason to biopsy diabetic patients is to examine if renal dysfunction (especially proteinuria) can be explained by diabetic nephropathy alone or concomitant renal diseases exist. As we pointed out above, clinical biopsies, usually done because of atypical clinical presentations, caused a selection bias and overestimation of nondiabetic kidney diseases, especially in patients with T2D. [41]. A pathologic classification for both T1D and T2D based on classic lesions of diabetic nephropathy has been proposed by Tervaert et al. [44]. This classification system includes 4 progressive classes based on GBM thickening (class I), mesangial expansion (class II), presence of Kimmelstiel-Wilson nodules (class III), and extensive global glomerulosclerosis (class IV). This classification is a step towards developing a clinically useful pathology reporting system. However, a few important aspects of diabetic nephropathy, such as heterogeneity of patterns of renal injury in T2D, and tubulointerstitial and vascular lesions are not included in this classification [45]. A recent study of patients with T2D and proteinuria found that, while glomerular classes were not significant predictors of renal outcome, interstitial fibrosis, tubular atrophy, and interstitial inflammation were independent variables associated with kidney survival [46]. However, another study of patients with T2D found that 5-year kidney survival correlated with glomerular classes [47], but the independent contribution of glomerular, tubulointerstitial and vascular lesions were not evaluated. Whether this classification has any prognostic value in early stages of diabetic nephropathy, when a biomarker is mostly needed to guide treatment options and outcomes, remains to be validated.
Conclusions
The natural history of diabetic nephropathy in both T1D and T2D is characterized by a long clinically silent period followed by an accelerated phase of renal functional decline. Most studies analyzing glomerular structural changes and structural–functional relationships of diabetic nephropathy in research biopsies have been performed in patients with T1D. These studies indicate that classic lesions of diabetic glomerulopathy, including GBM thickening, mesangial expansion, and reduced filtration surface density evolve and progress largely in parallel and correlate with progression of albuminuria and GFR loss across a wide range of renal function. The vast majority of variances of AER and GFR can be explained by these glomerular structural parameters alone, especially when nonlinear regression models are used. Interstitial fibrosis follows glomerular lesions and is a late finding in T1D. Our knowledge about the natural history and structural-functional relationships of diabetic nephropathy in T2D is far less well known than in T1D. It appears that renal lesions are more heterogeneous in T2D compared with T1D. A substantial fraction of patients with T2D, may have significant proteinuria while lacking advanced diabetic glomerulopathy lesions, There is a great need to have more research biopsy longitudinal studies, especially in patients with T2D to better understand the natural history and pathophysiologic mechanism involved in development and progression in this by far the most common cause of ESRD.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
USRDS, U S Renal Data System, USRDS 2012 Annual Data Report. Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda. 2012.
Krolewski AS, Bonventre JV. High risk of ESRD in type 1 diabetes: new strategies are needed to retard progressive renal function decline. Semin Nephrol. 2012;32:407–14.
Osterby R. Kidney structural abnormalities in early diabetes. Adv Metab Disord. 1973;2 Suppl 2:323–40.
• Caramori ML et al. Cellular basis of diabetic nephropathy: 1. Study design and renal structural-functional relationships in patients with long-standing type 1 diabetes. Diabetes. 2002;51:506–13. This study describes structural-functional relationships of diabetic nephropathy in a wide range of renal function in type 1 diabetic patients in a cross-sectional design.
Steffes MW et al. Studies of kidney and muscle biopsy specimens from identical twins discordant for type I diabetes mellitus. N Engl J Med. 1985;312:1282–7.
Osterby R, Nyberg G. New vessel formation in the renal corpuscles in advanced diabetic glomerulopathy. J Diabetes Complicat. 1987;1:122–7.
Mauer SM et al. Structural-functional relationships in diabetic nephropathy. J Clin Invest. 1984;74:1143–55.
Steffes MW et al. Cell and matrix components of the glomerular mesangium in type I diabetes. Diabetes. 1992;41:679–84.
• Steinke JM et al. The early natural history of nephropathy in Type 1 Diabetes: III. Predictors of 5-year urinary albumin excretion rate patterns in initially normoalbuminuric patients. Diabetes. 2005;54:2164–71. This study describes early glomerular structural changes in type 1 diabetic patients in a large cohort and examines which parameters at baseline predict progression to microalbuminuria at 5 years follow up.
Drummond K, Mauer M. The early natural history of nephropathy in type 1 diabetes: II. Early renal structural changes in type 1 diabetes. Diabetes. 2002;51:1580–7.
Saito Y et al. Mesangiolysis in diabetic glomeruli: its role in the formation of nodular lesions. Kidney Int. 1988;34:389–96.
Moriya T et al. Glomerular hyperfiltration and increased glomerular filtration surface are associated with renal function decline in normo- and microalbuminuric type 2 diabetes. Kidney Int. 2012;81:486–93.
Osterby R et al. Glomerular volume and the glomerular vascular pole area in patients with insulin-dependent diabetes mellitus. Virchows Arch. 1997;431:351–7.
Bilous RW et al. Mean glomerular volume and rate of development of diabetic nephropathy. Diabetes. 1989;38:1142–7.
Bendtsen TF, Nyengaard JR. The number of glomeruli in type 1 (insulin-dependent) and type 2 (noninsulin-dependent) diabetic patients. Diabetologia. 1992;35:844–50.
White KE et al. Podocyte number in normotensive type 1 diabetic patients with albuminuria. Diabetes. 2002;51:3083–9.
Patari A et al. Nephrinuria in diabetic nephropathy of type 1 diabetes. Diabetes. 2003;52:2969–74.
Perrin NE et al. The course of diabetic glomerulopathy in patients with type I diabetes: a 6-year follow-up with serial biopsies. Kidney Int. 2006;69:699–705.
Toyoda M et al. Podocyte detachment and reduced glomerular capillary endothelial fenestration in human type 1 diabetic nephropathy. Diabetes. 2007;56:2155–60.
Nakamura T et al. Urinary excretion of podocytes in patients with diabetic nephropathy. Nephrol Dial Transplant. 2000;15:1379–83.
Steffes MW et al. Glomerular cell number in normal subjects and in type 1 diabetic patients. Kidney Int. 2001;59:2104–13.
Pagtalunan ME et al. Podocyte loss and progressive glomerular injury in type II diabetes. J Clin Invest. 1997;99:342–8.
Dalla Vestra M et al. Is podocyte injury relevant in diabetic nephropathy? Studies in patients with type 2 diabetes. Diabetes. 2003;52:1031–5.
Weil EJ et al. Podocyte detachment in type 2 diabetic nephropathy. Am J Nephrol. 2011;33 Suppl 1:21–4.
Weil EJ et al. Podocyte detachment and reduced glomerular capillary endothelial fenestration promote kidney disease in type 2 diabetic nephropathy. Kidney Int. 2012;82:1010–7.
•• Najafian B et al. Glomerulotubular junction abnormalities are associated with proteinuria in type 1 diabetes. J Am Soc Nephrol. 2006;17(4 Suppl 2):S53–60. This study describes glomerulotubular junctionabnormalities in diabetic nephropathy in type 1 diabetes. In addition, it suggests through structural-functional relationship models that the vast majority of AER and GFR variance in type 1 diabetic patients can be explained by glomerular lesions alone.
Najafian B et al. Atubular glomeruli and glomerulotubular junction abnormalities in diabetic nephropathy. J Am Soc Nephrol. 2003;14:908–17.
Friedrich C et al. Podocytes are sensitive to fluid shear stress in vitro. Am J Physiol Ren Physiol. 2006;291:F856–65.
Brito PL et al. Proximal tubular basement membrane width in insulin-dependent diabetes mellitus. Kidney Int. 1998;53:754–61.
Thomsen OF et al. Renal changes in long-term type 1 (insulin-dependent) diabetic patients with and without clinical nephropathy: a light microscopic, morphometric study of autopsy material. Diabetologia. 1984;26:361–5.
Bohle A et al. The pathogenesis of chronic renal failure in diabetic nephropathy. Investigation of 488 cases of diabetic glomerulosclerosis. Pathol Res Pract. 1991;187:251–9.
Katz A et al. An increase in the cell component of the cortical interstitium antedates interstitial fibrosis in type 1 diabetic patients. Kidney Int. 2002;61:2058–66.
Mauer SM et al. Development of diabetic vascular lesions in normal kidneys transplanted into patients with diabetes mellitus. N Engl J Med. 1976;295:916–20.
Harris RD et al. Global glomerular sclerosis and glomerular arteriolar hyalinosis in insulin dependent diabetes. Kidney Int. 1991;40:107–14.
Osterby R et al. Neovascularization at the vascular pole region in diabetic glomerulopathy. Nephrol Dial Transplant. 1999;14:348–52.
Horlyck A, Gundersen HJ, Osterby R. The cortical distribution pattern of diabetic glomerulopathy. Diabetologia. 1986;29:146–50.
Perkins BA et al. Microalbuminuria and the risk for early progressive renal function decline in type 1 diabetes. J Am Soc Nephrol. 2007;18:1353–61.
Hayashi H et al. An electron microscopic study of glomeruli in Japanese patients with noninsulin dependent diabetes mellitus. Kidney Int. 1992;41:749–57.
Lemley KV. Diabetes and chronic kidney disease: lessons from the Pima Indians. Pediatr Nephrol. 2008;23:1933–40.
Lemley KV et al. Evolution of incipient nephropathy in type 2 diabetes mellitus. Kidney Int. 2000;58:1228–37.
Fioretto P, Mauer M. Histopathology of diabetic nephropathy. Semin Nephrol. 2007;27:195–207.
Mazzucco G et al. Different patterns of renal damage in type 2 diabetes mellitus: a multicentric study on 393 biopsies. Am J Kidney Dis. 2002;39:713–20.
Fioretto P et al. Patterns of renal injury in NIDDM patients with microalbuminuria. Diabetologia. 1996;39:1569–76.
Tervaert TW et al. Pathologic classification of diabetic nephropathy. J Am Soc Nephrol. 2010;21:556–63.
Fioretto P, Mauer M. Diabetic nephropathy: diabetic nephropathy-challenges in pathologic classification. Nat Rev Nephrol. 2010;6:508–10.
Okada T et al. Histological predictors for renal prognosis in diabetic nephropathy in diabetes mellitus type 2 patients with overt proteinuria. Nephrology. 2012;17:68–75.
Oh SW et al. Clinical implications of pathologic diagnosis and classification for diabetic nephropathy. Diabetes Res Clin Pract. 2012;97:418–24.
Acknowledgments
This work was in part supported by grants from the National Institutes of Health (NIH) (DK13083) and 2P01DK013083 and National Center for Research Resources (MO1-KK00400). Behzad Najafian has received a subaward of N001447101 from NIH.
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
Cecilia Ponchiardi declares that she has no conflict of interest.
Michael Mauer declares that he has no conflict of interest.
Behzad Najafian is a PI and co-PI of grants supported by the Genzyme and Roche.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ponchiardi, C., Mauer, M. & Najafian, B. Temporal Profile of Diabetic Nephropathy Pathologic Changes. Curr Diab Rep 13, 592–599 (2013). https://doi.org/10.1007/s11892-013-0395-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11892-013-0395-7