Abstract
Purpose of Review
The current standard treatment for locally advanced or metastatic colorectal cancer often includes radiotherapy delivered under computed tomography (CT)–based image guidance. Magnetic resonance–guided radiotherapy (MRgRT) offers a substantial improvement in target and adjacent organ visualization and allows for real-time imaging throughout treatment to ensure target accuracy with each fraction. However, this technology is in its relative infancy, with many open questions regarding how to maximize the potential of this new treatment modality. We review the literature and share our institutional experience to highlight the strengths and limitations of MRgRT for treatment of colorectal cancer.
Recent Findings
MRgRT is safe and effective in both the locally advanced and metastatic settings. Dose can be safely escalated in locally advanced cases, potentially improving rates of pathologic complete response. Functional imaging offers insight into treatment response dynamics, opening the possibility for nonoperative management of select cases. Liver metastases can be treated to ablative doses with high rates of local control.
Summary
MRgRT has the potential to shift the paradigm of treatment for locally advanced and metastatic colorectal cancer. Improved target accuracy and real-time gating allows for dose prescriptions beyond what has been achievable with CT-based imaging, allowing for higher rates of tumor control with no significant increase in toxicity. Future work will focus on optimal dose fractionation schemes and functional radiographic assessment of tumor response.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Radiation therapy (RT) remains a cornerstone of cancer treatment, and up to 60% of all patients with cancer undergo RT at some point in their care, whether with curative or palliative intent [1, 2]. Advances in technology have led to increasingly conformal and accurate delivery of RT. The first major advance of the modern era was through the use of intensity-modulated RT (IMRT) with image guidance (IGRT). The IMRT technique modulates both the geometry and amount of radiation delivered through various beam angles in order to create highly complex and conformal dose plans capable of delivering appropriate dose to target structures while minimizing dose to adjacent organs at risk (OARs). A subsequent development was to dramatically increase the dose delivered per fraction via stereotactic body radiotherapy (SBRT). Because the dose gradients used in highly conformal plans are steep, reproducible and accurate alignment is required to ensure that the target remains in the high-dose region for each fraction of RT. IGRT encompasses a range of solutions for ensuring accurate daily targeting, and is most commonly performed using on-board imaging solutions including cone-beam computed tomography (CBCT) and stereoscopic pairs of x-ray images.
Although CBCT is commonly used for daily target alignment in the delivery of RT, magnetic resonance imaging (MRI) is often preferred in the target segmentation step of RT planning due to superior soft tissue contrast as compared with CT [3, 4]. This allows for more accurate delineation of target and avoidance structures and improves plan generation. Ultimately, though, delivery of these more accurate plans is limited by the inability for conventional CBCT to isolate soft tissue targets amid surrounding isodense OARs. In contrast, MRI integrated into the treatment platform offers substantial benefits to treatment planning and delivery. MRI performed just before daily RT offers the potential for online adaptive therapy based on daily variations in internal anatomy. Similarly, MRI performed throughout radiation delivery allows for real-time tracking and gating without use of surrogate targets or invasively placed fiducial markers. Given these advantages, a number of systems have been developed to integrate MR technology with the radiation treatment platform in order to deliver MR-guided RT (MRgRT).
Two such systems have matured to full clinical implementation, including the ViewRay MRIdian system with a 0.35 T MRI and the Elekta Unity system with a 1.5 T MRI [5, 6]. There are several tradeoffs present between platforms using a low vs high magnetic field strength. Thorwarth and Low [7] discuss these tradeoffs in great detail, but they can be summarized as a compromise between image quality, distortion and artifacts, and accuracy of dose delivery. In general, higher magnetic field strength yields superior image quality due to higher signal-to-noise ratio; however, with post-processing, a 0.35 T image can be optimized for target and OAR delineation. In contrast, a lower magnetic field strength results in reduced anatomic distortion and artifacts from implanted foreign bodies, but again post-processing and image acquisition adjustments can mitigate some of these effects on a 1.5 T system. Finally, the magnetic field itself exerts a directional Lorentz force on the secondary electrons generated by the x-rays used during treatment, introducing a field size-dependent distortion of the delivered radiation dose. While this dose distortion effect is more pronounced with a 1.5 T system, advanced Monte Carlo–based dose calculation software used by both platforms can adjust for these Lorentz forces on an individual patient treatment plan level [7]. The ViewRay MRIdian system has been specifically engineered to physically shield the magnet and linear accelerator elements from each other.
MRgRT holds particular promise in the treatment of colorectal cancer (CRC). In cases of locally advanced rectal cancer (LARC), the primary target resides low in the pelvis and soft tissue delineation between tumor and normal rectum can be difficult on CT. Additionally, the most common site of metastatic spread with CRC is to the liver, another treatment site with poor contrast between tumor and normal tissue on CT [8].
Technical Advantages of MRgRT
Integration of MRI with the radiation therapy system offers a host of technical advantages when compared with conventional CT-guided RT (CTgRT). MR image acquisition is performed without any ionizing radiation, allowing for repeated and real-time imaging without delivering excess radiation dose to the patient. Interfraction variation due to daily changes in bladder and rectal filling can result in anatomic deviations of up to 7 mm [9,10,11]. In addition to this random interfraction variability, the tumor itself may regress during the course of RT [12, 13]. MRgRT can address both sources of interfraction variability through imaging and plan adaptation prior to daily treatment. An MRI can be obtained, and relevant OAR and target anatomy segmentation from the initial plan can be adjusted to match the current imaging. Doing so allows for accurate delineation of where the true target and OARs are right before treatment delivery. The treatment plan can then be re-optimized in real time to account for these changes and a more accurate plan can be delivered. A study of such an “online adaptive” approach found that non-adaptive treatment of liver tumors would have resulted in underdosing the target in 47% of treatments and overdosing of adjacent OARs in 21% of treatments [14].
MRgRT can also be used to good effect when operated throughout radiation delivery. Intrafraction variability occurs when the treatment target moves during RT delivery due to normal respiration, bowel peristalsis, or other changes in regional anatomy. This motion is often managed with surrogate trackers such as breath-hold techniques that track surface anatomy or implanted fiducial markers. Real-time MRI allows for accurate, non-invasive target tracking throughout the radiation treatment. If the target moves out of the planned radiation field due to internal or external patient motion, the beam can be turned off until the target returns to the appropriate position. This real-time gating approach has been shown to mitigate the effects of intrafraction motion in a variety of abdominal and pelvic malignancies [15,16,17]. Providing direct visual feedback to patients undergoing such gated treatments has demonstrated quantifiable improvements in tumor excursion outside the gating boundary as well as beam-on time throughout treatment [18]. This approach may also allow for the patient to be involved in their care directly with potential psychological benefits.
MRgRT for Localized Colorectal Cancer
MRI is the imaging modality of choice for local staging of rectal cancer due to superior soft tissue contrast and characterization of tumor invasion of and relation to key adjacent anatomic structures [19]. MRI staging has increasingly begun to supplant CT- and endoscopic ultrasound (EUS)–based staging, as MRI can accurately identify T- and N-stage, extramural vascular invasion, and predict for positive circumferential resection margin, which is associated with an increased risk for tumor recurrence [20, 21]. As a result, there has been great interest in integrating MRI with treatment planning, image guidance, and adaptive planning techniques.
An in silico analysis of 10 patients with LARC compared IMRT treatment plans both with and without the magnetic field activated on a commercially available 0.35 T MRgRT device using a tri-Co-60 delivery system [22]. The simulated treatment plans were also compared to volumetric modulated arc therapy (VMAT) and IMRT plans delivered with standard CTgRT linear accelerators (linacs). There were no differences in the tri-Co-60 plans based on presence of the magnetic field, and the tri-Co-60 plans were able to meet all standardly accepted dose constraints. As a result, they were able to demonstrate a proof of concept for delivering fully fractionated neoadjuvant RT on a tri-Co-60 MRI platform [22].
A follow-up retrospective study by the same group was the first reported clinical experience using the tri-Co-60 MRgRT platform for treatment of LARC [23••]. In this study, 22 patients were treated to a dose of 45 Gy in 25 fractions to the mesorectum and elective lymph node regions with a simultaneous integrated boost (SIB) of 55 Gy in 25 fractions to the primary tumor [23••]. A prior meta-analysis had identified that similar dose escalation for LARC was associated with higher rates of local control and pathologic complete response (pCR) [24]. The 0.35 T tri-Co-60 MRgRT platform was used for both image acquisition for treatment planning and for gating during treatment delivery [23••]. The latter was achieved via real-time cine-MRI images using a 5% region of interest (ROI) at a 3-mm expansion boundary around the clinical treatment volume (CTV) based on the primary tumor. Three patients experienced a clinical complete response (cCR) and did not proceed with planned surgery. All three patients with cCR who did not undergo subsequent surgery were alive without evidence of disease at the time the study was reported. Three additional patients were found to have a pCR after surgery, for a total of 27% of patients with either cCR or pCR on final analysis [23••]. This rate is comparable to the 24% pCR rate in the contemporaneously reported randomized INTERACT study for dose escalation with IMRT [25].
Another in silico analysis compared four different boost strategies for LARC on a commercially available 1.5 T MRgRT device using a 7 MV linac delivery system [26]. Five patients were treated with standard of care neoadjuvant chemoradiotherapy to 50.4 Gy in 28 fractions. Boost plans of 15 Gy in 5 fractions were generated retrospectively either as an up-front concomitant boost delivered in the first week of therapy or as an adaptive boost delivered once weekly through 5 weeks of therapy, with either standard (7–10 mm) or reduced (3 mm) margins for both approaches. The authors identified a substantial reduction in the boost planning target volume (PTV) with the weekly adaptive boost at both margin levels, and that 3 of 5 patients could safely have been treated with the adaptive boost and reduced margins strategy compared to none with the up-front boost strategy regardless of margins used [26].
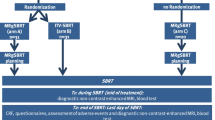
The above studies demonstrate the feasibility and efficacy of dose-escalated therapy in LARC using MRgRT. One additional area of active research in the treatment of LARC concerns the rate of pathologic complete response and whether a subset of patients can be managed without surgical resection. Thought-provoking observational data supports the potential for nonoperative management (NOM) in a well-selected population of patients [27,28,29]. In parallel, two large randomized trials have demonstrated a doubling of pCR rates when patients are treated with a total neoadjuvant therapy (TNT) approach as compared to the conventional treatment for LARC involving adjuvant chemotherapy after total mesorectal excision (TME) [30••, 31]. As a result, there is growing interest both in maximizing the rate of cCR and pCR while also aiming to identify the patients most likely to benefit from a nonoperative approach.
Traditional attempts at stratifying patient response to treatment have typically involved anatomic assessment either through direct examination (i.e., endoscopy) or anatomy-based radiographic assessment, such as MRI with T1- or T2-weighted imaging. Functional imaging and advanced radiomics open the possibility of extracting additional treatment response information from patient scans to identify treatment response. Diffusion-weighted imaging (DWI) can use the differential diffusion of water to identify areas of free vs restricted diffusion. The resultant apparent diffusion coefficient (ADC) maps can identify areas of cell membrane loss associated with RT-related treatment response via necrosis or apoptosis [32]. Mean tumor ADC obtained on diagnostic 1.5 T MRI has been demonstrated to correlate with pathologic tumor downstaging, and this result has been replicated on imaging obtained on a 0.35 T MRgRT platform [33, 34]. A follow-up study demonstrated the superiority of a deep learning–based radiomic approach to analysis of ADC maps in rectal cancer patients treated on the same 0.35 T MRgRT platform [35]. These early studies raise the intriguing possibility of utilizing imaging biomarkers to identify treatment response to RT in near real-time while adapting treatments either to reduce dose to areas that have had a favorable biologic response or to boost dose to areas of relative radioresistance.
The treatment approach to LARC has increasingly shifted toward use of short-course RT and TNT with growing interest in boost to residual primary to improve rates of pCR and potentially allow for nonoperative management [30••, 36]. MRgRT is uniquely positioned to maximize the benefits of these trends, as the system allows for accurate daily positioning and adaptation for higher doses of radiation delivered in fewer treatments and is a natural platform for real-time assessment of tumor response through imaging biomarkers.
MRgRT for Oligometastatic Colorectal Cancer
A consensus definition of the oligometastatic state usually centers on the presence of a limited number of metastatic sites, often cited as being 1–5, all of which can be treated safely with metastasis-directed therapy with curative intent [37]. Approximately 20–25% of patients with a new diagnosis of CRC have synchronous metastatic CRC (mCRC), and among those patients, the most common site of metastasis is the liver [38]. Although hepatectomy for liver-only mCRC has been demonstrated to prolong survival and even cure a subset of patients, only 10–20% of patients with mCRC are deemed to have surgically resectable disease [39].
Given the potential for life-prolonging or curative treatment of mCRC patients combined with the unmet need of 80–90% of patients not having resectable metastases, there is substantial interest in identifying alternative treatment modalities capable of providing the same survival benefits. One randomized study of radiofrequency ablation (RFA) demonstrated a fourfold increase in the rate of 8-year overall survival in patients receiving aggressive local treatment in addition to systemic therapy [40]. Not all patients are good candidates for RFA, however, as the presence of adjacent large blood vessels or lesions > 3 cm can impact safety, efficacy, and local control [41]. In contrast, a series of patients treated for cholangiocarcinoma on a 0.35 T MRgRT system demonstrated that excellent local control and low toxicity (grade 3 events < 10%) can be achieved with SBRT in the hilum of the liver where adjacent vessels and luminal OARs traditionally limit other treatment approaches [42]. There is additional evidence to support SBRT as an alternative modality for treatment of liver metastases, and that achieving high biologically effective dose (BED) improves local control [43].
Treatment of liver metastases with the SBRT technique is often limited by target visualization—governed by poor soft tissue contrast between the lesion and normal liver on CT—and organ motion due to respiration. The MRgRT platform neatly overcomes both limitations with MR-based image guidance offering superior target visualization and real-time target gating through the breathing cycle. Examples of such superior visualization can be seen in Fig. 1. In addition, the MRgRT platform offers the potential for online adaptive therapy that reoptimizes the treatment plan daily to compensate for interfraction changes in the position of adjacent OARs. Henke et al. [44] demonstrated the first clinical use of this stereotactic MR-guided online adaptive radiotherapy (SMART) approach for abdominal malignancies. Twenty patients were treated, 10 of whom were treated for lesions in the liver. Among the 97 fractions delivered, they identified that OAR constraint violations would have occurred in 63% of fractions had they not adapted therapy. Ultimately, they reported zero grade 3 or higher toxicities among the cohort [44]. Their experience was expanded in a multi-institutional review of liver-specific SMART in which eight of 26 patients were treated for liver metastases secondary to colorectal cancer [45•]. Only two patients experienced worsening of Child–Pugh score, and neither had mCRC [45•].
Visualization advantages of MR-guided (bottom row) vs CT-based (top row) radiotherapy planning and delivery. MR provides superior soft tissue contrast (left), better daily visualization of small targets resulting in decrease planning margins (center), and novel contrast agents that help localize tumors difficult to see even on non-enhanced MR sequences (right)
Our institutional experience with MRgRT for liver metastases aligns with the findings above. In one recent study, 20 patients were treated for liver metastases, 7 of whom had mCRC [46]. The majority of patients were able to be treated with an ablative biologically effective dose (BED) ≥ 100 Gy10, and the 1- and 2-year estimates of local control were 95% and 80%, respectively. There were no acute grade ≥ 3 toxicities and only one patient experienced late grade ≥ 3 toxicity [46]. Gani et al. [47] demonstrated similar feasibility of the approach on a 1.5 T platform, with 10 patients treated for liver metastases with high rates of patient acceptance and no patient-initiated treatment interruptions. Prior studies have demonstrated similar safety and efficacy with the SBRT technique for liver metastases using CT-based radiotherapy [48,49,50,51]. To achieve these results, most of these trials relied on motion management techniques that incorporated the motion of the tumor through the breathing cycle [48,49,50]. Although this motion could be minimized through breath control or abdominal compression devices, planning margins were still in the range of 7–15 mm added to the target to account for daily variability [48,49,50]. One trial was able to reduce the added planning margin to 5–7 mm by implanting fiducial markers within the target to provide real-time target tracking [51]. The use of MRgRT can allow for such real-time tracking and smaller, 5 mm added planning margins, without the use of invasive fiducial markers which have small but measurable risks of infection or bleeding. Intuitively, a smaller treatment volume with the same or higher treatment dose would allow for improved safety and efficacy outcomes. The SMART approach to treatment of abdominal metastatic disease is flexible and generalizable, and there is even a case report of a radiographic complete response in the treatment of a chemoresistant peritoneal carcinomatosis nodule with the MRgRT platform [52].
Treatment Considerations
MRgRT offers substantial benefits to the current standard radiotherapy approach to treatment of LARC and mCRC. However, adoption of a novel treatment delivery system requires great care to ensure optimal treatment delivery to realize the full potential of the platform. All elements of the treatment workflow, including but not limited to patient selection, treatment planning, staff training, and MR-specific precautions, must be considered.
Online adaptive MRgRT is the specific use case with the most intense resource utilization given the unique integration of real-time adaptive planning. Careful patient selection is paramount, as treatment times can be prolonged as the adaptive re-planning process takes place while the patient is on the table in a tightly enclosed space. Our institutional experience has demonstrated that visual inspection alone is not reliable enough to determine which plans would benefit from online adaptive re-planning [53]. One study investigating SBRT for liver metastases showed that the majority of the benefit to online adaptive re-planning is realized when the target is within 2 cm of a critical OAR [54]. Furthermore, it is likely that at least 10% of SMART fractions could have improved target dose coverage with more extensive offline re-planning [55]. Identifying such disease-site-specific heuristics for determining when to adapt high-dose ablative radiation may allow for a balanced approach between delivering safe treatment with optimal target dose coverage while minimizing treatment duration in patients who would experience little benefit from the more resource-intensive approach.
When treating liver metastases in the setting of mCRC, several techniques can be employed to improve target accuracy and reduce dose to OARs and treatment toxicity. Our institutional experience has demonstrated the importance of contouring individual loops of bowel adjacent to the target and keeping the V35 Gy to less than 0.35 cm3 [46]. Recommended OAR dose constraints and target dose fractionation schemes are available in Table 1, with target doses offering a BED ≥ 100 Gy10 in alignment with studies that have shown increased local control of liver lesions above that threshold [43]. Importantly, multiple liver lesions can be safely targeted with SBRT on the MRgRT platform, and the availability of real-time cine gating with or without gadoexatate disodium (Eovist®) allows for avoidance of invasive fiducial marker placement which results in an estimated personnel and materials cost savings of over $1000 per patient [56].
Conclusions
MRgRT offers significant advantages when compared to conventional CT-based radiotherapy for LARC and mCRC. Superior soft tissue contrast and real-time target tracking with gated treatment delivery allow for more accurate and precise delivery of high doses of radiation. Adoption of this technology requires careful examination of the entire treatment workflow, including patient selection, treatment planning, and staff training. Access to on-board functional imaging will allow for imaging biomarker-driven therapy, determining both regions in need of boost dose targeting and/or allowing for assessment of treatment response and potential treatment de-escalation.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Thompson MK, Poortmans P, Chalmers AJ, Faivre-Finn C, Hall E, Huddart RA, et al. Practice-changing radiation therapy trials for the treatment of cancer: where are we 150 years after the birth of Marie Curie? Br J Cancer. 2018;119:389–407. https://doi.org/10.1038/s41416-018-0201-z.
International Atomic Energy Agency. Planning national radiotherapy services: A practical tool, human health series No. 14, IAEA, Vienna. 2011
Mitchell DG, Snyder B, Coakley F, Reinhold C, Thomas G, Amendola M, et al. Early invasive cervical cancer: tumor delineation by magnetic resonance imaging, computed tomography, and clinical examination, verified by pathologic results, in the ACRIN 6651/GOG 183 Intergroup Study. J Clin Oncol. 2006;24:5687–94. https://doi.org/10.1200/JCO.2006.07.4799.
Chang JH, Lim Joon D, Nguyen BT, Hiew C-Y, Esler S, Angus D, et al. MRI scans significantly change target coverage decisions in radical radiotherapy for prostate cancer. J Med Imaging Radiat Oncol. 2014;58:237–43. https://doi.org/10.1111/1754-9485.12107.
Klüter Se. Technical design and concept of a 0.35 T MR-Linac. Clin Transl Radiat Oncol. 2019;18:98–101. https://doi.org/10.1016/j.ctro.2019.04.007.
Winkel D, Bol GH, Kroon PS, van Asselen B, Hackett SS, Werensteijn-Honingh AM, et al. Adaptive radiotherapy: the Elekta Unity MR-linac concept. Clin Transl Radiat Oncol. 2019;18:54–9. https://doi.org/10.1016/j.ctro.2019.04.001.
Thorwarth D, Low DA. Technical challenges of real-time adaptive MR-guided radiotherapy. Front Oncol. 2021;11:634507. https://doi.org/10.3389/fonc.2021.634507.
Kow AWC. Hepatic metastasis from colorectal cancer. J Gastrointest Oncol. 2019;10:1274–98. https://doi.org/10.21037/jgo.2019.08.06.
Ippolito E, Mertens I, Haustermans K, Gambacorta MA, Pasini D, Valentini V. IGRT in rectal cancer. Acta Oncol. 2008;47:1317–24. https://doi.org/10.1080/02841860802256459.
Nijkamp J, de Jong R, Sonke J-J, Remeijer P, van Vliet C, Marijnen C. Target volume shape variation during hypo-fractionated preoperative irradiation of rectal cancer patients. Radiother Oncol. 2009;92:202–9. https://doi.org/10.1016/j.radonc.2009.04.022.
Brierley JD, Dawson LA, Sampson E, Bayley A, Scott S, Moseley JL, et al. Rectal motion in patients receiving preoperative radiotherapy for carcinoma of the rectum. Int J Radiat Oncol Biol Phys. 2011;80:97–102. https://doi.org/10.1016/j.ijrobp.2010.01.042.
Roels S, Slagmolen P, Nuyts J, Lee JA, Loeckx D, Maes F, et al. Biological image-guided radiotherapy in rectal cancer: challenges and pitfalls. Int J Radiat Oncol Biol Phys. 2009;75:782–90. https://doi.org/10.1016/j.ijrobp.2008.11.031.
Van den Begin R, Kleijnen J-P, Engels B, Philippens M, van Asselen B, Raaymakers B, et al. Tumor volume regression during preoperative chemoradiotherapy for rectal cancer: a prospective observational study with weekly MRI. Acta Oncol. 2018;57:723–7. https://doi.org/10.1080/0284186X.2017.1400689.
Rogowski P, von Bestenbostel R, Walter F, Straub K, Nierer L, Kurz C, et al. Feasibility and early clinical experience of online adaptive MR-guided radiotherapy of liver tumors. Cancers. 2021;13:1523. https://doi.org/10.3390/cancers13071523.
Hegde JV, Cao M, Yu VY, Kishan AU, Shaverdian N, Lamb J, et al. Magnetic resonance imaging guidance mitigates the effects of intrafraction prostate motion during stereotactic body radiotherapy for prostate cancer. Cureus. 2018;10:e2442. https://doi.org/10.7759/cureus.2442.
Tetar SU, Bruynzeel AME, Lagerwaard FJ, Slotman BJ, Bohoudi O, Palacios MA. Clinical implementation of magnetic resonance imaging guided adaptive radiotherapy for localized prostate cancer. Phys Imaging Radiat Oncol. 2019;9:69–76. https://doi.org/10.1016/j.phro.2019.02.002.
Prins FM, Stemkens B, Kerkmeijer LGW, Barendrecht MM, de Boer HJ, Vonken E-JPA, et al. Intrafraction motion management of renal cell carcinoma with magnetic resonance imaging-guided stereotactic body radiation therapy. Pract Radiat Oncol. 2019;9:e55-61. https://doi.org/10.1016/j.prro.2018.09.002.
Kim T, Lewis BC, Price A, Mazur T, Gach HM, Park JC, et al. Direct tumor visual feedback during free breathing in 0.35T MRgRT. J Appl Clin Med Phys. 2020;21:241–7. https://doi.org/10.1002/acm2.13016.
Horvat N, Rocha CCT, Oliveira BC, Petkovska I, Gollub MJ. MRI of rectal cancer tumor staging, imaging techniques, and management. Radiographics. 2019;39:367–87. https://doi.org/10.1148/rg.2019180114.
Balyasnikova S, Brown G. Optimal imaging strategies for rectal cancer staging and ongoing management. Curr Treat Options Oncol. 2016;17:32. https://doi.org/10.1007/s11864-016-0403-7.
Taylor FGM, Quirke P, Heald RJ, Moran B, Blomqvist L, Swift I, et al. One millimetre is the safe cut-off for magnetic resonance imaging prediction of surgical margin status in rectal cancer. Br J Surg. 2011;98:872–9. https://doi.org/10.1002/bjs.7458.
Boldrini L, Placidi E, Dinapoli N, Azario L, Cellini F, Massaccesi M, et al. Hybrid Tri-Co-60 MRI radiotherapy for locally advanced rectal cancer: an in silico evaluation. Tech Innov Patient Support Radiat Oncol. 2018;6:5–10. https://doi.org/10.1016/j.tipsro.2018.02.002.
Chiloiro G, Boldrini L, Meldolesi E, Re A, Cellini F, Cusumano D, et al. MR-guided radiotherapy in rectal cancer: first clinical experience of an innovative technology. Clin Transl Radiat Oncol. 2019;18:80–6. https://doi.org/10.1016/j.ctro.2019.04.006. The first clinical report using MRgRT for the treatment of rectal cancer.
Burbach JPM, den Harder AM, Intven M, van Vulpen M, Verkooijen HM, Reerink O. Impact of radiotherapy boost on pathological complete response in patients with locally advanced rectal cancer: a systematic review and meta-analysis. Radiother Oncol. 2014;113:1–9. https://doi.org/10.1016/j.radonc.2014.08.035.
Valentini V, Gambacorta MA, Cellini F, Aristei C, Coco C, Barbaro B, et al. The INTERACT trial: long-term results of a randomised trial on preoperative capecitabine-based radiochemotherapy intensified by concomitant boost or oxaliplatin, for cT2 (distal)-cT3 rectal cancer. Radiother Oncol. 2019;134:110–8. https://doi.org/10.1016/j.radonc.2018.11.023.
Bonomo P, Lo Russo M, Nachbar M, Boeke S, Gatidis S, Zips D, et al. 1.5 T MR-linac planning study to compare two different strategies of rectal boost irradiation. Clin Transl Radiat Oncol. 2021;26:86–91. https://doi.org/10.1016/j.ctro.2020.11.016.
Habr-Gama A, São Julião GP, Vailati BB, Sabbaga J, Aguilar PB, Fernandez LM, et al. Organ preservation in cT2N0 rectal cancer after neoadjuvant chemoradiation therapy: the impact of radiation therapy dose-escalation and consolidation chemotherapy. Ann Surg. 2019;269:102–7. https://doi.org/10.1097/SLA.0000000000002447.
Dossa F, Chesney TR, Acuna SA, Baxter NN. A watch-and-wait approach for locally advanced rectal cancer after a clinical complete response following neoadjuvant chemoradiation: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2017;2:501–13. https://doi.org/10.1016/S2468-1253(17)30074-2.
Fernandez LM, São Julião GP, Figueiredo NL, Beets GL, van der Valk MJM, Bahadoer RR, et al. Conditional recurrence-free survival of clinical complete responders managed by watch and wait after neoadjuvant chemoradiotherapy for rectal cancer in the International Watch & Wait Database: a retrospective, international, multicentre registry study. Lancet Oncol. 2021;22:43–50. https://doi.org/10.1016/S1470-2045(20)30557-X.
Bahadoer RR, Dijkstra EA, van Etten B, Marijnen CAM, Putter H, Kranenbarg E-MK, et al. Short-course radiotherapy followed by chemotherapy before total mesorectal excision (TME) versus preoperative chemoradiotherapy, TME, and optional adjuvant chemotherapy in locally advanced rectal cancer (RAPIDO) a randomised, open-label, phase 3 trial. Lancet Oncol. 2021;22:29–42. https://doi.org/10.1016/S1470-2045(20)30555-6. Landmark RCT demonstrating superior outcomes with total neoadjuvant therapy compared to standard of care treatment with adjuvant chemotherapy.
Conroy T, Bosset J-F, Etienne P-L, Rio E, François É, Mesgouez-Nebout N, et al. Neoadjuvant chemotherapy with FOLFIRINOX and preoperative chemoradiotherapy for patients with locally advanced rectal cancer (UNICANCER-PRODIGE 23): a multicentre, randomised, open-label, phase 3 trial. Lancet Oncol. 2021;22:702–15. https://doi.org/10.1016/S1470-2045(21)00079-6.
Hamstra DA, Rehemtulla A, Ross BD. Diffusion magnetic resonance imaging: a biomarker for treatment response in oncology. J Clin Oncol. 2007;25:4104–9. https://doi.org/10.1200/JCO.2007.11.9610.
Sun Y-S, Zhang X-P, Tang L, Ji J-F, Gu J, Cai Y, et al. Locally advanced rectal carcinoma treated with preoperative chemotherapy and radiation therapy: preliminary analysis of diffusion-weighted MR imaging for early detection of tumor histopathologic downstaging. Radiology. 2010;254:170–8. https://doi.org/10.1148/radiol.2541082230.
Shaverdian N, Yang Y, Hu P, Hart S, Sheng K, Lamb J, et al. Feasibility evaluation of diffusion-weighted imaging using an integrated MRI-radiotherapy system for response assessment to neoadjuvant therapy in rectal cancer. Br J Radiol. 2017;90:20160739. https://doi.org/10.1259/bjr.20160739.
Fu J, Zhong X, Li N, Van Dams R, Lewis J, Sung K, et al. Deep learning-based radiomic features for improving neoadjuvant chemoradiation response prediction in locally advanced rectal cancer. Phys Med Biol. 2020;65:075001. https://doi.org/10.1088/1361-6560/ab7970.
Kim H, Pedersen K, Olsen JR, Mutch MG, Chin R-I, Glasgow SC, et al. Nonoperative rectal cancer management with short-course radiation followed by chemotherapy: a nonrandomized control trial. Clin Colorectal Cancer. 2021. https://doi.org/10.1016/j.clcc.2021.03.003.
Lievens Y, Guckenberger M, Gomez D, Hoyer M, Iyengar P, Kindts I, et al. Defining oligometastatic disease from a radiation oncology perspective: an ESTRO-ASTRO consensus document. Radiother Oncol. 2020;148:157–66. https://doi.org/10.1016/j.radonc.2020.04.003.
van der Geest LGM, Lam-Boer J, Koopman M, Verhoef C, Elferink MAG, de Wilt JHW. Nationwide trends in incidence, treatment and survival of colorectal cancer patients with synchronous metastases. Clin Exp Metastasis. 2015;32:457–65. https://doi.org/10.1007/s10585-015-9719-0.
Kanas GP, Taylor A, Primrose JN, Langeberg WJ, Kelsh MA, Mowat FS, et al. Survival after liver resection in metastatic colorectal cancer: review and meta-analysis of prognostic factors. Clin Epidemiol. 2012;4:283–301. https://doi.org/10.2147/CLEP.S34285.
Ruers T, Van Coevorden F, Punt CJA, Pierie J-PEN, Borel-Rinkes I, Ledermann JA, et al. Local treatment of unresectable colorectal liver metastases results of a randomized phase II trial. J Natl Cancer Inst. 2017;109:djx015. https://doi.org/10.1093/jnci/djx015.
Wong SL, Mangu PB, Choti MA, Crocenzi TS, Dodd GD, Dorfman GS, et al. American Society of Clinical Oncology 2009 clinical evidence review on radiofrequency ablation of hepatic metastases from colorectal cancer. J Clin Oncol. 2010;28:493–508. https://doi.org/10.1200/JCO.2009.23.4450.
Luterstein E, Cao M, Lamb JM, Raldow A, Low D, Steinberg ML, et al. Clinical outcomes using magnetic resonance-guided stereotactic body radiation therapy in patients with locally advanced cholangiocarcinoma. Adv Radiat Oncol. 2020;5:189–95. https://doi.org/10.1016/j.adro.2019.09.008.
Ohri N, Tomé WA, Méndez Romero A, Miften M, Ten Haken RK, Dawson LA, et al. Local control after stereotactic body radiation therapy for liver tumors. Int J Radiat Oncol. 2021;110:188–95. https://doi.org/10.1016/j.ijrobp.2017.12.288.
Henke L, Kashani R, Robinson C, Curcuru A, DeWees T, Bradley J, et al. Phase I trial of stereotactic MR-guided online adaptive radiation therapy (SMART) for the treatment of oligometastatic or unresectable primary malignancies of the abdomen. Radiother Oncol. 2018;126:519–26. https://doi.org/10.1016/j.radonc.2017.11.032.
Rosenberg SA, Henke LE, Shaverdian N, Mittauer K, Wojcieszynski AP, Hullett CR, et al. A multi-institutional experience of MR-guided liver stereotactic body radiation therapy. Adv Radiat Oncol. 2019;4:142–9. https://doi.org/10.1016/j.adro.2018.08.005. An important early multi-institutional analysis of MRgRT for liver SBRT.
van Dams R, Wu TC, Kishan AU, Raldow AC, Chu F-I, Hernandez J, et al. Ablative radiotherapy for liver tumors using stereotactic MRI-guidance: a prospective phase I trial. Radiother Oncol. 2021:Online ahead of print. https://doi.org/10.1016/j.radonc.2021.06.005.
Gani C, Boeke S, McNair H, Ehlers J, Nachbar M, Mönnich D, et al. Marker-less online MR-guided stereotactic body radiotherapy of liver metastases at a 1.5 T MR-Linac – feasibility, workflow data and patient acceptance. Clin Transl Radiat Oncol. 2021;26:55–61. https://doi.org/10.1016/j.ctro.2020.11.014.
Rusthoven KE, Kavanagh BD, Cardenes H, Stieber VW, Burri SH, Feigenberg SJ, et al. Multi-institutional phase I/II trial of stereotactic body radiation therapy for liver metastases. J Clin Oncol. 2009;27:1572–8. https://doi.org/10.1200/JCO.2008.19.6329.
Scorsetti M, Comito T, Tozzi A, Navarria P, Fogliata A, Clerici E, et al. Final results of a phase II trial for stereotactic body radiation therapy for patients with inoperable liver metastases from colorectal cancer. J Cancer Res Clin Oncol. 2015;141:543–53. https://doi.org/10.1007/s00432-014-1833-x.
Goodman BD, Mannina EM, Althouse SK, Maluccio MA, Cárdenes HR. Long-term safety and efficacy of stereotactic body radiation therapy for hepatic oligometastases. Pract Radiat Oncol. 2016;6:86–95. https://doi.org/10.1016/j.prro.2015.10.011.
Méndez Romero A, Keskin-Cambay F, van Os RM, Nuyttens JJ, Heijmen BJM, IJzermans JNM, et al. Institutional experience in the treatment of colorectal liver metastases with stereotactic body radiation therapy. Rep Pract Oncol Radiother. 2017;22:126–31. https://doi.org/10.1016/j.rpor.2016.10.003.
Boldrini L, Romano A, Placidi L, Mattiucci GC, Chiloiro G, Cusumano D, et al. Case report: first in human online adaptive MR guided SBRT of peritoneal carcinomatosis nodules: a new therapeutic approach for the oligo-metastatic patient. Front Oncol. 2020;10:601739. https://doi.org/10.3389/fonc.2020.601739.
Tyran M, Jiang N, Cao M, Raldow A, Lamb JM, Low D, et al. Retrospective evaluation of decision-making for pancreatic stereotactic MR-guided adaptive radiotherapy. Radiother Oncol. 2018;129:319–25. https://doi.org/10.1016/j.radonc.2018.08.009.
Mayinger M, Ludwig R, Christ SM, Dal Bello R, Ryu A, Weitkamp N, et al. Benefit of replanning in MR-guided online adaptive radiation therapy in the treatment of liver metastasis. Radiat Oncol. 2021;16:84. https://doi.org/10.1186/s13014-021-01813-6.
Chow PE, Chu F-I, Agazaryan N, Cao M, Tyran M, Yang Y, et al. Dosimetric quality of online adapted pancreatic cancer treatment plans on an MRI-guided radiation therapy system. Adv Radiat Oncol. 2021;6:100682. https://doi.org/10.1016/j.adro.2021.100682.
Parikh NR, Lee PP, Raman SS, Cao M, Lamb J, Tyran M, et al. Time-driven activity-based costing comparison of CT-guided versus MR-guided SBRT. JCO Oncol Pract. 2020;16:e1378–85. https://doi.org/10.1200/JOP.19.00605.
Acknowledgements
The editors would like to thank Dr. Shahid Umar for taking the time to review this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Ritchell van Dams declares no potential conflicts of interest. Ann C. Raldow is a consultant for ViewRay and a local PI for the SMART Pancreas Trial. Percy Lee is a Medical advisory board member for ViewRay and a National Co-PI for the SMART Pancreas Trial.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Radiation Therapy and Radiation Therapy Innovations in Colorectal Cancer
Rights and permissions
About this article
Cite this article
van Dams, R., Raldow, A.C. & Lee, P. Role of MR-guided Radiotherapy (MRgRT) in Colorectal Cancer. Curr Colorectal Cancer Rep 17, 69–76 (2021). https://doi.org/10.1007/s11888-021-00467-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11888-021-00467-6