Abstract
Electrocauterization causes foul smells and surgical smoke that affect operating room (OR) air quality. This study analyzed the concentration distribution of 87 volatile organic compounds (VOCs) in surgical smoke generated during head and neck surgeries and evaluated their size and concentration using pig skin and pork tissues. Surgical smoke from 22 head and neck surgeries were collected; VOC concentrations were analyzed using a gas chromatography–mass spectrometry. In vitro experiments utilized an electrosurgical model to burn pig skin and pork tissues; thereafter, the particle size and concentration of surgical smoke in different sampling areas were analyzed. High methanol and carcinogen levels were observed in the surgical smoke generated by head and neck surgeries. The concentrations of 87 identified VOCs in surgical smoke were affected by human tissues and electrosurgical units. Moreover, the median concentrations of particulate matter from the electrical burning of pig skin measured in the breathing area of simulated surgical personnel were significantly higher than those in pork tissue. High VOC levels in surgical smoke from head and neck surgeries were affected by human tissues and electrosurgical units. Ultrafine aerosols primarily existed in surgical smoke from the smoke generation area. Human oral mucosa tissues treated with carbon dioxide (CO2) lasers produced higher VOC concentrations than craniofacial adipose tissues that were treated using conventional electrosurgical knives. Medical staff in ORs should be informed of the hazards of exposure to VOCs and ultrafine aerosols in surgical smoke.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
An electrosurgical knife uses high-frequency currents to vigorously vibrate viscous body fluids in human tissue. Owing to frictional heat generation, the moisture in tissues evaporates rapidly to achieve tissue separation or coagulation (Massarweh et al. 2006). The electric cautery machine is used to cut tissue by heating cells to a boiling point of 100 °C (212 °F) using a continuous current. This causes cells to rupture, resulting in the evaporation of cell fluids. The coagulation function of the electric cautery machine uses an intermittent current to gradually increase the temperature of cell fluids. When the temperature is higher than 90 °C (194 °F), the fluid inside cells evaporates, proteins denature, and cells lose their structural integrity. Once the temperature reaches 200 °C (392 °F), tissues carbonize. During this time, cell debris are released into the air along with particulate matter (Massarweh et al. 2006).
Surgical smoke is composed of 95% water, 5% particulate matter, and gaseous pollutants (Ulmer 2008). The size distribution of suspended particles in ambient air is divided into coarse, fine, and ultrafine particles (Kwon et al. 2020). Particles larger than 2.5 µm are coarse particles, whereas fine particles have an aerodynamic diameter equal to or less than 2.5 µm (PM2.5) that can be suspended in the air for longer periods of time and inhaled (Kwon et al. 2020). Ultrafine suspended particles have an aerodynamic diameter of less than 0.1 µm (Li et al. 2019). Owing to their poor solubility, ultrafine suspended particles are easily transported from the lungs to the bloodstream (Moreno et al. 2021). VOCs including benzene, alkenes, formaldehyde, and polycyclic aromatic hydrocarbons are gaseous pollutants (Choi et al. 2014; Kocher et al. 2019). A Japanese study used pigs to perform laparoscopic surgery experiments and qualitatively identified 37 VOCs in surgical smoke samples. Among them, acetaldehyde and dimethylformamide have been identified by the International Agency for Research on Cancer (IARC) as compounds that pose health risks (Takahashi et al. 2013). Kocher et al. found an average concentration of 272.69 ppb of carcinogenic or toxic VOCs measured at the height of the surgeon’s nasal cavity without a suction device during thoracic surgery, with a maximum concentration of 8991 ppb. Among them, the average concentrations of pentadiene, crotonaldehyde, and g-butyrolactone measured in traditional thoracotomy were significantly higher than those in minimally invasive surgery, while the average concentrations of acetonitrile and acetaldehyde in minimally invasive surgery were significantly higher than those in traditional thoracotomy (Kocher et al. 2022).
Li et al. showed that the concentration of suspended particulates sized between 0.3 μm and 0.5 μm measured in the surgical area was significantly higher than that outside of the operating table after using the electrocautery knife for 5–10 min during otolaryngology surgery (Li et al. 2022). Eshleman et al. (2017) observed that the average concentration of ultrafine suspended particles (22,916.8 particles/cm3) generated during laser hair removal surgery was significantly higher than that in the waiting room (14,957.4 particles/cm3). Moreover, the concentration of ultrafine particles during operations was 2.89 times the background concentration measured before surgery. Ragde et al. (2016) pointed out that regardless of surgical smoke, ultrafine suspended particles account for > 70% of overall particle size distribution. Previous studies have found that high concentrations of ultrafine aerosols are absorbed by the human body and are associated with increased lung disease and cardiovascular mortality. Ultrafine particles can be detected in the body (liver, heart, and nervous system) even after a few hours of exposure (Moreno et al. 2021). In addition, they can induce inflammation and promote thrombosis, atherosclerosis, and other cardiovascular diseases (Schulz et al. 2005). Ultrafine particles not only affect lung function (Pietropaoli et al. 2004), but also indirectly affect the autonomic nervous system and directly lead to cell mutations in various organs (Harder et al. 2005; Samet et al. 2004). Long-term exposure to ultrafine particles in postmenopausal women may increase the incidence of cardiovascular disease and mortality (Miller et al. 2007). Rats exposed to the smoke generated by CO2 lasers suffered from lung diseases, such as interstitial pneumonia, bronchiolitis, and emphysema; furthermore, the risk of disease increased with longer exposure to smoke (Baggish and Elbakry 1987; Freitag et al. 1987; Wenig et al. 1993). Most surgical procedures produce high concentrations of suspended particles within a short period of time. These pollutants are not easily eliminated by the human body and may cause cumulative exposure hazards. Therefore, the exposure risk of OR personnel to surgical smoke needs to be urgently addressed.
Limited studies have evaluated the change in the concentrations of suspended particles and VOCs in surgical smoke generated from different tissues using different electrosurgical units. Thus, this study aimed to evaluate the composition and concentration distribution of VOCs in surgical smoke from human head and neck surgery and that of suspended particles in surgical smoke from pig tissues.
Materials and methods
Study location and subjects
This study selected three head and neck surgery ORs in the Linkuo Chang Gung Memorial Hospital in northern Taiwan. This research location was categorized as an International Organization for Standardization (ISO) 14644-1 class 7 (ISO 2015) and had room volumes between 110 and 140 m3. The indoor temperature and relative humidity in the head and neck surgery ORs were maintained between 19–23 °C and 55–65%, respectively. High-efficiency particulate air H14 filters were installed in the center ceiling of each OR and were replaced once per year. Throughout the day, ORs were ventilated at a rate between 20 and 22 air changes per hour, with approximately 85% of the total circulating airflow returning to the supply air system through four return air vents.
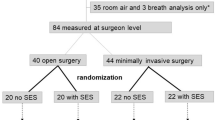
This study recruited 20 patients undergoing head and neck surgery during electrosurgical procedures. A total of 22 surgical smoke samples generated from head and neck surgery were collected, including craniofacial subcutaneous tissues (n = 10), craniofacial adipose tissues (n = 3), radix linguae tissue (n = 3) using conventional electrosurgical knives, and oral mucosa tissue (n = 6) using a CO2 laser.
Surgical smoke sampling and analysis
A 6-L evacuated canister was operated for 30 s following the National Institute for Occupational Safety and Health draft canister method (LeBouf et al. 2012) and the Taiwan Environmental Analysis Laboratory NIEA A715.15B standard (Environmental Analytical Laboratory 2014). The stainless steel canisters should be cleaned, humidified, and tested before sampling. After repeating this step of vacuuming/pressurizing for canisters, vacuum again until the pressure was less than 0.05 mmHg and maintain this vacuum for at least 1 h, followed by canister leak testing and confirmation of analytical work. A grab sampling was to open the sampling valve of the stainless steel canister to allow the surrounding air to enter the sampling canister. After the sampling was completed, the sampling valve was closed. The sample number was pasted on the canister, and the samples were sent back to the laboratory for analysis. During the sampling period, surgical smoke was collected as close to the surgical site as possible (2–3 cm). A 10% stainless steel canister was used as the blank sample to ensure the canisters without contamination interference that may be from incorrect operation, incomplete cleaning or contamination of the analytical system. Additionally, a gas chromatography–mass spectrometry analysis, which was based on the Taiwan Environmental Analysis Laboratory NIEA A715.15B standard (Environmental Analytical Laboratory 2014), was used to analyze the composition and concentration of 87 VOCs in surgical smoke. The relative standard difference and recovery rates were below 25% and ranged between 70–130% in the surgical smoke samples. According to the IARC classification (IARC groups 1, 2A, 2B, and 3) based on the identification of carcinogenic hazards to humans (IARC 2022), this study also assessed the presence of IARC-classified carcinogens in surgical smoke. Moreover, the electrosurgical unit, electricity power, human tissues, and indoor thermal-hygrometric conditions of the ORs were recorded.
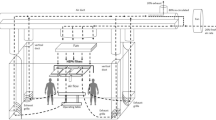
Simulating surgical smoke generation and monitoring particle size and concentration changes
In this study, pig skin and tissues were electrically burned to simulate surgical smoke. The electric burning process was carried out in a laboratory fume hood. A particle sampling device was installed in the smoke production area (10 cm from the electric-burning tissue) and the breathing area of simulated surgical personnel (40 cm from the electric-burning tissue) to simulate the clinical surgery situation. The electric burning process used the monopolar electric knife mode at 30 W to perform continuous electrocoagulation for 15 s, followed by a break for 45 s; this process lasted for 5 min. Once the process was completed, the exhaust system was turned on for 30 min, after which the background concentration was measured. When the obtained concentration was the same as the background concentration, the next set of experiments was started. Three replicate experiments were performed for each pig tissue sample.
This study used a direct-reading particle size analyzer (GRIMM particle size analyzer, model 1.109, Germany) and a handheld nanoparticle monitor (NanoTracer, Oxility, US) to determine the concentration and size of the particles. The direct-reading particle size analyzer measured particle concentrations of 0.265–34 μm in 31 size channels at a sampling flow rate of 1.2 L/min every 6 s. The particle sampling of the particle size analyzer was isokinetic sampling to have a possibly small measuring error. Additionally, the handheld nanoparticle monitor measured particle concentrations of 0.01–0.3 μm at a sampling flow rate of 0.3–0.4 L/min every 10 s. The measurement technology of the nanoparticle monitor was diffusion charging.
Data analysis
SPSS version 25.0 (SPSS, Chicago, Illinois, USA) was used for statistical analyses. The figures were graphed with GraphPad Prism 7.0 software (GraphPad Software, Inc., San Diego, CA, USA). The significance level was set at P < 0.05. The Kruskal–Wallis test and Mann–Whitney U test were used to analyze the composition and change in VOC concentrations in surgical smoke in different human tissues and electrosurgical units. In addition, the above statistical methods were used to analyze the differences in the number and mass concentrations of the suspended particulates monitored in the smoke generation area and breathing area of stimulated surgical personnel when analyzing pig skin and pork tissues that were electrically burned.
Results
The range of indoor temperature and relative humidity values in the ORs where head and neck surgeries were performed were 18.82–22.96 °C and 43.37–66.20%, respectively. The dominant surgeries performed in the ORs included submaxillary gland tumor ablations, neck mass excisions, and oral tumor excisions. This study found that the median value of 87 VOC concentration generated from oral mucosa tissues (1411.77 ppb) using CO2 lasers was significantly higher than that from adipose tissues (406.92 ppb, P = 0.039). However, there was no difference in the concentration of VOCs generated from craniofacial subcutaneous tissues (2708.32 ppb) and radix linguae tissues (3510.85 ppb) when using conventional electrosurgical knives, as shown in Fig. 1.
The mean level of methanol (1917.68 ppb) generated from craniofacial subcutaneous tissue using conventional electrosurgical knives was the highest, followed by acetonitrile (529.97 ppb), propane (212.29 ppb), acetone (184.01 ppb), 1,3-butadiene (182.62 ppb), acrylonitrile (146.38 ppb), acrolein (123.31 ppb), benzene (63.92 ppb), 1-hexene (59.59 ppb), and chloromethane (37.28 ppb) (Table 1). The mean level of methanol (622.91 ppb) generated from craniofacial adipose tissues using conventional electrosurgical knives was the highest, followed by acetonitrile (340.41 ppb), propane (180.28 ppb), 1,3-butadiene (175.18 ppb), acrolein (166.16 ppb), acetone (77.41 ppb), acrylonitrile (75.53 ppb), 1-hexene (69.61 ppb), trans-2-butadiene (48.23 ppb), and benzene (43.2 ppb). The mean levels of methanol (2,511.2 ppb) generated from craniofacial adipose tissues using conventional electrosurgical knives was the highest, followed by acetonitrile (826.83 ppb), acetone (617.5 ppb), propane (420.58 ppb), acrolein (296.49 ppb), 1,3-butadiene (283.54 ppb), acrylonitrile (260.93 ppb), benzene (163.03 ppb), 1-hexene (126.69 ppb), and chloromethane (102.77 ppb). Furthermore, the VOCs generated from oral mucosa tissues using CO2 laser primarily included acetonitrile (539.9 ppb), methanol (372.05 ppb), acetone (160.66 ppb), acrylonitrile (129.88 ppb), chloromethane (79.82 ppb), methyl methacrylate (74.68 ppb), propane (62.75 ppb), toluene (44.29 ppb), 1,3-butadiene (33.25 ppb), and 2-butanone (27.79 ppb). This study further evaluated the changes in the concentration of carcinogenic VOC generated from head and neck surgery using conventional electrosurgical knives and a CO2 laser. According to the results, the median levels of the IARC group 1’s benzene (54.75 ppb) and 1,3-butadiene (137.1 ppb) generated from craniofacial subcutaneous tissues, using conventional electrosurgical knives were significantly higher than from oral mucosa tissues (benzene: 16.53 ppb, P = 0.023; 1,3-butadiene: 27.83 ppb, P = 0.02) using CO2 lasers. However, this study found no difference in the median vinyl chloride level generated from head and neck surgeries using different types of electrosurgical units. Furthermore, no differences were found between the median levels of the IARC group 2A generated from craniofacial subcutaneous tissues (benzyl chloride: 0.93 ppb; methylene chloride: 0.68 ppb; styrene: 5.07 ppb), craniofacial adipose tissues (benzyl chloride: under detection limit; methylene chloride: 0.52 ppb; styrene: 1.33 ppb), radix linguae tissues (benzyl chloride: 0.57 ppb; methylene chloride: 0.72 ppb; styrene: 5.01 ppb), and oral mucosa tissues (benzyl chloride: 1.18 ppb; methylene chloride: 0.75 ppb; styrene: 3.77 ppb) using CO2 lasers. The median levels of the IARC group 2B generated from craniofacial subcutaneous tissues (acrylonitrile: 102.7 ppb; chloroform: 0.15 ppb; 1,2-dichloroethane: 0.38 ppb; ethyl-benzene: 4.76 ppb; vinyl acetate: 8.2 ppb), craniofacial adipose tissues (acrylonitrile: 31.31 ppb; chloroform: 0.18 ppb; 1,2-dichloroethane: 0.1 ppb; ethylbenzene: 1.57 ppb; vinyl acetate: 1.29 ppb), radix linguae (acrylonitrile: 142.3 ppb; chloroform: 0.2 ppb; 1,2-dichloroethane: under detection limit; ethylbenzene: 6.04 ppb; vinyl acetate: 10.36 ppb), and oral mucosa (acrylonitrile: 86.92 ppb; chloroform: 0.27 ppb; 1,2-dichloroethane: 0.11 ppb; ethylbenzene: 4.37 ppb; vinyl acetate: 4.84 ppb) using CO2 lasers were similar.
Figure 2 shows that the mean number and mass concentration distributions of suspended particles in surgical smoke samples from the smoke generation area and breathing area of simulated surgical personnel when pig skin and pork tissues were electrically burned. The number and mass concentrations of the background environment before electrocauterization were 0–2234.56 particles/m3 and 0–4.57 μg/m3, respectively, in the particle size of 0.265–34 μm. There were no statistically significant differences in the number and mass concentrations of particulate matter equal to or less than 10 μm in aerodynamic diameter (PM10), PM2.5, and particulate matter equal to or less than 1 μm in aerodynamic diameter (PM1) measured in the smoke generation area and breathing area of the simulated surgical personnel when pig skin tissue was electrically burned (Table 2). However, the median particle number concentration of particulate matter 0.01–0.3 μm in aerodynamic diameter (PM0.01–0.3) measured in the breathing area (1.48 × 1012 particles/m3) for simulated surgical personnel during the electric burning of pig skin was significantly lower than that of the smoke generation area (1.38 × 1013 particles/m3, P < 0.01). When the pork tissue was electrically burned, the median particle number concentration of particulate matter equal to or larger than 0.5 μm in aerodynamic diameter (PM≥0.5) (3.5 × 104 particles/m3), PM10 (2.76 × 106 particles/m3), PM2.5 (2.76 × 106 particles/m3), and PM1 (2.76 × 106 particles/m3) that was measured in the smoke generation area was significantly higher than that of the breathing area for simulated surgical personnel (PM≥0.5: 1.94 × 104 particles/m3, P < 0.01; PM10: 1.86 × 106 particles/m3, P < 0.01; PM2.5: 1.86 × 106 particles/m3, P < 0.01; PM1: 1.85 × 106 particles/m3, P < 0.01). Moreover, a comparison of the median mass concentrations of PM≥0.5, PM10, PM2.5, and PM1 measured in the smoke generation area and breathing area for simulated surgical personnel during the electric burning of pork tissue revealed a similar trend. Furthermore, the difference in concentration of ultrafine suspended particles measured in the smoke generating area and breathing area for simulated surgical personnel when different tissues were electronically burned was compared. This comparison revealed that the median concentration of ultrafine suspended particles in the smoke generating area (1.38 × 1013 particles/m3) when pig skin was electronically burned was significantly higher than that of pig tissue (4.16 × 1012 particles/m3, P < 0.01). The median concentration of ultrafine suspended particles measured in the breathing area of the simulated surgical personnel produced by electrically burning pork tissue (2.92 × 1012 particles/m3) was significantly higher than when electrically burning pork skin (1.48 × 1012 particles/m3, P < 0.01).
This study found that the average particle size (41 nm) of ultrafine suspended particles generated from electrically-burned pig skin measured in the smoke generation area was significantly smaller than that generated from electrically-burned pork tissue (54 nm, P < 0.01). When pig skin and pork tissue were electrically burned, the average particle sizes of ultrafine suspended particles measured in the breathing area of stimulated surgical personnel were 48 nm and 48.5 nm, respectively; a significant difference (P = 0.023) in particle size was found (Table 3).
Discussion
This study was the first to analyze the composition and concentration of VOCs in surgical smoke generated during head and neck surgery. The median values of 87 VOC concentration generated from craniofacial subcutaneous tissues and radix linguae tissues when using conventional electrosurgical knives were not significantly higher than that from craniofacial adipose tissues when using conventional electrosurgical knives and oral mucosa tissues when using CO2 lasers. This result would be associated with the less sample size and wide ranges of VOC concentrations generated from different human tissues (craniofacial subcutaneous tissues: 91.51–7321.32 ppb; craniofacial adipose tissues: 91.32–4651.47 ppb; radix linguae tissues: 680.16–13,766.06 ppb; oral mucosa tissues: 463.45–3421.47 ppb). It still warrants further attentions to the medical personnel in ORs. The results showed that the concentration of methanol was higher in surgical smoke generated by electrocauterization (craniofacial subcutaneous tissue: 1917.68 ppb, craniofacial adipose tissue: 622.91 ppb, radix linguae tissue: 2511.2 ppb). The concentration of methanol when different tissues of the human body were burned using an electrosurgical knife during surgery was 25–100 ppb, 77 times higher than the background air concentration measured during skin disinfection. This result was similar to that of the study by Cheng et al. (2021), which observed high concentrations of methanol when electrosurgical knives or plasma knifes were used to burn different parts of human tissue. Thus, methanol is a contaminant that cannot be ignored in surgical smoke. In addition, Cheng et al. (2021) and the National Institute of Occupational Safety and Health (Lee et al. 2018) concluded that ethanol and isopropanol were the main components in the surgical smoke generated from the electric burning of fibroadipose tissue. Our study found that ethanol and isopropanol were present in surgical smoke, but their concentration distribution differed from those reported in previous findings (Cheng et al. 2021; Lee et al. 2018). This could be due to the differences in human tissues, sampling conditions, and wattage.
Methanol is absorbed by the skin. Studies have pointed out that exposure to excessive methanol vapors can cause central nerve depression, which may lead to symptoms such as optic nerve damage, headaches, fatigue, and drowsiness (U.S. Coast Guard 1999). The US Occupational Safety and Health Administration recommends that the short-term average permissible concentration of methanol and maximum permissible concentration of methanol are 250 ppm and 1000 ppm, respectively. This level should not be breached to avoid the risk of irritation or chronic/irreversible tissue injury. In this study, the concentration of methanol during head and neck surgery did not exceed the recommended concentration; however, its potential health hazards cannot be ignored (OSHA 2021). Moreover, benzene (12.18–90 ppb), 1,3-butadiene (18.84–137.1 ppb), and vinyl chloride (0.86–3.09 ppb) were detected as first-level carcinogens during head and neck surgery. Previous animal experiments have also pointed out that long-term exposure to benzene, 1,3-butadiene, and vinyl chloride might be related to the occurrence of tumors (Melnick et al. 1990; Radike et al. 1981; Wong 1987). Due to the great variability in the types of surgeries and working hours that OR personnel were exposed to, the health risks to human body caused by surgical smoke are worthy of in-depth research in the future.
Given that particle sampling and analysis during actual human surgery may interfere with clinical operations, this study conducted in vitro experiments. The results revealed that when the pig skin or pork tissue was electrically burned, the surgical smoke in the smoke generation area and the breathing area of the simulated surgical personnel primarily contained ultrafine suspended particles. This deserves further attention and requires environmental monitoring in ORs. In addition, the mass concentration of suspended particles in the smoke generation area when the pig skin was electrically burned did not differ from that when the pork tissue was electrically burned. The mass concentration of suspended particles in the surgical smoke samples from pig skin and pork tissues was slightly higher than that reported by Karjalainen et al. (2018), which estimated the mass concentrations of suspended particles from electrically-burned pig skeletal muscle tissue (PM10: 3 × 106 μg/m3, PM2.5: 3.7 × 105 μg/m3, and PM1: 1.5 × 105 μg/m3) and electrically-burned pig skin (PM10: 3.7 × 105 μg/m3, PM2.5: 6.1 × 104 μg/m3, PM1: 3.4 × 104 μg/m3). The possible reason for this difference in mass concentration could be related to the use of a local smoke evacuation system during the experiment.
The size of ultrafine suspended particles ranged between 41 and 54 nm. A previous study indicated that the size of suspended particles generated from human surgery (hemihepatectomy, laparoscopic adhesiolysis, mesh hernia repair, biliodigestive anastomosis, and laparoscopic appendectomy) via electrocauterization and electrocoagulation ranged from 10 to 1000 nm, with concentrations reaching up to 100,000 particles/cm3 (Brüske-Hohlfeld et al. 2008). Thus, ultrafine aerosols were primarily produced from electrically burned tissues. The concentration of ultrafine aerosols in the surgical area varied with the surgical burn site. Exposure of OR personnel to ultrafine aerosols in surgical smoke required consideration of the duration and frequency of exposure (D'Alicandro and Mauro 2022). Past literature has pointed out that exposure of pregnant women to PM10 is associated with neural tube defects in newborns (Zhang et al. 2020). Furthermore, inhalation of PM10 may cause chest pain, cough, and dyspnea (Jiménez et al. 2009). It can also penetrate in the gas exchange area of the lungs, causing decreased lung function or increased risk of asthma (Pinkerton et al. 2000). Additionally, ultrafine suspended particles can infiltrate the alveoli and enter cell tissues or the circulatory system (Valavanidis et al. 2008). Ultrafine suspended particles can also cause inflammation when deposited on the alveolar epithelial tissues (Laumbach and Kipen 2012) and cause cardiovascular diseases. Previous studies used 24 h ambulatory blood pressure monitors to assess the correlation between the concentrations of ultrafine suspended particles in the atmospheric environment and blood pressure; these concluded that every 10,000 particles/cm3 increase in ultrafine suspended particles led to a significant increase of diastolic blood pressure by 2.7 mmHg (Soldevila et al. 2020). Moreover, exposure to ultrafine aerosols could cause nonfatal myocardial infarction disease (Chen et al. 2020).
Furthermore, instantaneous maximum concentration of suspended particles measured during the electric burning process can exceed the maximum detection limit of the handheld nanoparticle monitor (4 × 107 ultrafine particles/cm3). This indicates surgeons and medical staff around the electric burning area may be exposed to extremely high concentrations of suspended particles in a short period of time. Therefore, it is necessary to choose an appropriate local suction system to remove the surgical smoke generated during surgery and maintain adequate ventilation in the ORs. Previous studies have pointed out that local smoke extraction systems and medical surgical masks have limited effectiveness in removing VOCs from surgical smoke (Kocher et al. 2019; Lee et al. 2018). Liu et al. (2020) indicated that a local smoke exhaust system can effectively reduce the concentration of ultrafine suspended particles (0.02–1 μm) in surgical smoke concentration. Moreover, wearing a surgical mask during surgery can effectively filter PM2.5 particles (Shakya et al. 2017). Surgical masks have a filtration efficiency between 70 and 83% for particle sizes equal to and larger than 0.1 μm, whereas N95 masks can reach a 99% filtration efficiency (Davidson et al. 2013). The heating, ventilation and air conditioning system affected the air quality, temperature, humidity, and comfort level, as well as the distribution and elimination of surgical smoke in ORs (D'Alicandro et al. 2021). The distribution of surgical smoke in ORs was affected by the wind speed, airflow path, and concentration of the surgical area. The removal efficiency of surgical smoke was related to the number of exhaust vents and the distance between the operating table and exhaust vents in ORs (D'Alicandro and Mauro 2022). In terms of the feasibility of current clinical practice, using a local smoking extraction system close to the surgical wound and paying attention to the operation and function of the ventilation system in ORs will be important actions to protect the health and safety of the OR personnel.
To the best of our knowledge, few studies have evaluated the long-term health effects of exposure to suspended particles and VOCs in surgical smoke generated from electrical burning of different human tissues (Limchantra et al. 2019). To protect the health of medical staff and patients in ORs, it is important to maintain good air quality. Due to the difficulty of ultrafine aerosols sampling during the operation, some studies had used the numerical models of fluid dynamics to evaluate the pathway, settling, and removal of ultrafine aerosols in the ORs (Romano et al. 2015). The concentrations of ultrafine aerosols in ORs measured by the numerical models were in good agreements with those measured by actual experiments (D'Alicandro and Mauro 2022; Massarotti et al. 2021; Mohamed et al. 2020). This study had several limitations. First, the human tissue samples that were collected were not large enough to evaluate the difference in VOC concentration in surgical smoke under different electrocautery conditions. Second, the sampling time of surgical smoke was short to avoid interference with surgeries; therefore, it may not directly reflect the exposure of the medical staff to VOCs in ORs. Third, this study used pig skin and pork tissues to evaluate the concentration change of suspended particles in surgical smoke samples. These results may vary from the actual electrical burning of human skin and muscle tissues. Lastly, the aging process of suspended particles such as growth, shrink, coagulation, and falling down could appear during the sampling period.
Conclusion
In head and neck surgery, the concentration of total VOCs produced when the radix linguae tissues were electrocauterized was the highest, followed by their concentration when the craniofacial subcutaneous tissues were electrocauterized. The concentration of methanol was the highest in human surgical smoke samples. The number and mass concentrations of the suspended particles in surgical smoke produced by electrocauterization varied with different pig tissues. Ultrafine aerosols were primarily present in the surgical smoke generated from electrically burned pig skin and pork tissues.
Data availability
All data generated or analyzed during this study are included in this published article.
References
Baggish MS, Elbakry M (1987) The effects of laser smoke on the lungs of rats. Am J Obstet Gynecol 156:1260–1265. https://doi.org/10.1016/0002-9378(87)90158-x
Brüske-Hohlfeld I, Preissler G, Jauch KW et al (2008) Surgical smoke and ultrafine particles. J Occup Med Toxicol 3:31. https://doi.org/10.1186/1745-6673-3-31
Chen K, Schneider A, Cyrys J et al (2020) Hourly exposure to ultrafine particle metrics and the onset of myocardial infarction in augsburg Germany. Environ Health Perspect 128:17003. https://doi.org/10.1289/EHP5478
Cheng MH, Chiu CH, Chen CT, Chou HH, Pao LH, Wan GH (2021) Sources and components of volatile organic compounds in breast surgery operating rooms. Ecotoxicol Environ Saf 209:111855. https://doi.org/10.1016/j.ecoenv.2020.111855
Choi SH, Kwon TG, Chung SK, Kim TH (2014) Surgical smoke may be a biohazard to surgeons performing laparoscopic surgery. Surg Endosc 28:2374–2380. https://doi.org/10.1007/s00464-014-3472-3
D’Alicandro AC, Massarotti N, Mauro A (2021) Aerosol hazards in operating rooms: a review of numerical and experimental studies. J Aerosol Sci 158:105823. https://doi.org/10.1016/j.jaerosci.2021.105823
D’Alicandro AC, Mauro A (2022) Effects of operating room layout and ventilation system on ultrafine particle transport and deposition. Atmos Environ 270:118901. https://doi.org/10.1016/j.atmosenv.2021.118901
Davidson CS, Green CF, Gibbs SG et al (2013) Performance evaluation of selected n95 respirators and surgical masks when challenged with aerosolized endospores and inert particles. J Occup Environ Hyg 10:461–467. https://doi.org/10.1080/15459624.2013.818243
Environmental Analytical Laboratory (EAL) (2014) Environmental Protection Administration, Taiwan. Analytical method for determining volatile organic compound in air-stainless steel canister/gas chromatography-mass spectrometry (NIEA A715.15B). Available from: https://www.rootlaw.com.tw/LawArticle.aspx?LawID=A040300081066800-1100105. Accessed 20 Oct 2021 (In Chinese)
Eshleman EJ, LeBlanc M, Rokoff LB et al (2017) Occupational exposures and determinants of ultrafine particle concentrations during laser hair removal procedures. Environ Health 16:30. https://doi.org/10.1186/s12940-017-0239-z
Freitag L, Chapman GA, Sielczak M, Ahmed A, Russin D (1987) Laser smoke effect on the bronchial system. Lasers Surg Med 7:283–288
Harder V, Gilmour P, Lentner B et al (2005) Cardiovascular responses in unrestrained WKY rats to inhaled ultrafine carbon particles. Inhal Toxicol 17:29–42. https://doi.org/10.1080/08958370590885681
International Agency for Research on Cancer (IARC) (2022) Agents classified by the IARC monographs 1–131. Available from: https://monographs.iarc.who.int/agents-classified-by-the-iarc/. Accessed 1 May 2022
International Organization for Standardization (ISO) (2015) Cleanrooms and associated controlled environments. Part 1: classification of air cleanliness by particle concentration; ISO standard 14644–1:1999. International Organization for Standardization: Geneva, Switzerland. Available from: https://zoser.com.co/wp-content/uploads/2015/10/ISO%2014644-1%20Version%202015.pdf. Accessed 5 Nov 2021
Jiménez E, Linares C, Rodríguez LF, Bleda MJ, Díaz J (2009) Short-term impact of particulate matter (PM2.5) on daily mortality among the over-75 age group in Madrid (Spain). Sci Total Environ 407:5486–5492. https://doi.org/10.1016/j.scitotenv.2009.06.038
Karjalainen M, Kontunen A, Saari S et al (2018) The characterization of surgical smoke from various tissues and its implications for occupational safety. PLoS One 13:e0195274. https://doi.org/10.1371/journal.pone.0195274
Kocher GJ, Sesia SB, Lopez-Hilfiker F, Schmid RA (2019) Surgical smoke: still an underestimated health hazard in the operating theatre. Eur J Cardiothorac Surg 55:626–631. https://doi.org/10.1093/ejcts/ezy356
Kocher GJ, Koss AR, Groessl M, Schefold JC, Luedi MM, Quapp C et al (2022) Electrocautery smoke exposure and efficacy of smoke evacuation systems in minimally invasive and open surgery: a prospective randomized study. Sci Rep 12:4941. https://doi.org/10.1038/s41598-022-08970-y
Kwon HS, Ryu MH, Carlsten C (2020) Ultrafine particles: unique physicochemical properties relevant to health and disease. Exp Mol Med 52:318–328. https://doi.org/10.1038/s12276-020-0405-1
Laumbach RJ, Kipen HM (2012) Respiratory health effects of air pollution: update on biomass smoke and traffic pollution. J Allergy Clin Immunol 129:3–11; quiz 12–13. https://doi.org/10.1016/j.jaci.2011.11.021
LeBouf RF, Stefaniak AB, Virji MA (2012) Validation of evacuated canisters for sampling volatile organic compounds in healthcare settings. J Environ Monit 14:977–983. https://doi.org/10.1039/c2em10896h
Lee T, Soo JC, LeBouf RF et al (2018) Surgical smoke control with local exhaust ventilation: Experimental study. J Occup Environ Hyg 15:341–350. https://doi.org/10.1080/15459624.2017.1422082
Li CI, Chou YH, Pai JY, Chen CH, Chiang MC (2022) Investigating surgical smoke in otolaryngology operating rooms. Sci Rep 12:1719. https://doi.org/10.1038/s41598-022-05701-1
Li N, Chen G, Liu F et al (2019) Associations of long-term exposure to ambient PM(1) with hypertension and blood pressure in rural Chinese population: the Henan rural cohort study. Environ Int 128:95–102. https://doi.org/10.1016/j.envint.2019.04.037
Limchantra IV, Fong Y, Melstrom KA (2019) Surgical smoke exposure in operating room personnel: a review. JAMA Surg 154:960–967. https://doi.org/10.1001/jamasurg.2019.2515
Liu N, Filipp N, Wood KB (2020) The utility of local smoke evacuation in reducing surgical smoke exposure in spine surgery: a prospective self-controlled study. Spine J 20:166–173. https://doi.org/10.1016/j.spinee.2019.09.014
Massarotti N, Mauro A, Mohamed S, Romano MR (2021) Air contamination inside an actual operating room due to ultrafine particles: an experimental-numerical thermo-fluid dynamic study. Atmos Environ 249:118155. https://doi.org/10.1016/j.atmosenv.2020.118155
Massarweh NN, Cosgriff N, Slakey DP (2006) Electrosurgery: history, principles, and current and future uses. J Am Coll Surg 202:520–530. https://doi.org/10.1016/j.jamcollsurg.2005.11.017
Melnick RL, Huff J, Chou BJ, Miller RA (1990) Carcinogenicity of 1,3-butadiene in C57BL/6 x C3H F1 mice at low exposure concentrations. Cancer Res 50:6592–6599
Miller KA, Siscovick DS, Sheppard L et al (2007) Long-term exposure to air pollution and incidence of cardiovascular events in women. N Engl J Med 356:447–458. https://doi.org/10.1056/NEJMoa054409
Mohamed S, Buonanno G, Massarotti N, Mauro A (2020) Ultrafine particle transport inside an operating room equipped with turbulent diffusers. J Build Perform Simul 13:443–455. https://doi.org/10.1080/19401493.2020.1766567
Moreno R, Tejeda Benítez L, Bustillo LC (2021) Sources, characteristics, toxicity, and control of ultrafine particles: an overview. Geosci Front 13:101147. https://doi.org/10.1016/j.gsf.2021.101147
Occupational Safety and Health Administration (OSHA) (2021) Methyl alcohol (Methanol). Available from: http://www.osha.gov/chemicaldata/chemResult.html?RecNo=474. Accessed 5 Nov 2021
Pietropaoli AP, Frampton MW, Hyde RW et al (2004) Pulmonary function, diffusing capacity, and inflammation in healthy and asthmatic subjects exposed to ultrafine particles. Inhal Toxicol 16(Suppl 1):59–72. https://doi.org/10.1080/08958370490443079
Pinkerton KE, Green FH, Saiki C et al (2000) Distribution of particulate matter and tissue remodeling in the human lung. Environ Health Perspect 108:1063–1069. https://doi.org/10.1289/ehp.001081063
Radike MJ, Stemmer KL, Bingham E (1981) Effect of ethanol on vinyl chloride carcinogenesis. Environ Health Perspect 41:59–62. https://doi.org/10.1289/ehp.814159
Ragde SF, Jørgensen RB, Føreland S (2016) Characterisation of Exposure to ultrafine particles from surgical smoke by use of a fast mobility particle sizer. Ann Occup Hyg 60:860–874. https://doi.org/10.1093/annhyg/mew033
Romano F, Marocco L, Gustén J, Joppolo CM (2015) Numerical and experimental analysis of airborne particles control in an operating theater. Build Environ 89:369–379. https://doi.org/10.1016/j.buildenv.2015.03.003
Samet JM, DeMarini DM, Malling HV (2004) Biomedicine. Do airborne particles induce heritable mutations? Science 304:71–972. https://doi.org/10.1126/science.1097441
Schulz H, Harder V, Ibald-Mulli A et al (2005) Cardiovascular effects of fine and ultrafine particles. J Aerosol Med 18:1–22. https://doi.org/10.1089/jam.2005.18.1
Shakya KM, Noyes A, Kallin R, Peltier RE (2017) Evaluating the efficacy of cloth facemasks in reducing particulate matter exposure. J Expo Sci Environ Epidemiol 27:352–357. https://doi.org/10.1038/jes.2016.42
Soldevila N, Vinyoles E, Tobias A et al (2020) How do ultrafine particles in urban air affect ambulatory blood pressure? J Hypertens 38:845–849. https://doi.org/10.1097/HJH.0000000000002343
Takahashi H, Yamasaki M, Hirota M et al (2013) Automatic smoke evacuation in laparoscopic surgery: a simplified method for objective evaluation. Surg Endosc 27:2980–2987. https://doi.org/10.1007/s00464-013-2821-y
U.S. Coast Guard (1999) Chemical hazard response information system (CHRIS)-hazardous chemical data. Commandant Instruction 16465.12C. Washington, D.C.: U.S. Government Printing Office. Available from: https://hero.epa.gov/hero/index.cfm/reference/details/reference_id/5208492. Accessed 5 Nov 2021
Ulmer BC (2008) The hazards of surgical smoke. AORN J 87:721–734;quiz 735–8. https://doi.org/10.1016/j.aorn.2007.10.012
Valavanidis A, Fiotakis K, Vlachogianni T (2008) Airborne particulate matter and human health: toxicological assessment and importance of size and composition of particles for oxidative damage and carcinogenic mechanisms. J Environ Sci Health C Environ Carcinog Ecotoxicol Rev 26:339–362. https://doi.org/10.1080/10590500802494538
Wenig BL, Stenson KM, Wenig BM, Tracey D (1993) Effects of plume produced by the Nd:YAG laser and electrocautery on the respiratory system. Lasers Surg Med 13:242–245. https://doi.org/10.1002/lsm.1900130213
Wong O (1987) An industry wide mortality study of chemical workers occupationally exposed to benzene. II. Dose response analyses. Br J Ind Med 44:382–395. https://doi.org/10.1136/oem.44.6.382
Zhang JY, Wu QJ, Huang YH et al (2020) Association between maternal exposure to ambient PM(10) and neural tube defects: a case-control study in Liaoning Province. China Int J Hyg Environ Health 225:113453. https://doi.org/10.1016/j.ijheh.2020.113453
Acknowledgements
The authors thank Mrs. Chi Wang for her assistance on administration affairs of the operating rooms and Ms. Pei-Chen Yang and Ms. Pei-Hung Chen for their technical assistances in this study.
Funding
The authors received financial support from the Ministry of Science and Technology and Chang Gung Medical Foundation, Taiwan, under grants MOST107-2314-B-182–054, MOST108-2813-C-182–033-B, and BMRP441.
Author information
Authors and Affiliations
Contributions
CTC: investigation, formal analysis, writing original draft. SFH: investigation, formal analysis, writing review. CJL: investigation, formal analysis. JMH: investigation, funding acquisition. KPC: investigation. GHW: conceptualization, methodology, investigation, writing original draft, writing review & editing, project administration, funding acquisition.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All authors consent to the publication of this study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, CT., Huang, SF., Li, CJ. et al. Distribution of ultrafine aerosols and volatile organic compounds from surgical smoke during electrocauterization. Air Qual Atmos Health 15, 2009–2020 (2022). https://doi.org/10.1007/s11869-022-01233-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11869-022-01233-9