Abstract
Heart failure is a major burden to the health care system in terms of not only cost, but also morbidity and mortality. Appropriate use of biomarkers is critically important to allow rapid identification and optimal risk stratification and management of patients with both acute and chronic heart failure. This review will discuss the biomarkers that have the most diagnostic, prognostic, and therapeutic value in patients with heart failure. We will discuss established biomarkers such as natriuretic peptides as well as emerging biomarkers reflective of myocyte stress, myocyte injury, extracellular matrix injury, and both neurohormonal and cardio-renal physiology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Heart failure is recognized as a major cause of mortality and morbidity [1]. The CDC estimated that in 2010 the total direct and indirect cost for the treatment of heart failure (HF) in the United States was $34 billion [2]. The focus on lowering cost, reducing readmission rates, and ultimately to provide the most advanced care for patients with HF have driven recent studies in biomarkers that not only expedite diagnosis, but also predict mortality and morbidity, and even facilitate in therapy guidance in patients.
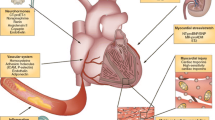
There are a variety of biomarkers that have shown prognostic value in HF and they widely differ in their mechanism of action. Figure 1 provides a schematic overview of the biomarkers in discussion. While some biomarkers are specific to the failing myocardium, others are nonspecific, originating external to cardiac myocytes, but still having some prognostic value in heart failure [3].
Schematic representation of biomarkers in patients with heart failure categorized according to level and type of myocardial change. Markers of myocyte stress: B-type natriuretic peptide (BNP), N-terminal pro B-type natriuretic peptide (NT-proBNP), soluble ST2 (sST2); Markers of myocyte injury/death; cardiac troponins; Extracellular matrix biomarker; Galectin 3; Neurohormonal markers; Mid-regional pro adrenomedullin (MR-proADM), Copeptin
This manuscript will review biomarkers that have shown the most prognostic value in patients with HF, including natriuretic peptides and troponins that have been well studied, as well as newer biomarkers like sST2, galectin, MR-proADM, and Copeptin. We will further discuss the use of a new generation of biomarkers for patients with HF who concurrently also have renal disease or cardio-renal syndrome. These cardio-renal biomarkers seem to circumvent the limitations of prior biomarkers used for HF patients whose values were not as reliable in the presence of renal disease.
Pathophysiology of Heart Failure
The pathophysiology of HF is quite extensive. It is initiated with the cardiac pump system being impaired by any number of reasons including coronary artery disease, idiopathic dilated cardiomyopathy, toxins, hypertensive disease, arrhythmias, etc. that lead to the activation of neurohormonal pathways to compensate for the cardiac impairment and low blood circulation state.
As a response to the impaired cardiac myocardium the sympathetic nervous system compensates by increasing contractility and heart rate to try to maintain cardiac output. There is compensatory systemic vasoconstriction, decreased renal perfusion, and activation of the renin-angiotensin system among other changes, which leads to arteriolar vasoconstriction, release of aldosterone, endothelial dysfunction, and sodium and water retention. Vasopressin is also released by baroreceptor stimuli and non-osmotic changes leading to sodium and water retention. These compensatory mechanisms that counteract to balance the effects of HF over time result in a vicious downward spiral leading to cardiac remodeling, myocardial cell death, and end-organ failure [4].
Biomarkers of Myocyte Stress
Background
Several biomarkers have emerged that reflect myocardial wall stress or stretch that occurs in the failing myocardium. The best studied of all the biomarkers thus far are the Natriuretic Peptides (NPs). NPs are a family of peptide hormones that include atrial natriuretic peptic (ANP), brain natriuretic hormone (BNP), C-type natriuretic peptide (CNP) and dendroaspis natriuretic peptide, a D-type natriuretic peptide (DNP). Of these, ANP and BNP are released from the atria and ventricle respectively and have been the forerunner in HF diagnostic and prognostic utility with BNP the most clinically used and well established.
NPs have similar ring shaped structures. ANP is a 126 pro-hormone and is mainly synthesized in the atria of the heart [5]. BNP was initially identified from the porcine brain but later found to be predominantly stored in small quantities in the ventricles of the human heart [5]. BNP and N terminal BNP (NT-proBNP) both circulate and are synthesized from a 108 amino acid pro-hormone (proBNP) [5]. Since the pro BNP messenger RNA is unstable, BNP is produced and up-regulated depending on the degree of ventricular wall stretch seen in HF [5]. The half -life of BNP is about 20 minutes, which is significantly longer than that of ANP [6]. NT-proBNP has an estimated half-life of 60-90 minutes which is longer than that of BNP [6]. BNP is removed from the circulation by endopeptidases and NT- proBNP is cleared by the kidneys [6]. BNP and NT-proBNP outperform ANP in the diagnosis of HF due to their longer half-lives. However, it is important to note that NT pro BNP/BNP values are not as reliable in certain patients including those with renal disease or obesity.
Once released BNP, NT-proBNP and ANP have multiple functions, including vasodilation, natriuresis, kaliuresis, and inhibition of both the renin–aldosterone– angiotensin system and the sympathetic nervous system.
Diagnostic Use of Natriuretic Peptides in Heart Failure
Numerous studies have demonstrated the diagnostic capacity of both BNP and NT-proBNP. In the Breathing Not Properly Study, McCullough et al. [7] showed that BNP at 100 pg/ml had a sensitivity of 90 % and specificity of 73 % for heart failure in patients in the Emergency Department with acute dyspnea. They also found that BNP values added to clinical judgment and enhanced diagnostic accuracy of HF from 74 to 81 %. The study showed that BNP was better than clinical judgment alone for diagnostic purposes and improved provider clinical judgment. Receiver operating characteristic (ROC) analysis revealed an area under the curve (AUC) of 0.86 for clinical judgment and 0.90 for BNP using a cutoff off 100 pg/ml. When clinical judgment was combined with BNP, the AUC curve was 0.93 [7]. BNP studies have likewise shown similar improvement of diagnostic accuracy in the outpatient primary care setting and as a result led to quicker initiation of therapy [8]. The IMPROVE –CHF study showed that the knowledge of NT-pro BNP in ED in diagnosing heart failure reduced ED visit duration by 21 % (6.3 to 5.6 hours; P = 0.031), reduced re-admission over the next 2 months by 35 % (51 to 33; P = 0.046), and reduced overall cost over 2 months from presentation (US $6129 to US $5180 per patient; P = 0.023) [9]. Not surprisingly, NPs are therefore also a part of the ESC guidelines in the diagnosis and treatment of acute and chronic HF [10].
Prognostic Use of Natriuretic Peptides in Heart Failure
In addition, the prognostic guidance of BNP/NT-proBNP can accurately predict mortality and morbidity and distinguish those heart failure patients who would benefit from admission [10]. The REDHOT Study showed that admission BNP from the ED was predictive of 90-day event rates (CHF visits, admissions, mortality) [11]. In patients admitted with BNP <200 pg/ml the combined event rate was 9 % but it was 29 % in patients admitted with BNP >200 pg/ml [11]. Metra et al. [12] similarly found the independent prognostic value of serial changes and discharge NT-pro BNP in hospitalized patients with acute heart failure. In a multivariate analysis, Noveanu et al. [13] found that in patients admitted with acute decompensated HF, serial BNP levels at 24 hours, 48 hours, and at discharge, along with predischarge NT-pro BNP, independently predicted one year mortality but were not predictive of 1 year readmission rates. Di Somma et al. [14] in the Italian RED study have shown that BNP reduction during hospitalization along with discharge BNP are both powerful tools of prognosis. In acute decompensated heart failure patients with discharge BNP of <300 pg/ml and percentage decrease of BNP at discharge of <46 % compared to discharge BNP <300 pg/ml and percentage decrease at discharge of >46 % had an odds ratio for adverse events of 4.775. Patients with discharge BNP >300 pg/ml and percentage decrease at discharge of <46 % compared to those with discharge BNP <300 pg/ml and percentage decrease at discharge of >46 % had an odds ratio for adverse events of 9.614 [14]. Furthermore, the prognostic value of BNP was demonstrated in stable HF patients as well in the outpatient setting by Jan et al. [15] who showed that increasing tertile of BNP and elevated BNP predicts combined mortality and morbidity outcome.
It is important to discuss that a new investigation has shown that pro BNP (1-108), which circulates in normal humans, may be useful in the prognosis of heart failure patients based on fluctuation due to heart failure stage [16]. It is much less potent compared to BNP and NT-proBNP in its natriuretic function and vasodilation. Macheret et al. [16] showed that pro BNP has 78.8 % sensitivity and 86.1 % specificity for detecting LV systolic dysfunction, which is similar to BNP and less that of NT proBNP. They further showed that proBNP(1-108) to NT-proBNP(1-76) ratio decreases based on heart failure stage [16]. These findings are exciting, but relatively new, and further investigations will need to be conducted to show how useful proBNP can be for clinical use.
Natriuretic Peptide Therapy Guidance in Heart Failure
The diagnostic and prognostic utility of BNP/NT proBNP naturally led to investigation into the therapy guidance utilizing these biomarkers. Studies suggest that NP therapy guidance may be beneficial in guiding HF therapy. Gaggin et al. [17] recently reported data from the PROTECT study which showed that in outpatient NT-proBNP tailored therapy (goal set at <1000) in chronic heart failure patients age >75 years decreased NT-proBNP 2664 to 1418 pg/mL, and had the lowest cardiovascular event rate at 0.71 events per patient compared to the standard of care arm where patients increased NT-proBNP 2570 to 3523 pg/mL, and showed the highest cardiovascular event rate at 1.76 events per patient. This improvement in cardiac event rate with NT-proBNP tailored therapy was most significant in those above age 75 and not as significant in those below 75 years of age. Valle et al. [18], showed that in acute decompensated HF, sequential measurements of BNP and BIVA (combined bioelectrical vectorial impedance analysis for body water analysis) and tailoring therapy to titrate BNP to <250 pg/ml and BIVA, showed that discharge BNP value of ≤250 pg/ml was associated with a 25 % event rate within 6 months compared to a 37 % event rate with a value >250 pg/ml, even with similar discharge body water values from BIVA [18]. A recent expert review by Januzzi on BNP/NT-proBNP tailored therapy thoroughly reviewed the negative and positive outcome trials for tailored therapy and clearly shows that the key difference in these studies was the goal BNP/NT-pro BNP. The positive outcome trials set low BNP/NT-pro BNP (with targets set at BNP ≤100 pg/mL and NT-proBNP ≤1000 pg/mL, respectively); whereas those with negative outcomes set higher goal values for BNP and NT-proBNP [19•]. The review went on to support BNP/NT-proBNP heart failure guided therapy. The basic recommendations for tailoring therapy according to BNP/NT pro-BNP are outlined by Januzzi as an expert guideline in Table 1.
sST2
Background
ST2, a member of the interleukin-1 receptor family, plays an active role in myocardial remodeling and is a valuable marker of prognosis in patients with heart failure. ST2 exists as both a soluble isoform (sST2) and a membrane-bound receptor (ST2L), previously studied as a cell surface marker of the TH2 lymphocyte [20]. Both isoforms are expressed by cardiac myocytes and fibroblasts in response to ventricular wall stress [21]. The functional ligand of ST2L is interleukin-33 (IL-33), a cardiac fibroblast protein produced in response to myocyte stretch [22, 23]. The IL-33/ST2L interaction on cardiac myocytes has a protective effect against ventricular remodeling by inhibiting the development of hypertrophy and fibrosis in response to mechanical stress or injury [24]. sST2 competes with IL-33 for ST2L binding, thereby blocking the interaction of IL-33 and ST2L and promoting a fibrotic response [24]. Consequently, elevated sST2 concentration appears to indicate activation of a fibrotic response to injury, resulting in an increased level of myocardial fibrosis and cardiac remodeling [24].
sST2 elevation has been described in several pulmonary conditions, including asthma, acute lung inflammation, idiopathic pulmonary fibrosis, acute eosinophilic pneumonia, and other more common conditions including pneumonia, pulmonary embolism, and chronic obstructive pulmonary disease [25–29]. However, its predictive value is strongest in cardiovascular disease. sST2 has been found to be predictive of worsening disease requiring hospitalization and mortality in the setting of both acute and chronic HF as well as in the setting of acute myocardial infarction (MI) [30]. Conveniently, while sST2 assays are affected moderately by interleukin-6 and gender, they are unaffected by fasting state, age, renal function, or body mass index [31], making it an attractive biomarker for clinical use in HF.
Prognostic Value of sST2 in Heart Failure
sST2 has prognostic value in stable heart failure. Serum levels of sST2 are significantly higher in subjects with NYHA function class III and IV compared to subjects without heart failure [32]. sST2 also correlates independently with both left and right heart chamber size and function [33]. In addition, sST2 adds to the prognostic value of NT-proBNP and clinical risk scores in patients with stable chronic heart failure [34]. Furthermore, serial sST2 monitoring in outpatients with heart failure offers additional prognostication. Patients with chronic heart failure who demonstrate a 15 % reduction in sST2 levels over time have more favorable long-term outcomes [32, 35].
sST2 also plays a role in prediction of heart failure. Baseline sST2 levels in patients with acute MI have been shown to predict incident heart failure [36, 37]. This phenomenon may be a function of infarct size. Higher levels of sST2 at the time of infarction have been associated with greater subendocardial and transmural extent of infarction, and are inversely associated with ejection fraction at baseline and 6 months post-MI [38]. Interestingly, this effect may be partly dependent on aldosterone [38], raising the possibility that aldosterone antagonists may have a role in the prevention of myocardial fibrosis and remodeling following MI.
In addition to its role in stable heart failure or in the prediction of heart failure, sST2 has strong prognostic value in acute decompensated heart failure (ADHF). Among patients presenting to the ED with acute dyspnea, baseline sST2 levels strongly predict one-year mortality among patients, including patients with [39] and without [40] an eventual diagnosis of ADHF. sST2 is as prognostically significant in patients with preserved ejection fraction as in those with systolic dysfunction [41]. sST2 has even been shown to be superior to NT-proBNP for prediction of one year mortality in patients with ADHF, although it has less diagnostic utility than natriuretic peptides [39].
Use of a combination of biomarkers including sST2 and natriuretic peptides in the acute setting may improve risk stratification of patients with ADHF. Patients with elevated levels of both sST2 and BNP have been shown to carry a 2.6-fold higher risk of one year mortality compared to patients with only a single marker elevated, and a 5.5-fold higher risk compared to patients with neither marker elevated, even after adjustment in multivariate analysis [42]. sST2 and BNP therefore appear to provide additive information. While BNP is a better indicator of left ventricular filling pressure and wall stress, sST2 serves as a measure of remodeling and fibrotic change.
Biomarkers of Myocyte Injury/Death
Background
Although cardiac troponin (cTn) is used primarily to diagnose acute coronary syndrome, cTn elevation has been well described in the setting of heart failure and can offer powerful prognostic information. Detection of cTn classically indicates the presence of myocyte necrosis. An elevated troponin above the 99th percentile upper reference limit with a rising and/or falling pattern and other symptoms or signs of ischemia indicates a diagnosis of type 1 MI. However, several other cellular processes induce release of cTn into the circulation, including apoptosis [43], cellular release of cTn degradation products [44], and increased cell wall permeability due to myocardial wall stretch or ischemia [45]. Ischemia in the absence of thrombosis can lead to cTn elevation by inducing supply and demand imbalances in coronary blood flow seen with tachycardia, hypotension, or anemia [46]. In heart failure, cTn elevation can be observed in part due to subendocardial ischemia [47], although coronary endothelial dysfunction [48] as well as myocardial injury from wall stretch [47] likely contribute as well. Other proposed mechanisms of troponin elevation in heart failure include globally, rather than regionally, reduced myocardial perfusion and impaired renal function [49]. Furthermore, other processes that can result in heart failure, such as amyloidosis, toxin exposure, myocarditis, or stress-induced cardiomyopathy, can lead to elevations in cTn [50].
Prognostic Use of Troponins in Heart Failure
cTn elevation has been well described in stable heart failure without overt evidence of cardiac ischemia [51]. This phenomenon is particularly apparent with the use of high-sensitivity cTn assays, which offer a 10 to 100-fold lower detection limit [52]. The prevalence of cTn elevation in stable HF has been reported as high as 10 % using a conventional cTnT assay, 51 % using a conventional cTnI assay, and 92 % using a high-sensitivity assay [52, 53]. Higher baseline cTn levels have consistently been associated with higher rates of adverse outcomes, including overall mortality [52, 53], worsening heart failure [54], new or recurrent MI [54], and cardiac transplantation [55]. Serial cTn measurements may also be relevant. A downward trending pattern of elevation is associated with better outcomes than a persistent or upward trending pattern [55]. Together, these data indicate that worsening ventricular function and adverse clinical outcomes in heart failure may be a result of myocardial injury. cTn may also offer prognostic information for risk of developing heart failure. In asymptomatic adults, detectable cTn has been associated with future risk of developing heart failure [56].
In ADHF, cTn elevation is more common and can be more marked. A diagnosis of Type I MI should always be carefully considered as a precipitant of an acutely decompensated state, and the pattern of elevation of cTn should not be used to imply the mechanism of troponin elevation [50]. Elevated cTn is a relatively common finding in ADHF even in the absence of other signs or symptoms of Type 1 MI. In the Acute Decompensated Heart Failure National Registry (ADHERE) study, 75 % of patients hospitalized with ADHF had detectable levels of cTn, though elevations above the 99th percentile upper reference limit were seen in only 6.2 % of patients [57]. Patients with cTn elevation had a 2.6-fold higher rate of in-hospital mortality, even after adjustment for other clinical variables [58]. The Enhanced Feedback for Effective Cardiac Treatment (EFFECT) study confirmed these results and also demonstrated a dose-response relationship between the magnitude of cTn and likelihood of adverse outcomes [59]. Serial measurements of cTn in patients hospitalized with ADHF also carry prognostic significance. cTn elevation in ADHF typically declines over time to a baseline level similar to that seen in stable heart failure [58], but patients with up-trending cTn levels during hospital admission have increased rates of 90-day mortality and readmission for HF, when compared to patients with stable or decreasing cTn [60, 61]. Furthermore, the discharge cTn value by itself carries prognostic value, even in the absence of serial measurements. Elevated levels of high-sensitivity cTnI at discharge, using an ROC-determined cutoff of 23.25 ng/L, have been associated with increased risk for 90-day mortality and readmission for heart failure [61]. Discharge values of high-sensitivity cTnI predict adverse outcomes as effectively as discharge values of BNP, when using a receiver operating characteristic (ROC)-determined BNP cutoff of 360 ng/L [61]. Unfortunately, while cTn clearly offers prognostic information in the setting of ADHF, data are lacking regarding targeted interventions for heart failure based on the presence or degree of cTn elevation [50].
Extracellular Matrix Biomarkers
Several extracellular matrix biomarkers have been found to have correlation to HF. The dynamic changes of biomarkers in the extracellular matrix have shown to play a role in the inflammatory response, alteration of collagen and protein metabolism, and fibrosis that lead to cardiac remodeling. Biomarkers like collagen propeptide, matrix metalloproteinases (MMPs), tissue inhibitors of metalloproteinases (TIMPs), N-terminal collagen type III peptide, and galectin 3 have shown to have a role in heart failure. Of these, Galectin 3 has been of particular interest due to growing data showing its prognostic value in HF.
Galectin 3
Background
Galectin 3 is a 29-35 kDa chimera type galectin from a family of soluble beta-galactoside-binding lecithins [62]. It is found in a wide range of tissues and localized primarily in the cytoplasm, and also in the mitochondria and nucleus. Galectin 3, which is secreted by macrophages, interacts with cell surface receptors and glycoproteins to activate transmembrane signaling pathways leading to a number of physiologic and pathologic changes including inflammation and fibrosis. Galectin 3 works as a paracrine and endocrine factor to stimulate additional macrophages, pericytes, myofibroblasts, and fibroblasts. This leads to cellular proliferation and secretion of procollagen I. Procollagen I is irreversibly crosslinked to form collagen and result in cardiac fibrosis (Fig. 2).
Galectin-3 pathways. The network represents molecular relationships between different gene products. Node shapes indicate the functional class of the gene product, whereas node colors indicate a role in general fibrosis (orange) or cardiac fibrosis (green). Edge colors indicate up-regulation or activation (red), down-regulation or inhibition (green) or involvement without clear directionality (yellow). (With permission from: de Boer RA, Voors AA, Muntendam P, van Gilst WH, van Veldhuisen DJ. Galectin-3: a novel mediator of heart failure development and progression. Eur J Heart Fail. 2009 Sep;11(9):811-7
Prognostic Value of Galectin 3 in Heart Failure Patients
Recent studies have shown the prognostic benefit and usefulness of Galectin 3. Ho et al. [63] showed that Galectin 3 was associated with and increased risk of incident heart failure in the community with hazard ratio HR 1.28 per 1 SD increase in log Galectin 3 and remained significant after adjustment for clinical variables and BNP with HR 1.23. It correlated significantly with the risk for all cause mortality as well (multivariable-adjusted HR 1.15) [63]. De Boer et al. [64] showed that doubling of Galectin 3 levels was associated with increased all cause mortality and heart failure hospitalization in patients with reduced and preserved ejection fraction (HF 1.97). They also showed that when combining Galectin 3 and BNP levels, area under the curve (AUC) 0.69 P < 0.05, increased prognostic value over either BNP or Galectin 3 alone, AUC 0.65 (P < 0.001) and AUC of 0.67 (P = 0.004) respectively [64]. Interestingly, the predictive value of Galectin 3 was stronger in HF patients with preserved ejection fraction than those with reduced left ventricular ejection fraction [64]. McCullough et al. [65] also showed that regardless of symptoms, clinical findings, and other laboratory measures, a Galectin 3 level >25.9 ng/mL is predictive of rapid progression of heart failure, hospitalization, and death. Shah et al. [66] showed that in dyspneic patients in the ER, Galectin 3 levels were associated with echocardiographic markers of ventricular dysfunction and in ADHF patients, Galectin 3, irrespective of echocardiographic findings, was an independent predictor of mortality up to 4 years. The good news is that Galectin 3 assays are also showing acceptable performance and similar outcomes in recent studies [67], which will make their use more universally accepted.
Neurohormonal Biomarkers
Background
Of the newer biomarkers, a neurohormone, midregion proadrenomedullin (MR-proADM), has been shown in recent studies to have strong prognostic value. Adrenomedullin, like NPs, has vasodilatory and natriuretic properties through the second messenger cyclic adenosine 3′,5′-monophosphate (cAMP), nitric oxide and the renal prostaglandin system. It is found in a wide variety of tissues including the cardiovascular, gastrointestinal, renal, pulmonary, cerebral, endocrine systems, as well as vascular endothelium and smooth muscle. It also has local paracrine and autocrine functions [68].
Prognostic Value of MR-proADM in Heart Failure
Mid-regional proadrenomedullin (MR-proADM) is a stable peptide of adrenomedullin and readily measurable. In a large, multicentered trial, Maisel et al. [69] showed that MR-proADM (≥ 120 pmol/l) was as useful as BNP (≥100 pg/ml) in diagnosis of acute decompensated heart failure in patients with dyspnea in the ER. MR-proADM may also be useful in patients with intermediate BNP values. Most importantly, Maisel et al. showed using cut off values from ROC analysis that MR-proADM has a 73 % accuracy to predict 90-day mortality in HF patients while for BNP it was 62 % and that MR-proADM added prognostic value to BNP values [69]. A follow up analysis by Maisel et al. [70], recently emphasized that MR-proADM may be superior to BNP, troponins, and other biomarkers, in predicting 90 day all cause mortality in patients presenting with shortness of breath in the ER. Furthermore, they showed that serial monitoring of MR-proADM could be very useful to classify high risk patients [70] although further studies are needed to evaluate the prognostic value of serial measurements. In addition, Von Haehling et al. [71] found that increasing MR-proADM during a one year period is an independent predictor of mortality in chronic heart failure patients, hazard ratio 1.82, and that MR-proADM was stronger prognostically than NT-proBNP when added to the base model [71]. In the GISSI trial [72], changes in MR-proADM tertile were proportionally related to mortality, while other biomarkers including mid-regional pro-atrial natriuretic peptide (MR-proANP), C-terminal pro-endothelin-1 (CT-proET-1) and C-terminal pro-vasopressin (CT-proAVP or Copeptin) were not. MR-proADM again showed prognostic value in this study independent of natriuretic peptides which makes it a potential powerful biomarker [72]. MR-proADM assay is now available for clinical use and can be available within 30 to 60 mins. MR-proADM may also be very helpful clinically in HF patients with renal dysfunction, obesity, or advanced age when NP values are not as reliable [69].
Copeptin
Background
In HF patients the release of arginine vasopressin (AVP) also known as the anti-diuretic hormone, occurs mainly in direct response to changes in plasma volume and osmolality [73–75]. The instability in-vitro, small size and fast clearance rate makes AVP difficult to measure [74, 75]. Copeptin is the C-terminal segment of the AVP precursor peptide and is released in equimolar amounts along with ADH from the hypothalamus. Copeptin is a glycosylated peptide containing a 39-amino acid structural motif with a leucine core [75, 76]. Copeptin has been demonstrated to be more stable in-vitro compared to AVP allowing a successful measurement in the clinical setting [73, 75, 77].
Diagnostic and Prognostic Utility of Copeptin in Heart Failure
The OPTIMAAL study [77] demonstrated that in patients developing heart failure after acute myocardial infarction, COX hazard analysis revealed that elevated Copeptin levels along with BNP and NT-proBNP were significantly associated with mortality. ROC analysis in predicting mortality revealed an AUC of 0.81 for Copeptin compared to AUC 0.66 for BNP and 0.67 for NT-proBNP [77]. Moreover in one month follow-up, changes in Copeptin levels from baseline was significantly associated with increased mortality HR 3.5, p = 0.002. The study highlighted the role of Copeptin in heart failure patients, suggesting that poor cardiac output, hyponatremia and elevated angiotensin II levels drive the release of Copeptin in heart failure [77]. Another study [78] demonstrated that Copeptin levels were directly proportional to left-ventricular volumes and inversely related to ejection fractions in patients developing post-acute myocardial heart failure. Maisel et al. [79] demonstrated that in 557 patients with acute HF presenting to the emergency department, increased 90-day mortality was seen in patients with elevated Copeptin levels HR 3.85, p < 0.001. The study tested composite endpoints of mortality, readmission and ED visits with results revealing that Copeptin levels were significantly increased in such patients [79]. Hyponatremia, along with elevated Copeptin levels, was also found to be significantly associated with high risk of mortality HR 7.36, p < 0.001 [79].
Copeptin has provided robust evidence as an effective marker of heart failure severity especially in ischemic heart failure. Once in the circulation, AVP affects cardiac contractility resulting in decreased cardiac output and retention of volume leading to dilutional hyponatremia [77, 79]. Copeptin is stoichiometrically released along with AVP thus making it a sensitive and specific marker of heart failure disease progression [80]. Although a majority of the studies assessing Copeptin levels were conducted in relative small cohorts of patients with acute HF post-acute myocardial infarction, future studies should aim at assessing longer follow-ups.
Cardiorenal Biomarkers
Renal impairment in HF is common and associated with high mortality and the prevalence of HF worsens with the degree of renal damage [81]. Smith et al. [82] found that of 80,098 hospitalized and non-hospitalized HF patients, 63 % of patients had at least minimal renal impairment, and 29 % had moderate to severe impairment. They found that mortality increased proportionally with the decline in renal dysfunction. Specifically they demonstrated a 15 % increased mortality for every 0.5 mg/dl increase in creatinine and 7 % increased mortality for every 10 ml/min decrease in eGFR [82]. Cardiorenal syndrome is a disease process where the interplay of a neurohormonal, intrarenal, and transrenal perfusion pressure lead to the worsening of both cardiac and renal function. There are five subtypes of cardiorenal syndrome as depicted in Fig. 3 [83••]. Cardiorenal patients are so prevalent and have such high mortality risks that the need for more reliable biomarkers has been the focus of much research. One of the limitations of NPs which are the primary biomarkers used in clinical practice in HF patients is in the setting of renal disease where their values are less reliable [83••].
Pathophysiology and definitions of the 5 subtypes of cardiorenal syndrome. (With permission from: Ronco C, McCullough P, Anker SD, Anand I, Aspromonte N, Bagshaw SM, et al; Acute Dialysis Quality Initiative (ADQI) consensus group. Cardio-renal syndromes: Report from the consensus conference of the acute dialysis quality initiative. Eur Heart J. 2010;31:703 – 711) [83••]
Cystatin C
Background
Cystatin C is an endogenous renal marker from the family of cysteine proteinase inhibitors secreted by nucleated cells at a constant rate [84]. It is proposed to be more sensitive than creatinine and GFR for kidney dysfunction. It freely crosses the glomerular membrane, catabolized by the proximal tubules, and it is not affected by age, sex, or muscle mass [84, 85].
Prognostic Value of Cystatin C in Heart Failure
Elevated Cystatin C levels have been associated with higher all cause mortality [84, 86, 87] and CVD related deaths [87–89]. Ix et al. [86] found that in ambulatory patients with coronary heart disease the highest quartile (> or = 1.30 mg/L) of Cystatin C were at increased risk of all-cause mortality, HR 3.6, cardiovascular events HR 2.0, and incident heart failure, HR 2.6 compared to the lowest quartile (< or = 0.91 mg/L). The results were similar in patients regardless of GFR or presence of microalbuminuria [86]. Lassus et al. [90] showed that in acute HF patients Cystatin C above 1.30 mg/L had the highest adjusted HR of 3.2 and mortality increased with each tertile of Cystatin C. Interestingly, they also found that normal plasma creatinine, but elevated Cystatin C levels were associated with significantly higher mortality [90]. Furthermore, Carrasco-Sanchez et al. [91] demonstrated that in patients with HF with preserved ejection fraction patients with higher quartile of Cystatin C were associated with increased risk for adverse events [91]. Patients with highest quartile of Cystatin C level had a HR 3.40 for the primary end point and HR 8.14 for all-cause mortality and the association of elevated Cystatin C and poor prognosis held even with normal renal function [91]. In fact, the Dallas Heart Study [92] demonstrated that higher Cystatin C levels were associated with LV mass and a concentric LV hypertrophy, regardless of creatinine or GFR. The study concluded that Cystatin C may be useful in identifying patients at risk for cardiac structural abnormalities, with or without renal disease [92]. Current studies continue to be done on the value of Cystatin C in combination with other biomarkers in heart failure and in search of the mechanism by which it is so closely related to both heart disease and renal disease.
Neutrophil Gelatinase Associated Lipocalin
Background
Neutrophil gelatinase-associated lipocalin (NGAL) is a 25 kDa protein and part of the lipocalin family [93]. NGAL is produced as a result of renal toxic or ischemic injury and data suggests that it detects renal injury within a couple hours of the insult versus the couple of days it takes for creatinine to increase [94, 95].
The precise mechanism of action of NGAL is unclear. It is secreted by different tissues (endothelium, hepatocytes, cardiocytes, renal cell) and stored in granules in neutrophils [85]. It has been shown to likely play a role in the immune/inflammatory process in the natural history of HF [95]. Recent studies indicate that NGAL might be a marker of mineralocorticoid related injury [96]. The study showed that in mice mineralocorticoid pathologic challenge led to increased expression of NGAL in cardiomyocytes, aorta, and increased level in plasma.
Prognostic Value of NGAL in Heart Failure
The GALLANT trial [97] showed that in acute HF adding discharge NGAL, over BNP alone, showed a 10.3 % improvement in classification in those with follow up events (30 day readmission or all cause mortality) and 19.5 % in those without follow up events. This was a net reclassification improvement of 29.8 % (P = 0.010). In addition, patients with both elevated BNP and NGAL had a hazard ratio (HR) = 16.85 while those with low BNP yet high NGAL had a HR = 9.95 [97]. The authors showed that NGAL is a strong prognostic indicator of adverse outcome. A recent study [98] indicates that both serum and urine NGAL predicts renal injury, but serum NGAL showed stronger correlation with GFR while urine NGAL correlated with distal tubular injury (as in diuresis or natriuresis). Damman et al. [99] also showed that urine NGAL is predictive of tubular damage in chronic HF patients, where median urinary NGAL values in chronic heart failure patients was 175 (70-346) versus that in controls was 37 (6-58) microg/gCr [99].
Naturally, more studies will need to be done to see the precise role of NGAL in heart failure and renal disease, but its prognostic utility is promising.
Kidney Injury Molecule-1
Background
Another biomarker rapidly gaining attention in detecting acute kidney injury is Kidney Injury Molecule-1 (KIM-1). In post-ischemic rodent models the up-regulation of the KIM-1 gene in the proximal tubule demonstrated its use as an early marker of acute kidney injury [100]. Structurally, KIM-1 is a type 1 transmembrane protein containing immunoglobin ectodomains and mucin subdomains [100, 101]. In the early phase of acute ischemic kidney injury affecting the proximal tubule, a temporal progression of complex molecular events occur [100]. One of these events is the upregulation of transmembrane proteins and their release into the blood stream and urine, making them effective biomarkers of acute kidney injury.
Diagnostic and Prognostic Utility of KIM-1 in Heart Failure
Compared to serum creatinine, studies have shown that KIM-1 has a faster response rate and is released sooner in the setting of acute kidney injury [102, 103]. In a multivariate analysis study [104] assessing the temporal elevation of urinary biomarkers in AKI in post-cardiac surgery patients, the combination of KIM-1 and NGAL achieved a net reclassification improvement of 48 % (p < 0.05) at 6 hours [104]. On ROC analysis, KIM-1 achieved an AUC of 0.7 in predicting AKI at 2 hours [104]. Another multicenter study [105] demonstrated that in 1635 patients hospitalized after presenting to the ED, KIM-1 achieved an AUC of 0.71 in detecting inpatient intrinsic AKI. Urinary KIM-1 levels were significantly elevated in patients with intrinsic AKI compared to those with CKD and pre-renal AKI [105]. Furthermore, KIM-1 and NGAL were significantly able to predict a combined outcome of in-hospital death and/or dialysis initiation [105]. KIM-1 achieved a negative predictive value of 95 % in diagnosing intrinsic AKI [105]. Jungbauer et al. [106] demonstrated that in symptomatic HF patients, urinary KIM-1 was significantly elevated at 1100, interquartile range 620-1920 ng/gCr as compared to 550, interquartile range 320-740 ng/gCr, when compared to healthy controls. The study showed that urinary KIM-1 increased significantly with worsening left ventricular function and significantly correlated in severity with New York Heart Association (NYHA)-class. KIM-1 also predicted all-cause mortality, the composite of all-cause mortality, and rehospitalization for heart failure [106]. Interestingly, NGAL did not show much significance in this study [106]. Damman et al. [107] also found that urinary KIM-1 significantly increased in chronic systolic HF patients 277 (188-537) ng/gCr when compared with healthy controls. They found that urinary KIM-1, regardless of GFR, correlated with risk of death or HF hospitalizations, HR = 1.15 [107]. These studies highlight the importance of tubular damage and role of tubular markers in cardiorenal patients.
The role of KIM-1 in heart failure still needs further investigation prior to definite conclusions and clinical use; however, there seems to be strong evidence of its predictive value in this patient population which can hopefully be used clinically in the future.
Conclusions
The place of biomarkers in patients with HF is rapidly evolving and progressing with new studies and data. The goal is to optimize management and treatment of HF expeditiously given the high rates of mortality and morbidity of this disease. Biomarkers are objective tools to help physicians classify those patients that would benefit most from admission, need more aggressive treatment, and identify those with poor outcomes. The future of biomarkers in HF is expanding. They will not only improve diagnosis and prognosis of heart failure but also likely guide medical therapy and positively influence the normal progression of the disease.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, De Simone G, et al. Heart disease and stroke statistics--2010 update: a report from the American Heart Association. Circulation. 2010;121(7):e46–215.
Heart Disease and Stroke Prevention Addressing the Nation's Leading Killers: At A Glance 2011. Centers for Disease Control and Prevention. http://www.cdc.gov/chronicdisease/resources/publications/AAG/dhdsp.htm
Van Kimmenade RR, Januzzi Jr JL. Emerging biomarkers in heart failure. Clin Chem. 2012 Jan;58(1):127–38.
Jackson G, Gibbs CR, Davies MK, Lip GY. ABC of heart failure. Pathophysiology BMJ. 2000;320(7228):167–70.
Pandit K, Mukhopadhyay P, Ghosh S, Chowdhury S. Natriuretic peptides: Diagnostic and therapeutic use. Indian J Endocrinol Metab. 2011 Oct;15 Suppl 4:S345–53.
Kimura K, Yamaguchi Y, Horii M, Kawata H, Yamamoto H, Uemura S, et al. ANP is cleared much faster than BNP in patients with congestive heart failure. Eur J Clin Pharmacol. 2007 Jul;63(7):699–702.
McCullough PA, Nowak RM, McCord J, Hollander JE, Herrmann HC, Steg PG, et al. B-type natriuretic peptide and clinical judgment in emergency diagnosis of heart failure: analysis from Breathing Not Properly (BNP) Multinational Study. Circulation. 2002 Jul 23;106(4):416–22.
Moe GW, Howlett J, Januzzi JL, Zowall H, Canadian Multicenter Improved Management of Patients With Congestive Heart Failure (IMPROVE-CHF) Study Investigators. N-terminal pro-B-type natriuretic peptide testing improves the management of patients with suspected acute heart failure: primary results of the Canadian prospective randomized multicenter IMPROVE-CHF study. Circulation. 2007;115(24):3103–10.
Moe GW, Howlett J, Januzzi JL, Zowall H, Canadian Multicenter Improved Management of Patients With Congestive Heart Failure (IMPROVE-CHF) Study Investigators. N-terminal pro-B-type natriuretic peptide testing improves the management of patients with suspected acute heart failure: primary results of the Canadian prospective randomized multicenter IMPROVE-CHF study. Circulation. 2007;115(24):3103–10.
Dickstein K, Cohen-Solal A, Filippatos G, McMurray JJ, Ponikowski P, Poole-Wilson PA, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). Eur Heart J. 2008;29(19):2388–442.
Maisel A, Hollander JE, Guss D, McCullough P, Nowak R, Green G, et al. A multicenter study of B-type natriuretic peptide levels, emergency department decision making, and outcomes in patients presenting with shortness of breath. J Am Coll Cardiol. 2004;44(6):1328–33.
Metra M, Nodari S, Parrinello G, Specchia C, Brentana L, Rocca P, et al. The role of plasma biomarkers in acute heart failure. Serial changes and independent prognostic value of NT-proBNP and cardiac troponin-T. Eur J Heart Fail. 2007;9(8):776–86.
Noveanu M, Breidthardt T, Potocki M, Reichlin T, Twerenbold R, Uthoff H, et al. Direct comparison of serial B-type natriuretic peptide and NT-proBNP levels for prediction of short- and long-term outcome in acute decompensated heart failure. Crit Care. 2011;15(1):R1.
Di Somma S, Magrini L, Pittoni V, Marino R, Mastrantuono A, Ferri E, et al. In-hospital percentage BNP reduction is highly predictive for adverse events in patients admitted for acute heart failure: the Italian RED Study. Crit Care. 2010;14(3):R116.
Jan A, Murphy NF, O'Loughlin C, Ledwidge M, McDonald K. Profiling B-type natriuretic peptide in a stable heart failure population: a valuable adjunct to care. Ir J Med Sci. 2011;180(2):355–62.
Macheret F, Boerrigter G, McKie P, Costello-Boerrigter L, Lahr B, Heublein D, et al. Pro-B-type natriuretic peptide(1-108) circulates in the general community: plasma determinants and detection of left ventricular dysfunction. J Am Coll Cardiol. 2011 Mar 22;57(12):1386–95.
Gaggin HK, Mohammed AA, Bhardwaj A, Rehman SU, Gregory SA, Weiner RB, et al. Heart Failure Outcomes and Benefits of NT-proBNP-Guided Management in the Elderly: Results From the Prospective, Randomized ProBNP Outpatient Tailored Chronic Heart Failure Therapy (PROTECT) Study. J Card Fail. 2012 Aug;18(8):626–34.
Valle R, Aspromonte N, Milani L, Peacock FW, Maisel AS, Santini M, et al. Optimizing fluid management in patients with acute decompensated heart failure (ADHF): the emerging role of combined measurement of body hydration status and brain natriuretic peptide (BNP) levels. Heart Fail Rev. 2011 Nov;16(6):519–29.
• Januzzi Jr JL. The role of natriuretic peptide testing in guiding chronic heart failure management: review of available data and recommendations for use. Arch Cardiovasc Dis. 2012;105(1):40–50. This review provides insights into natriuretic peptide goal directed therapy in heart failure, highlighting the importance of reducing natriuretic peptide levels in order to chart progression of heart failure treatment.
Xu D, Chan WL, Leung BP, et al. Selective expression of a stable cell surface molecule on type 2 but not type 1 helper T cells. J Exp Med. 1998;187:787–94.
Townsend MJ, Fallon PG, Matthews DJ, et al. T1/ST2-deficient mice demonstrate the importance of T1/ST2 in developing primary T helper cell type 2 responses. J Exp Med. 2000;191:1069–76.
Schmitz J, Owyeng A, Oldham E, et al. IL-33, an interleukin-1-like cytokine that signals via the IL-1 receptor-related protein ST2 and induces T helper type 2-associated cytokines. Immunity. 2005;23:479–90.
Wang TJ, Wollert KC, Larson MG, et al. Prognostic utility of novel biomarkers of cardiovascular stress: the framingham heart study. Circulation. 2012;126:1596–604.
Sanada S, Hakuno D, Higgins LJ, et al. IL-33 and ST2 comprise a critical biomechanically induced and cardioprotective signaling system. J Clin Invest. 2007;117:1538–49.
Oshikawa K, Kuroiwa K, Tago K, et al. Elevated soluble ST2 protein levels in sera of patients with asthma with an acute exacerbation. Am J Respir Crit Care Med. 2001;164:277–81.
Oshikawa K, Yanagisawa K, Tominaga S, et al. ST2 protein induced by inflammatory stimuli can modulate acute lung inflammation. Biochem Biophys Res Commun. 2002;299:18–24.
Tajima S, Oshikawa K, Tominaga S, et al. The increase in serum soluble ST2 protein upon acute exacerbation of idiopathic pulmonary fibrosis. Chest. 2003;124:1206–14.
Oshikawa K, Kuroiwa K, Tokunaga T, et al. Acute eosinophilic pneumonia with increased soluble ST2 in serum and bronchoalveolar lavage fluid. Respir Med. 2001;95:532–3.
Martinez-Rumayor A, Camargo CA, Green SM, et al. Soluble ST2 plasma concentrations predict 1-year mortality in acutely dyspneic emergency department patients with pulmonary disease. Am J Clin Pathol. 2008;130:578–84.
Shimpo M, Morrow DA, Weinberg EO, et al. Serum levels of the interleukin-1 receptor family member ST2 predict mortality and clinical outcome in acute myocardial infarction. Circulation. 2004;109:2186–90.
Dieplinger B, Januzzi Jr JL, Steinmair M, et al. Analytical and clinical evaluation of a novel high-sensitivity assay for measurement of soluble ST2 in human plasma–the Presage ST2 assay. Clin Chim Acta. 2009;409:33–40.
Weinberg EO, Shimpo M, Hurwitz S, et al. Identification of serum soluble ST2 receptor as a novel heart failure biomarker. Circulation. 2003;107:721–6.
Shah RV, Chen-Tournoux AA, Picard MH, et al. Serum levels of the interleukin-1 receptor family member ST2, cardiac structure and function, and long-term mortality in patients with acute dyspnea. Circ Heart Fail. 2009;2:311–9.
Ky B, French B, McCloskey K, et al. High-sensitivity ST2 for prediction of adverse outcomes in chronic heart failure. Circ Heart Fail. 2011;4:180–7.
Bayes-Genis A, Pascual-Figal D, Januzzi JL, et al. Soluble ST2 monitoring provides additional risk stratification for outpatients with decompensated heart failure. Rev Esp Cardiol. 2010;63:1171–8.
Sabatine MS, Morrow DA, Higgins LJ, et al. Complementary roles for biomarkers of biomechanical strain ST2 and N-terminal prohormone B-type natriuretic peptide in patients with ST-elevation myocardial infarction. Circulation. 2008;15(117):1936–44.
Kohli P, Bonaca MP, Kakkar R, et al. Role of ST2 in non-ST-elevation acute coronary syndrome in the MERLIN-TIMI 36 trial. Clin Chem. 2012 Jan;58(1):257–66.
Weir RA, Miller AM, Murphy GE, et al. Serum soluble ST2: a potential novel mediator in left ventricular and infarct remodeling after acute myocardial infarction. J Am Coll Cardiol. 2010;55:243–50.
Januzzi Jr JL, Peacock WF, Maisel AS, et al. Measurement of the interleukin family member ST2 in patients with acute dyspnea: results from the PRIDE (Pro-Brain Natriuretic Peptide Investigation of Dyspnea in the Emergency Department) study. J Am Coll Cardiol. 2007;50:607–13.
Socrates T. deFilippi C, Reichlin T et al. Interleukin family member ST2 and mortality in acute dyspnoea. J Intern Med. 2010;268:493–500.
Shah KB, Kop WJ, Christenson RH, et al. Prognostic utility of ST2 in patients with acute dyspnea and preserved left ventricular ejection fraction. Clin Chem. 2011;57:874–82.
Daniels LB, Clopton P, Iqbal N, et al. Association of ST2 levels with cardiac structure and function and mortality in outpatients. Am Heart J. 2010;160:721–8.
White HD. Pathobiology of troponin elevations: do elevations occur with myocardial ischemia as well as necrosis? J Am Coll Cardiol. 2011;57:2406–8.
McDonough JL, Arrell DK, Van Eyk JE. Troponin I degradation and covalent complex formation accompanies myocardial ischemia/reperfusion injury. Circ Res. 1999;84:9–20.
Hessel MH, Atsma DE, van der Valk EJ, et al. Release of cardiac troponin I from viable cardiomyocytes is mediated by integrin stimulation. Pflugers Arch. 2008;455:979–86.
Daubert MA, Jeremias A. The utility of troponin measurement to detect myocardial infarction: review of the current findings. Vasc Health Risk Manag. 2010;6:691–9.
Thygesen K, Mair J, Katus H, et al. Recommendations for the use of cardiac troponin measurement in acute cardiac care. Eur Heart J. 2010;31:2197–204.
Katz SD, Hryniewicz K, Hriljac I, et al. Vascular endothelial dysfunction and mortality risk in patients with chronic heart failure. Circulation. 2005;111:310–4.
Kociol RD, Pang PS, Gheorghiade M, et al. Troponin elevation in heart failure prevalence, mechanisms, and clinical implications. J Am Coll Cardiol. 2010;56:1071–8.
Januzzi JL, Filippatos G, Nieminen M, et al. Troponin elevation in patients with heart failure: on behalf of the third Universal Definition of Myocardial Infarction Global Task Force: Heart Failure Section. Eur Heart J. 2012;33:2265–71.
Missov M, Mair J. A novel biochemical approach to congestive heart failure: cardiac troponin T. Am Heart J. 1999;139:95–9.
Latini R, Masson S, Anand IS, et al. Prognostic value of very low plasma concentrations of troponin T in patients with stable chronic heart failure. Circulation. 2007;116:1242–9.
Miller WL, Hartman KA, Burritt MF, et al. Serial biomarker measurements in ambulatory patients with chronic heart failure: the importance of change over time. Circulation. 2007;116:249–57.
Gattis WA, O'Connor CM, Hasselblad V, et al. Usefulness of an elevated troponin-I in predicting clinical events in patients admitted with acute heart failure and acute coronary syndrome (from the RITZ-4 trial). Am J Cardiol. 2004;93:1436–7.
Miller WL, Hartman KA, Burritt MF, et al. Profiles of serial changes in cardiac troponin T concentrations and outcome in ambulatory patients with chronic heart failure. J Am Coll Cardiol. 2009;54:1715–21.
Sundstrom J, Ingelsson E, Berglund L, et al. Cardiac troponin-I and risk of heart failure: a community-based cohort study. Eur Heart J. 2009;30:773–81.
Peacock WF, De Marco T, Fonarow GC, et al. Cardiac troponin and outcome in acute heart failure. N Engl J Med. 2008;358:2117–26.
Biolo A, Fisch M, Balog J, et al. Episodes of acute heart failure syndrome are associated with increased levels of troponin and extracellular matrix markers. Circ Heart Fail. 2010;3:44–50.
You JJ, Austin PC, Alter DA, et al. Relation between cardiac troponin I and mortality in acute decompensated heart failure. Am Heart J. 2007;153:462–70.
Metra M, Nodari S, Parrinello G, et al. The role of plasma biomarkers in acute heart failure: Serial changes and independent prognostic value of NT-proBNP and cardiac troponin-T. Eur J Heart Fail. 2007;9:776–86.
Xue Y, Clopton P, Peacock WF, et al. Serial changes in high-sensitive troponin predict outcome in patients with decompensated heart failure. Eur J Heart Fail. 2011;13:37–42.
de Boer RA, Voors AA, Muntendam P, van Gilst WH, van Veldhuisen DJ. Galectin-3: a novel mediator of heart failure development and progression. Eur J Heart Fail. 2009 Sep;11(9):811–7.
Ho JE, Liu C, Lyass A, Courchesne P, Pencina MJ, Vasan RS, et al. Galectin-3, a Marker of Cardiac Fibrosis, Predicts Incident Heart Failure in the Community. J Am Coll Cardiol. 2012 Oct 2;60(14):1249–56.
de Boer RA, Lok DJ, Jaarsma T, van der Meer P, Voors AA, Hillege HL, et al. Predictive value of plasma galectin-3 levels in heart failure with reduced and preserved ejection fraction. Ann Med. 2011 Feb;43(1):60–8.
McCullough PA, Olobatoke A, Vanhecke TE. Galectin-3: a novel blood test for the evaluation and management of patients with heart failure. Rev Cardiovasc Med. 2011;12(4):200–10.
Shah RV, Chen-Tournoux AA, Picard MH, van Kimmenade RR, Januzzi JL. Galectin-3, cardiac structure and function, and long-term mortality in patients with acutely decompensated heart failure. Eur J Heart Fail. 2010 Aug;12(8):826–32.
La'ulu SL, Apple FS, Murakami MM, Ler R, Roberts WL, Straseski JA. Performance Characteristics of the ARCHITECT Galectin-3 Assay. Clin Biochem. 2013 Jan;46(1–2):119–22.
Jougasaki M, Burnett Jr JC. Adrenomedullin: potential in physiology and pathophysiology. Life Sci. 2000;66:855–72.
Maisel A, Mueller C, Nowak R, Peacock WF, Landsberg JW, Ponikowski P, et al. Mid-region pro-hormone markers for diagnosis and prognosis in acute dyspnea: results from the BACH (Biomarkers in Acute Heart Failure) trial. J Am Coll Cardiol. 2010 May 11;55(19):2062–76.
Maisel A, Mueller C, Nowak RM, Peacock WF, Ponikowski P, Mockel M, et al. Midregion prohormone adrenomedullin and prognosis in patients presenting with acute dyspnea: results from the BACH (Biomarkers in Acute Heart Failure) trial. J Am Coll Cardiol. 2011 Aug 30;58(10):1057–67.
von Haehling S, Filippatos GS, Papassotiriou J, Cicoira M, Jankowska EA, Doehner W, et al. Mid-regional pro-adrenomedullin as a novel predictor of mortality in patients with chronic heart failure. Eur J Heart Fail. 2010 May;12(5):484–91.
Masson S, Latini R, Carbonieri E, Moretti L, Rossi MG, Ciricugno S, et al. The predictive value of stable precursor fragments of vasoactive peptides in patients with chronic heart failure: data from the GISSI-heart failure (GISSI-HF) trial. Eur J Heart Fail. 2010;12(4):338–47.
Morgenthaler NG, Struck J, Alonso C, Bergman A. Assay for the measurement of copeptin, a stable peptide derived from the precursor of vasopressin. Clin Chem. 2006;52:112–9.
Stoiser B et al. Copeptin, a fragment of the vasopressin precursor, as a novel predictor of outcome in heart failure. Eur J Clin Invest. 2006;36:771–8.
Szinnai G, Morgenthaler NG, Berneis K, et al. Changes in plasma copeptin, the c-terminal portion of arginine vasopressin during water deprivation and excess in healthy subjects. J Clin Endocrinol Metab. 2007;92:3973–8.
Chatterjee K. Neurohormonal activation in congestive heart failure and the role of vasopressin. Am J Cardiol. 2005;95:8B–13.
Voors AA, von Haehling S, Anker SD, et al. OPTIMA- AL Investigators. C-terminal provasopressin (copeptin) is a strong prognostic marker in patients with heart failure after an acute myocardial infarction: results from the OPTIMAAL study. Eur Heart J. 2009;30:1187–94.
Kelly D, Squire IB, Khan SQ, et al. C-terminal provasopressin (copeptin) is associated with left ventricular dysfunction, remo- deling, and clinical heart failure in survivors of myocardial infarction. J Card Fail. 2008;14:739–45.
Maisel A, Xue Y, Shah K, et al. Increased 90-Day Mortality in Patients With Acute Heart Failure With Elevated Copeptin: Secondary Results From the Biomarkers in Acute Heart Failure (BACH) Study. Circ Heart Fail. 2011;4:613–20.
Meijer E, Bakker SJ, Halbesma N, et al. Copeptin, a surrogate marker of vasopressin, is associated with microalbuminuria in a large population cohort. Kidney Int. 2010;77:29–36.
Górriz Teruel JL, Beltrán CS. Assessment of renal function, iatrogenic hyperkalemia and acute renal dysfunction in cardiology. Contrast-induced nephropathy. Rev Esp Cardiol. 2011 Dec;64(12):1182–92.
Smith GL, Lichtman JH, Bracken MB, Shlipak MG, Phillips CO, DiCapua P, et al. Renal impairment and outcomes in heart failure: systematic review and meta-analysis. J Am Coll Cardiol. 2006 May 16;47(10):1987–96.
•• Ronco C, McCullough P, Anker SD, Anand I, Aspromonte N, Bagshaw SM, et al. Cardio-renal syndromes: Report from the consensus conference of the acute dialysis quality initiative. Eur Heart J. 2010;31:703–11. This review provides a good understanding of the underlying pathophysiology in patients with heart failure and concomitant renal dysfunction, namely the cardiorenal syndromes.
Roger VL, Go AS, Lloyd-Jones DM, Adams RJ, Berry JD, Brown TM, et al. Heart disease and stroke statistics--2011 update: a report from the American Heart Association. Circulation. 2011;123(4):e18–209.
Iwanaga Y, Miyazaki S. Heart failure, chronic kidney disease, and biomarkers–an integrated viewpoint–. Circ J. 2010 Jul;74(7):1274–82.
Ix JH, Shlipak MG, Chertow GM, Whooley MA. Association of cystatinC with mortality, cardiovascular events, and incident heart failure amongpersons with coronary heart disease: data from the Heart and Soul Study. Circulation. 2007;115:173–9.
Shlipak MG, Wassel Fyr CL, Chertow GM, Harris TB, Kritchevsky SB, Tylavsky FA, et al. Cystatin C and mortality risk in the elderly: the Health, Aging, and BodyComposition Study. J Am Soc Nephrol. 2006;17:254–61.
Shlipak MG, Katz R, Kestenbaum B, Fried LF, Siscovick D, Sarnak MJ. Clinical and subclinical cardiovascular disease and kidney function decline in the elderly. Atherosclerosis. 2009;204:298–303.
Koenig W, Twardella D, Brenner H, Rothenbacher D. Plasma concentrationsof cystatin C in patients with coronary heart disease and risk for secondary cardiovascular events: more than simply a marker of glomerular filtration rate. Clin Chem. 2005;51:321–7.
Lassus J, Harjola VP, Sund R, Siiril-Waris K, Melin J, Peuhkurinen K, et al. Prognostic value of cystatin C in acute heart failure in relation to other markers of renal function and NT-proBNP. Eur Heart J. 2007;28:1841–7.
Carrasco-Sánchez FJ, Galisteo-Almeda L, Páez-Rubio I, Martínez-Marcos FJ, Camacho-Vázquez C, Ruiz-Frutos C, et al. Prognostic value of cystatin C on admission in heart failure with preserved ejection fraction. J Card Fail. 2011;17(1):31–8.
Patel PC, Ayers CR, Murphy SA, Peshock R, Khera A, de Lemos JA, et al. Association of cystatin C with left ventricular structure and function: The Dallas Heart Study. Circ Heart Fail. 2009;2:98–104.
Kjeldsen L, Johnsen AH, Sengelov H, Borregaard N. Isolation and primary structure of NGAL, a novel protein associated with human neutrophil gelatinase. J Biol Chem. 1993;268:10425–32.
Mishra J, Dent C, Tarabishi R, Tarabishi R, Mitsnefes M, Kelly C, et al. Neutrophil gelatinase-associated lipocalin (NGAL) as a biomarker for acute renal injury after cardiac surgery. Lancet. 2005;365:1231–8.
Yndestad A, Landrø L, Ueland T, Dahl CP, Flo TH, Vinge LE, et al. Increased systemic and myocardial expression of neutrophil gelatinase-associated lipocalin in clinical and experimental heart failure. Eur Heart J. 2009 May;30(10):1229–36.
Latouche C, El Moghrabi S, Messaoudi S, Nguyen Dinh Cat A, Hernandez-Diaz I, Alvarez de la Rosa D, et al. Neutrophil gelatinase-associated lipocalin is a novel mineralocorticoid target in the cardiovascular system. Hypertension. 2012;59(5):966–72.
Maisel AS, Mueller C, Fitzgerald R, Brikhan R, Hiestand BC, Iqbal N, et al. Prognostic utility of plasma neutrophil gelatinase-associated lipocalin in patients with acute heart failure: the NGAL EvaLuation Along with B-type NaTriuretic Peptide in acutely decompensated heart failure (GALLANT) trial. Eur J Heart Fail. 2011 Aug;13(8):846–51.
Shrestha K, Shao Z, Singh D, Dupont M, Tang WH. Relation of systemic and urinary neutrophil gelatinase-associated lipocalin levels to different aspects of impaired renal function in patients with acute decompensated heart failure. Am J Cardiol. 2012 Nov 1;110(9):1329–35.
Damman K, van Veldhuisen DJ, Navis G, Voors AA, Hillege HL. Urinary neutrophil gelatinase associated lipocalin (NGAL), a marker of tubular damage, is increased in patients with chronic heart failure. Eur J Heart Fail. 2008;10:997–1000.
Ichimura T, Hung CC, Yang SA, Stevens JL, Bonventre JV. Kidney injury molecule-1: a tissue and urinary biomarker for nephrotoxicant-induced renal injury. Am J Physiol Renal Physiol. 2004;286(3):F552–63.
Devarajan P. Biomarkers for the early detection of acute kidney injury. Curr Opin Pediatr. 2011;23:194–200.
Przybylowski P, Malyszko J, Kozlowska S, Malyszko JS. Kidney Injury Molecule-1 Correlates with Kidney Function in Heart Allograft Recipients. Transplant Proc. 2011;43:3061–3.
Éndre ZH, Pickering JW, Walker RJ, Devarajan P, et al. Improved performance of urinary biomarkers of acute kidney injury in the critically ill by stratification for injury duration and baseline renal function. Kidney Int. 2011;79:1119–30.
Krawczeski CD, Goldstein SL, Woo JG, Wang Y, et al. Temporal relationship and predictive value of urinary acute kidney injury biomarkers after pediatric cardiopulmonary bypass. J Am Coll Cardiol. 2011;58:2301–9.
Nickolas TL, Schmidt-Ott KM, Canetta P, Forster C, Singer E, et al. Diagnostic and prognostic stratification in the emergency department using urinary biomarkers of nephron damage. J Am Coll Cardiol. 2012;59:246–55.
Jungbauer CG, Birner C, Jung B, Buchner S, Lubnow M, von Bary C, et al. Kidney injury molecule-1 and N-acetyl-β-D-glucosaminidase in chronic heart failure: possible biomarkers of cardiorenal syndrome. Eur J Heart Fail. 2011 Oct;13(10):1104–10.
Tubular damage in chronic systolic heart failure is associated with reduced survival independent of glomerular filtration rate.. Damman K, Van Veldhuisen DJ, Navis G, Vaidya VS, Smilde TD, Westenbrink BD, Bonventre JV, Voors AA, Hillege HL. Heart. 2010 Aug;96(16):1297-302.
Acknowledgments
Research support for this paper was provided by Alere, Abbott, Nanosphere, Brahms-thermofisher, and Novartis.
Conflict of Interest
Punam Chowdhury declares that he has no conflict of interest.
Devin Kehl declares that he has no conflict of interest.
Rajiv Choudhary declares that he has no conflict of interest.
Alan Maisel has been a consultant for Alere, BG Medicine, and Critical Diagnostics; has received grant support from BG Medicine and Alere; has received payment for development of educational presentations including service on speakers’ bureaus for BG Medicine; and has received travel/accommodations expenses covered or reimbursed from multiple companies.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Congestive Heart Failure
Rights and permissions
About this article
Cite this article
Chowdhury, P., Kehl, D., Choudhary, R. et al. The Use of Biomarkers in the Patient with Heart Failure. Curr Cardiol Rep 15, 372 (2013). https://doi.org/10.1007/s11886-013-0372-4
Published:
DOI: https://doi.org/10.1007/s11886-013-0372-4