Abstract
Desertification and climate warming trends pose a global ecological and environmental problem. The city of Be'er Sheva (Southern Israel) is located at the margins of the Sahara-Arabian dust belt and is frequently subjected to dust storm (DS) with high levels of particular matter (PM), making it an ideal location for investigating the health effects. The objective of this study was to investigate the impact of DS on patients with chronic obstructive pulmonary disease (COPD) in an arid urban environment. We obtained health data of patients 18 years or older discharged from Soroka University Medical Center (SUMC) with a primary diagnosis consistent with COPD exacerbation. Data on meteorological parameters and air pollutants were obtained from two monitoring stations in the city of Be'er Sheva. Time series analysis was performed to assess the COPD exacerbation incidence rate ratio (IRR) resulting from dust storm exposures. We found that daily PM10 concentrations were extremely high during dust storm days, and there is a positive association between dust storms and rate of hospitalization for COPD exacerbation: (IRR = 1.16; 95 %CI, 1.08–1.24; p < 0.001). In addition, an increase per interquartile range in PM10 concentrations increases the IRR by 1.03 (95 %CI, 1.01–1.06; p < 0.001). The effect increased with age and was higher in women. Short-term exposure to natural PM10 during dust storms increases the risk for hospital admission for COPD exacerbation. Further studies are needed to understand the impact of individual characteristics on the health effects of outdoor and indoor PM pollution from dust storms.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
The adverse impact of particulate matter (PM) on human health has been documented. Recently, special attention has been given to air pollution originating from mineral dust particles, which may cause a health effect (Karanasiou et al. 2012). Natural soils in arid and semiarid zones are source areas for air pollution through emissions of PM to the atmosphere during dust storms. The dust may contain organic matter or toxic chemicals which may be a serious health threat (Wilson and Suh 1997). Although the association between PM exposure and respiratory morbidity exists (Schwartz 1996; Brunekreef and Forsberg 2005; Donaldson et al. 1998; Annesi-Maesano et al. 2007; Atkinson et al. 2001), our understanding of the impact of chronic and acute exposure to PM originating from dust storms on patients with preexisting respiratory morbidity is limited.
Several studies investigated the role of coarse particles (between 2.5 and 10 μm in diameter) from desert dust on health (Sandstrom and Forsberg 2008). A study by Perez et al. (2008) showed that an increase of 10 μg/m3 of PM10-2.5 during Sahara originated dust storms was associated with an increase in all-cause daily mortality of 8.4 %. In Italy, Sajani and colleagues evidenced that there was an increased respiratory mortality for people aged 75 or older on Sahara dust days and that respiratory mortality increased by 22.0 % (95 %CI, 4.0–43.1 %) on dust days (Zauli Sajani et al. 2011). A 10-year analysis of respiratory and cardiovascular morbidity in Nicosia, Cyprus (Nicos et al. 2008) showed that all-cause and cardiovascular admissions were 4.8 % (95 %CI, 0.7–9.0 %) and 10.4 % (95 %CI, −4.7 to 27.9 %) higher during dust storm days, respectively. However, the majority of these studies were performed in non-arid urban environments.
Desertification and global warming trends pose significant global ecological and environmental problems (Schwartz et al. 2006), e.g., land degradation processes resulting in increasing exposure of population to dust sources in arid and semiarid soils and possible dust storms (Mulitza et al. 2010). The Negev region is located between the Saharan and the Arabian deserts (the world's largest dust belt), and every year, it is exposed to several intensive dust storms (Ganor et al. 2010; Krasnov et al. 2014). The area is inhabited by two main ethnic groups: predominantly urban Jews (69 %) and rural Bedouin Arabs (31 %).
In the current study, we sought to assess the impact of acute exposure to PM10 dust particles on the frequency of chronic obstructive pulmonary disease (COPD) exacerbations requiring hospital admission.
Methods
Health data
We obtained health data of patients 18 years or older discharged from Soroka University Medical Center (SUMC) with a primary diagnosis consistent with chronic obstructive pulmonary disease exacerbation (ICD-9 codes: 490, 491, 492, 496) during the period 2001–2010. SUMC is the only medical center in this area serving a population of approximately 700,000 as the only primary hospital in Northern Negev and nearly one million as a tertiary hospital. The following comorbidities were assessed: diabetes (ICD-9: 231, 225) and congestive heart failure (ICD-9: 428). The study was approved by the institutional review board of Soroka University Medical Center.
Environmental data
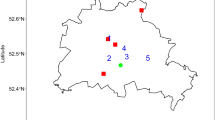
Data on meteorological parameters and air pollutants were obtained from two monitoring stations in the city of Be'er Sheva. Seasons were defined according to Alpert et al. (2004): winter (December 7–March 30), summer (May 31–September 22) each lasting about 4 months (3 months and 23 days), autumn (September 23–December 6), and spring (March 31–May 30) each lasting only 2 months (75 and 61 days, respectively).
Dust storm definition
Most of the dust storms in the Negev region originate from the Sahara desert. We define a dust storm (DS) day as a day with an averaged PM10 concentration that is 2 standard deviations above the background value (Krasnov et al. 2014). The background value which was calculated on the basis of the average PM10 concentration for 12 h (from 6 a.m. to 6 p.m.) during the summer season (dust-free period) reflects the background level including anthropogenic particles, i.e., caused or produced by humans (Ganor et al. 2010). We define days with mild dust storms as a day with PM10 level between 71 and 200 μg/m3 and days with intensive dust storm with a PM10 level above 200 μg/m3.
Statistical analysis
We performed multivariate statistical analysis by using generalized additive Poisson regression model. The models provide estimates of incidence relative risk (IRR)-characterized effect of dust storm exposure on the hospital admission number for COPD exacerbation. We had two models, controlling for seasonal and meteorological factors: in one where exposure was expressed as daily mean PM10 concentration and another where exposure was expressed as a dust storm indicator variable. For both models, we tested lag effect.
The model was defined as follows:
where Y is the daily count of admissions. Linear terms in the models include M for vector of meteorological variables (maximum temperature, difference in daily temperatures and maximum relative humidity), DS is an indicator of the dust storm day, and P is a vector of pollutants (PM10, NO2, NO, CO, and O3). In addition, the model included interaction terms to examine an interaction between the pollutants (P × P) and terms P × M are used to investigate a possible effect modification by temperature and relative humidity.
To adjust for seasonality and other temporal effects, we used nonlinear terms with penalized splines for time with 5 degrees of freedom per year and 5 degrees of freedom for maximum temperature.
Analyses were performed using the MGCV package in the R software (R2.2.0) and SPSS (version 18).
Results
Patient population
The study population consists of 2,147 patients that experienced 7,582 admissions with primary diagnosis of acute exacerbation of COPD. As expected, the median number of daily admissions with COPD exacerbation was higher during the winter season (median of 3 per day), compared to autumn and spring (median of 2 per day) and summer season with 1 admission a day.
Table 1 shows the study population characteristics. The average age was 69.5 years and 60.7 % were male. Frequent comorbidities included diabetes mellitus (486 patients, 22.6 %) and congestive heart failure (115 patients, 5.4 %). Median length of the hospitalization for COPD was 3 days (IQ range 2–5), and 1.8 % died in hospital. During the study period, 16.5 % of the patients were admitted twice, and 18.4 % were admitted more than three times.
Pollutant exposures
The duration of the pollutant and meteorological data series was 3,652 days (10 years). Out of 3,652 days, the missing measurements rates varied by pollutant: 115 (3.1 %) for PM10, 78 (2.1 %) for NO2, 79(2.2 %) for NO, 59 (1.6 %) for CO, 77(2.1 %) for SO2, and 97 (2.7 %) for O3. Daily average concentrations of PM10, CO, NO, NO2, SO2, and O3, as well as daily meteorological factors during 2001–2010 in Be'er Sheva, are presented in Table 2. Overall, during 955 days (26.15 %) of the study period, the PM10 levels exceeded the WHO-recommended daily guideline of 50 μg/m3 (World Health Organization 2006). During the summer period, the average 12-h concentration of PM10 was 42 ± 14.5 μg/m3. Therefore, the resulting threshold value for a dust day was 71 μg/m3.
Following this definition, we have identified 445 dust storm days (12.2 %) during the study period based on our calculated value (71 μg/m3) with the majority occurring during the winter and spring seasons (from December to May). Daily average of PM10 levels during 2001–2010 in Be'er Sheva is presented in Fig. 1. Three hundred and forty-five days (9.44 %) was defined as days with mild dust storms (<200 μg m3), and 99 days (2.7 %) was defined as days with intensive dust storm (>200 μg m3). Values of PM10 during the DS days reached the average and maximum levels of 157.5 ± 138.2 and 4,797 μg/m3, respectively, and were higher than those observed during the “non-dust storm” days (38.4 ± 29.7 μg/m3). The average temperature was 13.6 ± 3.4 °C in the winter and 25.8 ± 1.8 °C in the summer, reaching a maximal temperature of 31.9 ± 2.7 °C in August. In addition, the warm seasons, summer and spring, were characterized by a high difference between the minimum and maximum temperature (differences in daily temperature, 10.8 ± 2.4 °C in summer and 11.7 ± 3.8 °C in spring).
Effect of PM10 and dust storm days on the incidence of acute COPD exacerbations
We found a positive association between the incidence of hospitalizations with COPD exacerbation and PM10 levels measured during the same day (Fig. 2). Multivariate model adjusted for meteorological factors, pollutants, and their interactions demonstrated that an increase in interquartile ranges of PM10 (micrograms per meter) was associated with an IRR of 1.03 (95 %CI, 1.01–1.010; p < 0.001). We tested a possible lag effect up to 3 days following the exposure: the association remained significant for 1-day lag only: IRR = 1.004 (95 %CI, 1.01–1.06; p = 0.001), but not for 2- or 3-day lags: IRR = 0.996 (95 %CI, 0.991–1.008; p = 0.357) and IRR = 0.997 (95 %CI, 0.991–1.008; p = 0.504), respectively.
We found a positive association between DS and incidence of hospitalization for COPD exacerbation (IRR = 1.16; 95 %CI, 1.08–1.24; p < 0.001, Table 3). In addition, incidence relative risk (IRR) for COPD exacerbations during the mild dust storms days was 1.12 (95 %CI, 1.03–1.21) compared to the days without dust storm, and during the intensive dust storms, the IRR was 1.27 (95 %CI, 1.12–1.43; p = 0.001) compared to the days without dust storm. The examination of the interaction between PM10 exposure and presence of the dust storm showed similarity of the dust effects during the storm days compared to the non-storm days. In the non-dust storm days, an increase per interquartile range in PM10 concentrations results in an IRR of 1.018 (95 %CI, 0.99–1.04; p = 0.06); during the dust storm days, the IRR was 1.017 (95 %CI, 1.01–1.03; p < 0.001). Mean daily temperature did not affect the hospitalization incidence. However, days with a higher daily variation in temperature, as seen during the summer and spring, were associated with an increase in admission rates (IRR = 1.014 (95 %CI, 1.02–1.026; p = 0.022). As for the other pollutants, we found that an interaction between 10 units of SO2 (parts per billion) and CO (parts per million) and between 10 units of O3 (parts per billion) and maximum temperature was associated with an increased number of COPD admissions by IRR = 1.001 (95 %CI, 1.000–1.002; p = 0.001) and by IRR = 1.005 (95 %CI, 1.002–1.008; p = 0.001), respectively.
Age and gender were effect modifiers for the association between the dust storms DS and rate of COPD exacerbation hospitalizations (Table 4). The IRR adjusted for seasonality, meteorological factors, and pollutants increased from 1.110 (95 %CI, 1.008–1.222; p = 0.032) in patients 50 to 70 years old to 1.167 (95 %CI, 1.059–1.285; p = 0.002) in patients older than 70 years. Among female patients, the rate of COPD exacerbation hospitalizations was 1.278 (95 %CI, 1.148–1.427; p < 0.001) compared to the rate among men, which was 1.053 (95 %CI, 0.963–1.151; p = 0.251).
Discussion
In this population-based study, we aimed to investigate the association between the natural desert dust exposure and respiratory morbidity in an urban area. The main findings revealed that dust storms are mainly responsible for the extremely high levels of daily atmospheric PM10 concentrations detected during dust storm days (up to 4,797 μg/m3). We have found a positive association between DS and incidence of hospitalizations with COPD exacerbation. The degree of the association increased with age and was higher in women. Moreover, we have found an additional, but smaller, effect of the anthropogenic pollution (PM10, O3, CO, and SO2) on the incidence of COPD exacerbation.
The results of our study are consistent with previous reports investigating the health effects of PM pollution. The APHEA-2 study (Atkinson et al. 2001) showed that hospital admissions for asthma and COPD among people older than 65 years increased by 1.0 % (0.4–1.5 %) per 10 μg/m3 PM10. The PM10 levels detected in that study of European cities were significantly lower than those observed in our geographical area, e.g., the maximum level of PM10 reported in Barcelona was 131.7 μg/m3. The National Morbidity, Mortality, and Air Pollution Study (NMMAPS) (Samet et al. 2000) examined the association between hospital admissions for COPD and PM10 in 14 US cities. It reported an increase of 1.98 % (95 %CI, 1.49–2.47 %) in COPD admissions per 10 μg/m3 of PM10 in patients aged above 64 years.
The magnitude of the increase in hospitalization we observed in our study was somewhat lower, IRR of 1.03 (95 %CI, 1.01–1.010; p < 0.001) per interquartile ranges of PM10, than that reported in the aforementioned studies. This may be explained by the fact that we focused on the exposure to a natural phenomenon such as desert-originated DS, rather than particles of anthropogenic origin which can contain potentially toxic components such as elemental and organic carbon, metals, sulfate, etc. Even though the effect of the estimated rate of hospitalization was rather low, the overall risk of hospitalization is extremely high because of the high concentration of PM10 during the dust storm events, especially during the intensive ones, compared to the concentration of the particles related to the anthropogenic sources. We have observed a dose response of the effect, with a higher risk for hospitalization during the intensive dust storms, with a PM10 level above 200 μg m3, compared to the days with mild dust storms. Most of the intensive dust storms during the study period (2001–2010) occur in the winter season. The winter storms are associated mainly with the passage of western cold front in this region (i.e., the Cyprus Low) followed by relatively high wind speeds (>6 m/s). However, mild storms occur also in the spring and autumn seasons due to Sharav Low and Red Sea Trough systems with relatively low wind speeds (Krasnov et al. 2014).
Only few studies have investigated the effect of PM from natural sources on health outcomes. In a study conducted in Cyprus (Nicos et al. 2008), the authors used a time series approach to investigate the association between daily levels of PM10 on the number hospital admissions for all respiratory and cardiovascular causes. Short-term PM10 exposures increased the risk of same-day, all-cause, and cardiovascular, but not for respiratory, hospitalizations. The authors suggested that there might be a misclassification of admission diagnosis, particularly in people with both respiratory and cardiovascular diagnosis. A study by Perez et al. (2008) examined the impact of DS on daily mortality in Barcelona showing an 8.4 % increase per 10 μg/m3 increase in coarse particles (PM10-2.5) during days with Sahara DS compared to1.4 % during non-Saharan dust days. In a study from Taiwan (Chen et al. 2004), the authors found that DS increased the risk for respiratory death by 7.66 % 1 day after the storm. A case-crossover study from Hong Kong (Tam et al. 2012) examined the effects of DS on emergency hospital admissions due to the respiratory diseases. That study showed a significant increase in emergency hospital admission due to COPD 2 days after DS. The relative risk for 2-day lag was 1.05 (95 %CI, 1.01–1.09) per 10 mg/m3 of PM10.
In contrast, Schwartz et al. (1999) did not find a significant effect of DS on mortality in a study conducted in Spokane, Washington. The study investigated a dry period subjected to the occasional DSs after [crops] harvest. No increase in all-cause mortality was observed during the DS days (average PM10 concentration of 263 μg/m3) compared to control days (average PM10 concentration of 42 μg/m3).
In a laboratory study (Kim and Hu 1998) of young healthy adults, it was shown that women had a 11–23 % higher deposition of inhaled particle in the central airways compared to men. This gender difference was in particular true for coarser particles (>5 μm) and assumed to be associated with women having narrower airways than men. Patients with COPD suffer from debilitating shortness of breath which is caused by expiratory flow limitation induced by dynamic hyperinflation; in order to overcome shortness of breath, patients change their breathing pattern to a larger volume at a slower pace to allow for a complete expiration, thus reducing hyperinflation and the work of breathing. When COPD patients are exposed to environmental PM, the deposition is different and uneven from that seen in persons with normal lung functions, resulting in higher concentrations of PM in the central airways. The higher concentration of PM in the central airways induces a more intense irritation and inflammation which will induce an acute exacerbation of COPD (Seaton et al. 1995).
One of the strengths of our investigation is the long study period allowing for the robust analysis of both exposure and health outcomes. The fact that Be'er Sheva is located in the margins of the dust belt provides ideal conditions for analyzing the effect of DS on health outcomes. Furthermore, the unique combination of a centralized modern medical system and urban population residing in this arid region makes Negev an ideal “environmental lab” for studying the health effect of global environmental change. Our data provide an insight into the possible health effect of the desertification defined as “land degradation in arid, semiarid, and dry subhumid areas, resulting from various factors, including climatic changes and human activity” (United Nations Environment Programme 1994).
Our study has several limitations. We used outdoor air pollution concentrations measured at fixed point monitors (ambient PM concentrations), whereas people spend most of the time indoors, especially patients with respiratory problems. Secondly, the role of chemical toxicity in PM is poorly understood, especially as it relates to particle exposures to arid versus non-arid areas, together with the ability of the Sahara dust particles to serve as carriers of anthropogenic pollutants and microorganisms as they pass from Africa to Middle East and Europe. Finally, COPD exacerbation diagnosis was based on the discharge note; therefore, we cannot rule out the misclassification.
Conclusions
Dust storms are a major cause of PM episodes in our geographical areas adjacent to the deserts. During dust storms, short-term exposure to PM10 and gaseous co-pollutants increases the risk for hospital admission due to the acute exacerbation of COPD. Further studies are needed to understand the impact of the individual level factors of the effects of PM and DS air pollution on respiratory morbidity.
References
Alpert P, Osetinsky I, Ziv B, Shafir H (2004) A new seasons definition based on classified daily synoptic systems: an example for the eastern Mediterranean. Int J Climatol 24(8):1013–1021
Annesi-Maesano I, Forastiere F, Kunzli N et al (2007) Particulate matter, science and EU policy. Eur Respir J 29(3):428–431
Atkinson RW, Anderson HR, Sunyer J et al (2001) Acute effects of particulate air pollution on respiratory admissions: results from APHEA 2 project. Air Pollution and Health: a European Approach. Am J Respir Crit Care Med 164(10 Pt 1):1860–1866
Brunekreef B, Forsberg B (2005) Epidemiological evidence of effects of coarse airborne particles on health. Eur Respir J 26(2):309–318
Chen YS, Sheen PC, Chen ER et al (2004) Effects of Asian dust storm events on daily mortality in Taipei, Taiwan. Environ Res 95(2):151–155
Donaldson K, Li X, MacNee W (1998) Ultrafine (nanometre) particle mediated lung injury. J Aerosol Sci 29(5–6):553–560
Ganor E, Stupp A, Osetinsky I, Alpert P (2010) Synoptic classification of lower troposphere profiles for dust days. J Geophys Res 115(D11), D11201
Karanasiou A, Moreno N, Moreno T et al (2012) Health effects from Sahara dust episodes in Europe: literature review and research gaps. Environ Int 47:107–114
Kim CS, Hu SC (1998) Regional deposition of inhaled particles in human lungs: comparison between men and women. J Appl Physiol 84(6):1834–1844
Krasnov H, Katra I, Koutrakis P, Friger M (2014) Contribution of dust storms to PM10 levels in an urban arid environment. J Air Waste Manage Assoc 64:89–943
Mulitza S, Heslop D, Pittauerova D et al (2010) Increase in African dust flux at the onset of commercial agriculture in the Sahel region. Nature 466(7303):226–228
Nicos M, Panayiotis Y, Savvas K et al (2008) A 10-year time-series analysis of respiratory and cardiovascular morbidity in Nicosia, Cyprus: the effect of short-term changes in air pollution and dust storms. Environ Health Glob Access Science Source 7:39
Perez L, Tobias A, Querol X et al (2008) Coarse particles from Saharan dust and daily mortality. Epidemiology 6:800–807
Samet JM, Zeger SL, Dominici F et al (2000) The National Morbidity, Mortality, and Air Pollution Study. Part II: morbidity and mortality from air pollution in the United States. Res Rep Health Eff Inst 94(Pt 2):5–70, discussion 71-9
Sandstrom T, Forsberg B (2008) Desert dust: an unrecognized source of dangerous air pollution? Epidemiology 19(6):808–809
Schwartz J (1996) Air pollution and hospital admissions for respiratory disease. Epidemiology 7(1):20–28
Schwartz J, Norris G, Larson T et al (1999) Episodes of high coarse particle concentrations are not associated with increased mortality. Environ Health Perspect 107(5):339–342
Schwartz BS, Parker C, Glass TA, Hu H (2006) Global environmental change: what can health care providers and the environmental health community do about it now? Environ Health Perspect 114(12):1807–1812
Seaton A, MacNee W, Donaldson K, Godden D (1995) Particulate air pollution and acute health effects. Lancet 345(8943):176–178
Tam WW, Wong TW, Wong AH, Hui DS (2012) Effect of dust storm events on daily emergency admissions for respiratory diseases. Respirology 17(1):143–148
United Nations Environment Programme (1994) Agenda 21. Managing Fragile Ecosystems: Sustainable Mountain Development. Retrieved January 06, 2013, from http://www.unep.org.
Wilson WE, Suh HH (1997) Fine particles and coarse particles: concentration relationships relevant to epidemiologic studies. J Air Waste Manag Assoc 47(12):1238–1249
World Health Organization (2006) WHO air quality guidelines for particulate matter, ozone, nitrogen dioxide and sulfur dioxide. Global update summary of risk assessment. WHO, Geneva
Zauli Sajani S, Miglio R, Bonasoni P et al (2011) Saharan dust and daily mortality in Emilia-Romagna (Italy). Occup Environ Med 68(6):446–451
Acknowledgments
This work was supported by the Israeli Environmental Health Fund (EHF) Grant # RGA 1004. The authors would like to thank Mr. Hilel Vardi for providing programming support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vodonos, A., Friger, M., Katra, I. et al. The impact of desert dust exposures on hospitalizations due to exacerbation of chronic obstructive pulmonary disease. Air Qual Atmos Health 7, 433–439 (2014). https://doi.org/10.1007/s11869-014-0253-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11869-014-0253-z