Abstract
Over the past several years, there have been a significant number of new agents developed for the treatment of type 2 diabetes. Our goal in this article is to review the cardiovascular effects (risks and benefits) of these oral and non-insulin injectable agents. We review six major categories of diabetic therapies: biguanides, sulfonylureas, alpha-glucosidase inhibitors, thiazolidinediones, GLP-1 agonists, and DPP-IV inhibitors. In order to achieve a personalized regimen that aims for optimal outcomes, we must take into consideration each drug’s side effects, patients’ cardiovascular risk factors, and their individual health profile.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes affects 25.8 million people in the United States (8.3 % of the US population) and is currently the 7th leading cause of death. The major cause of death in these patients (>65 %) is due to cardiovascular disease and the total diabetes cost in the US is estimated to be approximately $174 billion/year [1]. Given the significant morbidity and mortality of diabetes and its related complications, it is clear to see why proper treatment of this disease is so crucial. Over the past few years, there have been a significant number of new agents developed for the treatment of type 2 diabetes. Our goal in this paper is to review the cardiovascular effects (risks and benefits) of these oral and non-insulin injectable agents.
Although our goal for diabetic patients seems to be focused on getting A1c and glucose values at target, the ultimate objective should be to reduce mortality and risk of micro and macro-vascular complications [2]. As evidence-based medicine teaches us, we should not simply look at laboratory values as our endpoints, but rather consider outcomes such as cardiovascular events and all-cause mortality. Recent clinical trials have dramatically changed the way we treat diabetes by revealing that aggressively reducing A1c below the recommended range (<7 %) does not necessarily have any beneficial impact on cardiovascular benefits, and that very tight control may actually increase mortality [3, 4]. Since the answer to reducing cardiovascular disease in diabetic patients may not merely lie in strict glucose control, we reviewed other characteristics of anti-diabetic agents that may help patients’ cardiovascular profiles independent of glucose control.
Biguanides
The most studied and widely used of the biguanide class is metformin. It has several unique properties that make it efficacious both as monotherapy and in combination with other diabetes treatments. The major effects of metformin include reduction of gluconeogenesis, increase in insulin sensitivity, and modulation of endothelial dysfunction. Metformin decreases insulin resistance by increasing insulin-mediated glucose uptake in skeletal muscle and adipocytes.
The underlying mechanism by which metformin exerts many of its effects is through activation of AMP kinase, which inhibits degradation of AMP, increasing the ratio of AMP to ATP. This inhibits mitochondrial respiration in hepatocytes, thereby reducing gluconeogenesis and excess plasma glucose. At the level of the endothelium, this increase in AMP also activates endothelial nitric oxide synthase (eNOS), which increases nitric oxide and endothelial vasodilation. Activation of AMP by metformin has been shown to prevent myocardial reperfusion injury, limit infarct size, reduce collagen expression, prevent cardiac fibrosis, and preserve myocardial viability through inhibition of apoptosis, thereby preventing cardiac remodeling and heart failure. In fact, studies in rat models show administration of metformin immediately before reperfusion of coronary vessels can reduce infarct size by up to 50 %, an effect called metabolic pre-conditioning. Metformin also directly activates the Akt pathway and the adenosine receptor independent of AMP kinase. In vitro studies of human cells have shown metformin decreases growth of smooth muscle cells and fibroblasts, decreases proliferation of hypoxic endothelial cells, and decreases synthesis of CAD-associated PAI-1 [5•].
Metformin improves several cardiovascular risk factors. It stimulates oxidation of free fatty acids, which decreases plasma free fatty acids, decreases total cholesterol up to 17 %, decreases triglycerides up to 25-40 %, decreases LDL up to 9-24 %, and increases HDL by 15-20 %, often independent of improvement in glycemic control [6]. Although data are somewhat inconsistent, metformin has generally been shown to improve blood pressure, particularly diastolic. Metformin prevents weight gain in combination with sulfonylureas and insulin, and may cause modest weight loss (1-3 kg) in obese patients. The mechanism is unclear, but may in part be due to malabsorption, increased utilization of carbohydrates, or adverse gastrointestinal effects [5•].
The landmark study of the cardiovascular benefits of metformin was the UKPDS (n = 753), a prospective, randomized multicenter trial. Type 2 diabetes patients were assigned to conventional lifestyle modification or intensive treatment with metformin, sulfonylureas or insulin. At 10 year follow up, there was a 36 % risk reduction in all-cause mortality in the metformin vs. conventional group. There was also a 39 % risk reduction in myocardial infarction and 30 % risk reduction in composite macrovascular outcomes (MI, sudden death, angina, stroke, peripheral artery disease) with metformin, but this difference was not statistically different than the other intensive treatment group. Similar results were seen in a randomized controlled trial (n = 390) of diabetic patients already on insulin, with a 39 % risk reduction in macrovascular endpoints with metformin vs. placebo, (NNT = 16) [7]. A meta-analysis of 40 randomized controlled trials also showed a 26 % relative risk reduction in cardiovascular mortality with metformin versus any other oral diabetic medication or placebo [8••].
In patients with diabetes and preexisting cardiovascular disease, there is lower mortality with metformin vs. sulfonylureas [5•]. In a large retrospective study of all adult Danish residents on metformin vs. sulfonylurea monotherapy (n = 107,806), metformin was associated with 19-40 % lower risk of all-cause and cardiovascular mortality in those without previous MI, and in those with previous MI (n = 9607), there was 30-53 % lower risk of mortality with metformin vs. sulfonylureas [9].
There is growing evidence that metformin is particularly beneficial in heart failure. However metformin is often withheld in heart failure due to concern for lactic acidosis, although increased risk in this population has not been proven. In the Reduction of Atherothrombosis for Continued Health (REACH) registry (n = 19,691), patients with diabetes and history of atherothrombosis had a 34 % lower risk of all-cause mortality, including among subgroups with congestive heart failure, age >65 years, and CrCl 35–60 ml/min [10]. In a retrospective cohort study of diabetic patients on oral monotherapy (n = 5631), patients on metformin had a 24 % lower risk of developing heart failure than with sulfonylureas. The risk was also higher with high vs. low dose sulfonylureas [11]. A meta-analysis of oral agents vs. insulin in diabetics with heart failure showed metformin was the only medication that was associated with lower rates of hospitalization. Metformin was also correlated to lower all-cause mortality compared to other oral agents and insulin [12].
One of the major goals of diabetes treatment is to prevent macrovascular complications. Current guidelines from the American Diabetes Association recommend metformin as a first-line agent for the treatment of type 2 diabetes. Although there is strong evidence that metformin provides cardiovascular protection, there have been few prospective randomized trials of metformin since the UKPDS. The molecular mechanisms by which metformin exerts cardiovascular protection are currently under investigation.
Sulfonylureas
The sulfonylureas are insulin secretogogues that have been used for diabetes since the 1960s. The safety profile of older generation agents (tolbutamide, chlorpropamide) had been questioned after the University Group Diabetes Program (UGDP) trial found increased cardiovascular deaths associated with tolbutamide, although this result might have been confounded by differences in baseline characteristics. The newer generation sulfonylureas (glipizide, glyburide, glimeperide, gliclazide, meglintides) are the subject of continuing research, especially with regard to cardiovascular outcomes. For example, in a retrospective matched case control study (n = 76 vs. 152 controls), patients who developed coronary artery disease were more than two times more likely to be on sulfonylureas (2.4× with glibenclamide, 2× with glipizide, 2.9× with either) than controls [13].
Sulfonylureas inhibit ATP-sensitive potassium channels in beta cells, which leads to depolarization, opening of Ca-gated channels, and Ca-dependent release of insulin by exocytosis. These ATP-sensitive potassium channels are also present in cardiac myocytes. Normally, intracellular ATP keeps these channels closed. In the presence of chronic ischemia, anaerobic metabolites increase the resistance of these channels to ATP, a mechanism that is cardioprotective called pre-conditioning. However, in the presence of sulfonylureas this pre-conditioning adaptation is blunted, which is thought to be why patients on sulfonylureas are prone to more arrhythmias and larger infarct size with myocardial ischemia.
Tolbutamide, chlorpropamide, gliclazide, and glipizide are the so-called pancreatic-specific sulfonylureas, whereas glibenclamide and glimeperide are tissue non-specific [14]. There is conflicting data on whether these differences have meaningful cardiovascular consequences. In a retrospective analysis, diabetic patients (n = 3331) on pancreatic-specific sulfonylureas had no difference in mortality compared to those on non-specific sulfonylureas [15]. Comparing glipizide, glimeperide, and glyburide, there was no significant difference in mortality in a retrospective analysis (n = 11,141), although there was a trend to mortality benefit with glimepiride [16]. In a retrospective analysis, mortality among patients (n = 3477) hospitalized for congestive heart failure was not different between sulfonylureas: glimperide, glipizide, glyburide, glicazide, or tolbutamide [17]. There are conflicting data on the relative cardiovascular effects of meglintides (nateglinide, repaglinide) vs. sulfonylureas.
On the other hand, glibenclamide may be more harmful in chronic ischemia than other sulfonylureas. In a randomized controlled trial, glibenclamide impaired ischemic pre-conditioning and increased cardiac pain compared to placebo [18]. This was also confirmed in a randomized controlled trial (n = 45) of patients with stable coronary artery disease, showing glibenclamide impaired cardiac pre-conditioning more than glimeperide and placebo [19]. In-hospital mortality of patients admitted for myocardial infarction (n = 1310) has also been shown to be greater with glibenclamide vs. gliclazide or glimepiride [20].
Another major morbidity tied to sulfonylureas is hypoglycemia. There is concern that recurrent hypoglycemia can increase risk of cardiovascular events. In the landmark UKPDS trial (n = 753) of obese diabetic patients, glibenclamide was associated with a 2.5 % risk of major hypoglycemic event vs. 0.7 % in the conventional (diet-controlled) group [21]. A meta-analysis of 21 studies found glyburide was associated with a 53 % higher risk of hypoglycemia than all other secretagogues, and an 83 % increased risk of hypoglycemia compared to other sulfonylureas, although there was no difference in cardiovascular outcomes [22].
There does seem to be an increased risk of mortality and cardiovascular disease with sulfonylureas compared to metformin. A retrospective analysis of patients (n = 23,915) starting monotherapy with metformin vs. sulfonylureas found a 59-68 % increased risk of mortality with sulfonylureas. Among patients with pre-existing coronary artery disease, glyburide had a 38 % and glipizide a 41 % increased risk of mortality [23•]. Several other retrospective studies of sulfonylureas have shown similar results that are dose-dependent. Another retrospective analysis of patients (n = 5730) on monotherapy found a 43 % increased all-cause mortality and 70 % increased cardiovascular mortality with sulfonylureas vs. metformin. Patients on metformin/sulfonylurea combination therapy have been shown to have even higher mortality, although results from other studies of combination therapy are mixed [24].
Careful consideration should be given to patients with high risk or existing cardiovascular disease being prescribed sulfonylureas. Sulfonylureas are often initiated to avoid the inconvenience of injectable insulin. However like insulin, they pose the risk of hypoglycemia. They may also paradoxically increase adverse cardiovascular outcomes through inhibition of cardiac pre-conditioning, even though their ultimate purpose is to reduce risk of macrovascular and microvascular complications of hyperglycemia. Further prospective trials need to be done with careful adjustment for baseline characteristics to elucidate whether the long-term benefits of sulfonylurea treatment outweigh the risks.
Thiazolidinediones
Another major class of oral agents used for the treatment of diabetes includes thiazolidinediones (TZDs), which are peroxisome proliferator-activated receptor gamma (PPAR-r) agonists. These agents lower glucose predominantly by increasing insulin sensitivity in peripheral tissues [25] and may slow the progression of beta cell failure [26]. They are known to lower A1c by approximately 0.5-1.4 % [27]. The three drugs in this category that have been introduced in the United States are troglitazone, rosiglitazone, and pioglitazone. Of these three, troglitazone was removed from the market in 2000 due to hepatoxicity, and rosiglitazone and pioglitazone both have black box warnings due to being linked with congestive heart failure. Because of recent studies, there has been a great deal of skepticism in using TZDs mostly due to concern of congestive heart failure and increased risk of myocardial infarction with rosiglitazone and now a concern of bladder cancer with pioglitazone. Surprisingly, according to the AHA/ADA consensus statement on TZD use, the beneficial effects of TZDs on cardiovascular risk factors actually make them attractive agents for type 2 diabetics who are at high risk for cardiovascular disease [28].
TZDs are unique in that they decrease insulin resistance at the level of the peripheral tissue, which is important, because in epidemiologic studies, insulin resistance has been associated with hypertension [29]. Thus, it may be inferred that TZDs should have a positive effect in lowering blood pressure. In a meta-analysis of 37 trials conducted by Qayyum and Adomaityte, it was found that when compared with baseline, TZDs lowered SBP by 4.70 mmHg and DBP by 3.78 mmHg; and when compared to controls, TZDs lowered SBP by 3.47 mmHg and DBP by 1.84 mmHg [30]. The exact mechanism of why this occurs is not known, and it is unclear how clinically significant this decrease is.
In regards to effects on lipid profile, rosiglitazone has been shown to reduce triglyceride levels by 39 % in one study [31], however increased by 15 % in another study comparing rosiglitazone with pioglitazone [32]. Pioglitazone decreased triglycerides by 15 % in that study [32]. Both pioglitazone and rosiglitazone have been shown to increase HDL level by approximately 8-15 %, with pioglitazone having better effects [32]. They both increase LDL level as well by approximately 16-23 % with pioglitazone causing less of an increase; however the nature of the LDL particles changes from small to the large, less atherogenic forms [32]. These alterations in the lipid profile become significant since a large number of our diabetic population also has co-existing hyperlipidemia. TZDs have been shown to reduce levels of inflammatory markers such as tumor necrosis factor-alpha and resistin, and increase levels of adiponectin, all of which beneficially affect the cardiovascular profile as well [33].
Given the concern of TZDs causing an increase in edema and CHF, it is important to take a look at the incidence of these side effects. Based on the consensus statement from the American Heart Association and American Diabetes Association, it is noted that when used as monotherapy, the incidence of edema with TZDs ranges from 3-5 % and is greater when used with sulfonylureas (7.5 % vs. 2.1 % on SU alone). There is also a significant increase in edema when using TZDs in addition to insulin (13-16 % vs. 4-7 % in those taking insulin alone). The incidence of CHF is actually much lower than expected. It was found to be <1 % for rosiglitazone monotherapy and 2-3 % when used with insulin vs. 1.1 % for pioglitazone monotherapy and combination with insulin [28]. While not an insignificant increase in edema and heart failure, it is important to note that we should not completely avoid using TZDs altogether based on these concerns alone.
While it is interesting to see the individual effects of TZDs on cardiovascular markers, the most important determinant of whether drugs have beneficial long term effects is to look at endpoints such as cardiovascular events and mortality. In the PROACTIVE trial, which included 5238 patients with type 2 DM and known cardiovascular disease randomized to placebo vs. pioglitazone, the primary outcome was composite of CVD events. While the primary outcome was only insignificantly reduced with the pioglitazone group, the secondary outcome (all cause mortality, non-fatal MI, and stroke) was significantly reduced by 16 % in the pioglitazone group [34]. Another major randomized control trial, the PERISCOPE trial, found that pioglitazone significantly lowered the rate of coronary atherosclerosis progression (as measured by intravascular ultrasound) when compared to glimepiride [35].
Rosiglitazone, unfortunately, has not had the same positive findings. In a meta-analysis of 42 trials, it was discovered that rosiglitazone was actually associated with a statistically significant increase in risk of MI and borderline significant increase in cardiovascular mortality, with odds ratios of 1.43 and 1.62, respectively [36]. When deciding to choose a TZD for diabetes therapy, rosiglitazone and pioglitazone may not have a class effect in terms of risk/benefit profile and the treatment plan should be carefully individualized for each patient.
Currently, pioglitazone is the only FDA approved TZD routinely available for prescription in the US. Given the risks associated with rosiglitazone, it can only be prescribed if both the prescribing physician and patient taking the medication are enrolled in the Avandia-Rosiglitazone Medicines Access Program [37]. Pioglitazone has significant therapeutic effects in reducing insulin resistance, although there should be caution when using this drug, it might be beneficial for a selective group of patients. Further research will be helpful in carefully determining the significance of the long-term benefits and risks profile.
Alpha-Glucosidase Inhibitors
Postprandial hyperglycemia is a known predictor of cardiovascular disease risk. The alpha glucosidase inhibitors (acarbose, voglibose, miglitol) are a class of oral diabetes drugs that target postprandial hyperglycemia. Their primary mechanism of action is competitive inhibition of alpha glucosidase in the proximal small bowel, which delays digestion and absorption of complex carbohydrates and blunts postprandial hyperglycemia. Although they are not usually first-line treatment in the US, in some countries alpha glucosidase inhibitors (AGI) are the most widely prescribed oral antiglycemic agents [38•]. Acarbose, the most studied of the class, effects a modest A1c reduction of 0.8 % [39].
AGI offer several potential advantages over other classes of diabetes drugs. Acarbose and voglibose are not systemically absorbed but rather partially metabolized by gut bacteria, while miglitol is absorbed and cleared renally. Therefore these drugs have virtually no drug-drug interactions and can be used safely with all other antiglycemic agents, including insulin, for a synergistic effect. Unlike sulfonylureas, AGI do not directly affect insulin secretion, hence they do not cause hypoglycemia, which may be an independent risk factor for cardiovascular mortality. Acarbose has been shown in several trials to cause more weight loss than placebo, sulfonylureas, and DPP4 inhibitors, both as monotherapy and in combination with metformin and sulfonylureas [40•]. Additionally, adaptation to delayed carbohydrate absorption by AGI may enhance endogenous GLP-1 secretion by stimulating L-cells in the lower small intestine [38•].
One of the major factors limiting the widespread use and study of AGI in the US is tolerance of the adverse effects. Flatulence, abdominal discomfort, and diarrhea are common with AGI, owing to their alteration of carbohydrate metabolism. These gastrointestinal effects generally attenuate with gradual titration of dosing. Interestingly, the flatulence caused by AGI may actually be a unique mechanism of cardiovascular protection. Administration of AGI causes gut bacteria to produce excess H2 by digestion of unabsorbed carbohydrates. Suzuki and Kajiyama have shown that this excess H2, through its reductive properties, reverses oxidative stress and atherogenesis, and that this effect is sustained between meals. H2 production by oral acarbose seems to be superior to oral administration of H2-dissolved water [41, 42].
The largest trial of AGI to date was the landmark 2002 Study to Prevent Non-insulin Dependent Diabetes Mellitus (STOP-NIDDM) involving acarbose. This multicenter, double-blind, randomized controlled trial (n = 1429) of patients with impaired glucose tolerance showed a 36 % relative risk reduction (RRR) of developing diabetes with treatment [43]. An analysis of secondary outcomes showed a 34 % RRR (5.3 % ARR) of hypertension. It also showed an impressive 49 % RRR (2.5 % ARR) of cardiovascular events with acarbose, including myocardial infarction, new angina, revascularization, cardiovascular death, congestive heart failure, cerebrovascular events, and peripheral vascular disease [44]. A subgroup analysis of the STOP-NIDDM (n = 132) showed that with acarbose vs. placebo there was a 50 % reduction per year of progression of intima media thickness, a strong predictor of coronary artery disease and stroke [45]. Similarly, a meta-analysis of seven trials of acarbose vs. placebo (MeRIA) pooling 2190 patients, more than half of which had pre-existing cardiovascular disease, showed a 35 % RRR of CV events, 64 % risk reduction of MI, and significant decrease in blood pressure with treatment [46]. Another double-blind randomized controlled trial (n = 44) showed a significant decrease in systolic and diastolic blood pressure with acarbose. This effect was shown to be significantly higher than that achieved with sulfonylureas, namely glibenclamide [47]. These effects cannot be solely attributed to improved overall glycemic control, as the CAPRI study showed that postprandial glucose peak is correlated to carotid intima media thickness out of proportion to the A1c [48].
One explanation for the unique benefits of AGI is their role in inflammation. Studies using continuous glucose monitors have shown that postprandial glucose, particularly peak glucose, is correlated with markers of oxidative stress [38]. In fact, in vitro studies of human endothelial cells have shown that fluctuations in glucose levels, rather than sustained hyperglycemia, are correlated with the most oxidative damage and endothelial dysfunction [49]. Treatment with acarbose or voglibose has been shown to reduce many inflammatory markers, including NfKB, intercellular adhesion molecule 1, fibrinogen, D-dimer, prothrombin, and CRP [50, 51]. Miglitol has been shown to increase adiponectin, an anti-inflammatory molecule, and reduce urinary albumin excretion rates significantly more than meglintide, a sulfonylurea [52]. In addition, AGI improve lipid profiles, which are closely linked to risk of atherogenesis. Acarbose can decrease postprandial and fasting triglycerides by 15 % [50].
Alpha-glucosidase inhibitors are safe anti-glycemic agents that can work synergistically with other classes to reduce postprandial hyperglycemia. Despite the relatively modest reduction in A1c with AGI, there is evidence of their protective cardiovascular effects that may be attributed to production of H2, reduction of inflammatory and increase of anti-inflammatory markers, reduction of blood pressure, and reduction of atherogenic lipids. Still, these data come from studies with low total cardiovascular event rates. The Acarbose Cardiovascular Evaluation (ACE), an ongoing trial of 7500 high risk patients in China with recent myocardial infarction may further elucidate whether acarbose vs. placebo can significantly prevent cardiovascular events [38•].
Incretin Based Therapies
One of the newer classes of diabetes medications includes the incretin based therapies, of which there are two subcategories: DPP-IV inhibitors and GLP-1 agonists. Glucagon like peptide-1 (GLP-1) is secreted by intestinal cells and is rapidly inactivated by dipeptidyl peptidase IV (DPP IV) in the human body [53]. Normally the physiological half-life of GLP-1 is only 1–2 minutes due to rapid degradation by DPP-IV, but with the administration of the DPP-IV inhibitors, the action of this peptide hormone can be prolonged. It is well documented that the GLP-1 response is impaired in patients with longstanding type 2 DM, which is why this class of medications address a specific functional defect in type 2 DM [54].
GLP-1 Agonists
Exenatide (twice daily), exenatide extended-release (once weekly) and liraglutide (once daily) are the three injectable GLP-1 agonists that are most widely available in the US. The effects of these agents are multi-factorial. GLP-1 stimulates insulin secretion, but only in a glucose-dependent fashion. GLP-1 also inhibits glucagon secretion, slows gastric emptying, and reduces appetite [55]. GLP-1 agonists are injectable and usually tend to be more effective than DPP-IV inhibitors since they provide pharmacological levels of exogenous GLP-1 compared to supraphysiologic levels of endogenous active GLP-1 seen with DPP-IV inhibitors [54]. GLP-1 agonists reduce A1c by approximately 1-2 % [56].
Looking strictly at the cardiovascular effects of these agents, there seems to be an association with improved cardiovascular profiles, independent of glucose control. It is difficult to ascertain whether these results are due to weight loss or simply effects of the therapy through a different mechanism. The DPP-IV inhibitors are mostly weight neutral, in contrast to GLP-1 agonists, which usually promote weight loss. This is a favorable characteristic of this class since usually oral hypoglycemic agents and insulin tend to result in weight gain [57••]. According to a retrospective review of over 44,000 patients treated with exenatide, sitagliptin, or insulin, it was found that exenatide-treated patients lost a mean +/− SD of 3 +/− 7.33 kg, sitagliptin-treated patients lost 1.1 +/− 5.39 kg, and insulin-treated patients gained 0.6 +/− 9.49 kg [58].
It is also well noted that incretin based therapies provide improvements in lipid profile and reduction in blood pressure. In one study of 217 patients who used exenatide for at least three years, there was an average decrease of triglycerides of 12 %, total cholesterol by 5 %, LDL by 6 %, and increase in HDL by 24 % [59]. In regards to blood pressure, the GLP-1 agonists seem to have a very minor effect in lowering systolic blood pressure: 2–4 mmHg with exenatide and 2–3 mmHg with liraglutide [60•].
One of the cardiovascular benefits that the incretin based therapies may provide is improvement of endothelial function, which in turn may help reduce atherosclerosis. Diabetic patients are thought to have increased cardiovascular disease in part due to endothelial dysfunction. Adipose tissue is known to release cytokines such as TNF-alpha, leptin, and plasminogen activator inhibitor 1 (PAI-1), which all contribute to this process [61]. It has been shown that treatment with GLP-1 agonists can reduce levels of PAI-1 and TNF-alpha, which might help prevent vascular endothelial dysfunction seen in diabetic patients [62].
In a retrospective analysis of over 400,000 patients treated with exenatide versus other therapies, it was found that patients treated with exenatide were less likely to have a cardiovascular disease event compared to the patients treated with other agents (hazard ratio 0.81) and lower rates of CVD related hospitalization (HR 0.88) [63].
GLP-1 agonists are one of the newest classes of medications available for the treatment of diabetes. They are an interesting class of anti-diabetes medication because, in addition to the beneficial effects on glucose control, the patients have shown moderate reduction in body weight. The most common side effects are gastrointestinal, dizziness, and hypoglycemia. Nausea is not infrequent, but usually mild; the more severe side effects are some risks of pancreatitis and renal failure. We will likely learn more about the long-term safety profile of these drugs in the near future.
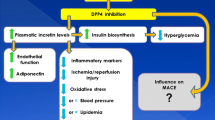
DPP IV Inhibitors
The DDP IV inhibitors available in the US include sitagliptin, saxagliptin, and linagliptin. DPP-IV inhibitors are administered orally and increase GLP-1 levels in the body by about two-fold. These agents reduce A1c by approximately 0.5-1 % [56]. As mentioned above, DPP-IV inhibitors are mostly weight neutral, however in the retrospective study comparing exenatide, sitagliptin, and insulin, sitagliptin was associated some degree of weight loss, however not as significant as exenatide [58]. The blood pressure and lipid profile benefits mentioned above for GLP-1 agonists apply to the DPP-IV inhibitors as well; these seem to be class effects of the incretin based therapies.
Given all the above findings, the question arises whether all these improvements in cardiovascular profile actually have benefits on mortality and actual cardiovascular events. In a randomized control trial of 4607 patients, Frederich et al. compared saxagliptin vs. others (placebo, metformin, or glyburide). CV events were experienced by 1.1 % in saxagliptin vs. 1.8 % in others, CV death occurred in 0.2 % in saxagliptin group vs. 0.8 % in others, and all-cause mortality occurred in 0.3 % in saxagliptin vs. 1.0 % in others [64]. Another trial that is currently underway is the trial evaluating cardiovascular outcomes with sitagliptin (TECOS), which is a multinational randomized double-blind placebo-controlled trial which will incorporate over 14,000 patients with diabetes and documented cardiovascular disease. Primary endpoint in this trial will be first occurrence of cardiovascular outcome. This trial should provide valuable outcome data in regards to one of the first used DPP-IV inhibitors in the US [65].
The long-term benefits and risks have not yet been established in DPP-IV inhibitors, and these drugs are not recommended to be used as first line agent. Overall DPP-IV inhibitors have a modest anti-glycemic effect; however, can be beneficial in patients who need additional agents to reach target A1c. This class of drug is usually well tolerated with modest risk of side effects, including slightly increased risk of upper respiratory tract and urinary tract infections. Like GLP-1 agonists, cases of pancreatitis have been reported. The cardiovascular benefits of DPP-IV inhibitors have been shown in the laboratory and in initial human studies; more definitive trials that are currently underway should help clarify these findings.
Conclusions
When choosing a therapeutic regimen for diabetic patients, it is important to evaluate patients’ clinical profiles and cardiovascular risk factors. Metformin is recommended as a first line agent for type 2 DM, and second line therapy can be either combination therapy with additional oral medications or combining metformin with insulin. It is also important to keep in mind that diabetes cannot be well-controlled without lifestyle modifications, including proper diet and exercise. Diabetes is a chronic disease that requires a multi-disciplinary approach to optimize blood glucose, blood pressure, and lipid control. In order to achieve a personalized regimen that aims for optimal outcomes, we must take into consideration each drug’s side effects, patients’ cardiovascular risk factors, and their individual health profile.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
National Diabetes Fact Sheet, 2011. Available at http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2011.pdf. Accessed 2011.
Hemmignsen B, Lund SS, Wetterslev J, Vaag A. Oral hypoglycemic agents, insulin resistance and cardiovascular disease in patients with type 2 diabetes. Eur J Endocrinol. 2009;161:1–9.
The Action to Control Cardiovascular Risk in Diabetes Study Group. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358:2545–59.
The ADVANCE Collaborative Group. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008;358:2560–72.
• Messaoudi SE, Rongen GA, de Boer RA, Riksen NP. The cardioprotective effects of metformin. Curr Opin Lipidol. 2011;22:445–53. This is a recent review of myocardial ischemia-reperfusion injury and metformin in animal models.
Palumbo PJ. Metformin: effects on cardiovascular risk factors in patients with non insulin-dependent diabetes mellitus. J Diabetes Complicat. 2008;12:110–9.
Selvin E, Bolen S, Yeh HC, et al. Cardiovascular outcomes in trials of oral diabetes medications: a systematic review. Arch Int Med. 2008;168:2070–80.
•• Kooy A, de Jager J, Lehert P, et al. Long-term effects of metformin on metabolism and microvascular and macrovascular disease in patients with type 2 diabetes mellitus. Arch Intern Med. 2009;169:616–25. This is one of the few randomized controlled trials, as a follow up to the UKPDS, that showed an improvement in macrovascular outcomes when metformin was added to an insulin regimen.
Schramm TK, Gislason GH, Vaag A, et al. Mortality and cardiovascular risk associated with different insulin secretagogues compared with metformin in type 2 diabetes, with or without a previous myocardial infarction: a nationwide study. Eur Heart J. 2011;32:1900–8.
Roussel R, Travert F, Pasquet B, et al. Metformin use and mortality among patients with diabetes and atherothrombosis. Arch Intern Med. 2010;170:1892–9.
McAlister FA, Eurich DT, Majumdar SR, Johnson JA, et al. The risk of heart failure in patients with type 2 diabetes treated with oral agent Monotherapy. Eur J Heart Fail. 2008;10:703–8.
Eurich DT, McAlister FA, Balckburn DF, et al. Benefits and harms of antidiabetic agents in patients with diabetes and heart failure: systematic review. Available at bmj.com. Accessed 2007.
Sadikot S, Mogensen CE. Risk of coronary artery disease associated with initial sulfonylurea treatment of patients with type 2 diabetes: a matched case–control study. Diabetes Res Clin Pr. 2008;82:391–5.
Brady PA, Terzic A. The sulfonylurea controversy: more questions from the heart. JACC. 1998;31:950–6.
Evans JMM, Ogston SA, Reimann F, et al. No differences in mortality between users on pancreatic-specific and non-pancreatic specific sulfonylureas: a cohort analysis. Diabetes Obes Metab. 2008;10:350–2.
Pantalone KM, Kattan MW, Yu C, et al. The risk of overall mortality in patients with type 2 diabetes receiving glipizide, glyburide, or glimeperide monotherapy. Diabetes Care. 2010;33:1224–9.
Andersson C, Gislason GH, Jorgensen JH, et al. Comparable long-term mortality risk associated with individual sulfonylureas in diabetes patients with heart failure. Diabetes Res Clin Pr. 2011;94:119–25.
Tomai F, Crea F, Gaspardone A, et al. Ischemic preconditioning during coronary angioplasty is prevented by glibenclamide, a selective ATP-sensitive K + channel blocker. Circulation. 1994;90:700–5.
Klepzig H, Kober G, Matter C, et al. Sulfonylureas and ischaemic preconditioning: a double-blind placebo controlled evaluation of glimeperide and glibenclamide. Eur Heart J. 1999;20:439–46.
Zeller M, Danchin M, Simon D, et al. Impact of type of preadmission sulfonylureas on mortality and cardiovascular outcomes in diabetic patients with acute myocardial infarction. J Clin Endocrinol Metab. 2010;95:4993–5002.
UK Prospective Diabetes Study Group (UKPDS). Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 2008;352:853–7.
Gangji AS, Cukierman T, Gerstein HC, Goldsmith CH, Clase CM. A systematic review and meta-analysis of hypoglycemia and cardiovascular events. Diabetes Care. 2007;30:389–94.
• Pantalone KM, et al. Increase in overall mortality risk in patients with type 2 diabetes receiving glipizide, glyburide or glimeperide monotherapy versus metformin: a retrospective analysis. Diabetes Obes Metab. 2012;14:803–9. A recent large retrospective review that showed an increased mortality with 3 different sulfonylureas compared to metformin.
Evans JMM, Ogston SA, Emslie-Smith A, Morris AD. Risk of mortality and adverse cardiovascular outcomes in type 2 diabetes: a comparison of patients treated with sulfonylureas and metformin. Diabetologia. 2006;49:930–6.
Vameq J, Latruffe N. Medical significance of peroxisome proliferator-activated receptors. Lancet. 1999;354:141–8.
Kahn SE, Haffner SM, Heise MA, et al. Glycemic durability of rosiglitazone, metformin, and glyburide monotherapy. N Engl J Med. 2006;355:2427–43.
Nathan DM, Buse JB, Davidson MB, et al. Medical management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy: a consensus statement from the American diabetes association and the European association for the study of diabetes. Diabetes Care. 2006;29:1963–72.
Nesto RW, Bell D. Thiazolidinedione use, fluid retention, and congestive heart failure: a consensus statement from the American heart association and American diabetes association. Circulation. 2003;108:2941–8.
Haffner SM. Epidemiology of hypertension and insulin resistance syndrome. J Hypertens Suppl. 1997;15:S25–30.
Qayyum R, Adomaityte J. A meta-analysis of the effect of thiazolidinediones on blood pressure. J Clin Hypertens. 2006;8:19–28.
Mayerson AB, Hundal RS, Dufour S, et al. The effects of rosiglitazone on insulin sensitivity, lipolysis, and hepatic and skeletal muscle triglyceride content in patients with type 2 diabetes. Diabetes. 2002;51:797–802.
Goldberg RB, Kendall DM, Deeg MA, et al. A comparison of lipid and glycemic effects of pioglitazone and rosiglitazone in patients with type 2 diabetes and dyslipidemia. Diabetes Care. 2005;28:1547–54.
Robinson JG. Should we use PPAR agonists to reduce cardiovascular risk? PPAR Res. Article ID. 2008;891425:1–13.
Dormandy JA, Charbonnel B, Eckland DJA, et al. Secondary prevention of macrovascular events in patients with type 2 diabetes in the PROactive study (PROspective pioglitAzone clinical trial in macroVascular events): a randomised controlled trial. Lancet. 2005;366:1279–89.
Nissen SE, Nicholls SJ, Wolski K, et al. Comparison of pioglitazone vs glimepiride on progression of coronary atherosclerosis in patients with type 2 diabetes: the PERISCOPE randomized controlled trial. JAMA. 2008;299:1561–73.
Nissen SE, Wolski K. Effect of rosiglitazone on the risk of myocardial infarction and death from cardiovascular causes. N Engl J Med. 2007;356:2457–71.
Medication Guide Avandia. Available at http://www.fda.gov/downloads/Drugs/DrugSafety/ucm085922.pdf. Accessed 2011.
• Standl E, Schnell O, Alpha-glucosidase inhibitors. Alpha-glucosidase inhibitors 2012 – cardiovascular considerations and trial evaluation. Diabetes Vasc Dis Res. 2012;0:1–7. A recent review of studies done on the cardiovascular effects of acarbose.
Van de Laar FA, Lucassen PL, Akkerma RP, et al. Alpha-glycosidase inhibitors for patients with type 2 diabetes: results from a Cochrane systematic review and meta-analysis. Diabetes Care. 2005;28:154–63.
• Lin SD, Wang JS, Hsu SR, et al. The beneficial effect of alpha-glucosidase inhibitor on glucose variability compared with sulfonyurea in Taiwanese type 2 diabetic patients inadequately controlled with metformin: preliminary data. J Diabetes Complicat. 2011;25:332–8. A randomized study that showed the addition of acarbose to metformin causes much lower glucose variability throughout the day compared to the addition of a sulfonylurea, glimeperide.
Suzuki Y, Sano M, Hayashida K, et al. Are the effects of a-glucosidase inhibitors on cardiovascular events related to elevated levels of hydrogen gas in the gastrointestinal tract? FEBS Lett. 2009;583:2157–215.
Kajiyama S, Hasegawa G, Asano M, et al. Supplementation of hydrogen-rich water improves lipid and glucose metabolism in patients with type 2 diabetes or impaired glucose tolerance. Nutr Res. 2008;28:137–43.
Chiasson J, Josse RG, Gomis R, et al. Acarbose for prevention of type 2 diabetes mellitus: the STOP-NIDDM randomised trial. Lancet. 2002;359:2072–7.
Chiasson J, Josse RG, Gomis R, et al. Acarbose treatment and the risk of cardiovascular disease and hypertension in patients with impaired glucose tolerance: the STOP-NIDDM trial. JAMA. 2003;290:486–94.
Hanefeld M, Chiasson JL, Koehler C, et al. Acarbose slows progression of intima-media thickness of the carotid arteries in subjects with impaired glucose tolerance. Stroke. 2004;35:1073–8.
Hanefeld M, Cagatay M, Petrowitsch T. Acarbose reduces the risk of myocardial infarction in type 2 diabetics: meta-analysis of seven long-term studies. Eur Heart J. 2004;25:10–6.
Rosenthal JH, Mauersberger H. Effects on blood pressure of the alpha-glucosidase inhibitor acarbose compared with the insulin enhancer glibenclamide in patients with hypertension and type 2 diabetes mellitus. Clin Drug Invest. 2002;22:695–701.
Esposito K, Ciotola M, Carleo D, et al. Post-meal glucose peaks at home associate with carotid intima-media thickness in type 2 diabetes. J Clin Endocrinol Metab. 2008;93:1345–50.
Schisano B, Tripathi G, McGee K, et al. Glucose oscillations, more than constant high glucose, induce p53 activation and a metabolic memory in human endothelial cells. Diabetologia. 2011;54:1219–26.
Hanefeld M, Fischer S, Schulze J, et al. Therapeutic potentials of acarbose as first-line drug in NIDDM insufficiently treated with diet alone. Diabetes Care. 1991;14:732–7.
Satoh N, Shimatsu A, Yamada K, et al. An a-glucosidase inhibitor, voglibose, reduces oxidative stress markers and soluble intercellular adhesion molecule 1 in obese type 2 diabetic patients. Metabolism. 2006;55:786–7.
Yokoyama H, Kannno S, Ishimura I, et al. Miglitol increases the adiponectin level and decreases urinary albumin excretion in patients with type 2 diabetes mellitus. Metabolism. 2007;56:1458–63.
Kim W, Egan J. The role of incretins in glucose homeostasis and diabetes treatment. Pharmacol Rev. 2008;60:470–512.
Chia CW, Egan JM. Incretin-based therapies in type 2 diabetes mellitus. J Clin Endocrinol Metab. 2008;93:3703–16.
Ahren B, Landin-Olsson M, Jansson P, et al. Inhibition of dipeptidyl peptidase-4 reduces glycemia, sustains insulin levels, and reduces glucagon levels in type 2 diabetes. J Clin Endocrinol Metab. 2004;89:2078–84.
Drucker DJ, Nauck MA. The incretin system: glucagon-like peptide-1 receptor agonists and dipeptidyl peptidase-4 inhibitors in type 2 diabetes. Lancet. 2006;368:1696–705.
•• Mingrone G, Panunzi S, De Gaetano A, et al. Bariatric surgery versus conventional medical therapy for type 2 diabetes. N Engl J Med. 2012;366:1577–85. Important article demonstrating how significantly different diabetes outcomes are in patients who undergo bariatric surgery versus medical treatment of diabetes. This could potentially change the stringent requirements patients have to meet in order to qualify for bariatric surgery.
Horton ES, Silberman C, Davis KL, Berria R. Weight loss, glycemic control, and changes in cardiovascular biomarkers in patients with type 2 diabetes receiving incretin therapies or insulin in a large cohort database. Diabetes Care. 2010;33:1759–63.
Klonoff DC, Buse JB, Nielsen LL, et al. Exenatide effects on diabetes, obesity, cardiovascular risk factors and hepatic biomarkers in patients with type 2 diabetes treated for at least 3 years. Curr Med Res Opin. 2008;24:275–86.
• Addison D, Aguilar D. Diabetes and cardiovascular disease: the potential benefit of incretin-based therapies. Curr Atheroscler Rep. 2011;13:115–22. Review article describing benefits of incretin therapies in treatment of cardiovascular disease.
Forst T, Weber MM, Pfutzner A. Cardiovascular benefits of GLP-1 based therapies in patients with diabetes mellitus type 2: effects on endothelial and vascular dysfunction beyond glycemic control. Exp Diabetes Res. 2012;2012:1–9.
Courreges JP, Vilsbollt T, Zdravkovic M, et al. Beneficial effects of once-daily liraglutide, a human glucagon like peptide-1 analogue, on cardiovascular risk biomarkers in patients with type 2 diabetes. Diabetic Med. 2008;25:1129–31.
Best JH, Hoogwerf BJ, Herman WH, et al. Risk of cardiovascular disease events in patients with type 2 diabetes prescribed the glucagon-like peptide 1 (GLP-1) receptor agonist Exenatide twice daily or other glucose-lowering therapies. A retrospective analysis of the LifeLink database. Diabetes Care. 2011;34:90–5.
Frederich R, Alexander JH, Fiedorek FT, et al. A systematic assessment of cardiovascular outcomes in the saxagliptin drug development program for type 2 diabetes. Postgrad Med. 2010;122:16–27.
Bethel MA, Green J, Califf RM, Holman RR. Rationale and design of the trial evaluating cardiovascular outcomes with sitagliptin (TECOS). Diabetes. 2009;58:A639.
Disclosure
No potential conflicts of interest relevant to this article were reported.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Diabetes and Cardiovascular Disease
Rights and permissions
About this article
Cite this article
Singh, S., Bhat, J. & Wang, P.H. Cardiovascular Effects of Anti-Diabetic Medications in Type 2 Diabetes Mellitus. Curr Cardiol Rep 15, 327 (2013). https://doi.org/10.1007/s11886-012-0327-1
Published:
DOI: https://doi.org/10.1007/s11886-012-0327-1