Abstract
Purpose of Review
Chronic rhinosinusitis (CRS) is a heterogenous disease process affecting a significant proportion of the population and impacting quality of life and productivity. Historically, CRS has been classified broadly into CRS with nasal polyps (CRSwNP) and CRS without nasal polyps (CRSsNP). Increased understanding regarding unique presentations of CRS subsets and their underlying inflammatory profiles has led to a new system for classifying CRS phenotypes.
Recent Findings
Consideration of CRS phenotypes has traditionally been a key factor in determining treatment paradigms. Under a new phenotype classification system, physical findings will continue to drive treatment decisions, but with more precision.
Summary
Recent rapidly accumulated knowledge indicates that the broad categorization of CRSwNP or CRSsNP is no longer clinically useful. Reorganization of CRS phenotypes and their underlying endotypes will lead to more targeted and efficacious therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic rhinosinusitis (CRS) is a heterogeneous disease characterized by facial pain and pressure, nasal obstruction, and rhinorrhea concurrent with signs of inflammation on endoscopy or imaging [1••]. Efforts to elucidate the pathophysiology of this underlying inflammatory pathway in CRS continue to be an area of active research. Historically, CRS has been phenotypically classified into CRS with nasal polyps (CRSwNP) and CRS without nasal polyps (CRSsNP), based upon the appearance of the sinus cavities on endoscopy [2]. Prior work has suggested that CRSwNP is related to underlying T helper 2 (Th2)-driven inflammation, while CRSsNP is precipitated by T helper 1 (Th1)-driven inflammation [3]. This general categorization has been disputed recently with Wang et al. [4] reporting geographic differences in the cytokine profiles of CRSwNP patients, with Asian countries having a higher incidence of non-Th2-mediated polyposis. Similarly, Stevens et al. [5] investigated the prevalence of different endotypes between CRSwNP and CRSsNP. While the main endotype of CRSwNP in this study was Th2-mediated inflammation, approximately one-third of patients with CRSsNP also demonstrated a predominance of Th2 inflammation. These results indicate that the inflammatory profiles in CRS are not as simple as the endoscopic determination of polyps vs. no polyps.
As knowledge regarding CRS continues to expand, these broad categorizations may no longer be precise, and as such, attempts at defining more clinically relevant phenotypes in CRS have commenced [1••, 6]. In the European Position Paper on Rhinosinusitis and Nasal Polyps 2020 (EPOS 2020), a new categorization of phenotypes has been proposed [7••]. The basis of the proposed phenotype classification is heralded on dividing CRS into primary and secondary, with further subdivisions being dependent on diffuse or localized disease, and Th2- or non-Th2-mediated inflammation. Secondary CRS is defined as being the consequence of another systemic disease or local pathology.
This review will focus on defining the features of primary CRS phenotypes, review recent research on inflammatory endotypes, and discuss the goals of treatment.
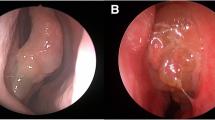
Primary Chronic Rhinosinusitis Phenotypes (Fig. 1)
Allergic Fungal Rhinosinusitis
Characteristics of Disease
Allergic fungal rhinosinusitis (AFRS) is a unique subset of CRS that is found almost exclusively in areas of high humidity and mold counts. AFRS typically presents in the 3rd–4th decade of life and is more common in African American males [8, 9]. It has a unilateral predominance in up to 50% of cases, and interestingly, in contrast to other Th2-driven phenotypes of CRS, comorbid asthma is found in less than 25% of patients with AFRS [10].
The diagnosis of AFRS is based clinically on the criteria outlined by Bent and Kuhn in 1994 [11]: type I hypersensitivity, nasal polyposis, characteristic computed tomography (CT) scan findings, eosinophilic mucin, and the presence of fungal hyphae in sinus contents. On magnetic resonance imaging (MRI), T1W1 and T2W1 these have characteristic hypodensity. Sinus opacification with central hyperdense secretions and bony remodeling/expansion are characteristic findings in AFRS [12].
Inflammatory Profile
The etiology behind the inflammation in AFRS has been extensively investigated and is likely related to factors in both the adaptive and innate immune systems. Tyler et al. [13] identified unique gene expression profiles in AFRS that were not present in idiopathic CRS. These unique gene expression profiles were linked with Th2 inflammation, co-stimulatory signaling, and T cell receptor signaling. Additionally, increased levels of antigen-specific IgE have been found in the sinonasal submucosa in AFRS patients when compared with other subtypes of CRS [14]. Additionally, the innate immune system has been implicated in the propagation of AFRS. Interleukin-33 receptors, a key promoter of Th2-related inflammation, are known to be upregulated in AFRS patients [15]. The innate immune system proteins, lactoferrin, surfactant protein-D, and histatins demonstrated lower expression levels in AFRS when compared with other CRS subtypes [9].
Management
Management of AFRS typically begins with upfront surgery to clear the sinuses of eosinophilic mucin and fungal debris in order to prevent early recurrence. In addition to surgery, post-operative medical management is paramount in controlling the disease. Suppression of the inflammatory response with topical and systemic corticosteroids is the mainstay of medical therapy. A recent review by Gan et al. [16] described the utility of systemic steroids in reducing post-operative mucosal disease, improving endoscopic appearance, and decreasing inflammatory markers. The efficacy of topical nasal steroids in CRSwNP has been established [17]. However, trials of topical nasal steroids specifically in AFRS are limited. Extrapolating from the benefits of topical steroids in CRS, many AFRS patients are managed with steroid sprays and irrigations [9, 16]. Several studies have investigated the role of antifungal therapy in the management of AFRS with some improvements noted in symptoms and endoscopic appearance, though there are design flaws in several of these studies limiting the evidence for, and the widespread use of antifungals in the management of AFRS [18,19,20,21]. Immunotherapy has also been explored as a therapeutic option in AFRS. In the systematic review by Gan et al. [16], 5 studies were identified that showed modest improvement in polyp burden and reduced need for additional steroid in patients undergoing immunotherapy. Thus, immunotherapy was recommended as an option for use in refractory cases of AFRS. Recently, biologic therapies targeting the Th2 inflammatory pathway have been incorporated in the treatment algorithm of CRSwNP. Omalizumab [22, 23], mepolizumab [24, 25], and dupilumab [26] are the most widely studied biologics in CRS; however, these studies did not focus on patients meeting diagnostic criteria for AFRS. Gan et al. [27] retrospectively reviewed 7 AFRS patients receiving omalizumab and found improvement in quality of life and endoscopy scores. Further prospective trials are needed to identify outcomes of biologic therapy on AFRS.
Eosinophilic Chronic Rhinosinusitis
Characteristics of Disease
Eosinophilic CRS is a subset of CRS that usually presents with extensive sinus disease [28]. Patients with eosinophilic chronic rhinosinusitis (eCRS) typically develop symptoms in the 4th–6th decade of life, usually without a history of significant allergic disease [29]. The presence of high tissue eosinophilia is known to confer worse post-operative outcomes, higher symptoms scores, less quality of life improvement, and higher risk of polyp recurrence [30,31,32]. These patients almost always present with comorbid lower airway disease including asthma, chronic cough, or wheezing [29]. Smell loss is also a common feature due to the extensive nature of sinus disease. Some patients will present with a subtype of CRS, aspirin exacerbation respiratory disease (AERD) that includes exacerbations related to nonsteroidal anti-inflammatory use due to blocking of the cyclooxygenase pathway and shunting of arachidonic acid metabolism toward leukotriene synthesis.
Historically, the diagnosis of eCRS has relied on the presence of elevated levels of tissue eosinophilia. There has been a debate over what level of eosinophilia dictates a diagnosis of eCRS; however, the majority of studies define a value of > 10 eosinophils per high power field on histopathology of sinus mucosa to be consistent with a diagnosis of eCRS [28, 29]. Radiographically, these patients have high Lund-Mackay CT scores, with a majority of patients presenting with pan-sinus opacification and evidence of neo-osteogenesis related to long-standing inflammation [29].
Inflammatory Profile
Similar to other phenotypes of CRS, the investigation of the underlying inflammatory pathway in eCRS is an active area of research. Previous studies have correlated the presence of eCRS with upregulation of Th2-mediated inflammation [5, 33]. Understanding the inflammatory profile, namely the role of Th2 cytokines IL-4 and IL-5, has led to the incorporation of new biologic therapies in the management of eCRS.
Management of eCRS
The treatment of eCRS relies on controlling the underlying inflammatory response, in addition to appropriate endoscopic sinus surgery. Similar to AFRS, these patients are typically very responsive to corticosteroids, both systemic and topical. Intermittent short courses of systemic steroids may be used to treat exacerbations or severed disease [34, 35]. However, use of systemic steroids more than 2–3 times per year is associated with increased risk of corticosteroid-related adverse effects. Topical steroids have shown promise in managing polyp recurrence in post-surgical cavities as well as managing milder disease. A randomized controlled trial has shown that large volume corticosteroid irrigations improve symptom control over corticosteroid sprays [36].
Despite adequate surgery and appropriate post-operative medical therapy, polyp recurrence may occur in a small percentage of eCRS patients. The frontal and ethmoid sinus cavities are at higher risk for polyp recurrence, though there is uncertainty whether this is related to limited access to topical therapy or an underlying propensity for more severe disease in these locations [34]. The advent of biologic therapies has offered another treatment option for these difficult to control patients. Omalizumab, an anti-IgE biologic, was shown to provide modest improvement in nasal polyp and CT scores in 2 small randomized controlled trials [22, 23]. Similarly, a large double-blind, randomized, placebo-controlled trial investigating mepolizumab, an anti-IL5, demonstrated significant improvement in nasal polyp scores and reduced need for surgery in patients receiving the biologic therapy [25]. Dupilumab targets IL-4 and IL-13 and has shown promise in treating CRSwNP, with significant improvement in Lund-Mackay CT scores and sinonasal outcome test-22 (SNOT-22) scores while receiving treatment which has been noted in phase 3 trials [26].
Central Compartment Atopic Disease
Characteristics of Disease
Central compartment atopic disease (CCAD) is a newly described phenotype of CRS that is strongly associated with inhalant allergy [37•]. CCAD is described as the deposition of allergens (via the pathway of normal airflow) within the central compartment of the nose: the middle and superior turbinates and posterior-superior nasal septum [37•]. CCAD patients generally have a strong allergy history, with 93% of patients having positive allergy testing in one study [38]. In contrast to eCRS, however, the prevalence of comorbid asthma in CCAD is quite low [38]. Characteristic radiographic findings of CCAD are that of centralized edema and mucosal thickening. The lateral sinuses are spared unless they become secondarily obstructed from the central disease [39]. Similarly, endoscopy reveals inflammation and polypoid changes along the middle and superior turbinates and nasal septum [37•, 38].
Inflammatory Profile
The association between central compartment atopic disease and inhalant allergy points toward an IgE-mediated pathway as the driver of the disease [37•]. CCAD patients will routinely demonstrate elevated and specific total IgE with a lack of serum eosinophilia [29]. IgE production is mediated through a Th2 pathway; however, further research on this unique patient population is required to fully characterize the endotype in CCAD.
Management
Treatment of the underlying inhalant allergy is key to controlling symptoms in CCAD [37•]. Surgery does have a role in removing polyps and preventing secondary obstruction of the lateral sinuses; however, it is not uncommon for post-operative symptoms to remain unchanged despite clear sinuses. Allergy-directed pharmacotherapy, including topical steroid sprays and irrigations, is generally used first line in these patients [37•, 38]. In patients whose symptoms remain uncontrolled, immunotherapy should be considered, although no studies to date have evaluated the effect of immunotherapy on CCAD. Omalizumab may play a role in otherwise medically refractory CCAD, although more studies are needed to assess its efficacy in managing symptoms and inflammation in this unique patient population.
Non-eosinophilic CRS
Characteristics of Non-eCRS
In contrast to eCRS, patients with non-eCRS typically present with more facial pain and pressure as opposed to nasal obstruction and anosmia [5]. The patient population has been reported to be predominantly female and middle-aged, usually with no history of significant allergy [29]. Non-eCRS has also been associated with obesity and history of tobacco use [40]. Historically, it was felt that non-eCRS patients were akin to CRSsNP patients; however, non-eCRS may still present with nasal polyps, particularly in Asian countries [41]. Radiographically, non-eCRS patients may be indistinguishable from those with eCRS.
Inflammatory Profile in Non-eCRS
The inflammatory response in non-eCRS tends to be driven by a non-Th2-mediated pathway. Non-eCRS is characterized by neutrophil-predominant inflammation and is associated with increased fibrosis and basement membrane remodeling [41]. Tissue neutrophilia in these patients has been correlated with the presence of non-Th2 inflammatory cytokines, and naturally, these patients have low eosinophil and IgE levels [42].
Management of Non-eCRS
Patients with non-eCRS may become frustrated as their symptoms are often not as steroid responsive as patients with eCRS or Th2-mediated inflammation. These patients may still benefit from endoscopic sinus surgery in an effort to resolve post-obstructive disease, although they tend to have persistent symptoms after surgery. It is the non-eCRS patients, however, that tend to have the greatest response to low-dose long-term macrolide therapy [43•]. Macrolides are known to have both anti-inflammatory and immunomodulatory properties. Studies have shown reduced production of pro-inflammatory cytokines IL2, IL-6, IL-8, and tumor necrosis factor-a (TNFa) with macrolide therapy [44, 45]. Additionally, clinical studies have reported improved quality of life and endoscopy in non-eCRS patients after treatment with macrolides [46]. Oakley et al. [43•] reported on characteristics that predicted response to macrolide therapy, identifying that low serum and tissue eosinophilia and absence of squamous metaplasia were positive predictors [43•]. Some surgeons prefer to use macrolide therapy as an adjunct after appropriate surgery and standard post-operative therapy fails and when there is pathologically proven low eosinophilia.
Secondary Chronic Rhinosinusitis Phenotypes (Fig. 2)
Localized Secondary CRS
Characteristics of Localized Secondary CRS
Localized secondary CRS includes odontogenic sinusitis, fungal ball, and CRS related to neoplasm, facial trauma, and foreign bodies. Odontogenic sinusitis has a reported prevalence of between 12 and 25% in CRS patients [47, 48]. It is typically observed in patients older than 40 years of age with a history of previous dental work. Symptoms include upper teeth pain, foul smelling drainage, and resistance to standard therapy. Radiography usually shows unilateral maxillary sinus opacification, though occasionally disease can extend into the anterior ethmoid and frontal sinus in a post-obstructive manner [47, 49]. It is important to recognize an odontogenic source in these patients as failure to do so can result in incomplete response to medical and surgical therapy [48]. Fungal balls are a non-invasive form of fungal sinusitis, and similar to odontogenic sinusitis, more commonly affect the maxillary sinus. Presenting symptoms of fungal balls are similar to that of other forms of CRS with facial pain, congestion, and nasal drainage. Imaging findings consistent with fungal ball include the presence of hyperdense ferromagnetic material within the sinus secretions as well as neo-osteogenesis of the sinus walls [50,51,52]. Benign and malignant tumors of the sinuses or nasal cavity can also precipitate a local inflammatory response in the sinuses usually secondary to obstruction of normal mucociliary flow.
Management of Localized Secondary CRS
Treatment of localized secondary cases of CRS typically involves surgical intervention as first line since anatomic modifications assist in treatment of the condition. Important in the management of odontogenic sinusitis is addressing the underlying dental pathology. Some studies have suggested that management of the dental pathology alone may be sufficient to manage disease and symptoms [48, 53]. Craig et al. [47] recently reported that upfront endoscopic sinus surgery may result in quicker resolution of symptoms and endoscopic improvement, particularly in patients with greater symptom scores at baseline. Treatment of sinus fungal balls is similar to other forms of localized secondary CRS. Symptoms typically resolve with standard endoscopic sinus surgery with very low reported recurrence rate of the fungal ball (~ 1%) [52]. However, patients may suffer from residual symptoms due to neo-osteogenesis or failure to recover normal mucociliary clearance.
Diffuse Secondary CRS
Characteristics of Diffuse Secondary CRS
Diffuse secondary CRS is the result of systemic diseases that also affect the sinonasal cavities. These can be broadly categorized into the following: diseases that affect the normal mucociliary clearance, autoimmune inflammatory diseases, and immunodeficiency.
Primary ciliary dyskinesia (PCD) and cystic fibrosis (CF) are autosomal recessive genetic diseases that impair normal mucociliary clearance in the sinuses. Sinusitis in PCD results from structural abnormalities of the cilia leading to downstream mucus stasis in the upper and lower airways. Sinusitis in PCD is typically diffuse, associated with sinus hypoplasia, and commonly presents with edema or frank polyposis [54, 55]. The genetic defect in CF affects a chloride transporter, the cystic fibrosis transmembrane conductance regulator (CFTR). Decreased chloride transport leads to increased viscosity of the airway-surface liquid, similarly resulting in decreased mucociliary transport [56]. Patients with the most common genetic defect, also the most severe form of the disease, usually present early in life with symptoms of CRS associated with polyposis and pan-sinus opacification. It is not uncommon for there to be hypoplasia or aplasia of the maxillary and frontal sinuses in CF [57, 58]. CF CRS is managed similar to idiopathic CRS, although recent advances in CF therapy may change this. Endoscopic sinus surgery is generally recommended for CF patients who fail maximal medical therapy. CFTR modulators have shown promise in treating CF lung and sinus disease [59,60,61,62].
Systemic autoimmune diseases may also have sinonasal involvement. Eosinophilic granulomatosis with polyangiitis (EGPA), formerly Churg-Strauss, is a small vessel-necrotizing vasculitis associated with asthma, rhinosinusitis, and evidence of vasculitis. These patients have diffuse tissue eosinophilia and thus present similar to patients with eCRS [63, 64]. Granulomatosis with polyangiitis (GPA), formerly Wegner’s granulomatosis, is another small vessel vasculitis affecting primarily the upper and lower airways and kidneys. Clinical manifestations of GPA include severe nasal crusting, epistaxis, and septal cartilage necrosis leading to saddle nose deformity [65, 66]. On endoscopy, polypoid nodules, white submucosal nodules, and bloody submucosal patches can be identified [65].
CRS secondary to immunodeficiency is an important consideration, particularly in difficult to treat patients. A meta-analysis in 2015 found immunoglobulin deficiencies in 23% of patients with refractory CRS [67]. Selective IgA deficiency, common variable immunodeficiency, and IgG subclass deficiencies are the most common findings in CRS [68]. Immunodeficiency-related CRS presents in a similar fashion to idiopathic CRS; thus, diagnosis of the immunodeficiency is often delayed. Recalcitrance to standard treatment and associated lower respiratory tract infections may direct the otolaryngologist to consider immunodeficiency [7••, 67, 68]. The extent of immunodeficiency workup prior to involving an immunologist is a topic of debate and largely depends on the depth of knowledge of the otolaryngologist [7••]. Specific studies investigating the management of immunodeficiency in CRS are limited, and further studies investigating the effect of immunoglobulin replacement, prophylactic antibiotics, and surgery on immunodeficiency-related CRS are needed.
Conclusion
Mounting evidence indicates that the classification of CRS patients into patients with or without nasal polyps is outdated and not clinically useful. Recent research has elucidated underlying inflammatory profiles that may guide precise treatment strategies for CRS patients. The newly described classification system provides more clinically relevant nomenclature relating to the diagnosis and specific treatment strategy for the different subgroups of CRS patients than the broad generalizations that have been used in the past (Table 1).
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Bachert C, Akdis CA. Phenotypes and emerging endotypes of chronic rhinosinusitis. J Allergy Clin Immunol Pract. 2016;4:621–8 Comment: Good overview of different phenotypes and corresponding endotypes.
Steinke JW, Borish L. Chronic rhinosinusitis phenotypes. Ann Allergy Asthma Immunol. 2016;117:234–40.
Han JK. Subclassification of chronic rhinosinusitis. Laryngoscope. 2013;123(Suppl 2):S15–27.
Wang X, Zhang N, Bo M, et al. Diversity of TH cytokine profiles in patients with chronic rhinosinusitis: a multicenter study in Europe, Asia, and Oceania. J Allergy Clin Immunol. 2016;138:1344–53.
Stevens WW, Peters AT, Tan BK, et al. Associations between inflammatory endotypes and clinical presentations in chronic rhinosinusitis. J Allergy Clin Immunol Pract. 2019;7:2812–20 e2813.
Naclerio RM, Baroody FM. Other phenotypes and treatment of chronic rhinosinusitis. J Allergy Clin Immunol Pract. 2016;4:613–20.
•• Fokkens WJ, Lund VJ, Hopkins C, et al. European position paper on rhinosinusitis and nasal polyps 2020. Rhinology. 2020;58:1–464 Comment: Discusses emerging definitions of CRS subclassifications.
Thahim K, Jawaid MA, Marfani MS. Presentation and management of allergic fungal sinusitis. J Coll Physicians Surg Pak. 2007;17:23–7.
Tyler MA, Luong AU. Current understanding of allergic fungal rhinosinusitis. World J Otorhinolaryngol Head Neck Surg. 2018;4:179–85.
Promsopa C, Kansara S, Citardi MJ, Fakhri S, Porter P, Luong A. Prevalence of confirmed asthma varies in chronic rhinosinusitis subtypes. Int Forum Allergy Rhinol. 2016;6:373–7.
Bent JP 3rd, Kuhn FA. Diagnosis of allergic fungal sinusitis. Otolaryngol Head Neck Surg. 1994;111:580–8.
Rowan NR, Janz TA, Schlosser RJ, Soler ZM. Radiographic nuances in allergic fungal rhinosinusitis. Am J Rhinol Allergy. 2019;33:310–6.
Tyler MA, Padro Dietz CJ, Russell CB, et al. Distinguishing molecular features of allergic fungal rhinosinusitis. Otolaryngol Head Neck Surg. 2018;159:185–93.
Wise SK, Ahn CN, Lathers DM, Mulligan RM, Schlosser RJ. Antigen-specific IgE in sinus mucosa of allergic fungal rhinosinusitis patients. Am J Rhinol. 2008;22:451–6.
Tyler MA, Russell CB, Smith DE, et al. Large-scale gene expression profiling reveals distinct type 2 inflammatory patterns in chronic rhinosinusitis subtypes. J Allergy Clin Immunol. 2017;139:1061–4 e1064.
Gan EC, Thamboo A, Rudmik L, Hwang PH, Ferguson BJ, Javer AR. Medical management of allergic fungal rhinosinusitis following endoscopic sinus surgery: an evidence-based review and recommendations. Int Forum Allergy Rhinol. 2014;4:702–15.
Orlandi RR, Kingdom TT, Hwang PH, et al. International consensus statement on allergy and rhinology: rhinosinusitis. Int Forum Allergy Rhinol. 2016;6(Suppl 1):S22–209.
Khalil Y, Tharwat A, Abdou AG, et al. The role of antifungal therapy in the prevention of recurrent allergic fungal rhinosinusitis after functional endoscopic sinus surgery: a randomized, controlled study. Ear Nose Throat J. 2011;90:E1–7.
Rojita M, Samal S, Pradhan P, Venkatachalam VP. Comparison of steroid and itraconazole for prevention of recurrence in allergic fungal rhinosinusitis: a randomized controlled trial. J Clin Diagn Res. 2017;11:MC01–3.
Seiberling K, Wormald PJ. The role of itraconazole in recalcitrant fungal sinusitis. Am J Rhinol Allergy. 2009;23:303–6.
Chan KO, Genoway KA, Javer AR. Effectiveness of itraconazole in the management of refractory allergic fungal rhinosinusitis. J Otolaryngol Head Neck Surg. 2008;37:870–4.
Pinto JM, Mehta N, DiTineo M, Wang J, Baroody FM, Naclerio RM. A randomized, double-blind, placebo-controlled trial of anti-IgE for chronic rhinosinusitis. Rhinology. 2010;48:318–24.
Gevaert P, Calus L, Van Zele T, et al. Omalizumab is effective in allergic and nonallergic patients with nasal polyps and asthma. J Allergy Clin Immunol. 2013;131:110–6 e111.
Gevaert P, Van Bruaene N, Cattaert T, et al. Mepolizumab, a humanized anti-IL-5 mAb, as a treatment option for severe nasal polyposis. J Allergy Clin Immunol. 2011;128:989–95 e981–988.
Bachert C, Sousa AR, Lund VJ, et al. Reduced need for surgery in severe nasal polyposis with mepolizumab: randomized trial. J Allergy Clin Immunol. 2017;140:1024–31 e1014.
Bachert C, Han JK, Desrosiers M, et al. Efficacy and safety of dupilumab in patients with severe chronic rhinosinusitis with nasal polyps (LIBERTY NP SINUS-24 and LIBERTY NP SINUS-52): results from two multicentre, randomised, double-blind, placebo-controlled, parallel-group phase 3 trials. Lancet. 2019;394:1638–50.
Gan EC, Habib AR, Rajwani A, Javer AR. Omalizumab therapy for refractory allergic fungal rhinosinusitis patients with moderate or severe asthma. Am J Otolaryngol. 2015;36:672–7.
Lou H, Zhang N, Bachert C, Zhang L. Highlights of eosinophilic chronic rhinosinusitis with nasal polyps in definition, prognosis, and advancement. Int Forum Allergy Rhinol. 2018;8:1218–25.
Grayson JW, Cavada M, Harvey RJ. Clinically relevant phenotypes in chronic rhinosinusitis. J Otolaryngol Head Neck Surg. 2019;48:23.
Vlaminck S, Vauterin T, Hellings PW, et al. The importance of local eosinophilia in the surgical outcome of chronic rhinosinusitis: a 3-year prospective observational study. Am J Rhinol Allergy. 2014;28:260–4.
Tosun F, Arslan HH, Karslioglu Y, Deveci MS, Durmaz A. Relationship between postoperative recurrence rate and eosinophil density of nasal polyps. Ann Otol Rhinol Laryngol. 2010;119:455–9.
Van Zele T, Holtappels G, Gevaert P, Bachert C. Differences in initial immunoprofiles between recurrent and nonrecurrent chronic rhinosinusitis with nasal polyps. Am J Rhinol Allergy. 2014;28:192–8.
Bachert C, Gevaert P, Holtappels G, Cuvelier C, van Cauwenberge P. Nasal polyposis: from cytokines to growth. Am J Rhinol. 2000;14:279–90.
Grayson JW, Li W. Ho Jet al. Int Forum Allergy Rhinol: Topography of polyp recurrence in eosinophilic chronic rhinosinusitis; 2020.
Grayson JW, Harvey RJ. Topical corticosteroid irrigations in chronic rhinosinusitis. Int Forum Allergy Rhinol. 2019;9:S9–S15.
Harvey RJ, Snidvongs K, Kalish LH, Oakley GM, Sacks R. Corticosteroid nasal irrigations are more effective than simple sprays in a randomized double-blinded placebo-controlled trial for chronic rhinosinusitis after sinus surgery. Int Forum Allergy Rhinol. 2018;8:461–70.
• DelGaudio JM, Loftus PA, Hamizan AW, Harvey RJ, Wise SK. Central compartment atopic disease. Am J Rhinol Allergy. 2017;31:228–34 Comment: Description of new subclassification: CCAD.
Marcus S, Schertzer J, Roland LT, Wise SK, Levy JM, DelGaudio JM. Central compartment atopic disease: prevalence of allergy and asthma compared with other subtypes of chronic rhinosinusitis with nasal polyps. Int Forum Allergy Rhinol. 2020;10:183–9.
Hamizan AW, Loftus PA, Alvarado R, et al. Allergic phenotype of chronic rhinosinusitis based on radiologic pattern of disease. Laryngoscope. 2018;128:2015–21.
Oakley GM, Harvey RJ, Lund VJ. The role of macrolides in chronic rhinosinusitis (CRSsNP and CRSwNP). Curr Allergy Asthma Rep. 2017;17:30.
Cho SW, Kim DW, Kim JW, Lee CH, Rhee CS. Classification of chronic rhinosinusitis according to a nasal polyp and tissue eosinophilia: limitation of current classification system for Asian population. Asia Pac Allergy. 2017;7:121–30.
Morse JC, Li P, Ely KA, et al. Chronic rhinosinusitis in elderly patients is associated with an exaggerated neutrophilic proinflammatory response to pathogenic bacteria. J Allergy Clin Immunol. 2019;143:990–1002 e1006.
• Oakley GM, Christensen JM, Sacks R, Earls P, Harvey RJ. Characteristics of macrolide responders in persistent post-surgical rhinosinusitis. Rhinology. 2018;56:111–7 Comment: Shows the role of macrolides in the management of non-eCRS.
Suzuki H, Shimomura A, Ikeda K, Furukawa M, Oshima T, Takasaka T. Inhibitory effect of macrolides on interleukin-8 secretion from cultured human nasal epithelial cells. Laryngoscope. 1997;107:1661–6.
Tamaoki J, Kadota J, Takizawa H. Clinical implications of the immunomodulatory effects of macrolides. Am J Med. 2004;117(Suppl 9A):5S–11S.
Wallwork B, Coman W, Mackay-Sim A, Greiff L, Cervin A. A double-blind, randomized, placebo-controlled trial of macrolide in the treatment of chronic rhinosinusitis. Laryngoscope. 2006;116:189–93.
Craig JR, McHugh CI, Griggs ZH, Peterson EI. Optimal timing of endoscopic sinus surgery for odontogenic sinusitis. Laryngoscope. 2019;129:1976–83.
Longhini AB, Ferguson BJ. Clinical aspects of odontogenic maxillary sinusitis: a case series. Int Forum Allergy Rhinol. 2011;1:409–15.
Grayson JW, Hopkins C, Mori E, Senior B, Harvey RJ. Contemporary classification of chronic rhinosinusitis: moving beyond CRSwNP and CRSsNP. JAMA Otolaryngol. 2020; In press.
Jiang RS, Huang WC, Liang KL. Characteristics of sinus fungus ball: a unique form of rhinosinusitis. Clin Med Insights Ear Nose Throat. 2018;11:1179550618792254.
Jun YJ, Shin JM, Lee JY, Baek BJ. Bony changes in a unilateral maxillary sinus fungal ball. J Craniofac Surg. 2018;29:e44–7.
Yoon YH, Xu J, Park SK, Heo JH, Kim YM, Rha KS. A retrospective analysis of 538 sinonasal fungus ball cases treated at a single tertiary medical center in Korea (1996-2015). Int Forum Allergy Rhinol. 2017;7:1070–5.
Wang KL, Nichols BG, Poetker DM, Loehrl TA. Odontogenic sinusitis: a case series studying diagnosis and management. Int Forum Allergy Rhinol. 2015;5:597–601.
Alanin MC, Aanaes K, Hoiby N, et al. Sinus surgery can improve quality of life, lung infections, and lung function in patients with primary ciliary dyskinesia. Int Forum Allergy Rhinol. 2017;7:240–7.
Bhatt JM, Muhonen EG, Meier M, Sagel SD, Chan KH. Rhinosinusitis in pediatric primary ciliary dyskinesia: impact of disease. Otolaryngol Head Neck Surg. 2019;161:877–80.
Lowery AS, Gallant JN, Woodworth BA, et al. Chronic rhino-sinusitis treatment in children with cystic fibrosis: a cross-sectional survey of pediatric pulmonologists and otolaryngologists. Int J Pediatr Otorhinolaryngol. 2019;124:139–42.
Grayson J, Tipirneni KE, Skinner DF, et al. Sinus hypoplasia in the cystic fibrosis rat resolves in the absence of chronic infection. Int Forum Allergy Rhinol. 2017;7:904–9.
Woodworth BA, Ahn C, Flume PA, Schlosser RJ. The delta F508 mutation in cystic fibrosis and impact on sinus development. Am J Rhinol. 2007;21:122–7.
Middleton PG, Mall MA, Drevinek P, et al. Elexacaftor-Tezacaftor-Ivacaftor for cystic fibrosis with a single Phe508del allele. N Engl J Med. 2019;381:1809–19.
McCormick J, Cho DY, Lampkin B, et al. Ivacaftor improves rhinologic, psychologic, and sleep-related quality of life in G551D cystic fibrosis patients. Int Forum Allergy Rhinol. 2019;9:292–7.
Rowe SM, Heltshe SL, Gonska T, et al. Clinical mechanism of the cystic fibrosis transmembrane conductance regulator potentiator ivacaftor in G551D-mediated cystic fibrosis. Am J Respir Crit Care Med. 2014;190:175–84.
Lommatzsch ST, Taylor-Cousar JL. The combination of tezacaftor and ivacaftor in the treatment of patients with cystic fibrosis: clinical evidence and future prospects in cystic fibrosis therapy. Ther Adv Respir Dis. 2019;13:1753466619844424.
Seccia V, Baldini C, Latorre M, et al. Focus on the involvement of the nose and paranasal sinuses in eosinophilic granulomatosis with polyangiitis (Churg-Strauss syndrome): nasal cytology reveals infiltration of eosinophils as a very common feature. Int Arch Allergy Immunol. 2018;175:61–9.
Greco A, Rizzo MI, De Virgilio A, et al. Churg-Strauss syndrome. Autoimmun Rev. 2015;14:341–8.
Beltran Rodriguez-Cabo O, Reyes E, Rojas-Serrano J, Flores-Suarez LF. Increased histopathological yield for granulomatosis with polyangiitis based on nasal endoscopy of suspected active lesions. Eur Arch Otorhinolaryngol. 2018;275:425–9.
Greco A, Marinelli C, Fusconi M, et al. Clinic manifestations in granulomatosis with polyangiitis. Int J Immunopathol Pharmacol. 2016;29:151–9.
Schwitzguebel AJ, Jandus P, Lacroix JS, Seebach JD, Harr T. Immunoglobulin deficiency in patients with chronic rhinosinusitis: systematic review of the literature and meta-analysis. J Allergy Clin Immunol. 2015;136:1523–31.
Ocampo CJ, Peters AT. Antibody deficiency in chronic rhinosinusitis: epidemiology and burden of illness. Am J Rhinol Allergy. 2013;27:34–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Woodworth is a consultant for Cook Medical, Smith and Nephew, and Baxter, outside the submitted work. The other authors declare no conflicts of interest relevant to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Rhinitis, Conjunctivitis, and Sinusitis
Rights and permissions
About this article
Cite this article
McCormick, J.P., Thompson, H.M., Cho, DY. et al. Phenotypes in Chronic Rhinosinusitis. Curr Allergy Asthma Rep 20, 20 (2020). https://doi.org/10.1007/s11882-020-00916-6
Published:
DOI: https://doi.org/10.1007/s11882-020-00916-6