Abstract
Cardiovascular disease in women during pregnancy poses particular challenges. It continues to be a leading cause of maternal mortality and contributes to significant morbidity. Echocardiography is essential in characterizing the extent and effects of heart disease prior to, during, and after pregnancy. By understanding the physiologic adaptation in pregnancy with increases in heart rate, blood volume, and cardiac output, and decrease in vascular resistance, one can anticipate and recognize the effects of these changes on various cardiac lesions. Cardiomyopathy, severe, obstructive valvular disease, aortic dilation due to Marfan’s disease, and cyanotic congenital heart disease are poorly tolerated in pregnancy. These disorders can be readily distinguished from normal structural changes of pregnancy and their severity assessed by echocardiography. Cardiovascular disease in women of reproductive age requires careful, multidisciplinary management by obstetric and medical teams ideally beginning preconception and continuing through the postpartum period.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The cardiovascular hemodynamic changes of pregnancy are vast and yet completely reversible. The physiologic adaptation to pregnancy speaks to the plasticity of the cardiovascular system. The normal heart and vasculature are able to accommodate the increased demands of pregnancy, but the diseased heart may worsen and decompensate. By understanding the normal physiologic changes of pregnancy, one can predict the response of specific cardiovascular lesions. There are more women with congenital and acquired heart disease choosing to become pregnant. This is due to a number of factors including advances in medicine and surgery, which allow patients with increasingly complex cardiac and medical conditions to survive longer and into their childbearing years. Furthermore, women are delaying childbirth so that they may have developed advanced valvular, myocardial, and coronary disease prior to pregnancy.
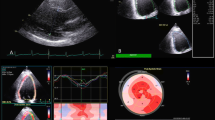
Ideally, patients with known cardiac pathology should be thoroughly assessed prior to planned pregnancy. The echocardiogram plays a central role in precisely defining the extent and severity of the cardiac lesion as well as the effects on ventricular and valvular functioning. This allows for informed preconception counseling about maternal and fetal morbidity and mortality risks. Furthermore, serial echocardiograms can be performed safely throughout gestation to reassess the lesion and the cardiovascular adaptation [1].
Cardiovascular Hemodynamics of Normal Pregnancy
The echocardiographic evaluation of cardiac structure and function in pregnant women requires an understanding of the normal physiologic changes of pregnancy, in particular the increase in blood volume (preload), decreased systemic vascular resistance (afterload), and increase in cardiac output (CO) (Table 1). Total blood volume increases by 30% to 40% (1,200–1,600 mL) during pregnancy due to increased erythrocyte mass and an even greater expansion in plasma volume, resulting in a physiologic anemia of pregnancy. This increase in blood volume begins early in the sixth week of gestation and plateaus by the third trimester [2].
Total peripheral resistance decreases during pregnancy, resulting in a 10- to 15-mm Hg decrease in mean arterial pressure that is maximal at the end of the second trimester. The increase in the compliance in the venous and arterial systems acts as a capacitor to accommodate the increased blood volume [3, 4].
Also, CO increases by 30% to 60% during the first and second trimesters of pregnancy, first as a result of increased preload and stroke volume and later as a result of increased heart rate [5–7]. There is discrepancy among studies as to whether CO increases further in the third trimester, plateaus, or decreases. Because most studies are small, differences may be explained by individual variation.
Echocardiographic Changes in Cardiac Structure and Function
Echocardiography is a powerful tool in pregnancy because it is a safe way to assess cardiac structure and function in gravid women, posing no risk of radiation to the mother or the fetus. However, it is important to understand normal structural and functional changes that occur during pregnancy when interpreting these studies. In all studies evaluating echocardiographic findings in normal pregnancy, the echocardiograms were done in the left lateral decubitus position. In supine patients, the gravid uterus compresses the inferior vena cava and decreases venous return, potentially confounding measurements and causing patient discomfort. A second caveat to remember when interpreting studies of echocardiographic measurements during pregnancy is that “preconception values” are almost always obtained postpartum for logistical reasons. Studies vary in the timing of this echocardiogram, from as early as 2 to 4 weeks postpartum to 6 months postpartum. True preconception echocardiograms are optimal, but in the absence of this, the 6-month time point appears to be the best surrogate; although the hemodynamic changes may have returned to preconception values by 6 to 12 weeks, structural changes can take months [8]. Differences in the timing of the postpartum echocardiogram probably account for some of the discrepancy in data (Table 1).
First, as mentioned above, the increase in blood volume and CO during pregnancy results in a physiologic state of volume overload. This leads to dilation of the heart and reversible eccentric hypertrophy, similar to that observed in well-trained athletes [9]. Most studies have found that left ventricular end-diastolic dimensions increase slightly during pregnancy although remain within normal limits. In all but one study, the mean end-diastolic diameter was less than 5 cm, with the average being approximately 4.9 cm. Left ventricular mass, even when corrected for changes in body surface area, increased during pregnancy by approximately 5% to 10% and decreased to baseline levels by 6 months postpartum. Moreover, the ventricular hypertrophy observed appears proportional to the increased workload imposed by pregnancy, and the ratio of wall thickness to ventricular radius does not change, consistent with eccentric rather than concentric hypertrophy [3, 4, 7, 10, 11]. In the one study that did not note an increase in left ventricular mass, the “control” postpartum echocardiogram was done early at 6 weeks postpartum, whereas other studies were done later [4].
Left ventricular systolic function, as assessed by the load-dependent measures of ejection fraction (EF), fractional shortening, and velocity of circumferential fiber shortening (VCFC), may increase slightly according to some studies, but does not appear to change significantly during pregnancy. The effect of pregnancy on myocardial contractility is somewhat controversial and must be determined using load-independent parameters such as the relationship between end-systolic wall stress and VCFC. When studies have looked at this relationship, some have shown an increase, others no change, and still others a decrease in intrinsic contractility in pregnancy [3, 4, 10, 11]. It is likely that any change in contractility is small.
Left ventricular diastolic function has been explored in several papers and appears to be preserved during normal pregnancy, despite increased preload and physiologic left ventricular hypertrophy. Similar to evaluation of intrinsic myocardial contractility, assessment of left ventricular diastolic function requires attention to load-dependent versus load-independent parameters. As preload increases with increased blood volume in the first and second trimesters, peak mitral inflow velocity increases in early diastole (E wave) and during atrial systole (A wave). The change in the A wave exceeds that of the E wave, resulting in a decreased E:A ratio during normal pregnancy. It has been hypothesized that mean left atrial filling pressures increase to within the upper limits of normal during pregnancy, forcing atrial contraction to contribute more to left ventricular filling [12, 13]. Tissue Doppler imaging, a relatively load-independent technique to assess diastolic function, confirms that left ventricular relaxation is preserved in normal pregnancy. The ratio of myocardial velocity (E′) to mitral inflow velocity (E) during early diastole, a validated marker of left atrial pressure, is unchanged or decreases during pregnancy. Similar to the decrease in E:A observed with pulsed-wave Doppler, there was a decrease in the ratio of myocardial velocity during early diastole (E′) to atrial systole (A′), which may be secondary to enhanced atrial contractility [12, 14•].
As one would predict with the increase in volumes and chamber dimensions, there is a slight increase in annular diameters during pregnancy, resulting in a greater number of patients who exhibit physiologic mitral (28%), tricuspid (94%), and pulmonic (94%) regurgitation. However, despite a small (∼5%) increase in left ventricular outflow tract diameter, aortic insufficiency should not develop during pregnancy [3, 5, 15]. Similarly, atrial size increases during pregnancy by approximately 10%, although measurements remain within normal limits [7].
Asymptomatic pericardial effusions are common in pregnancy, occurring in approximately 40% of women [16, 17]. One study of 57 healthy pregnant women noted that effusions became more common as patients progressed from the first to the third trimester, and found a greater frequency of effusion among primigravidas (69%) compared with multigravidas (36%). Pericardial effusions were more common in women who gained more than 12 kg, leading the authors to hypothesize that increased fluid retention may contribute to the development of effusions. All effusions resolved on repeat echocardiograms done at 6 weeks postpartum, and no patient had tamponade [16].
Pathology Seen on Echocardiogram in Pregnant Women
Peripartum Cardiomyopathy
Echocardiography is critical in the diagnosis of peripartum cardiomyopathy (PPCM) and may be helpful in predicting recovery of ventricular function. Clinically, PPCM is defined by the following criteria: development of congestive heart failure in the last month of pregnancy or within 5 months after delivery, absence of pre-existing cardiac disease, and absence of another identifiable cause of heart failure. Echocardiographic criteria have been developed based on the criteria used to diagnose idiopathic dilated cardiomyopathy and include left ventricular EF less than 45%, fractional shortening less than 30% on M-mode, and left ventricular end-diastolic dimension greater than 2.7 cm/m2 (or 4.3–4.8 cm in a 70- to 80-kg woman). Echocardiography is essential in ruling out other causes of congestive symptoms, including volume overload with normal systolic function, hypertensive heart disease, and valvular disease [18, 19].
The reported rate of recovery of ventricular function has varied widely (range, from 7% to 50%) based on older studies involving small numbers of patients. Mortality estimates are even more divergent, although had generally been quoted as 25% to 50%. Most of these case series preceded modern heart failure treatment with β blockers, angiotensin-converting enzyme inhibitors, ventricular assist devices, and cardiac transplantation. One study based on physician survey data reported normalization of function in 54% but a mortality of 9% [20]. A more recent retrospective case series of 55 patients found that EF improved in 62% of patients, remained unchanged in 25%, and declined in 4%. No deaths were reported in approximately 4 years of follow-up [21]. This is more in line with the experience at our institution over the past two decades.
The use of routine echocardiography in patients with PPCM has led to several studies evaluating parameters that might be able to predict recovery of systolic function. Studies have differed in their conclusions about which measurements are most predictive. There is some consensus that greater left ventricular end-diastolic dimension at the time of diagnosis portends a decreased chance of recovery, with cutoff values variably quoted as 5.6 to 6 cm [21, 22]. Some studies have found lower initial EF is associated with a worse chance of recovery [23••, 24], whereas Amos et al. [21] found that only EF at 2 months predicted long-term outcome.
There is also some evidence that dobutamine stress echocardiography may be useful in identifying the presence of contractile reserve and helping to predict long-term recovery. This may be particularly helpful in women with a history of PPCM who wish to become pregnant again, as these women carry a significant risk of recurrent heart failure (∼20% in those with a normalized EF and ∼44% in those with persistent left ventricular systolic dysfunction) [25]. One study of six women with PPCM and severely reduced systolic function (mean LVEF, 25%) found significant contractile reserve, with an improvement in LVEF to 54%. The peak EF during stress testing correlated well with resting LVEF at a mean of 5.6 months follow-up (r = 0.79), whereas resting LVEF at baseline did not correlate significantly (r = 0.66) [26]. An earlier study compared contractile reserve in seven patients with a history of PPCM and normalized LVEF to age-matched control subjects and found that contractile reserve was reduced in the group with recovered PPCM [27]. Of note, however, this study used only low-dose dobutamine (5 μg/kg/min), which may have been too low to elicit contractile reserve. Further prospective studies are needed to validate this modality for use in counseling women who wish to conceive after recovering from PPCM.
Mitral Stenosis
Rheumatic mitral stenosis is the most common cardiac disease found in women during pregnancy, mostly secondary to the high prevalence in developing countries. It may be asymptomatic prior to conception, but can become symptomatic when the increase in blood volume and heart rate that begin in early pregnancy stress a previously compensated system (Table 2). Mild mitral stenosis (valve area >1.5 cm2) is well tolerated, but moderate and severe stenosis are associated with increased rates of pulmonary edema, supraventricular arrhythmias, and hospitalization. Ideally, women should be diagnosed and evaluated by a multidisciplinary team prior to conception, but frequently patients and physicians are not aware of their disease until symptoms lead to an echocardiogram during pregnancy [28].
Mitral valve area may be underestimated by traditional echocardiographic parameters during pregnancy because gradients across the valve increase by the square root of CO. Therefore, mitral valve area should be estimated by independent echocardiographic measurements and calculations. Rokey et al. [29] showed that the continuity equation (mitral valve area = stroke volume/transmitral velocity time integral) yielded comparable values during pregnancy and postpartum. In contrast, the pressure half-time method (mitral valve area = 220/pressure half-time) appeared to overestimate valve areas during pregnancy. They suggest that this occurs because of normal hemodynamic changes during pregnancy that can have a significant effect on the equalization of pressures between the left atrium and left ventricle. As already stated, left atrial filling pressures may increase to within the upper limits of normal, causing greater transmitral gradients and decreased pressure half-time [29]. Percutaneous balloon mitral valvuloplasty has been established in several case series as a viable option for treatment of pregnant women with class III to IV heart failure who are refractory to medical management [30]. Echocardiography is essential in evaluating the degree of calcification, leaflet thickening, mobility, and subvalvular disease (components of the Block-Weyman score), with scores less than 8 predicting a more successful outcome [31]. Moreover, contraindications including greater than 2+ mitral regurgitation, subvalvular stenosis, and left atrial thrombi are also diagnosed by transthoracic echocardiogram, although transesophageal echocardiography (TEE) is more specific for the latter finding. TEE has been successfully performed in pregnant women for many different reasons without complications, and when clinically indicated, is an invaluable diagnostic tool [32].
Other Valvular Diseases
Similar to significant mitral stenosis, severe aortic stenosis is poorly tolerated in pregnancy for many of the same reasons cited above. Mild to moderate aortic stenosis with normal aortic and ventricular function is associated with much less morbidity. Serial echocardiograms in pregnant women have shown that maximum pressure gradients increase by 20 to 35 mm Hg in the third trimester as one would expect from the increase in blood volume and flow (CO) [33]. Therefore, echocardiographic measurements of planimetry and ratios of velocity time integrals in the left ventricular outflow tract and aortic valve may be better markers of severity and correlate better with aortic valve area in pregnant women than mean and peak gradients alone [29].
In contrast to the left-sided obstructive lesions, chronic valvular insufficiency is well tolerated in pregnancy, even when severe if patients have preserved ventricular function. The decreased systemic vascular resistance and systolic blood pressure seen in normal pregnancy are hemodynamically favorable for regurgitant lesions. The patient’s clinical status and ventricular function prior to pregnancy are most predictive of success. Although cardiac surgery has been performed later in pregnancy, it is rarely indicated except for class III and IV heart failure that is refractory to medical management [28, 34]. Echocardiography should be used to assess the ventricular function and the etiology of the regurgitation, particularly for those who develop acute regurgitation and decompensation.
Mechanical heart valves pose a significant risk to both mother and fetus during pregnancy, and echocardiography may be useful in diagnosing one of the most common complications, valve thrombosis. The rate of valve thrombosis depends on the anticoagulation regimen used during pregnancy, and appears lowest with continued use of oral anticoagulation with warfarin throughout pregnancy (∼4%) and higher (∼9%) with the substitution of heparin during weeks 6 to 12 for purposes of decreasing the risk of warfarin embryopathy [35]. There are no official recommendations for serial echocardiography during pregnancy in women with mechanical prosthetic valves, but the possibility of valve thrombosis should be considered when clinical signs and symptoms are suggestive.
Marfan’s Syndrome
The 2006 American College of Cardiology/American Heart Association guidelines for management of patients with valvular disease recommend against pregnancy in women with Marfan’s syndrome, although the National Marfan Foundation does not support this recommendation [34]. The greatest risk in all patients with Marfan’s syndrome, and particularly in pregnant women, is aortic dissection (Table 2). The risk increases with increasing aortic size above 4.0 cm, although dissections have rarely been reported in gravidas with a normal-sized aortic root. Ideally, echocardiography to assess aortic root dimension and help estimate risk of dissection should be performed in women planning a pregnancy. Elective repair has been recommended for aortic root dimension greater than 4.5 cm prior to conception [34]. Most authors have suggested monthly echocardiography during pregnancy beginning at the sixth week of gestation when plasma volume and increased heart rate begin to stress the cardiovascular system [36]. Transthoracic echocardiography is usually adequate, with TEE reserved for an inability to accurately measure aortic root diameter. MRI is also an alternative imaging modality when transthoracic windows are limited. Progressive dilatation may prompt consideration of urgent repair or consideration of termination of pregnancy.
Pulmonary Hypertension
Both primary and secondary pulmonary artery hypertension are associated with high rates of maternal mortality, approximately 30% and 50%, respectively [37, 38]. Most maternal deaths occur in the first month postpartum. Therefore, early recognition and diagnosis of pulmonary hypertension in pregnant women is essential to allow women the opportunity to receive counseling on the risks of pregnancy and make an informed decision whether to undergo therapeutic abortion. Pulmonary artery pressures in pregnancy are not normally increased despite the increase in blood volume because pulmonary vascular resistance also decreases. Pulmonary artery pressures, estimated as four times the velocity of the tricuspid regurgitant jet squared plus right atrial pressure (4V2 + RAP), are obtainable by transthoracic echocardiography in most pregnant women since tricuspid regurgitation is present in 94% of patients and should be within normal limits (mean pulmonary artery pressure <25 mm Hg at rest).
Congenital Heart Disease
With advances in diagnostic technique and surgical correction, many women with congenital heart disease (CHD) are living well into their reproductive years. Most women are aware of their condition, but similar to mitral stenosis secondary to rheumatic heart disease, the hemodynamic burden of pregnancy may unmask a previously well-compensated and undiagnosed lesion. Echocardiography is an invaluable tool in documenting the presence of CHD and assisting physicians in counseling women about the risks of pregnancy to themselves and their offspring.
In a recent literature review, Drenthen et al. [39••] described cardiac, obstetric, and neonatal outcomes in 2,491 pregnancies in women with structural CHD. They found that cardiac complications, defined as arrhythmias requiring treatment, heart failure, myocardial infarction, stroke, endocarditis, or cardiovascular mortality (not reported separately), were more common in women with CHD than in the general population. The greatest risk was in women with Eisenmenger’s syndrome, other cyanotic heart disease, and pulmonary atresia with ventricular septal defects. In contrast, obstetric complications were not more prevalent in the cohort of patients with CHD compared with the general population. Also, the neonatal mortality rate in women with CHD was 4% or approximately four times the rate in offspring of women with structurally normal hearts. The greatest risk of neonatal and maternal mortality occurred in women with Eisenmenger’s syndrome. Consequently, these patients are generally discouraged from becoming pregnant or encouraged to consider an elective termination should they become pregnant [39••]. Once CHD is identified by echocardiogram, patients should be referred to a multidisciplinary team of cardiologists, high-risk obstetricians, geneticists, and anesthesiologists for further counseling and care.
Using a cohort of 562 patients with CHD, Siu et al. [40] identified a risk index that assigned women 1 point for each of the following risk factors: 1) prior history of heart failure, transient ischemic attack, stroke, or arrhythmia; 2) New York Heart Association (NYHA) class greater than II or cyanosis; 3) left heart obstruction defined by echocardiography as mitral valve area less than 2 cm2, aortic valve area less than 1.5 cm2, and left ventricular outflow tract gradient greater than 30 mm Hg; and 4) EF less than 40%. They found that patients with 0, 1, or greater than 1 point had a 5%, 27%, and 75% chance, respectively, of a cardiac event. Similarly, a separate risk index was identified for adverse neonatal outcomes with 1 point assigned for 1) NYHA greater than II or cyanosis; 2) smoking during pregnancy; 3) multiple gestations; and 4) anticoagulation. When no risk factors were present, the risk of neonatal mortality was 2% compared with 4% in the presence of at least one risk factor [40]. These risk indices may serve as helpful tools for physicians counseling women with a history of CHD.
Conclusions
Pregnancy is characterized by significant hemodynamic and physiologic cardiovascular changes. Echocardiography can define and follow these changes through gestation. The normal echocardiogram in pregnancy may show modest increases in chamber dimensions, mass, and valvular insufficiency without increases in systemic or pulmonary pressures. A small pericardial effusion is common and a 50% increase in CO should be expected. The normal heart is able to adapt to the increase in volume and work, whereas the diseased heart may decompensate. Patients with acquired heart disease and CHD should be thoroughly assessed preconception, and then followed clinically by a team of specialists throughout gestation and by serial echocardiograms when indicated.
References
Papers of particular interest, published recently, have been highlighted as follows: • Of importance •• Of major importance
Task Force on the Management of Cardiovascular Diseases During Pregnancy of the European Society of Cardiology: Expert consensus document on management of cardiovascular diseases during pregnancy. Eur Heart J 2003, 24:761–781.
Lund CJ, Donovan JC: Blood volume during pregnancy. Significance of plasma and red cell volumes. Am J Obstet Gynecol 1967, 98:394–403.
Poppas A, Shroff SG, Korcarz CE, et al.: Serial assessment of the cardiovascular system in normal pregnancy. Role of arterial compliance and pulsatile arterial load. Circulation 1997, 95:2407–2415.
Gilson GJ, Samaan S, Crawford MH, et al.: Changes in hemodynamics, ventricular remodeling, and ventricular contractility during normal pregnancy: a longitudinal study. Obstet Gynecol 1997, 89:957–962.
Robson SC, Hunter S, Boys RJ, Dunlop W: Serial study of factors influencing changes in cardiac output during human pregnancy. Am J Physiol 1989, 256:H1060–H1065.
Duvekot JJ, Cheriex EC, Pieters FA, et al.: Early pregnancy changes in hemodynamics and volume homeostasis are consecutive adjustments triggered by a primary fall in systemic vascular tone. Am J Obstet Gynecol 1993, 169:1382–1392.
Katz R, Karliner JS, Resnik R: Effects of a natural volume overload state (pregnancy) on left ventricular performance in normal human subjects. Circulation 1978, 58:434–441.
Capeless EL, Clapp JF: When do cardiovascular parameters return to their preconception values? Am J Obstet Gynecol 1991, 165:883–886.
Eghbali M, Deva R, Alioua A et al.: Molecular and functional signature of heart hypertrophy during pregnancy. Circ Res 2005, 96:1208–1216.
Simmons LA, Gillin AG, Jeremy RW: Structural and functional changes in left ventricle during normotensive and preeclamptic pregnancy. Am J Physiol Heart Circ Physiol 2002, 283:H1627–H1633.
Mone SM, Sanders SP, Colan SD: Control mechanisms for physiological hypertrophy of pregnancy. Circulation 1996, 94:667–672.
Fok WY, Chan LY, Wong JT, et al.: Left ventricular diastolic function during normal pregnancy: assessment by spectral tissue Doppler imaging. Ultrasound Obstet Gynecol 2006, 28:789–793.
Mesa A, Jessurun C, Hernandez A, et al.: Left ventricular diastolic function in normal human pregnancy. Circulation 1999, 99:511–517.
• Bamfo JE, Kametas NA, Nicolaides KH, Chambers JB: Reference ranges for tissue Doppler measures of maternal systolic and diastolic left ventricular function. Ultrasound Obstet Gynecol 2007, 29:414–420. This well-done study provides normative values to use when assessing ventricular systolic and diastolic function in pregnancy.
Campos O, Andrade JL, Bocanegra J, et al.: Physiologic multivalvular regurgitation during pregnancy: a longitudinal Doppler echocardiographic study. Int J Cardiol 1993, 40:265–272.
Abduljabbar HS, Marzouki KM, Zawawi TH, Khan AS: Pericardial effusion in normal pregnant women. Acta Obstet Gynecol Scand 1991, 70:291–294.
Ristic AD, Seferovic PM, Ljubic A, et al.: Pericardial disease in pregnancy. Herz 2003, 28:209–215.
Hibbard JU, Lindheimer M, Lang RM: A modified definition for peripartum cardiomyopathy and prognosis based on echocardiography. Obstet Gynecol 1999, 94:311–316.
Pearson GD, Veille JC, Rahimtoola S, et al.: Peripartum cardiomyopathy: National Heart, Lung, and Blood Institute and Office of Rare Diseases (National Institutes of Health) workshop recommendations and review. JAMA 2000, 283:1183–1188.
Elkayam U, Akhter MW, Singh H, et al.: Pregnancy-associated cardiomyopathy: clinical characteristics and a comparison between early and late presentation. Circulation 2005, 111:2050–2055.
Amos AM, Jaber WA, Russell SD: Improved outcomes in peripartum cardiomyopathy with contemporary. Am Heart J 2006, 152:509–513.
Chapa JB, Heiberger HB, Weinert L, et al.: Prognostic value of echocardiography in peripartum cardiomyopathy. Obstet Gynecol 2005, 105:1303–1308.
•• Habli M, O’Brien T, Nowack E, et al.: Peripartum cardiomyopathy: prognostic factors for long-term maternal outcome. Am J Obstet Gynecol 2008, 199:415.e1–415.e5. This recent, large case series of patients with PPCM provides updated morbidity and mortality data that can be used to assess patients and prognosticate.
Duran N, Gunes H, Duran I, et al.: Predictors of prognosis in patients with peripartum cardiomyopathy. Int J Gynaecol Obstet 2008, 101:137–140.
Elkayam U, Tummala PP, Rao K, et al.: Maternal and fetal outcomes of subsequent pregnancies in women with peripartum cardiomyopathy. N Engl J Med 2001, 344:1567–1571.
Dorbala S, Brozena S, Zeb S, et al.: Risk stratification of women with peripartum cardiomyopathy at initial presentation: a dobutamine stress echocardiography study. J Am Soc Echocardiogr 2005, 18:45–48.
Lampert MB, Weinert L, Hibbard J, et al.: Contractile reserve in patients with peripartum cardiomyopathy and recovered left ventricular function. Am J Obstet Gynecol 1997, 176:189–195.
Tsiaras S, Poppas A: Mitral valve disease in pregnancy: outcomes and management. Obstet Med 2009, 2:6–10.
Rokey R, Hsu HW, Moise KJJ, et al.: Inaccurate noninvasive mitral valve area calculation during pregnancy. Obstet Gynecol 1994, 84:950–955.
Esteves CA, Munoz JS, Braga S, et al.: Immediate and long-term follow-up of percutaneous balloon mitral valvuloplasty in pregnant patients with rheumatic mitral stenosis. Am J Cardiol 2006, 98:812–816.
Abascal VM, Wilkins GT, O’Shea JP, et al.: Prediction of successful outcome in 130 patients undergoing percutaneous balloon mitral valvotomy. Circulation 1990, 82:448–456.
Stoddard MF, Longaker RA, Vuocolo LM, Dawkins PR: Transesophageal echocardiography in the pregnant patient. Am Heart J 1992, 124:785–787.
Lesniak-Sobelga A, Tracz W, KostKiewicz M, et al.: Clinical and echocardiographic assessment of pregnant women with valvular heart diseases—maternal and fetal outcome. Int J Cardiol 2004, 94:15–23.
Bonow RO, Carabello BA, Chatterjee K, et al.: ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing Committee to Revise the 1998 guidelines for the management of patients with valvular heart disease) developed in collaboration with the Society of Cardiovascular Anesthesiologists endorsed by the Society for Cardiovascular Angiography and Interventions and the Society of Thoracic Surgeons. J Am Coll Cardiol 2006, 48:e1–e148.
Chan WS, Anand S, Ginsberg JS: Anticoagulation of pregnant women with mechanical heart valves: a systematic review of the literature. Arch Intern Med 2000, 160:191–196.
Goland S, Barakat M, Khatri N, Elkayam U: Pregnancy in Marfan syndrome: maternal and fetal risk and recommendations for patient assessment and management. Cardiol Rev 2009, 17:253–262.
Weiss BM, Zemp L, Seifert B, Hess OM: Outcome of pulmonary vascular disease in pregnancy: a systematic overview from 1978 through 1996. J Am Coll Cardiol 1998, 31:1650–1657.
Weiss BM, Hess OM: Pulmonary vascular disease and pregnancy: current controversies, management strategies, and perspectives. Eur Heart J 2000, 21:104–115.
•• Drenthen W, Pieper PG, Roos-Hesselink JW, et al.: Outcome of pregnancy in women with congenital heart disease: a literature review. J Am Coll Cardiol 2007, 49:2303–2311. This well-researched and well-written state-of-the-art paper presents the compilation of published reports in clear and accessible tables to help assess individual maternal and fetal risk in pregnancy complicated by heart disease.
Siu SC, Sermer M, Colman JM, et al.: Prospective multicenter study of pregnancy outcomes in women with heart disease. Circulation 2001, 104:515–521.
Elkayam U, Bitar F: Valvular heart disease and pregnancy part I: native valves. J Am Coll Cardiol 2005, 46:223–230.
Disclosure
No potential conflicts of interest relevant to this article were reported.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tsiaras, S., Poppas, A. Cardiac Disease in Pregnancy: Value of Echocardiography. Curr Cardiol Rep 12, 250–256 (2010). https://doi.org/10.1007/s11886-010-0106-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11886-010-0106-9