Abstract
Purpose of Review
Examine the various technical considerations for pelvic colorectal reconstruction with respective functional and anastomotic healing outcomes. Additionally, several adjuncts to reduce anastomotic complications are individually explored to understand their relative impact on anastomotic healing.
Recent Findings
The benefit of a colorectal reservoir reconstruction instead of a straight anastomosis, in respect to leak and functional outcomes, is marginal, if any. Recent randomized evidence has shown no difference in morbidity, mortality, survival, leakage, or functional outcomes. Unfortunately, anastomotic leakage still occurs in the ideally constructed and managed pelvic anastomosis; however, modifiable variables appear to reduce the risk.
Summary
Pelvic colorectal anastomosis should be based on the surgeon’s technical ability and comfort level, since the evidence suggests that all techniques are comparable. There may be a slight advantage to colonic J-pouch anastomosis, although this has not been consistently shown. Future studies on the etiology of low anterior resection syndrome may provide insight on optimal reconstruction techniques.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Following proctectomy, a permanent stoma or a colorectal anastomosis may be constructed. Selection of the optimal type of colorectal anastomosis is not straightforward, however, since restoration of gastrointestinal continuity must take into consideration functional consequences with substantial quality-of-life (QOL) effects. Regardless of the surgical technique, dehiscence and subsequent leakage remain the most important immediate considerations. Since leakage may still occur when an anastomosis is technically correct, the surgeon must fully recognize modifiable risk factors to both prevent and diminish the incidence. Some patient-specific risk factors influencing leakage, such as gender, obesity, tobacco use, or nutrition status, are often not possible or difficult to modify when recommending an operation [1]. The unique extraperitoneal anatomic position of colorectal anastomoses, with absence of a serosal layer, and the characteristic need for colonic lengthening to construct tension-free apposition influence preoperative patient counseling, intraoperative decision-making, and postoperative management as well as long-term functional considerations. Despite these challenges, surgeon judgment and ancillary practices can help proactively reduce leak rates and/or early identification when they occur. This paper reviews various techniques used for colorectal anastomotic reconstruction and discusses modifiable perioperative adjuncts to potentially improve anastomotic healing outcomes.
Anastomotic Reconstruction Techniques
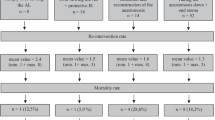
A variety of configurations are possible when creating a pelvic colorectal anastomosis. When contemplating the type of anastomosis for a patient, patient’s body habitus, anastomotic leak (AL) rate, and estimation of a patient’s ability to tolerate a leak, as well as functional outcomes, must be considered. Patients with a very narrow pelvis, bulky colon and mesentery, or inadequate colonic length may restrict the options to a straight end-to-end colorectal anastomosis. In addition, a stapled versus handsewn anastomosis is often most dependent on the distance from the anal verge (Fig. 1).
Straight Colorectal Anastomosis
A straight colorectal anastomosis (SCA) can be constructed either with sutures or staplers in an end-to-end fashion. A stapled SCA is typically performed with a circular intraluminal stapler introduced transanaly into a rectal stump that has been transversely stapled with a linear cutting stapler. An anvil is secured into the proximal end of the colon with a purse-string suture. The anvil and pin are then mated and the stapler fired to create a double-stapled SCA. Alternatively, a double purse-string may be performed if the stapler is introduced transanaly through a rectal stump that has been transected but not stapled closed. A purse-string suture is placed around the distal rectal stump and then tied down around the pin. The anvil is secured in the proximal conduit, mated to the pin, and then fired. A double purse-string approach avoids crossing staple lines that occur with the double-stapled technique, and may decrease the risk of AL, although high level evidence for this is not available.
A handsewn anastomosis may be performed to create a SCA. This is accomplished either transabdominally or transanally; however, in the low pelvis, adequate exposure for suturing transabdominally is difficult. Absorbable sutures are laid into the proximal and distal cut ends of the bowel, then tied down sequentially. This technique is generally reserved for circumstances when an anastomosis will be very distal, typically the anal canal; the tissue thickness cannot be accommodated by a stapler, or the stapler has malfunctioned. The colonic conduit is pulled through the anus transanally along with its mesentery. A self-expanding wound protector placed into the anus can facilitate the delivery of the conduit atraumatically.
Multiple studies have compared stapled to handsewn colorectal anastomoses, although the quality of these data remains limited. A Cochrane review including 1233 patients from nine trials examined stapled versus handsewn methods for colorectal anastomosis [2]. The authors found no superiority for any endpoint (mortality, AL, stricture, hemorrhage, reoperation, wound infection, anastomosis duration, or hospital stay) of stapled compared to handsewn colorectal anastomosis, regardless of the level of anastomosis from the anal verge. A similar systemic review from Slieker et al. reported no level 1a evidence of superiority of stapled over handsewn colorectal anastomoses. [3]
While a stapled SCA is the most commonly performed configuration establishing colorectal continuity, functional sequelae regarding stool evacuation or incontinence can be significant. The constellation of fecal urgency, frequency and clustering of bowel movements with incomplete stool evacuation, and incontinence to flatus and liquid stool, is collectively referred to as the low anterior resection syndrome (LARS), occurring in up to 80% of patients [4]. Although the precise mechanisms causing impairment in bowel function remain poorly understood, the loss of reservoir function following proctectomy is considered a major contributing cause. Despite partial improvement and recovery of bowel function over the course of the first postoperative year, the symptoms of LARS typically persist, with minimal to no improvement over the long term [5]. For this reason, various neorectum reconstruction techniques have been described to augment the reservoir capacity of the colonic conduit; unfortunately, the functional benefits appear only transiently beneficial.
Colonic J-Pouch Anastomosis
The goal of a colonic J-pouch is to create a neorectum reservoir to diminish functional problems associated with a SCA. Initially described similar to an ileal J-pouch, subsequent studies have shown that a shorter length of the efferent limb (6–8 cm) is best when constructing a colonic J-pouch [6]. The splenic flexure typically requires mobilization to provide adequate length to reach the rectal stump without tension. To construct a colonic J-pouch, a colotomy is made on the anti-mesenteric border 5–6 cm from the end of the divided colon. The colon is oriented to loop back on itself to create the J configuration. A linear cutting stapler is inserted through the colotomy and fired to create a channel between the two limbs, while ensuring that the mesentery remains free of the staple line. A purse-string suture can then be placed at the apical colotomy to secure the anvil for a stapled anastomosis.
A colonic J-pouch is not always technically feasible. A narrow pelvis can limit the ability to accommodate the conduit within the pelvis. In addition, a bulky mesentery or colon, insufficient colonic length, or diverticular disease can also interfere with its construction and placement within the pelvis.
Transverse Coloplasty
When a colonic J-pouch is not feasible for technical reasons, an alternative neorectum reservoir configuration is a transverse coloplasty. A longitudinal colotomy about 6–7 cm in length is made along the anti-mesenteric border of the colon, 4 cm proximal to the distal end. The colotomy is then closed transversely, creating a small reservoir. A stapled anastomosis can then be performed in an end-to-end fashion with the colotomy oriented anteriorly. A coloplasty may be better accommodated than a J-pouch when faced with a narrow pelvis or bulky mesentery. However, a coloplasty may not be possible when insufficient colonic length or diverticular disease limits reach into the low pelvis, similar to a colonic J-pouch.
Side-to-End Anastomosis
The side of the proximal conduit can be anastomosed to the end of the rectal stump creating a side-to-end anastomosis (SEA), also known as a Baker anastomosis [7] (Fig. 2). To construct a SEA, a colotomy on the anti-mesenteric border of the colonic conduit is made, 4 cm from the distal end. The efferent defunctionalized limb of the anastomosis, however, should be limited to several centimeters in length, as too much length can result in functional problems with retained debris or mucus. The anvil with the spike component attached is passed through the transected open end of the colon and pushed through the side of the colon where a colotomy would have been made on the anti-mesenteric border. The distal end of the conduit is then stapled closed. The stapler is then passed transanally to create the anastomosis. Alternatively, the stapler can be passed through the open end of the colon conduit with the pin brought out through the colonic wall and the anvil secured in the rectal stump with a purse-string suture, so as to avoid potential sphincter injury with transanal insertion of the stapler. The efferent limb of the colon then is closed with a linear stapler or sutured.
Comparison of Anastomotic Reconstruction Techniques
Complete anastomotic healing with optimal subsequent defecatory function is what the surgeon attempts to accomplish for the patient. Despite best efforts, establishing gastrointestinal continuity within the pelvis often results in impaired bowel evacuation and altered continence. Various colorectal configurations have been proposed to ameliorate these negative functional consequences, generally by virtue of constructing a larger reservoir for stool. Some studies have reported improvement in anastomotic healing rates as well as improvements in bowel function with reservoir colorectal reconstructions when compared to straight colorectal anastomoses. However, the summation of the data suggests that all the colorectal anastomotic techniques are comparable, with no clinically meaningful difference in leak rates, functional metrics, or QOL outcomes.
Hallbook et al. performed a multicenter randomizing 100 patients to SCA or colonic J-pouch anastomosis following low anterior resection (LAR) [8]. Bowel function was evaluated preoperatively, at 2 months and 1 year postoperatively. The authors found a significantly lower symptomatic AL rate in the colonic J-pouch group (2% vs 15%, p = 0.03) and significantly fewer bowel movements at 2 months and 1 year postoperatively in the J-pouch cohort. The ability to defer defecation was also better in the J-pouch group at both time points. The SCA group used more bowel slowing medications at the 2-month and 1-year mark as well. Sensation of incomplete evacuation was higher in the SCA group (p < 0.03) at 2 months postoperatively, but this was not significant at 1 year. However, more J-pouch patients required the use of an enema or suppository to evacuate the neorectum than in the SCA group at the 1 year time point (p = 0.046).
Fazio et al. performed a randomized multicenter trial comparing long-term functional outcomes, QOL, and complications after rectal cancer surgery [9••]. Patients were assigned to either J-pouch eligible or J-pouch ineligible group after proctectomy based on anatomy and patient factors. The J-pouch eligible group was then randomized to either J-pouch or coloplasty. The J-pouch ineligible group was randomized to either SCA or coloplasty. Overall, 297 patients were included in the analysis for functional outcomes and QOL, while 364 patients were included in the analysis for complications. The J-pouch ineligible group had a higher BMI than the J-pouch eligible group (30.5 vs 26.9, p = < 0.001). There were no significant differences in complications between groups. The J-pouch had improved functional outcomes compared with the coloplasty, but there was no clear advantage of the coloplasty over the SCA group. Additionally, QOL measurements were similar among all four groups. J-pouch anastomosis did show reduced clustering and pad usage over coloplasty at 24 months; however, this did not translate into an improvement in QOL. Of note, the J-pouch group was not directly compared to the SCA group in this study.
Hida et al. retrospectively reported long-term functional outcomes of J-pouch versus SCA after LAR for rectal cancer at 5 years in 94 patients [10]. Patients that developed an AL or experienced local recurrence were excluded from the study. Patients with an anastomosis less than 4 cm from the anal verge were analyzed separately from those 5–8 cm from the anal verge. Clinical function was measured using a 17-item questionnaire on a 0–2 scale. Physiologic reservoir function was assessed by measuring the maximum tolerable volume, threshold volume, and compliance with balloon testing. There was no significant difference in bowel function in terms of overall score for the J-pouch or SCA groups when anastomoses were 5 to 8 cm from the anal verge. However, the J-pouch group had fewer bowel movements at night and less urgency. In the group with an anastomosis less than 4 cm from the anal verge, the J-pouch group had fewer bowel movements during the daytime and at night, less urgency, and less soiling, and their functional score was better as well. Not surprisingly, the maximal tolerable volume was higher in the J-pouch group.
Huber et al. compared SEA to colonic J-pouch in 100 patients [11]. Both groups had similar frequency, continence, and functional scores at 1 year and at 2 years postoperatively. Although the J-pouch had a higher measured reservoir volume compared to SEA at 2 years, this did not translate to a clinically meaningful improvement in bowel function.
Marti et al. recently performed a prospective, randomized multicenter trial comparing SEA, J-pouch, and SCA anastomoses following total mesorectal excision [12••]. The primary outcome measured was defecation quality and evacuation problems, while secondary endpoints assessed composite evacuation and incontinence scores, morbidity, and overall survival. In total, 336 patients were enrolled with 112 randomized to each treatment arm (SEA, J-pouch, SCA). No significant differences between groups at baseline were present. Functional outcomes assessed at 6, 12, 18, and 24 months postoperatively did not demonstrate any significant differences. There were no differences in AL rates between groups. The type of reconstruction did not influence continence or evacuation. Notably, neoadjuvant chemoradiation was not associated with impairment in bowel function for any group as measured by composite evacuation score. The authors concluded that surgical technique for reconstruction should be based on surgeon technical ability and comfort level since the three anastomotic techniques are comparable.
Anastomotic Leakage
Anastomotic healing follows a predictable, orderly reparative timetable, with dehiscence occurring when radial forces exceed the resistive forces of the sutures/staples and early scar [13]. In 1887, Halsted demonstrated the importance of the submucosal connective tissue layer for anastomotic construction, the submucosal collagen content, and quality largely responsible for anastomotic integrity [14, 15]. Approximately 70% of initial anastomotic strength has been demonstrated to be lost within the first 72 h after creation, such that early anastomotic strength is dependent on the suture or staple-holding capacity of existing collagen until new collagen can be synthesized by fibroblasts and smooth muscle cells [15]. This portion of the review examines the effects of preoperative bowel preparation, level of mesenteric vessel ligation, mechanical leak testing, fluorescence angiography, fecal diversion, intraoperative pelvic drain placement, and perioperative non-steroidal anti-inflammatory drug (NSAID) use on anastomotic healing.
Preoperative Bowel Preparation
Preoperative administration of mechanical bowel preparation (MBP) with oral antibiotics is likely a key strategy in reducing anastomotic leakage in elective colorectal resection. Preoperative intraluminal antibiotic protection of colon anastomoses alters bacterial flora composition and concentrations and, in fact, has been well appreciated to promote anastomotic healing for decades [16, 17]. More recently, research investigating the intestinal microbiota has provided insight into the relationships between bacterial flora composition alterations, suggesting that the choice of antibiotic may be an important and under-appreciated factor in AL prevention. Research investigating the microbiome has highlighted that while antibiotic use has been demonstrated to be highly effective in preventing leak, the type, duration, and microbial targets of currently recommended antibiotics remain empirical and not yet validated [18, 19].
Two recent independent studies analyzing the Colectomy-Targeted American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database of patients undergoing elective colorectal resection showed MBP with oral antibiotics significantly reduced AL rate. These results emphasized that MBP with oral antibiotics, but not without, were independently associated with reduced AL [20, 21]. In a 2018 meta-analysis including 22 studies with 57,207 patients, comprising 14 randomized controlled trials and eight observational studies, preoperative oral antibiotics, in combination with intravenous antibiotics and MBP, was associated with a lower rate of AL than when oral antibiotics were not administered [22]. A 2017 audit of 3676 patients across 47 countries within the European Society of Coloproctology undergoing elective left-sided colonic or rectal resection also observed a decreased rate of AL when oral antibiotics with MBP (OR 0.52, p = 0.02) was administered, compared to MBP alone, or no bowel preparation. [23••]
Despite the evidence from these large hospital and population-based databases demonstrating a benefit to MPB with oral antibiotics in regard to AL, similar analyses have shown no difference or a higher incidence of leakage following MBP [24, 25]. However, a major limitation of the “no bowel prep” philosophy is the failure to understand that these data were obtained in the absence of the documented superior treatment arm, MBP with oral antibiotics. Therefore, the more accurate conclusion from these data is that MBP without oral antibiotics is equivalent to no MBP [26].
Mesenteric Vessel Ligation Level
A fundamental operative tenet is assuring excellent arterial perfusion and absence of tension on the conduit used for anastomosis. To this point, the level of arterial ligation, “high versus low” tie (origin of the inferior mesenteric artery (IMA) or distal to the left colic artery) during anterior resection has been investigated [27]. When a “high-tie” ligation at the origin of the IMA off the aorta is performed, the perfusion of the proximal limb of the anastomosis is then reliant on the marginal artery arising from the middle colic artery. Although considered adequate to sustain viability of the colon, some patients may have a deficient marginal artery at the splenic flexure, resulting in inadequate colonic perfusion and ischemia [28]. Excluding the oncologic considerations of adequate lymphadenectomy as well as autonomic nerve disruption and potential functional effects of high-tie ligation, and considering the level of mesenteric ligation in terms of colonic perfusion and length, randomized controlled trials have not shown a statistically significant influence on the rate of anastomotic leakage depending on the level of mesenteric vessel ligation [29, 30, 31••].
Irrespective of colonic perfusion, the level of mesenteric vessel ligation is directly related to the ability to construct a tension-free anastomosis. A high-tie ligation of the IMA allows mobility of the mesentery and consequently, the colonic conduit, to reach into the low pelvis. In an anatomical study using cadavers, Bonnet et al. compared the impact of high-tie and “low-tie” vascular transections on the gain in colon length and feasibility of pelvic anastomosis. The distance of proximal colon limb to the lower edge of the pubis symphysis after vascular division was measured after sequential levels of vascular division. The mean cumulative gain in length was significantly higher in high-tie vs low-tie vascular transections (19.1 ± 3.8 vs 8.8 ± 2.9 cm, p = 0.00089) [32•].
Intraoperative Evaluation of the Anastomosis
Once a colorectal anastomosis has been constructed, intraoperative maneuvers to assess its integrity and decrease the risk of leakage are essential. Establishing colorectal anastomotic integrity includes ensuring patency of the lumen without signs of mechanical disruption, bowel ischemia, or bleeding at the anastomosis. Intraoperative evaluation techniques have evolved over time but remain relatively limited, ranging from ensuring intact anastomotic “doughnuts,” mechanical air leak testing, endoluminal inspection, and more recently incorporation of autofluorescent fluorophores to ensure adequate perfusion [33]. The fact that technologies continue to be explored underscores the complexity and incomplete understanding of the multifactorial causative nature of anastomotic leakage.
Anastomotic Mechanical Integrity Testing (“Leak Test”)
No gold standard assessment of anastomotic integrity exists; however, basic mechanical leak tests are universally available in clinical practice, inexpensive, and without drawbacks, and therefore should be routine. Although rates and methods of air leak testing vary significantly in the literature, a decrease in postoperative anastomotic complications has been consistently observed [34, 35, 36••]. The Lahey clinic reported a clinical leak rate of 4.8% in 998 left-sided colorectal anastomoses without proximal diversion. Intraoperative air leaks were noted in 65 of 825 tested anastomoses (7.9%), and in these patients, a clinical leak was diagnosed in 7.7%, compared to 3.8% of anastomoses with a negative air leak test [36••]. Endoscopic interrogation may offer an advantage over rigid proctoscopic insufflation by enabling direct assessment of perianastomotic mucosa viability, mechanical disruptions, and intraluminal bleeding. Colonic mucosa has been shown to be less tolerant to underperfusion compared to the serosa, suggesting that endoscopy may allow a more global evaluation of anastomotic perfusion [33, 37]. Although studies demonstrating a benefit for endoscopic over rigid proctoscopic air leak tests are limited, direct insufflation of air at the level of the anastomosis by intraoperative endoscopy may be more reliable for ensuring adequate intraluminal pressure to demonstrate a leak, when compared to air injected through the anal canal [35].
Anastomotic Perfusion Testing with Fluorescence Angiography
Fluoresence angiography, using indocyanine green (ICG), for assessing anastomotic perfusion is an active area of investigation. This ancillary tool may assist with intraoperative determination of perfusion to the proximal edge of the colonic conduit, and theoretically reduce the rate of anastomotic leakage secondary to ishemia [38]. The PILLAR-2 trial compared a prospective cohort of 139 patients undergoing a left-sided anastomosis (mean distance from anal verge 10 ± 4 cm) with intraoperative ICG assessment matched to historical controls. In the ICG study group, a change in anastomotic plan occurred in 8% of patients, although this did not result in a statistically significant reduction in leak rate when compared to matched historical control patients [39•]. However, only two patients in the ICG group had a leak (1.4% leak rate), and no patient who underwent an operative change based on the ICG findings experienced a leak. Similar findings were reported in a case-matched series of patients of 42 patients undergoing laparoscopic LAR with ICG fluorescence angiography. The descending colon transection margin was changed in two patients (4.7%) based on ICG assessment, and the leak rate was zero for the overall study [38]. Shen et al. performed a meta-analysis including four studies pooling nonrandomized data of 1177 patients comparing colorectal AL in ICG and control groups. When combined, the odds ratio for AL in the ICG group was 0.27 (95% CI, 0.13–0.53, p < 0.001) [40]. The true benefit of intraoperative fluorescence angiography on reducing colorectal anastomotic leaks, despite its proven technical feasibility and low risk, remains to be fully understood [41]. Larger, multicentered, high-quality randomized controlled trials will be needed to confirm the benefit of ICG fluorescence angiography.
Proximal Fecal Diversion
Although fecal diversion after colorectal pelvic anastomosis is not without risks, specifically in relation to the morbidity associated with hypovolemia, electrolyte disturbances, peristomal skin irritation, and the need for a second operation, the consequences of a leak justify and outweigh the risks in the majority of patients. Many retrospective studies have attempted to clarify whether fecal diversion following a colorectal anastomosis decreases the rate of anastomotic leakage; however, retrospective studies are flawed to confidently draw conclusions because of inherent bias, since surgeons will tend to divert when concerned about a particular anastomosis. Several prospective randomized trials have been conducted, including a Cochrane Database meta-analysis of randomized trials reported in 2010, which reported a significant reduction in anastomotic leakage in diverted patients (RR 0.33; 95% CI 0.21–0.53) [42•, 43,42,45]. In the two largest randomized trials, AL rates were dramatically reduced [44, 45]. Matthieseen et al. performed a large multicenter randomized trial, 116 in the stoma group and 118 in the no stoma group [45]. There was a significantly higher leak rate in patients without a stoma (28.2%) compared to those with a stoma (10.3%), as well as a lower reoperation rate for pelvic sepsis in the diverted patients compared to non-diverted patients (8.6% vs 25.4%, respectively). Chude et al. randomized 136 patients to diversion and 120 patients to no diversion [44]. The leak rate was 10% compared to 2.2% in the non-diverted and diverted patients, respectively. Based on prospective, high-level evidence data consistently demonstrating lower leak rates and septic complications, fecal diversion following a pelvic colorectal anastomosis should be routinely practiced, and selectively omitted in patients only at lowest risk for developing leakage. Of course, balancing a patient’s wishes, prior treatments, and tumor-specific risk factors should be individualized, such that selective rather routine fecal diversion is part of the preoperative discussion and intraoperative decision making process.
Pelvic Drain Placement Intraoperatively
The impact of infraperitoneal pelvic drain placement following colorectal anastomosis on postoperative complications, including anastomotic leakage rate, has been prospectively studied [46]. Drains have been prophylactically placed in the pelvis for three reasons: to drain residual collecting fluid at risk for contamination, to detect an early leak, or to provide a track for late leakage. Yet, many studies have reported a very low sensitivity for detection of clinical leakage based on enteric or purulent contents within the drain, suggesting that drains do not accomplish their assumed function reliably. A considerable amount of evidence suggests that colorectal anastomoses can be safely performed with omission of a prophylactic drain, although most surgeons continue to use them routinely. A large French trial randomizing almost 500 patients undergoing a rectal or anal anastomosis to pelvic drainage or no drainage showed no difference in postoperative infectious, AL, or secondary reoperative rate between the groups [47]. A recently published large randomized trial, GRECCAR 5, examined whether drainage after infraperitoneal anastomoses after proctectomy for rectal cancer affected the rate of postoperative pelvic sepsis [48]. No significant difference was seen between the randomized groups in relation to pelvic sepsis (16.1% vs 18%, drain vs no drain, respectively) or rate or reoperation (16.6% vs 21%, drain vs no drain, respectively), suggesting that pelvic drainage may not confer benefit. Despite the findings of these randomized studies, a meta-analysis including 2277 patients from three randomized clinical trials (RCTs) and five non-RCTs determined that pelvic drainage reduced both the rate of leak and reintervention in patients with an extraperitoneal colorectal anastomosis (OR = 0.51, 95% CI 0.36–0.73, and OR = 0.29, 95% CI 0.18–0.46, respectively) compared to patients without drainage [49]. Although randomized controlled trials have not demonstrated a proven benefit, many confounding variables could potentially impact the true value of a pelvic drain, such that abandoning the practice altogether cannot be recommended at this time.
Non-steroidal Anti-inflammatory Drug Perioperative Pain Control
Opioid sparing postoperative pain management approaches have been increasingly employed to enhance rapid patient recovery. With the increase in the use of these medications perioperatively, non-steroidal anti-inflammatory drugs (NSAID), such as ketorolac, diclofenac, and ibuprofen, have been questioned regarding their potential deleterious impact on anastomotic healing as well as increased risk for bleeding complications [50, 51]. Animal models of bowel anastomoses in diclofenac-treated rats have demonstrated reduced tensile strength, reduced bursting pressure, and reduced anastomotic collagen deposition [52,51,54]. However, the available clinical evidence thus far has been limited by selection bias, large crossover, and inconsistent drugs, doses, and schedules. Kotagal et al. examined postoperative complications in 398,752 patients undergoing gastrointestinal surgery (56% colorectal surgery) within a large insurance claims database who were exposed to ketorolac on the day of surgery or afterwards [55]. Five percent of the patients had a claim for ketorolac during the index hospitalization, and in an adjusted analysis, patients receiving ketorolac had a higher odds of emergency department presentation within 30 days of surgery, readmission, and reintervention. In a meta-analysis containing 6 RCTs (n = 473 patients) and 11 observational studies (n = 20,184), postoperative NSAID use and intestinal anastomotic dehiscence was investigated. Each study comprising the analysis ranged from 40 to 166 patients and was predominantly colorectal operations; however, no trial or study was powered to detect differences in anastomotic complications. No difference in AL was detected among the randomized trials; however, the observational studies demonstrated a 1.46 odds ratio of increased AL when exposed postoperatively to an NSAID. On further subset analysis, only nonselective NSAIDs, as opposed to COX-2 selective NSAIDs, in the observational data resulted in an increased risk of AL [55, 56•]. The current low-quality evidence suggesting an association between perioperative NSAID use and anastomotic dehiscence certainly raises concern; however, high-quality prospective data is necessary to determine its true effect on colorectal anastomotic healing and leak.
Conclusions
Despite the various pelvic colorectal anastomotic reconstructive configurations and efforts to diminish anastomotic leakage, complete anastomotic healing with preserved bowel function remains imperfect. A neorectum reservoir may offer slight functional benefits over a straight end-to-end anastomosis; however, the strongest evidence suggests that all reconstruction outcomes are relatively equivalent. For this reason, the technique used by each surgeon should be individualized based on patient-specific factors, surgeon expertise, and preference. Better understanding of the causes of bowel dysfunction may also provide future insight into optimal reconstruction techniques. Anastomotic leakage is multifactorial, and its underlying cause still remains often unclear. However, several perioperative modifiable factors can reliably reduce leak rate, and must be carefully considered for every pelvic colorectal anastomosis created.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Kingham TP, Pachter HL. Colonic anastomotic leak: risk factors, diagnosis, and treatment. J Am Coll Surg. 2009;208(2):269–78.
Neutzling CB, et al. Stapled versus handsewn methods for colorectal anastomosis surgery. Cochrane Database Syst Rev. 2012;(2):CD003144.
Slieker JC, Daams F, Mulder IM, Jeekel J, Lange JF. Systematic review of the technique of colorectal anastomosis. JAMA Surg. 2013;148(2):190–201.
Martellucci J. Low anterior resection syndrome: a treatment algorithm. Dis Colon Rectum. 2016;59(1):79–82.
Bryant CL, Lunniss PJ, Knowles CH, Thaha MA, Chan CL. Anterior resection syndrome. Lancet Oncol. 2012;13:e403–8.
Lazorthes F, Gamagami R, Chiotasso P, Istvan G, Muhammad S. Prospective, randomized study comparing clinical results between small and large colonic J-pouch following coloanal anastomosis. Dis Colon Rectum. 1997;40(12):1409–13.
Baker JW. Low end to side rectosigmoidal anastomosis; description of technic. Arch Surg. 1950;61(1):143–57.
Hallbook O, et al. Randomized comparison of straight and colonic J pouch anastomosis after low anterior resection. Ann Surg. 1996;224(1):58–65.
•• Fazio VW, et al. A randomized multicenter trial to compare long-term functional outcome, quality of life, and complications of surgical procedures for low rectal cancers. Ann Surg. 2007;246(3):481–8 discussion 488–90. An important RCT comparing J pouch to coloplasty and coloplasty to straight end-to-end anastomosis demonstrating functional superiority of pouch to coloplasty but no difference between colopasty and straight anastomosis.
Hida J, Yoshifuji T, Tokoro T, Inoue K, Matsuzaki T, Okuno K, et al. Comparison of long-term functional results of colonic J-pouch and straight anastomosis after low anterior resection for rectal cancer: a five-year follow-up. Dis Colon Rectum. 2004;47(10):1578–85.
Huber FT, Herter B, Siewert JR. Colonic pouch vs. side-to-end anastomosis in low anterior resection. Dis Colon Rectum. 1999;42(7):896–902.
•• Marti, W.R., et al., Clinical outcome after rectal replacement with side-to-end, colon-J-pouch, or straight colorectal anastomosis following total mesorectal excision: a Swiss prospective, randomized, multicenter trial (SAKK 40/04). Ann Surg, 2018. A major RCT that showed no difference in functional outcomes between anastomotic configurations.
Thompson SK, Chang EY, Jobe BA. Clinical review: healing in gastrointestinal anastomoses, part I. Microsurgery. 2006;26(3):131–6.
Hawley PR. Causes and prevention of colonic anastomotic breakdown. Dis Colon Rectum. 1973;16(4):272–7.
Thornton FJ, Barbul A. Healing in the gastrointestinal tract. Surg Clin North Am. 1997;77(3):549–73.
Cohn I Jr, Rives JD. Antibiotic protection of colon anastomoses. Ann Surg. 1955;141(5):707–17.
LeVeen HH, Wapnick S, Falk G, Olivas O, Bhat D, Gaurdre M, et al. Effects of prophylactic antibiotics on colonic healing. Am J Surg. 1976;131(1):47–53.
Shogan BD, et al. Collagen degradation and MMP9 activation by enterococcus faecalis contribute to intestinal anastomotic leak. Sci Transl Med. 2015;7(286):286ra68.
Shogan BD, Smith DP, Christley S, Gilbert JA, Zaborina O, Alverdy JC. Intestinal anastomotic injury alters spatially defined microbiome composition and function. Microbiome. 2014;2:35.
Scarborough JE, Mantyh CR, Sun Z, Migaly J. Combined mechanical and oral antibiotic bowel preparation reduces incisional surgical site infection and anastomotic leak rates after elective colorectal resection: an analysis of colectomy-targeted ACS NSQIP. Ann Surg. 2015;262(2):331–7.
Kiran RP, et al. Combined preoperative mechanical bowel preparation with oral antibiotics significantly reduces surgical site infection, anastomotic leak, and ileus after colorectal surgery. Ann Surg. 2015;262(3):416–25 discussion 423–5.
McSorley ST, Steele CW, McMahon AJ. Meta-analysis of oral antibiotics, in combination with preoperative intravenous antibiotics and mechanical bowel preparation the day before surgery, compared with intravenous antibiotics and mechanical bowel preparation alone to reduce surgical-site infections in elective colorectal surgery. BJS Open. 2018;2(4):185–94.
•• European Society of Coloproctology collaborating, G. Association of mechanical bowel preparation with oral antibiotics and anastomotic leak following left sided colorectal resection: an international, multi-centre, prospective audit. Color Dis. 2018;20(Suppl 6):15–32 A large prospective "real world" analysis showing a reduction in anastomotic leakage when mechanical bowel preparation with oral antibiotics is administered for left sided colorectal anastomoses.
Jung B, Påhlman L, Nyström PO, Nilsson E, for the Mechanical Bowel Preparation Study Group. Multicentre randomized clinical trial of mechanical bowel preparation in elective colonic resection. Br J Surg. 2007;94(6):689–95.
Bucher P, et al. Mechanical bowel preparation for elective colorectal surgery: a meta-analysis. Arch Surg. 2004;139(12):1359–64 discussion 1365.
Senagore A. Difficult Decisions in Colorectal Surgery. In: Ferguson M, editor. Difficult decisions in surgery: an evidence-based approach. Switzerland: Springer; 2017.
Lange MM, Buunen M, van de Velde CJH, Lange JF. Level of arterial ligation in rectal cancer surgery: low tie preferred over high tie. A review. Dis Colon Rectum. 2008;51(7):1139–45.
Lange JF, Komen N, Akkerman G, Nout E, Horstmanshoff H, Schlesinger F, et al. Riolan’s arch: confusing, misnomer, and obsolete. A literature survey of the connection(s) between the superior and inferior mesenteric arteries. Am J Surg. 2007;193(6):742–8.
Matsuda K, Hotta T, Takifuji K, Yokoyama S, Oku Y, Watanabe T, et al. Randomized clinical trial of defaecatory function after anterior resection for rectal cancer with high versus low ligation of the inferior mesenteric artery. Br J Surg. 2015;102(5):501–8.
Koda K, Saito N, Seike K, Shimizu K, Kosugi C, Miyazaki M. Denervation of the neorectum as a potential cause of defecatory disorder following low anterior resection for rectal cancer. Dis Colon Rectum. 2005;48(2):210–7.
•• Fujii S, et al. Randomized clinical trial of high versus low inferior mesenteric artery ligation during anterior resection for rectal cancer. BJS Open. 2018;2(4):195–202 A RCT of "high vs low" tie vessel ligation showing no difference in rate of anastomotic leak.
• Bonnet S, et al. High tie versus low tie vascular ligation of the inferior mesenteric artery in colorectal cancer surgery: impact on the gain in colon length and implications on the feasibility of anastomoses. Dis Colon Rectum. 2012;55(5):515–21 A cadaver anatomic study demonstrating the impact and feasibility of low anastomosis by demonstrating successive gain in length of colon reach with increasing level of vascular ligation.
Nachiappan S, Askari A, Currie A, Kennedy RH, Faiz O. Intraoperative assessment of colorectal anastomotic integrity: a systematic review. Surg Endosc. 2014;28(9):2513–30.
Beard JD, Nicholson ML, Sayers RD, Lloyd D, Everson NW. Intraoperative air testing of colorectal anastomoses: a prospective, randomized trial. Br J Surg. 1990;77(10):1095–7.
Li VK, et al. Use of routine intraoperative endoscopy in elective laparoscopic colorectal surgery: can it further avoid anastomotic failure? Surg Endosc. 2009;23(11):2459–65.
•• Ricciardi R, et al. Anastomotic leak testing after colorectal resection: what are the data? Arch Surg. 2009;144(5):407–11 discussion 411–2. A large institutional experience reporting the impact of mechanical leak testing on anastomotic leak rates, suggesting its high clinical value and implications when a positive leak test is identified.
Singh DB, et al. Intraoperative measurement of colonic oxygenation during bowel resection. Adv Exp Med Biol. 2009;645:261–6.
Boni L, Fingerhut A, Marzorati A, Rausei S, Dionigi G, Cassinotti E. Indocyanine green fluorescence angiography during laparoscopic low anterior resection: results of a case-matched study. Surg Endosc. 2017;31(4):1836–40.
• Jafari MD, et al. Perfusion assessment in laparoscopic left-sided/anterior resection (PILLAR II): a multi-institutional study. J Am Coll Surg. 2015;220(1):82–92 e1 The landmark prospective trial investigating fluorescence angiography to assess perfusion of the colonic conduit showed feasibility, but no definitive evidence in reduction in anastomotic leakage rates.
Shen R, Zhang Y, Wang T. Indocyanine green fluorescence angiography and the incidence of anastomotic leak after colorectal resection for colorectal cancer: a meta-analysis. Dis Colon Rectum. 2018;61(10):1228–34.
Kin C, Vo H, Welton L, Welton M. Equivocal effect of intraoperative fluorescence angiography on colorectal anastomotic leaks. Dis Colon Rectum. 2015;58(6):582–7.
• Montedori, A., et al., Covering ileo- or colostomy in anterior resection for rectal carcinoma. Cochrane Database Syst Rev, 2010(5): p. CD006878. A Cochrane review of 6 RCT's showing significant reduction in anastomotic leak and re-operation when fecally diverted after a pelvic colorectal anastomosis.
Thoker M, Wani I, Parray FQ, Khan N, Mir SA, Thoker P. Role of diversion ileostomy in low rectal cancer: a randomized controlled trial. Int J Surg. 2014;12(9):945–51.
Chude GG, et al. Defunctioning loop ileostomy with low anterior resection for distal rectal cancer: should we make an ileostomy as a routine procedure? A prospective randomized study. Hepatogastroenterology. 2008;55(86–87):1562–7.
Matthiessen P, Hallbk O, Rutegrd J, Simert G, Sjdahl R. Defunctioning stoma reduces symptomatic anastomotic leakage after low anterior resection of the rectum for cancer: a randomized multicenter trial. Ann Surg. 2007;246(2):207–14.
Sagar PM, Hartley MN, Macfie J, Mancey-Jones B, Sedman P, May J. Randomized trial of pelvic drainage after rectal resection. Dis Colon Rectum. 1995;38(3):254–8.
Merad F, Hay JM, Fingerhut A, Yahchouchi E, Laborde Y, Pélissier E, et al. Is prophylactic pelvic drainage useful after elective rectal or anal anastomosis? A multicenter controlled randomized trial. French Association for Surgical Research. Surgery. 1999;125(5):529–35.
•• Denost Q, et al. To drain or not to drain infraperitoneal anastomosis after rectal excision for cancer: the GRECCAR 5 randomized trial. Ann Surg. 2017;265(3):474–80 A major RCT comparing drain or no drain in patients undergoing infraperitoneal anastomosis showing no difference in pelvic septic complications, rate of re-operation, or somta closure between the groups, suggesting drain placement intraoperatively does not confer benefit.
Rondelli F, Bugiantella W, Vedovati MC, Balzarotti R, Avenia N, Mariani E, et al. To drain or not to drain extraperitoneal colorectal anastomosis? A systematic review and meta-analysis. Color Dis. 2014;16(2):O35–42.
Klein M, Gogenur I, Rosenberg J. Postoperative use of non-steroidal anti-inflammatory drugs in patients with anastomotic leakage requiring reoperation after colorectal resection: cohort study based on prospective data. BMJ. 2012;345:e6166.
Kverneng Hultberg D, Angenete E, Lydrup ML, Rutegård J, Matthiessen P, Rutegård M. Nonsteroidal anti-inflammatory drugs and the risk of anastomotic leakage after anterior resection for rectal cancer. Eur J Surg Oncol. 2017;43(10):1908–14.
Inan A, Koca C, Sen M. Effects of diclofenac sodium on bursting pressures of anastomoses and hydroxyproline contents of perianastomotic tissues in a laboratory study. Int J Surg. 2006;4(4):222–7.
de Sousa JB, Soares EG, Aprilli F. Effects of diclofenac sodium on intestinal anastomotic healing. Experimental study on the small intestine of rabbits. Dis Colon Rectum. 1991;34(7):613–7.
Klein M, Krarup PM, Kongsbak MB, Ågren MS, Gögenur I, Jorgensen LN, et al. Effect of postoperative diclofenac on anastomotic healing, skin wounds and subcutaneous collagen accumulation: a randomized, blinded, placebo-controlled, experimental study. Eur Surg Res. 2012;48(2):73–8.
Kotagal M, Hakkarainen TW, Simianu VV, Beck SJ, Alfonso-Cristancho R, Flum DR. Ketorolac use and postoperative complications in gastrointestinal surgery. Ann Surg. 2016;263(1):71–5.
• Smith SA, et al. Postoperative nonsteroidal anti-inflammatory drug use and intestinal anastomotic dehiscence: a systematic review and meta-analysis. Dis Colon Rectum. 2016;59(11):1087–97 A meta-analysis showing no significant increase in anastomotic leak among the included RCT's (n=6), however, a statistically signficant increase in leak rate among the included observation studies (n=11).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Surgery and Surgical Innovations in Colorectal Cancer
Rights and permissions
About this article
Cite this article
Felder, S., Lee, J.T. Techniques for Colorectal Anastomotic Construction Following Proctectomy and Variables Influencing Anastomotic Leak. Curr Colorectal Cancer Rep 15, 8–17 (2019). https://doi.org/10.1007/s11888-019-00425-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11888-019-00425-3