Abstract
Purpose of Review
The minimally invasive approach to colorectal cancers has been validated as providing oncologic outcomes comparable to open surgery. Current laparoscopic instrumentation, however, has its limitations especially in the performance of rectal cancer resections. Robotic surgery for colorectal cancers is an important addition to the technologies available to the surgeon. We review the literature and draw on our own experience to examine the advantages and disadvantages of robot-assisted surgery for the treatment of colorectal cancers and the evidence for the superior outcomes frequently cited and to identify subsets that may benefit the most.
Recent Findings
Most of the evidence for robotic surgery emanates from nonrandomized studies. These studies show acceptable perioperative and oncologic outcomes, with lower conversion rates and circumferential margin positivity than with laparoscopy. The only randomized trial, the ROLARR, did not show any significant difference between the two modalities regarding conversion rates or pathologic outcomes.
Summary
Current evidence does not conclusively support robotic surgery over laparoscopy or vice versa. Robotics is an emerging field and innovations including the current da Vinci Xi system, single port, and TAMIS platforms may all enable more complex surgeries going forward. Robotic surgery has a short learning curve. Patients undergoing surgery for low rectal cancers, who have any combination of male gender, obesity, and T3 cancers, as well as the need for complete mesocolic excision in right colon cancers, may be considered for the robotic approach with appreciable benefits and no detriment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The laparoscopic approach to colon and rectal cancer surgery is well established, based on the evidence from large randomized trials. The evidence is robust for colon cancers from the MRC CLASICC, COLOR, and COST trials [1,2,3,4]. The evidence for the application of laparoscopy in rectal cancer surgery is not as robust, based on subset analyses of a small number of patients in the MRC trial and from the COLOR II trial comparing laparoscopy to open total mesorectal excision (TME) for rectal cancers [5]. A high conversion rate of 34% and a circumferential resection margin (CRM) positivity of 12% were found in the laparoscopic arm of the MRC trial [1]. Though the margin positivity did not translate into poorer survival outcomes, patients who converted from minimally invasive to open approach fared poorly in terms of 5-year disease-free survival.
Laparoscopy in its current form is well adapted for colon resections and multiquadrant surgery, but the rigid in-line instrumentation and 2-dimensional image systems are not well suited for dissection in the narrow confines of the pelvis, during TME for low rectal cancers. The long learning curve of 150–200 cases also makes training and dissemination of these skills an arduous task [6].
Robotics has developed from a need to overcome these limitations and provides a computer interface, high-definition 3-dimensional optics, and advanced wristed instrumentation, which together provide for a more ergonomic and precise dissection, especially during rectal cancer surgery. The major benefit comes from the highly magnified image that provides depth perception and the wristed instruments, which allow for 7 degrees of freedom, more than possible with laparoscopic instruments or indeed the human wrist. The ability of instrumentation to maneuver in tight, confined spaces allows unmatched precision, and this is of particular utility in prostatic and rectal cancer surgery. Tremor filtration by the computer interface negates physiologic tremor and prevents injuries due to past pointing [7].
The major issues with the robotic platform are increase in cost and lack of tactile tissue feedback known as haptics. Haptics is fundamental to our understanding of tissue structure and nature, and the lack of haptics can lead to tearing of tissues such as bowel, blood vessels, and mesentery, in inexperienced hands.
Colon and rectal surgery as a specialty adopted robotic surgery as early as 2002, with Weber et al. reporting the first robot-assisted resection (mobilization of the right colon and sigmoid) for benign pathology and Hashizume for malignant colonic pathology [8, 9]. This was rapidly followed by an incremental body of work by D’Annibale et al. from Italy [10]. In the USA, Rawlings, Pigazzi, and Prasad were the early pioneers, establishing the important tenets, techniques, and body of literature, which have been widely used, adapted, and quoted [11,12,13]. A significant contribution in recent years has been from South Korea, with SH Kim, NK Kim, GS Choi, DJ Choi, JH Baek, SH Baik, and BS Min performing some seminal and innovative work [14,15,16,17,18].
Robotic Colectomy for Cancer
Robotic surgery has been used to perform all defined colonic resections for cancer. While colectomy is feasible and can be safely performed, no study has shown an added benefit over conventional laparoscopy.
Right hemicolectomy is the most common procedure and has been extensively studied. Most of the early literature consisted of reports of colonic mobilization, with the vascular division and anastomosis performed extracorporeally. Essentially, the robot was used only to free the bowel, and hence, there was no difference in oncologic outcomes when compared with laparoscopy. de Souza et al. showed that robotic right colectomy increases operative time, with length of stay, leak rate, and short-term oncologic outcomes being similar to laparoscopy [19]. The robotic procedure was significantly more expensive than laparoscopy. They recommend that right hemicolectomy be part of the training pathway to eventual performance of robotic total mesorectal excision (RTME), a concept popularized by the senior author as detailed below.
Interest in robotic right hemicolectomy has resurfaced with the concept of complete mesocolic excision (CME), which involves ligation of the vascular pedicles on the superior mesenteric vessels and resection along the lines of embryologic fusion as developed by Hohenberger et al. [20]. This is a very difficult operation to perform laparoscopically, especially the dissection of the superior mesenteric vasculature and the vessels over the head of the pancreas (middle colic pedicle); the robotic platform facilitates this portion of the procedure. CME improves recurrence-free and disease-free survival and is an important advance in managing right colon cancers [21].
Sigmoid colectomy is the other procedure performed frequently. This represents the colonic mobilization, vascular ligation, and lymphadenectomy as performed in the initial phase of TME for rectal cancer. It has some merits in familiarizing the surgeon for eventual robotic TME. There is, however, no oncologic or clinical benefit over laparoscopy, when performed for sigmoid cancers. A significant increase in operative time and earlier return of bowel function for robotic sigmoid colectomy has been cited by most authors [22]. The presence of a single vascular pedicle in line with the axis of the bowel makes sigmoid colectomy well suited for a single incision or reduced port approach when performed robotically. There is no commercially available port for single port robotic colectomy as yet, but Min et al. [23] have devised an elegant approach using a wound retractor sealed with a glove to form the dome of the “single” port. Using robotic and conventional trocars through the cut fingers of the glove, they reported a series of sigmoid colectomies, with no conversions, no leaks, and a mean lymph node yield of 16.8 nodes. This may eventually become a paradigm for single incision robotic procedures across the board for all sites of colon and rectal cancer, with the development of better single port devices for the robotic platform.
Robotic Total Mesorectal Excision for Rectal Cancer
Fundamentals of Patient Preparation, Positioning, and Robotic Technique for RTME
Patient Preparation and Position
The patient is kept on a low residue diet and full bowel preparation (mechanical and oral antibiotics) is administered. Preoperative prophylaxis against deep vein thrombosis is given with fractionated or unfractionated heparin 12 h before the procedure. Sequential compression sleeves are placed and a single prophylactic dose of ertapenem 1 g is administered before incision.
The patient is positioned in the modified lithotomy position of Lloyd Davies with a steep Trendenlenburg with a right side down tilt of 15–20°. A beanbag is used to secure the patient and adequate padding with foam and gel pads used to cover all bony points and potential sites of nerve compression. Attention is also directed to padding over the shoulders and posterior triangles to prevent brachial plexopathy due to pressure from the shoulder restraints.
Robotic Technique
The procedure can be accomplished in two ways:
-
1.
Totally robotic approach: The entire procedure of left colon mobilization, vascular division, lymphadenectomy, splenic flexure mobilization, and total mesorectal excision is performed robotically. This often requires multiple movements of the robotic cart around the patient (left shoulder, left hip, and between the legs), since the commonly used da Vinci Si system has limited reach and the arms can collide at extremes of position. Due to the need to move the cart and redock, it is time-consuming. Variants of the technique using a left hip position with two sets of ports, one for suprapelvic dissection and another for the RTME with overlap between the ports, have been popularized by Choi et al. [15] and allow to perform the operation without changing cart position.
The latest Xi version of the robot is designed for multiquadrant surgery and allows a totally robotic procedure without the need for changing cart position or redocking.
-
2.
Hybrid approach: Here the suprapelvic component is completed rapidly laparoscopically, and the robot is docked at the left hip or between the legs only for the critical pelvic portion of the operation. This is our preferred approach [23]. The advantage is that it shortens the procedure, and as shown by Baik et al., it has a lower rate of complications than the totally robotic approach [16]. In the early part of the surgeon’s learning curve, it is preferable to begin with the hybrid approach and transition to the totally robotic technique once more experience accrues. The robotic cart between the legs is the most ergonomic for pelvic dissection and is easier for the novice surgeon. A reverse hybrid approach has also been described, where the RTME is first completed and then the laparoscopic colon mobilization and lymphadenectomy and anastomosis performed thereafter [24].
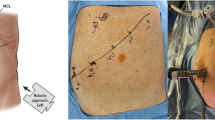
Whatever technique is used, ports are placed along the curve of an imaginary fan, with the tip representing the target anatomy in the pelvis. The optical trocar should be placed to the right of the midline, to allow enough space for the trocars in the left abdomen. The recommended approach for this technique is to select early or small rectal cancers in the upper and mid rectum to begin with and transition to more complex distal and/or bulky tumors.
Outcomes of RTME
There is concordance between robotic surgery and laparoscopy for most studied perioperative outcomes including operative time and blood loss, length of stay and return of bowel function, and resumption of diet. Conversion rates are, however, much lower than with laparoscopy, varying from 0 to 4.9% [13,14,15,26,16, 25–27] as compared to 7.3 to 34% in large laparoscopic series [1,29,, 28–30]. This lower conversion rate favoring robotic surgery (2%) versus 7.5% for laparoscopy (p = 0.0007) has been reported in the meta-analysis by Trastulli et al. [31]. The anastomotic leak rate ranges from 1.8 to 12.1% [13,14,15,26,16, 25–27], which is similar to the 13% leak rate reported in the COLOR II trial, which compared laparoscopic to open rectal cancer resection [5].
The pathologic outcomes for rectal cancer resections are comparable to open surgery with a CRM positivity rate of 0–7.1%, a distal margin positivity of 0–1.9%, and a lymph node yield of 13–20 nodes [13,14,15,26,16, 25–27] (Table 1). The CRM positivity is lower than that reported in trials of laparoscopic rectal surgery [1]. In a meta-analysis by Xiong et al. [34••], the CRM positivity for laparoscopy was 5.78 versus 2.74% for robotics (p = 0.04).
Disease-free (DFS) and overall survival (OS) rates are comparable to open and laparoscopic TME. The DFS rates at 3 years are between 73.7 and 79.2% and the OS rates between 90.1 and 97.0% [16, 18, 25, 27] (Table 1). Of the studies reporting 5-year survival data, Park et al. with a median follow-up of 58 months found no differences in 5-year OS, DFS, or local recurrence rates between patients treated with robotic and laparoscopic surgery for rectal cancer [33••]. The 5-year OS rate was 92.8% in robotic and 93.5% for laparoscopic surgical procedures. The 5-year DFS rates were 81.9 and 78.7%, respectively. In 200 consecutive resections for rectal cancer, Hara et al. [32••] reported local pelvic control and overall and disease-free survival rates of stage III rectal cancer patients at 5 years as 93.0, 88.6, and 76.6%, respectively.
Genitourinary function may become disturbed after TME, due to injury to the superior hypogastric nerves around the root of the inferior mesenteric artery (IMA) or to the pelvic splanchnic nerves. Sexual dysfunction occurs after laparoscopy and robotic surgery, but there is earlier recovery in the robotic arm (6 months) as compared to laparoscopy (1 year). Bladder filling and voiding function deteriorate when measured at 1 month but recover within 3 months in robotic versus 6 months in laparoscopy [35]. Luca et al. found no change in bladder function in the robotic arm and postulated that this is due to better visualization of the nerves and early catheter removal [36]. A better visualization and better tissue traction during robotic surgery lead to a clean and precise dissection, with reduced trauma to the nerves. The ability to dissect the root of the IMA completely before applying an energy device or clip reduces the risk of inadvertent injury to the superior hypogastric plexus that arises around the vessel origin.
ROLARR Trial
The ROLARR (Robotic versus Laparoscopic Resection for Rectal cancer) trial is an international, multicenter, prospective, randomized, and controlled, unblinded, parallel-group trial of robotic-assisted versus laparoscopic surgery for the curative treatment of rectal cancer [37••]. It is the only randomized study till date with reasonable numbers. The preliminary results were presented at the American Society of Colon and Rectal Surgeons 2015 meeting. Analysis of short-term outcomes shows that robotic systems have a lower conversion rate (CR) compared with the laparoscopic approach (8.1 vs. 12.2%), though not statistically significant (p = 0.158).
The best outcomes were in male patients (close to 50% CR reduction rate: 8.7% in the robotic group vs. 16% in the laparoscopic group, p = NS), low anterior resections (7.2 vs. 13.3%, p = NS), and obese patients (18.9 vs. 27.8%, p = NS).
The perioperative complication rates (33.1% in the robotic group vs. 31.7% in the laparoscopic group) and oncological outcomes (CRM positivity 5.1% in the robotic group vs. 6.3% in the laparoscopic group) were similar. The absence of a statistically significant difference might be explained by the limited number of patients enrolled in the study (around 400) and by the bias related to differences in the surgeons’ expertise in the robotic and laparoscopic approach. The surgeons in this group on average had performed a mean of 91 laparoscopic versus only 25 robotic anterior resections for rectal cancer. These were therefore expert laparoscopic surgeons who had likely not crossed their robotic learning curve. A randomized study with larger numbers, having surgeons comfortable with both the laparoscopic and robotic approaches, is needed to identify if the patient subgroups such as the obese, low rectal cancer, and male patients would show any significant difference with the two approaches.
The counterpoint is that both the ACOSOG Z6051 [38••] and the ALaCaRT [39••] trials did not support the noninferiority of laparoscopy versus open surgery for rectal cancers. If well-designed randomized controlled trials are unable to show a noninferiority of laparoscopic surgery for rectal cancer, when compared to open surgery, then the jury is still out with regard to the optimal surgical approach to rectal cancer.
Cost and Robotic Surgery
Robotic surgery is more expensive than laparoscopy due to the capital cost of purchase of the robotic system, which has to be amortized over multiple patients, increased operative time, and the cost of the instruments and disposables.
We observed that the mean cost of robotic TME was $22,640 ± 7300 (US dollars, USD) versus $18,330 ± 7940 for hybrid hand-assisted laparoscopic TME (p = 0.005) [25]. On average, robotic surgery was more expensive by $4300.
Similarly, Park et al. [33••] found that the total mean cost of laparoscopic surgery was $10,101.3 ± 2804.8 (USD) and that of robotic surgery was $12,742.5 ± 3509.9 (USD) (p < 0.001).
It is likely that cost will decrease once more companies enter the market with new robotic installations and create a competitive market.
Recent Advances and Trends in Robotic Surgery
-
1.
The da Vinci Xi system
The da Vinci Xi surgical robotic system is a highly advanced fourth generation device of the robotic line and is the most sophisticated surgical robotic system available. This platform, released in 2015, enhances the surgeon’s performance and simplifies the system setup and docking procedure. The major enhancements include the optics as well as the working arms. A completely new type of robotic arm support was introduced based on an overhead boom from which four independent robotic arms are suspended. This allows the arms to rotate as a group in a coordinated, computer-controlled fashion. This ergonomic design, together with a decreased size, extended range of motion, and increased reach of the instruments, is key to improving access to all quadrants of the abdomen without the need to redock the robotic system. A novel laser targeting facilitates docking of all arms and the system is able to optimize the arm position automatically. The optical system is significantly enhanced and simplified and the scope can be positioned in any robotic arm. All of these facilitate multiquadrant surgery without the need to reposition or redock the robot.
-
2.
Single incision/single port/reduced port robotic colorectal resections
No single port device approved for robotic colorectal surgery exists as yet. A modified port using an Alexis wound retractor placed through a transumbilical incision, with a surgical glove to create a diaphragm for the port has been used by Min et al. [23] to perform single port sigmoid colectomy. Robotic and assistant trocars are placed through the cut fingers of the glove and a three-arm robot configuration is used. Short-term oncologic outcomes and perioperative parameters are acceptable with this technique.
Reduced port surgery, using the FDA-approved single port through a transumbilical incision, with one additional robotic port in the right iliac fossa has been reported by Bae et al. [40] for left colon, sigmoid, and rectosigmoid cancers with no conversions and adequate pathologic outcome measures. The da Vinci single port has four ports: one for an 8.5-mm robotic camera, one for the assistant, and two curved trocars that allow the instruments to cross the field. The major advantage over single incision laparoscopy is that the computer is able to allocate each instrument to the hand on the side of the ipsilateral visual field enabling the left instrument to be controlled effortlessly with the right hand and vice versa.
-
3.
Transanal minimally invasive surgery with the robot
Transanal surgery has been practiced for several years using transanal endoscopic microsurgery techniques (TEM) and as laparoscopic transanal minimally invasive surgery (TAMIS) for local excision of rectal neoplasms and for performing the TME for the extraperitoneal portion of the rectum from below (reverse TME, bottom-up TME). The proponents of TAMIS TME claim a lower incidence of CRM positivity and, hence, better oncologic outcomes [41]. The first robotic transanal surgery (RTS) for local excision of a rectal neoplasm was performed in 2012 [42]. Subsequently, the first robot-assisted transanal TME (RATS TME) for rectal cancer as part of proctocolectomy in a patient with familial adenomatous polyposis was reported by Larach et al. [43]. The robot was used to develop the plane between the visceral and parietal fascia after division of the mucosa at the dentate line and closure of the rectal stump with a purse string. The GelPOINT path transanal access port (Applied Medical, Rancho Santa Margarita, CA, USA) is used to seal the anal canal, establish the air space, and provide the working interface for the robotic and assistant ports. The authors note that contrary to the experience with laparoscopic TAMIS TME, RATS TME is easiest for mid and distal rectal dissection and not for upper rectal dissection. This is a complex operation and should be undertaken only after considerable experience with robotic transabdominal TME, robotic transanal surgery, and TAMIS, and TAMIS TME has accrued.
Training and the Learning Curve in Robotic Colorectal Surgery
Training in robotic surgery presents unique challenges because the trainee has to master not only the steps of the operation but also the technologic interface and its nuances and operating remotely from the patient. A stepwise approach is required, ideally within the context of fellowship training:
-
Step 1: High fidelity training (preclinical training), consisting of didactic presentations, video analysis, exposure to port placements, and principles of docking and instrument handling in the dry lab
A porcine or cadaveric lab or workshop expedites this part of the process. A dV simulator, which is available for use with the da Vinci console, provides a virtual reality experience to understand the basics of instrument handling, switching of masters, suturing, and manipulation. It also helps to hone advanced skills as the trainee progresses.
-
Step 2: Bedside assistance
Bedside assistance fulfills two roles: the rapid acquisition of advanced laparoscopic skills and the understanding of port placement, cart position, and arm collisions and troubleshooting thereof. The initial procedure of choice is right hemicolectomy, and after assisting 5–10 cases, the trainee advances to RTME. After 10–15 pelvic dissections, the fellow is well setup for starting his/her console experience.
-
Step 3: Console experience
A dual console is invaluable during training. The mentor breaks each procedure into defined steps and allows the trainee to perform portions of each operation, with a gradual increase in responsibility and difficulty level, till he/she is able to complete the full procedure. Right hemicolectomy is the ideal procedure to start with, and the fellow progresses serially through division of lateral peritoneal attachments, retroperitoneal dissection, mobilization of hepatic flexure, medial to lateral dissection, and finally isolation and division of the ileocolic vessels.
After completing 5–10 cases of right hemicolectomy, progression to sigmoid colon mobilization and vascular ligation and eventually TME occurs. After 10–15 cases as the primary surgeon for low anterior resections, the trainee might be proficient. Once they are able to operate independently with a proctor observing and attesting to the safety and ability of the surgeon to complete the procedure, they could be certified for that robotic operation.
Learning Curve for Robotic Surgery
The learning curve for performing robotic colorectal operations is shorter than for laparoscopy and is crossed after 15–25 cases [15, 44].
Operative time is often used as a surrogate for efficiency but it is imperfect, and as shown by Chen et al. [45], shorter operative time and conversion rates do not always translate into better patient outcomes.
There is a paucity of reports specifically examining the learning curve involving robotic colorectal surgery. Most of the data are from surgeons with prior extensive laparoscopic experience. The study by Jiménez-Rodríguez et al. [46] was the only one to analyze outcome measures of success; it cited a learning curve of 21–23 cases. Akmal et al. [47] on the other hand found no significant learning curve or a discrete numerical cutoff point to quantify as a learning curve plateau over 80 robotic cases. They had already performed more than 100 laparoscopic colorectal procedures, including at least 20 total mesorectal excisions.
These are therefore extremely experienced and skilled laparoscopic surgeons who have reached a plateau with regard to laparoscopic skills, making a direct comparison of robotics with laparoscopy impossible. Their data suggests that laparoscopic skills are transferable to robotics rather than that robotic TME has a short learning curve.
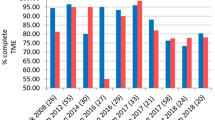
Melich et al. [48•] investigated perioperative outcomes and learning curves for a single surgeon trained in open colorectal surgery who simultaneously trains in laparoscopic and robotic surgery at the beginning of his foray into minimally invasive surgery (MIS).
The data in their manuscript show that initially longer total operative times for robotic surgery improve rapidly and, after 41 cases, become faster than those for laparoscopic surgery. Based on TME operative time curves, robotic TME becomes faster by case number 21 and continues improving beyond. More cases were required to reach operative time proficiency than the 15–30 cases reported by others. The authors of this study concluded that developing both laparoscopic and robotic skills simultaneously provides acceptable outcomes in rectal surgery from the beginning of the training pathway and might be a viable approach to MIS for a surgeon primarily trained in open colorectal surgery.
Irrespective of the approach to training, bedside robotic assistance and operating under a formal mentor is likely to reduce the learning curve.
Conclusions
The robotic platform is an important part of the technologic innovations that facilitate minimally invasive colorectal cancer surgery. While robotic surgery is feasible and safe regarding oncologic outcomes, it has not surpassed laparoscopy in head to head comparison, in a randomized trial. However, there are patient subgroups such as the obese patient with low rectal cancer and the narrow male pelvis in which robotics is potentially better than laparoscopy, though there is as yet no level I evidence. Additionally, extended multivisceral resections [49] and cylindrical extralevator abdominoperineal resection [50] are feasible and oncologically safe when performed robotically. In the field of colon cancer resections, robotics offers the opportunity to provide an essential learning pathway prior to performing complex rectal cancer resections and multivisceral resections. Future developments including the availability of new robotic systems and single port robotic platforms continue to evolve and contribute to progress in this area.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Guillou PJ, Quirke P, Thorpe H, et al. Short-term endpoints of conventional versus laparoscopic assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet. 2005;365:1718–26.
Jayne DG, Thorpe HC, Copeland J, Quirke P, Brown JM, Guillou PJ. Five-year follow-up of the Medical Research Council CLASICC trial of laparoscopically assisted versus open surgery for colorectal cancer. Br J Surg. 2010;97:1638–45.
Veldkamp R, Kuhry E, Hop WC, et al. Laparoscopic surgery versus open surgery for colon cancer. Lancet Oncol. 2005;6(7):477–84.
Fleshman J, Sargent DJ, Green E, et al. Laparoscopic colectomy for cancer is not inferior to open surgery based on 5-year data from the COST Study Group trial. Ann Surg. 2007;246:655–62.
Bonjer HJ, Deijen CL, Abis GA, et al. A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med. 2015;372:1324–32.
Kayano H, Okuda J, Tanaka K, Kondo K, Tanigawa N. Evaluation of the learning curve in laparoscopic low anterior resection for rectal cancer. Surg Endosc. 2011;25:2972–9.
Herron DM, Marohn M (2007) A consensus document on robotic surgery: prepared by the SAGES-MIRA Robotic Surgery Consensus Group. Available at: http://www.sages.org/publication/id/ROBOT/. Accessed 16 Oct 2016.
Weber PA, Merola S, Wasielewski A, Wasielewski GH. Telerobotic-assisted laparoscopic right and sigmoid colectomies for benign disease. Dis Colon Rectum. 2002;45:1689–94.
Hashizume M, Shimada M, Tomikawa M, Ikeda Y, Takahashi I, Abe R, et al. Early experiences of endoscopic procedures in general surgery assisted by a computer-enhanced surgical system. Surg Endosc. 2002;16:1187–91.
D’Annibale A, Morpurgo E, Fiscon V, Trevisan P, Sovernigo G, Orsini C, et al. Robotic and laparoscopic surgery for treatment of colorectal diseases. Dis Colon Rectum. 2004;47:2162–8.
Rawlings AL, Woodland JH, Crawford DL. Telerobotic surgery for right and sigmoid colectomies: 30 consecutive cases. Surg Endosc. 2006;20:1713–8.
Pigazzi A, Ellenhorn JD, Ballantyne GH, Paz IB. Robotic-assisted laparoscopic low anterior resection with total mesorectal excision for rectal cancer. Surg Endosc. 2006;20:1521–5.
de Souza AL, Prasad LM, Marecik SJ, et al. Total mesorectal excision for rectal cancer: the potential advantage of robotic assistance. Dis Colon Rectum. 2010;53:1611–7.
Baik SH, Kwon HY, Kim JS, Hur H, Sohn SK, Cho CH, et al. Robotic versus laparoscopic low anterior resection of rectal cancer: short-term outcome of a prospective comparative study. Ann Surg Oncol. 2009;16:1480–7.
Choi DJ, Kim SH, Lee PJ, Kim J, Woo SU. Single-stage totally robotic dissection for rectal cancer surgery: technique and short-term outcome in 50 consecutive patients. Dis Colon Rectum. 2009;52:1824–30.
Baik SH, Kim NK, Lim DR, Hur H, Min BS, Lee KY. Oncologic outcomes and perioperative clinicopathologic results after robot-assisted tumor-specific mesorectal excision for rectal cancer. Ann Surg Oncol. 2013;20:2625–32.
Park JS, Choi GS, Park SY, Kim HJ, Ryuk JP. Randomized clinical trial of robot-assisted versus standard laparoscopic right colectomy. Br J Surg. 2012;99:1219–26. doi:10.1002/bjs.8841.
Baek JH, McKenzie S, Garcia-Aguilar J, Pigazzi A. Oncologic outcomes of robotic-assisted total mesorectal excision for the treatment of rectal cancer. Ann Surg. 2010;251:882–6.
de Souza AL, Prasad LM, Park JJ, Marecik SJ, Blumetti J, Abcarian H. Robotic assistance in right hemicolectomy: is there a role? Dis Colon Rectum. 2010;53:1000–6.
Hohenberger W, Weber K, Matzel K, et al. Standardized surgery for colonic cancer: complete mesocolic excision and central ligation—technical notes and outcome. Colorectal Dis. 2009;11:354–64.
Bertelsen CA, Neuenschwander AU, Jansen JE, et al. Disease-free survival after complete mesocolic excision compared with conventional colon cancer surgery: a retrospective, population- based study. Lancet Oncol. 2015;16:161–8.
Lim DR, Min BS, Kim MS, et al. Robotic versus laparoscopic anterior resection of sigmoid colon cancer: comparative study of long-term oncologic outcomes. Surg Endosc. 2013;27:1379–85.
Lim MS, Melich G, Min BS. Robotic single-incision anterior resection for sigmoid colon cancer: access port creation and operative technique. Surg Endosc. 2013;27:1021.
Park IJ, You YN, Schlette E, et al. Reverse-hybrid robotic mesorectal excision for rectal cancer. Dis Colon Rectum. 2012;55:228–33.
Pai A, Marecik SJ, Park JJ, Melich G, Sulo S, Prasad LM. Oncologic and clinicopathologic outcomes of robot-assisted total mesorectal excision for rectal cancer. Dis Colon Rectum. 2015;58:659–67.
Hellan M, Anderson C, Ellenhorn JD, Paz B, Pigazzi A. Short-term outcomes after robotic-assisted total mesorectal excision for rectal cancer. Ann Surg Oncol. 2007;14:3168–73.
Pigazzi A, Luca F, Patriti A, Valvo M, Ceccarelli G, Casciola L, et al. Multicentric study on robotic tumor-specific mesorectal excision for the treatment of rectal cancer. Ann Surg Oncol. 2010;17:1614–20.
Rottoli M, Bona S, Rosati R, et al. Laparoscopic rectal resection for cancer: effects of conversion on short-term outcome and survival. Ann Surg Oncol. 2009;16:1279–86.
Agha A, Fürst A, Iesalnieks I, et al. Conversion rate in 300 laparoscopic rectal resections and its influence on morbidity and oncological outcome. Int J Colorectal Dis. 2008;23:409–17.
Yamamoto S, Fukunaga M, Miyajima N, et al. Impact of conversion on surgical outcomes after laparoscopic operation for rectal carcinoma: a retrospective study of 1073 patients. J Am Coll Surg. 2009;208:383–9.
Trastulli S, Farinella E, Cirocchi R, Cavaliere D, Avenia N, Sciannameo F, et al. Robotic resection compared with laparoscopic rectal resection for cancer: systematic review and meta-analysis of short-term outcome. Colorectal Dis. 2012;14:e134–56.
•• Hara M, Sng K, Yoo BE, Shin JW, Lee DW, Kim SH. Robotic-assisted surgery for rectal adenocarcinoma: short-term and midterm outcomes from 200 consecutive cases at a single institution. Dis Colon Rectum. 2014;57:570–7. The first study reporting 5-year data for recurrence free, disease free, and overall survival after robotic total mesorectal excision in a large series of 200 patients.
•• Park EJ, Cho MS, Baek SJ, Hur H, Min BS, Baik SH, et al. Long-term oncologic outcomes of robotic low anterior resection for rectal cancer: a comparative study with laparoscopic surgery. Ann Surg. 2015;261:129–37. One of only 2 studies reporting 5-year data for recurrence free, disease free, and overall survival after robotic total mesorectal excision.
•• Xiong B, Ma L, Zhang C, Cheng Y. Robotic versus laparoscopic total mesorectal excision for rectal cancer: a meta-analysis. J Surg Res. 2014;188:404–14. An important meta-analysis showing better outcomes with regard to conversion rates and margin positivity in robotic TME in comparison to laparoscopic TME.
Kim JY, Kim NK, Lee KY, Hur H, Min BS, Kim JH. A comparative study of voiding and sexual function after total mesorectal excision with autonomic nerve preservation for rectal cancer: laparoscopic versus robotic surgery. Ann Surg Oncol. 2012;19:2485–93.
Luca F, Valvo M, Ghezzi TL, Zuccaro M, Cenciarelli S, Trovato C, et al. Impact of robotic surgery on sexual and urinary functions after fully robotic nerve-sparing total mesorectal excision for rectal cancer. Ann Surg. 2013;257:672–8.
•• Collinson FJ, Jayne DG, Pigazzi A, Tsang C, Barrie JM, Edlin R, et al. An international, multicentre, prospective, randomised, controlled, unblinded, parallel-group trial of robotic-assisted versus standard laparoscopic surgery for the curative treatment of rectal cancer. Int J Colorectal Dis. 2012;27:233–41. The major RCT comparing robotic and laparoscopic rectal cancer resections that did not show a difference in outcomes between the two modalities.
•• Fleshman J, Branda M, Sargent DJ, et al. Effect of laparoscopic-assisted resection vs open resection of stage II or III rectal cancer on pathologic outcomes: the ACOSOG Z6051 randomized clinical trial. JAMA. 2015;314:1346–55. A landmark RCT that did not demonstrate non-inferiority of laparoscopic total mesorectal excision as compared to open TME.
•• Stevenson ARL, Solomon MJ, Lumley JW, et al. Effect of laparoscopic-assisted resection vs open resection on pathological outcomes in rectal cancer: the ALaCaRT randomized clinical trial. JAMA. 2015;314:1356–63. A well designed RCT that failed to show the non-inferiority of laparoscopy when compared to open surgery for rectal cancer.
Bae SU, Jeong WK, Baek SK. Robotic anterior resection for sigmoid colon cancer using reduced port access. Dis Colon Rectum. 2016;59:245–6.
Deijen CL, Velthuis S, Tsai A, et al. COLOR III: a multicentre randomised clinical trial comparing transanal TME versus laparoscopic TME for mid and low rectal cancer. Surg Endosc. 2016;30:3210–5.
Atallah S, Parra-Davilla E, DeBeche-Adams T, Albert M, Larach S. Excision of a rectal neoplasm using robotic transanal surgery (RTS): a description of the technique. Tech Coloproctol. 2012;16:389–92.
Atallah S, Nassif G, Polavarapu H, DeBeche-Adams T, Ouyang J, Albert M, et al. Robotic-assisted transanal surgery for total mesorectal excision (RATS-TME): a description of a novel surgical approach with video demonstration. Tech Coloproctol. 2013;17:441–7.
Bokhari MB, Patel CB, Ramos-Valadez DI, Ragupathi M, Haas EM. Learning curve for robotic-assisted laparoscopic colorectal surgery. Surg Endosc. 2011;25:855–60.
Chen G, Liu Z, Han P, Li J, Cui B. The learning curve for the laparoscopic approach for colorectal cancer: a single institution’s experience. J Laparoendosc Adv Surg Tech. 2013;23:17–21.
Jiménez-Rodríguez RM, Rubio-Dorado-Manzanares M, Díaz-Pavón JM, et al. Learning curve in robotic rectal cancer surgery: current state of affairs. Int J Colorectal Dis. 2016. doi:10.1007/s00384-016-2660-0.
Akmal Y, Baek J, McKenzie S, Garcia-Aguilar J, Pigazzi A. Robot-assisted total mesorectal excision: is there a learning curve? Surg Endosc. 2012;26:2471–6.
• Melich G, Hong YK, Kim J, et al. Simultaneous development of laparoscopy and robotics provides acceptable perioperative outcomes and shows robotics to have a faster learning curve and to be overall faster in rectal cancer surgery: analysis of novice MIS surgeon learning curves. Surg Endosc. 2015;29:558–68. A novel study looking at the learning curves for laparoscopic and robotic rectal cancer surgery when developed in parallel for an individual surgeon.
Shin US, Nancy You Y, Nguyen AT, et al. Oncologic outcomes of extended robotic resection for rectal cancer. Ann Surg Oncol. 2016;23:2249–57.
Marecik SJ, Zawadzki M, de Souza AL, Park JJ, Abcarian H, Prasad LM. Robotic cylindrical abdominoperineal resection with transabdominal levator transection. Dis Colon Rectum. 2011;54:1320–5.
Acknowledgments
This article is dedicated in memory of Dr. Leela M. Prasad. Our teacher and role model who always was first to try something new and inspired those around him to never stop learning.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Ajit Pai, George Melich, Slawomir J. Marecik, John J. Park, and Leela M. Prasad declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Surgery and Surgical Innovations in Colorectal Cancer
Leela M. Prasad is deceased.
Rights and permissions
About this article
Cite this article
Pai, A., Melich, G., Marecik, S.J. et al. Robotic Surgery for Colon and Rectal Cancer: Current Status, Recent Advances, and Future Directions. Curr Colorectal Cancer Rep 13, 37–44 (2017). https://doi.org/10.1007/s11888-017-0348-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11888-017-0348-7