Abstract
Background
Limited evidence has examined the association between balance and mobility measures with risk of fall.
Aim
To determine the prevalence and balance measures associated with falls and fear of falling among community adults aged 50 years and older.
Methods
This cross-sectional study included community-dwelling adults aged ≥ 50 years, living in Saudi Arabia. The participants were asked to report any history of falls in the past 12 months and fear of falling using the Falls Efficacy Scale (FES-I). Balance/mobility measures included the Timed Up and Go (TUG) test, Functional Reach Test (FRT), 10-m walk test (10-MWT), 6-min walk test (6-MWT), and Five Times Sit-to-Stand Test (5XSST).
Results
Two hundred and six participants, including 96 women, were included. The prevalence of falls was 12.6%, and the 5XSST was the only balance measure significantly associated with falls (OR 1.17, 95% CI [1.03, 1.33], p = 0.019) with a cutoff score of 13.93 s or more, a sensitivity of 0.73, and a specificity of 0.58. An increase in 5XSST time was associated with an increase in FES-I score, while a decrease in other balance measures (10-MWT, TUG, FRT, and 6-MWT) was associated with an increase in FES-I scores.
Conclusion
Adults living in Saudi Arabia had a low prevalence of falls. The 5XSST was the only significant balance/mobility measure that distinguished fallers from non-fallers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Falls are a major public health issue faced by older adults [1]. A fall is defined as “an event that causes a person to come to rest accidentally on the ground, floor, or at a lower level” [2]. Falls have been linked to increased morbidity, decreased functionality, reduced quality of life, and early admissions to nursing homes and hospitals [2,3,4,5]. Approximately one-third of people aged 65 years and older experience at least one fall annually [6]. Approximately 20–30% of people who fall acquire injuries that limit their mobility, and as a result, their ability to be independent in the future is hindered [3,4,5]. Fall mortality increases with age in both men and women, irrespective of race and ethnicity, with 70% of unintentional deaths occurring in individuals aged 75 years and older [7]. The most common risk factors for falls among older adults are impaired gait and balance, which can be caused by visual, sensorimotor, or vestibular system problems [8, 9].
Balance has been shown to predict functionality, mobility, and fall risk in patients with different demographic variables and various clinical settings [10, 11]. Deterioration in balance is common with aging and can be caused by illness and injury [12, 13]. It is also a leading cause of falls in older adults [14]. Therefore, balance measures that are sensitive enough to determine early signs of balance control impairment are required to establish prevention strategies for falls among older adults worldwide.
There is limited evidence of the prevalence of falls and fear of falling among the people of Saudi Arabia [15,16,17]. In this population, fear of falling was associated with neither polypharmacy nor number of medications but was associated with the history of falls [16]. No previous study has examined balance and mobility in relation to falls [15,16,17]. Previous research in Saudi Arabia has shown that the prevalence of falls in Gulf Cooperation Council countries is 45% [18]. According to this recent meta-analysis, there is a dearth of evidence on balance measures and their association with falls in older adults in Saudi Arabia. Another limitation is the lack of research on fall risk among adults aged ≥ 50 years. Although this age group might have a relatively low prevalence of falls, falling may indicate decreased functionality and poor balance and mobility measures. Hence, focusing on balance measures and the risk of falls in Saudi Arabia will aid in designing fall prevention programs across the region. Therefore, this study is aimed at determining the prevalence of falls and the associated balance measures using the Falls Efficacy Scale (FES-I) among community-dwelling adults aged 50 years and older. We hypothesized that poor balance measures would be associated with falls and FES-I among this population of older adults in Saudi Arabia.
Methods
Study design and participants
This cross-sectional study was conducted in Saudi Arabia between January 2022 and March 2022. Community-dwelling adults aged ≥ 50 years living in Saudi Arabia were included in the study. People who were non-Saudi, unable to read or write in Arabic, or unable to perform functional tasks safely were excluded from this study. Participants were recruited from regions across Saudi Arabia, including Riyadh, Al-Kharj, Jazan, Jeddah, Arar, Hail, and Tabuk. Licensed and trained physical therapists recruited participants from the community—from mosques, malls, clinics, and other locations. We selected Arabic speakers because of self-reported outcome measures that have been translated and validated in the Arabic language. All the participants were informed of the study goals before signing the consent form and were given the option to voluntarily withdraw from the study at any time. The participants signed informed consent forms before enrollment in the study. This study was approved by the Research Ethics Committee of Prince Sattam bin Abdulaziz University (No. RHPT/021/017).
Fall outcomes
History of falls
The primary outcome measure was history of falls based on an interview in which participants were asked if they had experienced a fall within the past 12 months. We chose the World Health Organization’s definition of a fall, “an unintentional laying down to the ground,” and if the answer was affirmative, we enquired regarding the number of falls [2].
Falls Efficacy Scale
The secondary outcome measure was fear of falling using FES-I. Data collection tools included the Arabic version of the FES-I, which is used for measuring fear or concern about falling [19, 20]. It is a valid and reliable scale for older adults and can be used to assess daily living activities, both in- and outdoors [21]. Dressing, bathing, getting into chairs, climbing stairs, walking up and down the slopes, and going to social events are few examples of the activities included in the questionnaire. The questionnaire has 16 items and employs a 4-point Likert scale as follows: 1 = not at all concerned, 2 = somewhat concerned, 3 = fairly concerned, and 4 = very concerned. The final FES-I score is the sum of all the item answers, with the total score ranging from 16 to 64. A greater FES-I score indicates that the participant is extremely prone to falling [22].
Demographics and measurements
Demographic and medical data obtained from the participants included age (years), sex (male or female), weight (kg), height (cm), marital status (married or divorced/widowed), education level, occupational status (unemployed or employed), smoking status (yes or no), number of chronic conditions, and currently used medications. Body mass index (BMI) was calculated by dividing the weight in kilograms by the height in m2. Educational level was categorized as below elementary school, elementary, middle, high school, or university level. The number of chronic conditions was recorded as the sum of self-reported chronic conditions, including arthritis, diabetes, hypertension, cardiovascular diseases, dyslipidemia, anemia, osteoporosis, neurological conditions, and lower back pain. The Arabic version of the Patient Health Questionnaire 9 (PHQ-9) was used to measure depressive symptoms [23]. This self-reporting questionnaire has good validity and reliability [24]. The scores ranged from 0 to 27, with a greater score indicating greater depressive symptoms.
Timed Up and Go (TUG) test
The TUG test was used to measure the risk of falls [25]. In this test, the participants are asked to stand up, walk 3 m, turn around, walk back, and sit down. Each participant completed three trials. The first trial was for practice, and the average of the scores from the other two was calculated. Studies have shown that TUG is a sensitive and specific measure for identifying community-dwelling adults who are at risk of falls [25].
Functional Reach Test (FRT)
The FRT has been used to assess stability and balance in many health conditions [26]. Each participant completed three trials. The first was practice, and the average of the scores from the other two was calculated. For every trial, the participant was directed to stand near a wall without touching it and to place the arm closest to the wall at a 90-degree angle of shoulder flexion and the hand in a closed fist. The assessor marked the initial position of the third metacarpal bone on a large ruler. The participant was given the following instructions: reach as much as possible without taking a step. The third metacarpal position at the end of reach was recorded. The distance between the beginning and finishing points was measured in centimeters. A shorter distance indicated a higher risk of falls and poor balance.
10-m walk test (10-MWT)
The 10-MWT was used to measure gait speed reliably among older adults [27]. This test was used to determine walking speed over a short distance in meter per second. Ten meters was measured, including 2 m at the beginning for acceleration and 2 m at the end for deceleration. Participants were asked to walk at a comfortable pace over the entire distance. They were then instructed to walk as fast as possible over the same distance (maximum speed). The timer was started when the toes passed the acceleration mark and stopped once their toes entered the deceleration mark. For each participant, two trials were conducted, and the average scores were calculated [27]. In this study, the comfortable gait speed was used for the analysis.
6-min walk test (6-MWT)
This test examines the distance walked in 6 min and can be considered a test of endurance and aerobic capacity [28]. A greater distance in meters indicates better endurance and performance. During this test, the participants could rest while standing as much as needed, but the timer was not stopped during the rest periods. The period and number of rests were documented. Participants could use any assistive device or brace, which was documented. The turnaround points were marked by a cone. The participants were asked to wear comfortable clothes and shoes and eat light meals before the test. While walking, participants were informed of every lapsed minute.
Five Times Sit-to-Stand Test (5XSST)
The 5XSST was used to measure functional lower extremity strength, balance, and fall risk [29]. A stopwatch and a straight-backed chair of standard height (40.64 cm high) were used for this test. Patients were instructed to sit with their backs against that of the chair, with their arms folded over their chests. The timer started when the patient moved his/her back away from the chair, and each stand was counted aloud to keep the patient oriented. The timer was stopped when the patient achieved a standing position on the 5th repetition. The lower time recorded indicated better scores. This test is considered a reliable and valid measure of mobility in older adults [29].
Statistical analysis
The primary outcomes of this study were fall history and the FES-I. Fall history was categorized as yes (fallers) or no (non-fallers). The FES-I was used as a continuous variable. Descriptive statistics were expressed as counts for categorical variables and means with standard deviations for continuous variables in fallers and non-fallers. To compare fallers and non-fallers based on demographics and clinical variables, we used the chi-squared or Fisher’s exact test for categorical variables and an independent t-test for continuous variables.
To examine the association between balance measures and fall history, multiple binary logistic regression was used with odds ratios (OR) and 95% confidence intervals (95% CI) for each risk factor. The primary analysis was adjusted for possible confounders, including age, sex, BMI, education, employment status, marital status, smoking status, number of chronic conditions, depressive symptoms, and all other balance measures, including 10-MWT, TUG, 5XSST, FRT, and 6-MWT. Missing variables were handled through case-wise deletions.
Multiple linear regression analysis was used to examine the association between the balance measures and FES-I. Data were expressed as unstandardized coefficients (B) along with the standard error (SE). The primary analysis was adjusted for possible confounders, including age, sex, BMI, education, employment status, marital status, smoking status, number of chronic conditions, depressive symptoms, and all other balance measures, including the 10-MWT, TUG, 5XSST, FRT, and 6-MWT.
To determine the cutoff score for significant balance and mobility measures, a receiver operating characteristic (ROC) curve was utilized. The area under the ROC curve (AUC) indicates the overall accuracy of the model in detecting the presence or absence of an outcome, such as a fall versus no fall. To determine the best cutoff score, the Youden index (sensitivity + [1 − specificity]) was calculated, and the largest Youden index was used as the cutoff. Sensitivity and specificity were calculated to indicate true positive and true negative results, respectively. An alpha level of 0.05 was used for all analyses. All analyses were performed using the IBM SPSS for Mac version 25.0 (SPSS Inc., Chicago, IL, USA).
Results
In total, 206 participants were included in the final analysis. In this study, the prevalence of falls was 12.6% among community-dwelling older adults. Participants were classified as fallers if they had at least one fall in the past 12 months (n = 26) and as non-fallers if they did not fall in the past 12 months (n = 180). Table 1 shows the demographics and clinical characteristics of fallers and non-fallers. Of these variables, only sex, number of chronic conditions, and 5XSST score were statistically different between fallers and non-fallers.
The results of the multiple binary logistic regression examining balance measures associated with falls are presented in Table 2 with ORs and 95% CIs. Only 5XSST was significantly associated with falls (OR 1.17, 95% CI [1.03, 1.33], p = 0.019) after controlling for other covariates, including age, sex, BMI, education, employment status, marital status, smoking status, number of chronic conditions, depressive symptoms, and other balance measures. Fallers were approximately 17% more likely to have an increased time (s) for the 5XSST when compared to non-fallers.
The results of the multiple linear regression examining the association between balance measures and FES-I are shown in Table 3, with beta coefficients and 95% CIs. All balance measures were significantly associated with FES-I scores. An increase in the 5XSST time was associated with an increase in the FES-I score. In contrast, a decrease in scores on other balance measures (i.e., 10-MWT, TUG, FRT, and 6-MWT) was associated with an increase in the FES-I scores. These results were controlled for other covariates, including age, sex, BMI, education, employment status, marital status, smoking status, number of chronic conditions, depressive symptoms, and all other balance measures.
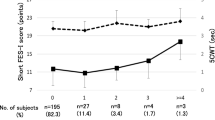
Cutoff scores were determined using ROC curves and AUC for significant balance measures associated with falls. Only 5XSST was significantly associated with falls, with a cutoff score of 13.93 s or more, a sensitivity of 0.73, and a specificity of 0.58 using Youden’s index, as shown in Table 4. The ROC curves are presented in Fig. 1.
Discussion
The current study is aimed at examining the prevalence of falls in community-dwelling adults in Saudi Arabia, as well as the balance measures associated with falls. This study showed that the prevalence of falls among community-dwelling adults was 12.6%. This was similar to the reported prevalence in some other countries, such as 12.9% (40–59 years old) and 16.5% (60–79 years old) in Japan [30]. Another study in Japan reported a prevalence of 15.9% [31], while one in China reported 11.1% [32]. However, these prevalence rates are much lower than those reported in our region, according to previous studies carried out in Riyadh (49.9% [33] and 57.7% [34]) and Unaizah (31.5%) [17]. Moreover, a meta-analysis reported that 45% of older adults living in Saudi Arabia and Gulf Cooperation Council countries had histories of falls [18]. Various factors could explain the disparities in fall prevalence rates between studies, including the differences in sample sizes and lack of controlling for possible covariates, such as the number of chronic conditions and lifestyle factors. However, the majority of these studies in Saudi regions were conducted on an older group of adults—those aged 60 years and older. This could explain the discrepancy in prevalence between previous evidence and our study.
In this study, we examined multi-balance outcome measures, including the TUG, 10-MWT, 5XSST, FRT, and 6-MWT. Only 5XSST was significantly associated with history of falls. Other balance measures were not associated with history of falls. This could be attributed to the low prevalence of falls in the current study (12.6%) and relatively younger adults (mean age 60 years). The 5XSST is a very reliable measure of dynamic balance and functional mobility, regardless of whether individuals are healthy or have disorders [29].
Poor sitting and standing performance are associated with a higher risk of falling [35]. Based on our results, an increase in 5XSST was significantly associated with an increased risk of falls. The findings of our study are consistent with a previous report indicating that a poor 5XSST time is associated with a higher risk of falls [36]. Other studies were consistent with our findings regarding the association between 5XSST and the risk of falls [37,38,39]. However, the majority of the previous studies included adults with a higher mean age than our study population, although the results were consistent [37,38,39]. Similar to our findings, a recent meta-analysis that included risk factors for falls among community-dwelling older adults found that 5XSST was a predictor of falls [39]. However, the studies included defined falling in a way (≥ 2 falls) different to our study (≥ 1 fall), and their included participants were older. In the current study, more than two falls were uncommon in fallers, which may be related to the generally younger age of the participants (mean age of participants = 60 years). In contrast to our results, Zhang et al. reported that the time to complete the 5XSST was not associated with fall risk [40]. This may be due to the difference in study design, theirs being a longitudinal study and ours a cross-sectional one.
Our study established the cutoff score (13.93 s) for 5XSST that was associated with falls in community-based Saudi adults aged 50 years and older. To our knowledge, this study was the first to determine a cutoff score for falls among the Saudi population. Therefore, comparisons with previously described population are not possible. Previous work has identified cutoff scores for 5XSST associated with falls in other regions in both eastern and western countries [36, 39, 41]. These cutoff scores ranged from 12 to 15 s for 5XSST [36, 39, 41]. Our cutoff score (13.93 s) was within this range of scores reported in previous literature. However, previous cutoff scores were based on at least two falls, a criterion different from ours, which was one fall or more. Future research should examine the prediction of falls using 5XSST using multiple approaches, such as longitudinal assessment and including recurrent falls.
In older adults, 5XSST performance has been linked to a variety of sensorimotor, balance, and psychological factors, in addition to knee extension, knee flexion, and ankle dorsiflexion strength [42]. Lord et al. found that nine measures (visual contrast sensitivity, lower limb proprioception, tactile sensitivity, simple foot reaction time, postural sway, body weight, reported pain, anxiety, and vitality) were significant and independent predictors of 5XSST performance [42]. Yamada and Demura suggested that there is a correlation between ground reaction force parameters during 5XSST, which might result in an increased risk of falls in older adults [35].
In our study, FES-I was significantly associated with 5XSST. These results are consistent with those of previous studies [43]. A previous study reported that greater FES-I scores were significantly associated with delayed time in the 5XSST and TUG [43]. This could indicate that participants with greater concern about falls and fear of falling had decreased functional mobility and balance.
Our study had some limitations. As this study was conducted on healthy and independent people aged 50 years and older, the findings cannot be generalized to all older adults. Another limitation was the cross-sectional study design, which could have limited the causality of these measures and the risk of falls. Future research should longitudinally examine the risk of falls and its relationship with balance and mobility measures. A sample size calculation was not done for the current study, although the number of participants and predictors was sufficient for statistical analysis using regression models. Therefore, the small sample might have affected the generalizability of the results. Future research should examine the statistical power and perform sample size calculations to minimize type II error. In addition, as the falls were self-reported in this study, the data was prone to recall bias, which may have affected the results. Finally, the sample size was small; therefore, future research should include more participants at a population-based level to obtain generalizable results.
Conclusion
This cross-sectional study found that the prevalence of falls is low (12.6%) among older adults living in Saudi Arabia. This fall rate was lower than that reported in previous studies conducted on different populations; thus, further research is required to confirm this finding. This study also found that an increase in time taken for performing the 5XSST was the only balance measure that was significantly associated with falls in older adults, with a cutoff score of 13.93 s and more. Slower gait speed, increased 5XSST time, decreased TUG time, decreased 6-MWT distance, and decreased FRT distance were associated with more concerns about falls, as identified using the FES-I. The 5XSST is an easy-to-administer test for mobility and can predict fall history among adults aged 50 years and older. The small sample size and cross-sectional design should be considered limitations of the current study. Future work should examine the risk of falls in a longitudinal study and with a larger sample size.
Data availability
Data will be available from the corresponding author based on reasonable request.
References
Sourdet S, van Kan GA, Soto ME et al (2012) Prognosis of an abnormal one-leg balance in community-dwelling patients with Alzheimer’s disease: a 2-year prospective study in 686 patients of the REAL.FR study. J Am Med Dir Assoc 13(4):407.e–6
World Health Organization, Ageing, and L.C. Unit (2008) WHO global report on falls prevention in older age. https://www.who.int/publications/i/item/9789241563536. Accessed 10 Nov 2022
Santos GM, Souza AC, Virtuoso JF et al (2011) Predictive values at risk of falling in physically active and no active elderly with Berg Balance Scale. Rev Bras Fisioter 15(2):95–101
Sterling DA, O’Connor JA, Bonadies J (2001) Geriatric falls: injury severity is high and disproportionate to mechanism. J Trauma 50(1):116–119
Tinetti ME, Williams TF, Mayewski R (1986) Fall risk index for elderly patients based on number of chronic disabilities. Am J Med 80(3):429–434
Cumming RG (1998) Epidemiology of medication-related falls and fractures in the elderly. Drugs Aging 12(1):43–53
Fuller GF (2000) Falls in the elderly. Am Fam Physician 61(7):2159
Sibley KM et al (2011) Balance assessment practices and use of standardized balance measures among Ontario physical therapists. Phys Ther 91(11):1583–1591
Bloem BR, Grimbergen YA, Cramer M et al (2001) Prospective assessment of falls in Parkinson’s disease. J Neurol 248(11):950–958
Berg K (1992) Measuring balance in the elderly: development and validation of an instrument. McGill University, Thesis
Lundin-Olsson L (2010) Community-dwelling older adults with balance impairment show a moderate increase in fall risk, although further research is required to refine how balance measurement can be used in clinical practice. Evid Based Nurs 13(3):96–97
Steffen TM, Mollinger LA (2005) Age- and gender-related test performance in community-dwelling adults. J Neurol Phys Ther 29(4):181–188
Steffen TM, Hacker TA, Mollinger L (2002) Age- and gender-related test performance in community-dwelling elderly people: six-minute walk test, Berg Balance Scale, Timed Up & Go test, and gait speeds. Phys Ther 82(2):128–137
Rubenstein LZ (2006) Falls in older people: epidemiology, risk factors and strategies for prevention. Age and ageing 35(suppl_2):ii37-ii41
Alamri S, Ghamri R, Alshehr W et al (2023) Falls and correlations among community-dwelling older adults: a cross-sectional study in Jeddah, Saudi Arabia. Pak J Med Sci 39(1)
Alenazi AM (2022) Number of medications and polypharmacy are associated with risk of fall in Saudi community-dwelling adults (in press). Saudi Pharm J
Alabdullgader A, Rabbani U (2021) Prevalence and risk factors of falls among the elderly in Unaizah City, Saudi Arabia. Sultan Qaboos Univ Med J 21(1):e86
Alqahtani BA, Alshehri MM, Hoover JC et al (2019) Prevalence of falls among older adults in the Gulf Cooperation Council countries: a systematic review and meta-analysis. Arch Gerontol Geriatr
Alghadir AH, Al-Momani M, Marchetti GF et al (2015) Cross-cultural adaptation and measurement properties of the Arabic version of the Fall Efficacy Scale International. Neurosciences 20(3):230–235
Halaweh H, Svantesson U, Rosberg S et al (2016) Cross-cultural adaptation, validity and reliability of the Arabic version of the Falls Efficacy Scale-International (FES-I). Med Princ Pract 25(1):1–7
Kempen GI, Todd CJ, Van Haastregt JC et al (2007) Cross-cultural validation of the Falls Efficacy Scale International (FES-I) in older people: results from Germany, the Netherlands and the UK were satisfactory. Disabil Rehabil 29(2):155–162
Kuo C-T, Chen DR, Chen YM et al (2021) Validation of the short Falls Efficacy Scale-International for Taiwanese community-dwelling older adults: associations with fall history, physical frailty, and quality of life. Geriatr Nurs 42(5):1012–1018
AlHadi AN, AlAteeq DA, Al-Sharif E et al (2017) An Arabic translation, reliability, and validation of Patient Health Questionnaire in a Saudi sample. Annals Gen Psychiatry 16(1):1–9
Kroenke K, Spitzer RL (2002) The PHQ-9: a new depression diagnostic and severity measure. SLACK Incorporated Thorofare, NJ. pp 509–515.
Shumway-Cook A, Brauer S, Woollacott M (2000) Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go test. Phys Ther 80(9):896–903
Behrman AL, Light KE, Flynn SM et al (2002) Is the Functional Reach Test useful for identifying falls risk among individuals with Parkinson’s disease? Arch Phys MedRehabil 83(4):538–542
Bohannon RW (1997) Comfortable and maximum walking speed of adults aged 20–79 years: reference values and determinants. Age Ageing 26(1):15–19
ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories (2002) ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med 166:111–117
Muñoz-Bermejo L, Adsuar JC, Mendoza-Muñoz M et al (2021) Test-retest reliability of Five Times Sit to Stand Test (FTSST) in adults: a systematic review and meta-analysis. Biology 10(6):510
Niino N, Tsuzuku S, Ando F et al (2000) Frequencies and circumstances of falls in the National Institute for Longevity Sciences, Longitudinal Study of Aging (NILS-LSA). J Epidemiol 10(1sup):90–94
Kitayuguchi J, Kamada M, Okada S et al (2015) Association between musculoskeletal pain and trips or falls in rural Japanese community-dwelling older adults: a cross-sectional study. Geriatr Gerontol Int 15(1):54–64
Fang X, Shi J, Song X et al (2012) Frailty in relation to the risk of falls, fractures, and mortality in older Chinese adults: results from the Beijing longitudinal study of aging. J Nutr Health Aging 16(10):903–907
Almegbel FY, Alotaibi IM, Alhusain FA et al (2018) Period prevalence, risk factors and consequent injuries of falling among the Saudi elderly living in Riyadh, Saudi Arabia: a cross-sectional study. BMJ Open 8(1):e019063
Alshammari SA, Alhassan AM, Aldawsari MA et al (2018) Falls among elderly and its relation with their health problems and surrounding environmental factors in Riyadh. J Family Community Med 25(1):29
Yamada T, Demura S-I (2009) Relationships between ground reaction force parameters during a sit-to-stand movement and physical activity and falling risk of the elderly and a comparison of the movement characteristics between the young and the elderly. Arch Gerontol Geriatr 48(1):73–77
Tiedemann A, Shimada H, Sherrington C et al (2008) The comparative ability of eight functional mobility tests for predicting falls in community-dwelling older people. Age Ageing 37(4):430–435
Intaruk R, Saengsuwan J, Amatachaya S et al (2021) The ability of Timed-Up and Go test and Five Times Sit-to-Stand Test to screen risk of fall in well-functioning elderly. Naresuan Phayao J 14(1):54–63
Manorangsan S, Panpeach P, Vorakittikul D (2015) Five-Times-Sit-to-Stand Test and activities-specific balance confidence scale in Thai fallers. Sci Technol Asia 20:18–28
Lusardi MM, Fritz S, Middleton A et al (2017) Determining risk of falls in community dwelling older adults: a systematic review and meta-analysis using posttest probability. J Geriatr Phys Ther 40(1):1
Zhang F, Ferrucci L, Culham E et al (2013) Performance on Five Times Sit-to-Stand Task as a predictor of subsequent falls and disability in older persons. J Aging Health 25(3):478–492
Buatois S, Perret-Guillaume C, Gueguen R et al (2010) A simple clinical scale to stratify risk of recurrent falls in community-dwelling adults aged 65 years and older. Phys Ther 90(4):550–560
Lord SR, Murray SM, Chapman K et al (2002) Sit-to-stand performance depends on sensation, speed, balance, and psychological status in addition to strength in older people. J Gerontol A Biol Sci Med Sci 57(8):M539–M543
Figueiredo D, Santos S (2017) Cross-cultural validation of the Falls Efficacy Scale-International (FES-I) in Portuguese community-dwelling older adults. Arch Gerontol Geriatr 68:168–173
Acknowledgements
The authors would like to thank the Prince Sattam bin Abdulaziz University.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by all authors. The first draft of the manuscript was written by all authors, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Participation was voluntary, in accordance with the Declaration of Helsinki, and all participants signed a consent form. The study was approved by the Research Ethics Committee of Prince Sattam bin Abdulaziz University (No. RHPT/021/017).
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Alosaimi, R.M., Almegbas, N.R., Almutairi, G.R. et al. The Five Times Sit-to-Stand Test is associated with both history of falls and fear of falling among community adults aged 50 years and older. Ir J Med Sci 192, 2533–2540 (2023). https://doi.org/10.1007/s11845-023-03287-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-023-03287-9