Abstract
Acute heart failure is associated with substantial morbidity and mortality. Goals of treatment are decongestion, correction of hemodynamic abnormalities, symptom relief, and reducing long-term morbidity and mortality. Loop diuretics are a first-line agent for treatment of volume overload, with ultrafiltration reserved for those who do not respond to pharmacologic therapy. In patients with normal or elevated blood pressure, vasodilators are used to correct hemodynamics and reverse central volume redistribution, although no currently available agent has been shown to improve outcomes. Intravenous inotropes and inodilators are associated with frequent adverse effects and are reserved for patients with hypotension and evidence of inadequate perfusion. Novel drugs designed to maximize hemodynamic benefits while minimizing adverse effects are under investigation, with several agents showing promise in clinical studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute heart failure (AHF) is a major public health challenge that is associated with over 1.1 million hospitalizations annually in the United States [1]. Hospitalization for AHF accounts for the majority of heart failure-related spending, and the number of patients presenting with heart failure is expected to increase as the population ages. While significant progress has been made in the management of chronic heart failure, no currently available therapy has been shown to improve long-term outcomes in patients with AHF. Not surprisingly, the prognosis for patients hospitalized for AHF is poor; in-hospital mortality is approximately 4 % [2], and 25-35 % of patients die within one year of hospitalization [3, 4]. Development of evidence-based therapies to improve outcomes is needed. In this article, we review the currently available therapies for AHF, focusing on recent advances.
Goals of Therapy
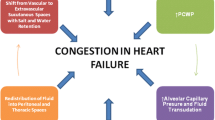
Short-term goals are to relieve symptoms, treat volume overload, and correct hemodynamic abnormalities. More than 80 % of AHF patients present with a primary complaint of dyspnea [5], and this has been a primary target in AHF clinical trials. Fluid overload and congestion account for approximately 90 % of heart failure related hospitalizations [2], but therapies should be directed to correcting the hemodynamic abnormalities specific to each patient. These hemodynamic goals may include reversing central volume redistribution, reducing cardiac filling pressures, decreasing afterload, and increasing cardiac output.
Long-term goals of AHF management focus on reducing mortality and re-hospitalization. Developing therapies that improve these outcomes has proven exceedingly difficult. Multiple agents have looked promising in phase II trials, but ultimately demonstrate little efficacy or unacceptable adverse effects when evaluated in larger phase III trials. The reasons for this are subject to debate [6], and efforts to improve the identification and evaluation of novel therapies are ongoing.
Management of Volume Overload
Diuretics
Loop diuretics are a cornerstone of therapy for volume overload in patients with AHF. To maximize bioavailability and rapidity of onset, loop diuretics are generally given intravenously. Several factors may increase the diuretic dosage needed to attain adequate diuresis in patients with AHF, including renal insufficiency and shifting of the dose–response curve [7]. Loop diuretics are most commonly administered as an intravenous bolus; however, there are theoretical benefits of a continuous diuretic infusion including less rebound sodium retention and improved diuresis.
Using a randomized, double-blind, 2 × 2 factorial design, the DOSE trial [8••] randomized 308 patients to treatment with IV furosemide using either twice-daily bolus dosing or a continuous infusion and to either a low (equivalent to the numerical value of the oral outpatient dose) or high dose (2.5 times the oral dose) strategy. There was no significant difference in either of the co-primary endpoints of global assessment of symptoms or change in creatinine at 72 hours with administration by bolus vs. infusion or with the low- vs. high-dose strategy. The high-dose strategy was associated with greater relief of dyspnea and net fluid loss at 72 hours, although more patients in the high-dose group had an increase in creatinine >0.3 mg/dL. The significance of this finding is unclear as the trial was not appropriately powered for long-term clinical outcomes, although there were no apparent differences in hospital length of stay or days alive out of the hospital. Overall, there were no differences in results between the continuous infusion and intermittent bolus strategies in the clinical trial setting of DOSE, suggesting that whichever approach is most likely to reliably produce the desired diuresis in the particular local clinical setting should be used. Interestingly, a secondary analysis of DOSE has suggested that patients with higher outpatient oral diuretic doses (≥120 mg furosemide equivalent daily) may have better responses to an intermittent bolus intravenous diuretic regimen [9].
Ultrafiltration
The development of venovenous ultrafiltration has generated significant interest in its use as an alternative to loop diuretics. The UNLOAD trial randomized 200 patients with AHF and hypervolemia to ultrafiltration or IV diuretics within 24 hours of hospitalization [10]. Patients in the ultrafiltration arm were treated exclusively with ultrafiltration for the first 48 hours. Patients in the diuretic arm were required to receive a dose of diuretic equal to at least twice their usual daily dose of oral diuretic for the first 48 hours. The ultrafiltration group showed significant improvement in one of the primary outcomes, weight loss at 48 hours (5.0 ± 3.1 kg in the UF group vs. 3.1 ± 3.5 g in the IV diuretic group, p = 0.001). The trial did not meet the second primary outcome of dyspnea score at 48 hours. Patients randomized to ultrafiltration experienced less hypokalemia, greater net fluid loss at 48 hours, fewer HF-related hospitalizations at 90 days, and fewer unscheduled office and emergency department visits within 90 days. There was no significant difference in the length of hospitalization or frequency of hypotension [10].
The CARRESS-HF trial randomized 188 patients with AHF, ongoing congestion and worsened renal function to ultrafiltration or stepped pharmacologic therapy within 10 days of hospitalization [11••]. The primary endpoint was the bivariate change from baseline in the serum creatinine and body weight, assessed 96 hours after randomization. Ultrafiltration was inferior to pharmacologic therapy, due to an increase in the serum creatinine level among the group randomized to ultrafiltration (mean change of +0.23 ± 0.7 mg/dL in the ultrafiltration group vs. -0.04 ± 0.53 mg/dL in the pharmacologic therapy group, p = 0.003). There was no significant difference in weight loss (5.5 ± 5.1 kg in the pharmacologic therapy group vs. 5.7 ± 3.9 kg in the ultrafiltration group, p = 0.58). There were no significant differences in mortality or rehospitalization at 60 days. Patients in the ultrafiltration arm had significantly more serious adverse events over 60 days of follow-up (72 % vs. 57 %, p = 0.03), including higher rates of renal failure, bleeding complications, and intravenous catheter-related complications.
Several important differences between UNLOAD and CARRESS-HF need to be considered. CARRESS-HF specifically targeted patients who developed worsening renal failure during their hospitalization using ultrafiltration as a rescue therapy, whereas UNLOAD enrolled patients within 24 hours of admission regardless of serum creatinine. Additionally, treatment algorithms used in both the pharmacologic and ultrafiltration arms differed significantly. Subjects in the pharmacologic therapy arm of CARRESS-HF were treated according to a strict algorithm that called for loop diuretics titrated to maintain a urine output of 3 to 5 liters per day. Subjects who failed to meet urine output goals with loop diuretics alone were then given thiazide diuretics, and finally IV vasodilators and/or inotropes depending on clinical characteristics. Pharmacologic therapy in UNLOAD, on the other hand, only required clinicians to administer IV loop diuretics at a dose at least twice the pre-hospitalization oral dose, with further titration at the clinician’s discretion. In the ultrafiltration arm of CARRESS-HF, the UF rate was fixed at 200 mL/hour, whereas UNLOAD allowed for titration of rates up to 500 mL/hour.
The findings from UNLOAD and CARRESS-HF can be interpreted in several ways. It is reasonable to conclude that ultrafiltration is not indicated for treatment of worsening renal function in AHF patients. Alternatively, it is possible that patients in the medical therapy arm of UNLOAD simply were not diuresed aggressively enough, or that subjects in the ultrafiltration arm of CARRESS-HF did not have fluid removed at a high enough rate. A larger trial of early ultrafiltration is currently underway (AVOID-HF; NCT01474200).
Guideline Recommendations Regarding Management of Volume Overload
The 2010 Heart Failure Society of America (HFSA) Comprehensive Heart Failure Practice Guideline recommends that patients with AHF and volume overload be treated with loop diuretics (LOE B) at doses sufficient to achieve optimal volume status without inducing excessively rapid reduction in extravascular volume or electrolytes [12••]. Ultrafiltration can be considered in lieu of diuretics (LOE B). When congestion fails to improve with diuretics further options include re-evaluating the presence of congestion, sodium/fluid restriction, increasing the dose of a loop diuretic, switching to a continuous infusion of a loop diuretic, adding a second class of diuretic, or considering ultrafiltration (LOE C) [12••]. The European Society of Cardiology (ESC) Guidelines for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 similarly recommend that loop diuretics be given as first-line therapy, and reserve ultrafiltration for those unresponsive or resistant to diuretics [13••]. Both the HFSA and ESC guidelines were released before the publication of CARRESS-HF.
Vasodilators
Intravenous vasodilators reduce preload and afterload and increase stroke volume. They have been used in the management of acute heart failure for decades, though their efficacy has not been rigorously demonstrated in clinical trials. Hypotension is the most frequent adverse effect of vasodilators, and close hemodynamic monitoring is generally advised. Nitroglycerin and sodium nitroprusside (SNP) are the most commonly used vasodilators in the management of AHF.
The Vasodilation in the Management of Acute CHF (VMAC) study is the only large, randomized trial to evaluate the efficacy of IV nitroglycerin in AHF [14]. Within the trial, 285 patients with dyspnea at rest due to heart failure were randomized to IV nitroglycerin or standard care. Although there was a trend toward reduced pulmonary capillary wedge pressure (PCWP) in patients receiving nitroglycerin, there was no difference in the co-primary endpoint of dyspnea. This relative lack of efficacy may have been due to the relatively low doses of nitroglycerin (mean 42 ± 61 μg/min). A single center subgroup analysis of 27 patients demonstrated that patients who received a higher dose of nitroglycerin (mean 160 μg/min) had a larger and significant reduction in PCWP, although tachyphylaxis developed within 24 hours [15].
An early study of 18 patients hospitalized for heart failure found that infusion of SNP resulted in a 15 mmHg decrease in PCWP [16]. A larger, retrospective study of 175 patients admitted for AHF with reduced cardiac output and elevated filling pressures found treatment with SNP (titrated to a target MAP of 65 to 70 mmHg) was associated with reduced all-cause mortality (OR 0.48, p = 0.005) [17]. There were no significant differences with respect to rehospitalization or cardiac transplant.
Patients with elevated left ventricular (LV) filling pressures following acute myocardial infarction (AMI) require special consideration with regard to SNP. One randomized trial of 328 patients with acute MI (but no requirement for heart failure) was stopped early due to beneficial effects of SNP on mortality, based on only 23 death events [18]. Another randomized trial of 812 men with acute MI and elevated left ventricular end diastolic pressure found no difference in mortality [19]. However, in a post-hoc analysis, SNP was associated with increased mortality compared to placebo when started within 9 hours of the onset of pain, but decreased mortality when started later. In patients with AMI, use of SNP should probably be reserved for those with persistently elevated filling pressures.
Nesiritide
Nesiritide is a recombinant form of human B-type natriuretic peptide (BNP) with venous, arterial, and coronary vasodilatory properties. The VMAC study was the first large-scale trial to evaluate nesiritide in AHF, randomizing 489 patients to intravenous nesiritide, nitroglycerin, or placebo [14]. At 3 and 24 hours, patients treated with nesiritide had significantly larger decreases in PCWP compared to patients receiving nitroglycerin or placebo. At 3 hours, dyspnea was significantly improved compared to patients receiving placebo, but not nitroglycerin. Nesiritide was approved by the FDA in 2001, however shortly after approval, pooled analyses suggested an increased risk of death and worsening renal function in patients treated with nesiritide [20, 21]. An expert panel recommended that a large multicenter trial be performed to assess the efficacy and safety of nesiritide.
To address these concerns, the ASCEND-HF trial randomized 7141 patients with AHF to nesiritide or placebo for 24 to 168 hours [22••]. At 30 days, there was no difference between patients receiving nesiritide and those receiving placebo with regard to the composite endpoint of death or rehospitalization for heart failure. Patients randomized to nesiritide more frequently reported moderately or markedly improved dyspnea at 6 hours, however this did not reach the prespecified level for significance. Use of nesiritide had no impact on worsening renal function, but was associated with an increase in the rate of hypotension.
Guideline Recommendations Regarding the Use of Vasodilators
The 2010 HFSA Guidelines, published before ASCEND-HF was released, recommend IV vasodilators (nitroglycerin or nitroprusside) in addition to diuretics for rapid relief of congestion in patients with pulmonary edema or severe hypertension (strength of evidence = C) [12••]. In the absence of hypotension, intravenous vasodilators (nitroglycerin, nitroprusside, or nesiritide) may be considered in addition to diuretics for rapid treatment of congestion, with close hemodynamic monitoring and reduction or discontinuation if hypotension develops (Strength of evidence = B).
The 2012 ESC Heart Failure Guidelines recommend a nitrate infusion be considered in patients with pulmonary edema and SBP > 110 mmHg to reduce PCWP and systemic vascular resistance (Class IIa, LOE B) [13••].
Inotropes/Inodilators
Inotropic agents have been used in the management of acute heart failure for decades despite the fact that none have been shown to improve outcomes. Many of the currently available agents have actually been associated with worse outcomes when given routinely to patients with AHF [23–25]. Common side effects include tachyarrhythmias and hypotension, and inotropes are currently best reserved for patients with low cardiac output with poor end-organ perfusion.
The most frequently used inotropes are milrinone, dobutamine, and dopamine. A large randomized trial of 949 patients comparing milrinone to placebo found higher rates of sustained hypotension and atrial and ventricular arrhythmias in the milrinone group with no difference in days hospitalized for cardiovascular causes [24]. A secondary analysis suggested a significant interaction between the etiology of the heart failure and treatment effect, predominantly driven by increased in-hospital mortality and a trend toward increased 60-day mortality in ischemic heart failure patients treated with milrinone [26].
The DAD-HF trial randomized 60 patients with AHF to high-dose furosemide or low-dose furosemide combined with low-dose dopamine (5 μg/kg/min) for 8 hours [27]. Although the dopamine group did have fewer episodes of worsening renal function, there were no significant differences in total diuresis, change in dyspnea score, length of stay, 60-day mortality or rehospitalization rates. A larger study of dopamine in AHF was recently completed (DAD-HF II; NCT01060293) and the ROSE-AHF study (Renal Optimization Strategies Evaluation in Acute Heart Failure; NCT01132846) is ongoing.
Levosimendan
Levosimendan is a calcium sensitizer that increases inotropy by binding cardiac troponin C in a calcium-dependent manner, increasing the affinity of troponin C for calcium. Levosimendan also facilitates opening of ATP-dependent potassium channels, resulting in vasodilation and has also been noted to have phosphodiesterase inhibitor activity. In early clinical studies levosimendan increased cardiac output, reduced cardiac filling pressures, and was associated with reduced symptoms and hospitalization [28, 29]. The REVIVE-II trial randomized 600 patients to levosimendan or placebo. Levosimendan was associated with improvement in symptoms at 5 days, although there was also an increase in early mortality [30]. An economic analysis of REVIVE-II found that patients treated with levosimendan had shorter hospital length of stay and lower hospital costs [31]. The SURVIVE trial randomized patients with AHF requiring inotropes to treatment with levosimendan or dobutamine [32]. There were no significant differences with regard to the primary endpoint of all-cause mortality at 180 days (HR 0.91, 95 % CI 0.74-1.13, p = 0.4) or the secondary endpoints of all-cause mortality at 31 days, days alive and out of hospital, patient assessment of dyspnea, and cardiovascular mortality at 180 days. Levosimendan acts independently of beta adrenoreceptors, and may prove superior to beta agonists in patients treated with beta-blockers at baseline. A substudy of SURVIVE found that in patients on beta-blocker therapy at admission levosimendan was associated with significantly lower mortality compared to dobutamine [33]. Levosimendan is not currently available in the United States.
Guideline Recommendations Regarding the Use of Inotropes
The 2010 HFSA Guidelines suggest that intravenous inotropes (milrinone or dobutamine) may be considered to improve symptoms and end-organ function in patients with advanced heart failure characterized by LV dilation, reduced EF, and inadequate peripheral perfusion. These agents should particularly be considered in patients with marginal blood pressure, symptomatic hypotension despite adequate filling pressures, or in patients who are intolerant of or unresponsive to IV vasodilators (Strength of evidence C). Inotropes may also be considered in volume-overloaded patients who are unresponsive to IV diuretics or in whom renal function worsens following administration of IV diuretics (Strength of evidence C). IV vasodilators should be given preference over inotropes when possible. Inotropes should only be done in the setting of continuous cardiac monitoring and frequent or continuous blood pressure monitoring (Strength of evidence C).
Vasopressin Receptor Antagonists
Levels of arginine vasopressin are inappropriately elevated in both acute and chronic heart failure, and contribute to fluid retention and hyponatremia. Tolvaptan is an oral, selective vasopressin V2-receptor antagonist that has been shown in small trials to decrease fluid retention and correct hyponatremia in heart failure patients with hyponatremia [34].
The EVEREST trial randomized 4133 patients within 48 hours of admission for heart failure to oral tolvaptan 30 mg daily vs. placebo for a minimum of 60 days. There were small but significant improvements in edema, body weight, and patient-assessed dyspnea at day 1. Additionally, patients with hyponatremia (<134 mEq/L) who received tolvaptan showed significant improvement in serum sodium [35]. During a mean follow-up of 9.9 months there was no significant difference in death or the composite outcome of cardiovascular mortality or hospitalization for heart failure [36]. Vasopressin antagonists (e.g., tolvaptan, conivaptan) may be considered for short-term treatment of hyponatremia in patients with AHF and volume overload who have persistent hyponatremia at risk for or having active cognitive symptoms, refractory to standard of care.
Investigational Therapies for AHF
Many therapies have looked promising in early studies but failed to demonstrate benefit in larger trials. Rolofylline, for example, is an adenosine A1-receptor antagonist which showed improved dyspnea and decreased rates of renal dysfunction in a small phase II study [37] but had no beneficial effect on outcomes in the larger, phase III PROTECT trial [38] and was associated with increased seizures and strokes [39]. Tezosentan is a short-acting, intravenous endothelin dual (A/B) receptor antagonist that causes vasodilation, increased cardiac index and reduced PCWP in patients with AHF. Two large, randomized, double-blind trials of tezosentan showed no effect on dyspnea or mortality [40]. Another novel vasodilator, cinaciguat, caused impressive changes in hemodynamics in early studies, however a group of three larger randomized trials evaluating cinaciguat in patients with AHF was recently terminated early due to an excess of hypotension in subjects receiving cinaciguat with no significant improvement in dyspnea or cardiac index [41]. Novel agents that currently show promise in the management of AHF are reviewed below and summarized in Table 1.
Omecamtiv Mecarbil
Cardiac myosin activators represent a new mechanistic class of agents designed to increase myocardial contractility. These agents increase the transition rate from the weakly bound to the strongly bound state necessary for initiation of a force-generating power stroke. Unlike current inotropes, they increase the systolic ejection time without altering the rate of LV pressure development, resulting in increased stroke volume and cardiac output [42].
Omecamtiv mecarbil is the first agent of this class to undergo testing in man. In healthy volunteers, administration of omecamtiv mecarbil produced dose-dependent increases in systolic ejection time, fractional shortening, and ejection fraction [43•]. In a subsequent double-blind, placebo-controlled, crossover, dose-ranging phase II trial, omecamtiv mecarbil was administered intravenously to 45 patients with heart failure and LV systolic dysfunction [44•]. Significant, concentration-dependent increases in LV systolic ejection time, stroke volume and ejection fraction were observed, along with decreases in left ventricular end-systolic and end-diastolic volumes. The medication was well-tolerated over a broad range of plasma concentrations, though cardiac ischemia was observed at very high plasma concentrations in two patients. A phase IIb study of omecamtiv mecarbil in patients with acute heart failure is nearing completion (ATOMIC-AHF; NCT01300013).
Serelaxin
Serelaxin is the recombinant form of human relaxin-2, a naturally occurring peptide that modulates multiple cardiovascular pathways. It binds its G-protein coupled receptor, RXFP-1, activating the endothelin B receptor and other signaling pathways, resulting in multiple effects including increased cGMP production and nitric oxide release. This increases vasodilation and renal blood flow among other actions. In the 234-patient dose-finding Pre-RELAX-AHF study, serelaxin treatment demonstrated trends in improving patient signs and symptoms of heart failure, as well as clinical outcomes, including survival [45]. The Phase III RELAX-AHF trial randomized 1161 patients within 16 hours of presentation with AHF to standard care plus serelaxin (30 μg/kg per day for up to 48 hours) or placebo [46••]. Enrollment criteria were dyspnea at rest or with minimum exertion, pulmonary congestion on chest radiograph, elevated natriuretic peptides, mild to moderate renal dysfunction (estimated glomerular filtration rate 30–75 mL/min per 1.73 m2), systolic blood pressure ≥ 125 mmHg, and treatment with at least 40 mg of IV furosemide or its equivalent prior to screening. Treatment with serelaxin resulted in a significant improvement in the change in patient-reported dyspnea, measured as the area under the curve of a visual analogue scale (VAS AUC) from baseline to day 5 (448 mm x h, 95 % CI 120–775; p = 0.007), but not when measured by Likert scale over 24 hours. The serelaxin-treated group also showed significant improvements in signs and symptoms of heart failure, fewer patients with worsening heart failure, and shorter hospital length of stay, but no effect on either of the two secondary efficacy endpoints (days alive and out of the hospital at 60 days; and cardiovascular death or readmission for heart failure or renal failure within 60 days), due to lack of an effect on readmissions. Treatment with serelaxin reduced both cardiovascular death (HR 0.63, 95 % CI 0.41–0.96; p = 0.028) and all-cause mortality (HR 0.63, 95 % CI 0.43–0.93 p = 0.019) at 180 days. A secondary analysis found that patients treated with serelaxin had significant improvements in markers of cardiac, renal, and hepatic injury, and improvements in these markers were associated with decreased mortality at 180 days [47]. Taken together, these findings suggest that serelaxin not only improved dyspnea and decreased worsening heart failure, but may also have reduced mortality by preventing end-organ damage during hospitalization for AHF. While these findings have the potential to be paradigm-shifting, it is important to remember RELAX-AHF was not designed or powered to be a mortality trial. RELAX-AHF also selected a specific subgroup of patients with AHF, most notably those with a systolic blood pressure >125 mmHg and other trial entry criteria, and the findings may not be generalizable to the entire AHF population.
Istaroxime
Istaroxime is a novel intravenous agent with both inotropic and lusitropic effects. It inhibits sodium-potassium ATPase activity while stimulating sarcoplasmic reticulum calcium adenosine triphosphatase isoform 2a (SERCA2a). This causes cytosolic calcium accumulation during systole (inotropic response) and rapid sequestration of calcium during diastole (lusitropic response).
The HORIZON-HF study randomized 120 patients with AHF and reduced systolic function to istaroxime or placebo [48]. Subjects receiving istaroxime showed significant, rapid improvement in the primary endpoint of PCWP at all doses studied for up to 6 hours. Istaroxime also significantly decreased heart rate, increased systolic blood pressure, and moderately improved echocardiographic measures of LV diastolic function.
Natriuretic Peptides
Multiple different natriuretic peptides continue to be developed and investigated for the treatment of AHF, including naturally-occurring and alternatively-spliced [49] peptides and chimeric designer peptides. Urodilatin, a modified version of pro-ANP, is a 32-amino-acid hormone, synthesized and secreted from the distal tubules of the kidney, that regulates renal sodium absorption and water homeostasis via binding to NPR1 receptors and increasing intracellular cGMP levels. In contrast to ANP and BNP, urodilatin is effective in distal renal tubules and was considered to have greater renal effects with less pronounced peripheral vasodilation. The effects of ularitide, synthetically produced urodilatin, have been evaluated in two studies. An ascending dose study (SIRIUS-I) tested 24-hour ularitide infusions (7.5, 15, and 30 ng/kg/min) compared to placebo in 24 patients with AHF [50]. After 6 hours, ularitide significantly decreased PCWP and tended to improve dyspnea. The subsequent SIRIUS-II study assessed the effects of the same doses of ularitide in 221 patients with symptomatic AHF [51]. Ularitide demonstrated a significant reduction of PCWP in all three dose groups, with decreased SVR and increased cardiac index at higher doses. These hemodynamic benefits were associated with improvements in dyspnea. As with many vasodilator programs, decreased blood pressure was the main adverse event with 8-16 % of ularitide-treated patients experiencing a significant blood pressure decrease and approximately 6 % experiencing symptomatic hypotension. The TRUE-AHF trial (NCT01661634) is currently enrolling patients with symptomatic AHF with a target sample size of 2116 randomized to a 48-hour infusion of either ularitide (15 ng/kg/min) or placebo.
Cenderitide (CD-NP) is a chimeric natriuretic peptide that combines C-type natriuretic peptide (CNP) and Dendroaspis NP (DNP) [52]. CNP is a selective venodilator, and thereby reduces the risk of hypotension observed with endogenous BNP. DNP is a potent natriuretic with additional diuretic and aldosterone-inhibiting properties. This designer peptide aims to provide the beneficial effects of predominantly venous vasodilation and natriuresis without the risk of hypotension. A small, open-label, study of CD-NP in patients with NYHA class II/III heart failure with reduced EF showed similar diuretic effects compared to furosemide, but with the additional effect of significantly improved renal function [53]. Larger trials are investigating potential therapeutic applications in outpatients with subacute or chronic heart failure.
Other Neurohormonal Agents
The success of the neurohormonal antagonists in chronic heart failure has encouraged application of this concept to AHF, although tempered by the experience of CONSENSUS II, where early administration of intravenous enalaprilat in patients with acute myocardial infarction caused significant hypotension and a trend toward worse outcomes [54]. Aliskiren is a direct renin inhibitor, acting at the root of the renin-angiotensin-aldosterone system (RAAS). In a study of 16 patients with AHF, 7 days of aliskiren treatment resulted in significant decreases in SVR and a trend toward increased cardiac index, but no difference in PCWP [55]. The ASTRONAUT trial is evaluating the 6-month efficacy and safety of chronic oral aliskiren therapy in addition to standard therapy, on post-discharge mortality and re-hospitalization rates when initiated early after AHF hospital admission and before discharge [56]. While this study is not per se an investigation of an AHF therapy, it is addressing the crucial “vulnerable” post-discharge period.
Conclusion
Improving care for patients with AHF poses a significant challenge. Novel agents with more favorable efficacy and tolerability profiles are currently under investigation.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics–2012 update: a report from the American Heart Association. Circulation. 2012;125:e2–220.
Adams Jr KF, Fonarow GC, Emerman CL, et al. Characteristics and outcomes of patients hospitalized for heart failure in the United States: rationale, design, and preliminary observations from the first 100,000 cases in the Acute Decompensated Heart Failure National Registry (ADHERE). Am Heart J. 2005;149:209–16.
Fonarow GC, Heywood JT, Heidenreich PA, et al. Temporal trends in clinical characteristics, treatments, and outcomes for heart failure hospitalizations, 2002 to 2004: findings from Acute Decompensated Heart Failure National Registry (ADHERE). Am Heart J. 2007;153:1021–8.
Solomon SD, Dobson J, Pocock S, et al. Influence of nonfatal hospitalization for heart failure on subsequent mortality in patients with chronic heart failure. Circulation. 2007;116:1482–7.
Gheorghiade M, Pang PS. Acute heart failure syndromes. J Am Coll Cardiol. 2009;53:557–73.
Gheorghiade M, Pang PS, O’Connor CM, et al. Clinical development of pharmacologic agents for acute heart failure syndromes: a proposal for a mechanistic translational phase. Am Heart J. 2011;161:224–32.
Ellison DH. Diuretic therapy and resistance in congestive heart failure. Cardiology. 2001;96:132–43.
•• Felker GM, Lee KL, Bull DA, et al. Diuretic strategies in patients with acute decompensated heart failure. N Engl J Med. 2011;364:797–805. DOSE was the first large, randomized trial of diuretic strategies in patients with AHF. Using a 2x2 factorial design, subjects were assigned to high vs. low-dose loop diuretics, and to bolus vs. continuous infusion. Neither intervention had a significant effect on the primary efficacy outcome (patient's global assessment of symptoms) or the primary safety outcome (change in creatinine).
Shah RV, McNulty S, O’Connor CM, et al. Effect of admission oral diuretic dose on response to continuous versus bolus intravenous diuretics in acute heart failure: an analysis from diuretic optimization strategies in acute heart failure. Am Heart J. 2012;164:862–8.
Costanzo MR, Guglin ME, Saltzberg MT, et al. Ultrafiltration versus intravenous diuretics for patients hospitalized for acute decompensated heart failure. J Am Coll Cardiol. 2007;49:675–83.
•• Bart BA, Goldsmith SR, Lee KL, et al. Ultrafiltration in decompensated heart failure with cardiorenal syndrome. N Engl J Med. 2012;367:2296–304. This randomized trial demonstrated the superiority of stepped pharmacologic therapy to ultrafiltration in patients with acute heart failure and worsening renal function.
•• Lindenfeld J, Albert NM, Boehmer JP, et al. HFSA 2010 comprehensive heart failure practice guideline. J Card Fail. 2010;16:e1–194. These comprehensive guidelines are available online and provide clinically relevant guidance in the treatment of chronic and acute heart failure.
•• McMurray JJV, Adamopoulos S, Anker SD, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2012;33:1787–847. These comprehensive documents provide clinically relevant guidance in the treatment of chronic and acute heart failure.
Intravenous nesiritide vs nitroglycerin for treatment of decompensated congestive heart failure: a randomized controlled trial. JAMA 2002, 287:1531–40.
Elkayam U, Akhter MW, Singh H, et al. Comparison of effects on left ventricular filling pressure of intravenous nesiritide and high-dose nitroglycerin in patients with decompensated heart failure. Am J Cardiol. 2004;93:237–40.
Guiha NH, Cohn JN, Mikulic E, et al. Treatment of refractory heart failure with infusion of nitroprusside. N Engl J Med. 1974;291:587–92.
Mullens W, Abrahams Z, Francis GS, et al. Sodium nitroprusside for advanced low-output heart failure. J Am Coll Cardiol. 2008;52:200–7.
Durrer JD, Lie KI, Van Capelle FJ, Durrer D. Effect of sodium nitroprusside on mortality in acute myocardial infarction. N Engl J Med. 1982;306:1121–8.
Cohn JN, Franciosa JA, Francis GS, et al. Effect of short-term infusion of sodium nitroprusside on mortality rate in acute myocardial infarction complicated by left ventricular failure: results of a Veterans Administration cooperative study. N Engl J Med. 1982;306:1129–35.
Sackner-Bernstein JD, Skopicki HA, Aaronson KD. Risk of worsening renal function with nesiritide in patients with acutely decompensated heart failure. Circulation. 2005;111:1487–91.
Sackner-Bernstein JD, Kowalski M, Fox M, Aaronson K. Short-term risk of death after treatment with nesiritide for decompensated heart failure: a pooled analysis of randomized controlled trials. JAMA. 2005;293:1900–5.
•• O’Connor CM, Starling RC, Hernandez AF, et al. Effect of nesiritide in patients with acute decompensated heart failure. N Engl J Med. 2011;365:32–43. The ASCEND-HF trial is the largest trial of patients with acute heart failure, demonstrating the safety of nesiritide, as well as its limited additional effectiveness compared to contemporary standard of care.
Mebazaa A, Parissis J, Porcher R, et al. Short-term survival by treatment among patients hospitalized with acute heart failure: the global ALARM-HF registry using propensity scoring methods. Intensive Care Med. 2011;37:290–301.
Cuffe MS, Califf RM, Adams Jr KF, et al. Short-term intravenous milrinone for acute exacerbation of chronic heart failure: a randomized controlled trial. JAMA. 2002;287:1541–7.
Abraham WT, Adams KF, Fonarow GC, et al. In-hospital mortality in patients with acute decompensated heart failure requiring intravenous vasoactive medications: an analysis from the Acute Decompensated Heart Failure National Registry (ADHERE). J Am Coll Cardiol. 2005;46:57–64.
Felker GM, Benza RL, Chandler AB, et al. Heart failure etiology and response to milrinone in decompensated heart failure: results from the OPTIME-CHF study. J Am Coll Cardiol. 2003;41:997–1003.
Giamouzis G, Butler J, Starling RC, et al. Impact of dopamine infusion on renal function in hospitalized heart failure patients: results of the Dopamine in Acute Decompensated Heart Failure (DAD-HF) Trial. J Card Fail. 2010;16:922–30.
Nieminen MS, Akkila J, Hasenfuss G, et al. Hemodynamic and neurohumoral effects of continuous infusion of levosimendan in patients with congestive heart failure. J Am Coll Cardiol. 2000;36:1903–12.
Slawsky MT, Colucci WS, Gottlieb SS, et al. Acute hemodynamic and clinical effects of levosimendan in patients with severe heart failure. Study Investigators Circulation. 2000;102:2222–7.
Packer M, Colucci WS, Fisher L, et al. Effect of levosimendan on the short-term clinical course of patients with acutely decompensated heart failure. J Am Coll Cardiol Heart Fail. 2013. doi:10.1016/j.jchf.2012.12.004.
De Lissovoy G, Fraeman K, Teerlink JR, et al. Hospital costs for treatment of acute heart failure: economic analysis of the REVIVE II study. Eur J Health Econ. 2010;11:185–93.
Mebazaa A, Nieminen MS, Packer M, et al. Levosimendan vs dobutamine for patients with acute decompensated heart failure: the SURVIVE Randomized Trial. JAMA. 2007;297:1883–91.
Mebazaa A, Nieminen MS, Filippatos GS, et al. Levosimendan vs. dobutamine: outcomes for acute heart failure patients on beta-blockers in SURVIVE. Eur J Heart Fail. 2009;11:304–11.
Ho JE, Teerlink JR. Role of tolvaptan in acute decompensated heart failure. Expert Rev Cardiovasc Ther. 2008;6:601–8.
Gheorghiade M, Konstam MA, Burnett Jr JC, et al. Short-term clinical effects of tolvaptan, an oral vasopressin antagonist, in patients hospitalized for heart failure: the EVEREST Clinical Status Trials. JAMA. 2007;297:1332–43.
Konstam MA, Gheorghiade M, Burnett Jr JC, et al. Effects of oral tolvaptan in patients hospitalized for worsening heart failure: the EVEREST Outcome Trial. JAMA. 2007;297:1319–31.
Cotter G, Dittrich HC, Weatherley BD, et al. The PROTECT pilot study: a randomized, placebo-controlled, dose-finding study of the adenosine A1 receptor antagonist rolofylline in patients with acute heart failure and renal impairment. J Card Fail. 2008;14:631–40.
Massie BM, O’Connor CM, Metra M, et al. Rolofylline, an adenosine A1-receptor antagonist, in acute heart failure. N Engl J Med. 2010;363:1419–28.
Teerlink JR, Iragui VJ, Mohr JP, et al. The safety of an adenosine A(1)-receptor antagonist, rolofylline, in patients with acute heart failure and renal impairment: findings from PROTECT. Drug Saf. 2012;35:233–44.
McMurray JJV, Teerlink JR, Cotter G, et al. Effects of tezosentan on symptoms and clinical outcomes in patients with acute heart failure: the VERITAS randomized controlled trials. JAMA. 2007;298:2009–19.
Gheorghiade M, Greene SJ, Filippatos G, et al. Cinaciguat, a soluble guanylate cyclase activator: results from the randomized, controlled, phase IIb COMPOSE programme in acute heart failure syndromes. Eur J Heart Fail. 2012;14:1056–66.
Malik FI, Hartman JJ, Elias KA, et al. Cardiac myosin activation: a potential therapeutic approach for systolic heart failure. Science. 2011;331:1439–43.
• Teerlink JR, Clarke CP, Saikali KG, et al. Dose-dependent augmentation of cardiac systolic function with the selective cardiac myosin activator, omecamtiv mecarbil: a first-in-man study. Lancet. 2011;378:667–75. This first-in-human study of the novel cardiac myosin activator demonstrated dose-dependent increases in cardiac performance in healthy volunteers. Omecamtiv mecarbil could represent the first in class of a novel agent for heart failure.
• Cleland JGF, Teerlink JR, Senior R, et al. The effects of the cardiac myosin activator, omecamtiv mecarbil, on cardiac function in systolic heart failure: a double-blind, placebo-controlled, crossover, dose-ranging phase 2 trial. Lancet. 2011;378:676–83. This small study evaluated omecamtiv mecarbil in patients with chronic heart failure. Compared to placebo, administration of omecamtiv mecarbil caused concentration-dependent increases in LV ejection time and stroke volume.
Teerlink JR, Metra M, Felker GM, et al. Relaxin for the treatment of patients with acute heart failure (Pre-RELAX-AHF): a multicentre, randomised, placebo-controlled, parallel-group, dose-finding phase IIb study. Lancet. 2009;373:1429–39.
•• Teerlink JR, Cotter G, Davison BA, et al. Serelaxin, recombinant human relaxin-2, for treatment of acute heart failure (RELAX-AHF): a randomised, placebo-controlled trial. Lancet. 2013;381(9860):29–39. This international, double-blind trial evaluated the efficacy of serelaxin, a novel vasodilator, in patients with acute heart failure. Treatment with serelaxin was associated with significant improvements in dyspnea, signs of heart failure, and mortality at 180 days.
Metra M, Cotter G, Davison BA, et al. Effect of serelaxin on cardiac, renal, and hepatic biomarkers in the Relaxin in Acute Heart Failure (RELAX-AHF) development program: correlation with outcomes. J Am Coll Cardiol. 2013;61:196–206.
Shah SJ, Blair JEA, Filippatos GS, et al. Effects of istaroxime on diastolic stiffness in acute heart failure syndromes: results from the hemodynamic, echocardiographic, and neurohormonal effects of istaroxime, a novel intravenous Inotropic and lusitropic agent: a Randomized Controlled Trial in Patients Hospitalized with Heart Failure (HORIZON-HF) trial. Am Heart J. 2009;157:1035–41.
Pan S, Chen HH, Dickey DM, et al. Biodesign of a renal-protective peptide based on alternative splicing of B-type natriuretic peptide. Proc Natl Acad Sci USA. 2009;106:11282–7.
Mitrovic V, Lüss H, Nitsche K, et al. Effects of the renal natriuretic peptide urodilatin (ularitide) in patients with decompensated chronic heart failure: a double-blind, placebo-controlled, ascending-dose trial. Am Heart J. 2005;150:1239.
Mitrovic V, Seferovic PM, Simeunovic D, et al. Haemodynamic and clinical effects of ularitide in decompensated heart failure. Eur Heart J. 2006;27:2823–32.
Lee CYW, Chen HH, Lisy O, et al. Pharmacodynamics of a novel designer natriuretic peptide, CD-NP, in a first-in-human clinical trial in healthy subjects. J Clin Pharmacol. 2009;49:668–73.
Lieu H, Goldsmith S, Neutal J, et al. Initial observations of intravenous CD-NP, chimeric natriuretic peptide, on renal functions in chronic heart failure patients. J Card Fail. 2009;15:S77.
Swedberg K, Held P, Kjekshus J, et al. Effects of the early administration of enalapril on mortality in patients with acute myocardial infarction. Results of the Cooperative New Scandinavian Enalapril Survival Study II (CONSENSUS II). N Engl J Med. 1992;327:678–84.
Brancalhao EO, Ochiai ME, Cardoso JN, et al. Haemodynamic effects of aliskiren in decompensated severe heart failure. J Renin Angiotensin Aldosterone Syst. 2012;13:128–32.
Gheorghiade M, Albaghdadi M, Zannad F, Fonarow GC, Böhm M, Gimpelewicz C, et al. Rationale and design of the multicentre, randomized, double-blind, placebo-controlled Aliskiren Trial on Acute Heart Failure Outcomes (ASTRONAUT). Eur J Heart Fail. 2011;13:100–6.
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
John R. Teerlink has been a consultant for Amgen, Cytokinetics, Corthera, Novartis, and St. Jude, and has received grant support from Amgen, Cytokinetics, Corthera, and Novartis.
Van N. Selby declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Congestive Heart Failure
Rights and permissions
About this article
Cite this article
Selby, V.N., Teerlink, J.R. What’s New in the Treatment of Acute Heart Failure?. Curr Cardiol Rep 15, 393 (2013). https://doi.org/10.1007/s11886-013-0393-z
Published:
DOI: https://doi.org/10.1007/s11886-013-0393-z