Abstract
Objectives
Data on vascular patients following amputation in Ireland is lacking, limiting capability to plan services. This paper seeks to benchmark survival and rehabilitation outcomes among vascular patients in Ireland following lower extremity amputation (LEA), and compare subgroups of those undergoing transfemoral (TFA) or transtibial amputation (TTA).
Methods
A review was conducted of all patients who underwent non-traumatic TFA or TTA from 2000 to 2009 in a tertiary vascular surgery centre. Demographics, surgical data, perioperative outcomes, medium-term functional outcomes, and survival were assessed.
Results
One hundred and seventy-two patients (2:1 male: female) underwent 192 non-traumatic LEAs. Median age for TFA was 75 years and TTA 67 (p = 0.002). A percentage of 36.5% had undergone prior attempts at surgical revascularization, 25% had undergone prior distal amputation or debridement. Thirty-three (17%) required stump revision. Twenty-three (13.2%) died in hospital. Median survival for those who died in hospital was 17 days (0–367), versus 17 months (2–106) for those who survived to discharge.
Conclusion
LEA for vascular pathology has significant morbidity and mortality, with long in-patient stays and short median survival; there is need to focus on improving quality of life in postoperative pathways.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
The incidence of the two major risk factors for LEA, diabetes and peripheral vascular disease (PVD), remain highly prevalent [1,2,3,4]. Public understanding of these conditions is relatively poor compared to other diseases, with limited awareness of their potential consequences [5,6,7]. Those with diabetes are 15 to 40 times more likely than non-diabetics to undergo amputation, and 53% of all LEA patients in Ireland are diabetic [8]. This is of increasing concern with the increasing prevalence of these conditions, currently estimated to be 4.5 to 8.8% of the general population [1,2,3,4]. These conditions are significant risk factors for LEA, and rates of amputation for diabetes mirror this trend in a significantly morbid population [4, 9, 10]. A 5-year survival following LEA is comparable to or worse than for most malignancies [9, 11].
Perioperative mortality is reported to be lower in those whom were selected for TTA (6.5%) compared to TFA (12.8%) [12, 13]. The higher level of amputation has correlates with frailty and morbidity. This has been shown not to be due to the amputation itself, but a reflection of the patient’s overall condition and frailty which led to the decision for TFA over TTA [12, 13].
LEA and the time that precedes it have a considerable impact on quality of life. Those with diabetes and its associated complications are two to three times more likely to suffer from depression while suicidal ideation was common among individuals 1 year after LEA [14, 15]. LEA impacts activities of daily living leading to increased hospital admissions, poor physical health and premature death [15]. LEA has a significant impact on ambulation and independence. Cruz et al. have shown a reduction in ambulation, from 73% of patient’s ambulating pre-LEA to only 23% post-LEA [16]. TTA provides advantages in terms of mobility compared to TFA due to preservation of the knee joint allowing for less energy expenditure and improved rehabilitation [17]. However, the reasons for selecting a TFA often relate to patient frailty and overall medical condition, with ambulation not being a realistic option for many of those selected for TFA due to their overall status [16].
LEA in a frail cohort with comorbidities has significant implications for service planning and delivery. Having data on patterns of LEA and outcomes is essential in designing services and primary and secondary prevention strategies in our study population.
There is very little data regarding this subject in Irish patients. Given the significant organizational difference of our healthcare provision to other jurisdictions internationally, it is important to have data specific to the Irish population to inform healthcare delivery. We have similar data for Irish patients with Charcot’s foot and diabetic feet, but not where that may lead—amputation [18, 19]. This study was conducted in a tertiary vascular centre which is one of two equally sized centres serving the needs of these patients in the Ireland East Hospital Group, representing a catchment population of 1.1million, with annual population growth of 0.8%, and a > 65 population growth of 3–4% [20].
This study focuses on transfemoral (TFA) and transtibial (TTA) amputations only. The objective of this study was to describe the characteristics, trends and outcomes of LEA in a tertiary vascular centre in Ireland, as a means of benchmarking outcomes in the Irish setting. We describe characteristics and 5-year survival outcomes of an Irish cohort of dysvascular LEA patients with TFA compared to TTA. The study also aimed to evaluate rehabilitation outcomes in a small subgroup of patients for whom this data was available. Through comparison, further detail on the prognosis of these patients can be accurately identified. Utilising this data, we can compare ourselves to international best practice and provide a basis upon which future care can be audited and improved.
Methods
Design and recruitment
Ethical approval for this retrospective study was obtained from St. Vincent’s University Hospital audit committee (no. 588). All patients who underwent non-traumatic lower extremity amputations at our tertiary centre between 1 January 2000 and 31 December 2009 were included. Data from our associated rehabilitation hospital was collected regarding mobility outcomes. Permission was obtained from the General Registry Office to utilize the National Death Registry; this was used to obtain a minimum of 5-year survival data for all patients and cross referenced with hospital records. For this study, only LEAs to the extent of a transtibial or transfemoral amputation were analysed; digital and partial foot amputations were not included. All amputations for trauma or oncological reasons were excluded.
Data sources
Data was gathered from a number of different sources including the Hospital In-Patient Enquiry (HIPE) database, patient medical records and operating theatre records. Survival data was collected via the National Death Registry over 5 years following the final recorded amputation in this population.
Patients
Demographic information collected included patient’s age, gender, side and level of amputation, length of stay, admission source, discharge source, 30 day mortality, date of death, primary cause of death, and date of last follow-up. Patient comorbidities were collected according to the Charleson comorbidity index.
Other information collected included radiological imaging results and number of admissions to the NRH.
Ambulation
Mobility outcomes following discharge from the NRH were scored using the SIGAM (Special Interest Group in Amputee Medicine) mobility grade. SIGAM scores were first described in a 2003 publication and its use increased over time, with the majority of patients from 2008 onwards having SIGAM scores recorded [21]. While individual needs may vary, service-wide mobility needs can be much more easily identified with this scoring, and is an easily calculated metric to measure progress among the patient population over time.
Statistics
Statistical analysis was performed using SPSS 24.0. Continuous variables were assessed for normality using the Shapiro–Wilk test. Variables are reported in reference to the median, and the Mann–Whitney U test was used to compare continuous variables between the two patient groups (TFA and TTA). The Pearson Chi-square test was used to compare categorical variables between groups. Kaplan–Meier curves were generated using censored modelling.
Results
Demographics
One hundred and ninety-two lower extremity amputations were performed on 172 patients over the study period. Forty-nine TTAs were performed, and 143 TFAs, giving a TTA:TFA ratio of 1:2.9. There was a significantly higher prevalence of diabetes among patients in the TTA than the TFA group (Table 1).
Sixty-three patients were female (36.6%) and 109 patients were male (63.4%). One hundred and twenty-five (65.1%) amputations were performed in men, and 67 (34.9%) in women. Patients undergoing TFA were significantly older (median 75 years) compared to those undergoing TTA (median 67 years) (p = 0.002). For those who underwent a TFA, 87 (60.8%) were male and 56 (39.2%) were female.
For those who underwent a TTA, 38 (77.6%) were male, while 11 (22.4%) were female.
The median length of stay (LOS) for patients who underwent a LEA during the study period was 28 days. This was significantly longer in the TTA group (41 days) compared to TFA (25 days) (p = 0.006).
Sixty-four (37.3%) patients or 76 (39.8%) of all amputations were diabetic; 41 (24.4%) patients were known to have cardiac disease (44 amputations, 22.9%); 26 (15.1%) patients had a history of myocardial infarction (30 amputations, 15.6%); 23 (13.4%) patients had a history of cerebrovascular disease (CVA) (24 amputations, 12.5%). The median CCI (Charleson comorbidity index) score was 6; the CCI scale runs up to 37, but no patient scored higher than 13. Mean follow-up was 27 months.
Previous imaging and revascularisation
Eight percent of patients had undergone a previous angiogram (contrast or CT); 20.3% had undergone previous endovascular revascularisation and 40.5% previous surgical revascularisation. A significantly higher proportion of TTA patients had previously undergone attempts at endovascular revascularisation (Table 1).
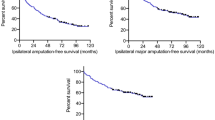
Survival post-LEA
Of the 174 operated patients, 23 (13.2%) died in hospital. The median survival for the whole group was 14.6 months postoperatively (SE .326), representing a non-linear mortality pattern as shown in the Kaplan–Meier curve in Fig. 1. Differences between amputation types were not statistically significant (Table 2).
A calculated 3-year survival was similar for TFA and TTA at 34% and 35% respectively. A 5-year survival rate was 19% and 28% for TFA and TTA respectively. Of the patients who died, 78.3% (18/23) had undergone urgent or emergency procedures and 73.9% (17/23) of those had a TFA performed.
Primary vs. secondary procedure
Twenty patients initially had other surgical procedures, and then progressed to requiring LEA as a secondary procedure during the same inpatient episode (Table 3). Many of these were distal amputations, revascularisation procedures, or combinations of both.
Stump revision
Thirty-three limbs required stump revisions (Table 4). The level (TTA or TFA) did not have an effect on rates. A history of surgical (but not interventional) revascularisation, and prior amputation at any level (even on the other side) was associated with stump revision.
Rehabilitation
Seventy-six of 192 patients (52%) patients were transferred to or attended the National Rehabilitation Hospital. Where data was available, their mean LOS in that hospital was 30 days (SD 29). The median Charleson comorbidity index was the same for those who attended as those who did not: 6. There was no difference between amputation type—36.7% (TTA) vs. 40.6% (TFA), p = 0.637. The mean waiting time for admission to the NRH was 53 days, with some patients attending the NRH after discharge from the hospital.
Of the 76 patients who went to the NRH, SIGAM (Special Interest Group in Amputee Medicine) outcome scores were available on 35 (46%) of them, which are given in Table 5. SIGAM scores were not available on patients who had been referred for rehabilitation prior to 2007, and the calculation of individual scores was not readily available, thus cannot be further analysed in depth. Reasons for SIGAM A outcomes included poor exercise tolerance, cardiac issues, stroke, inability to complete rehabilitation due to psychiatric issues, and two cases of delayed wound healing and contractures. Thirty-one percent of patients referred to rehabilitation were transferred back to hospital following rehabilitation.
Discussion
This study confirms the significant morbidity and mortality associated with LEA. There is very little available date on outcomes following amputation in Irish patients, and the data that is available often groups together unrelated aetiological causes such as trauma and oncological amputations with diabetic foot complications and peripheral vascular disease. Analysis of data confined to peripheral arterial disease and diabetes mellitus patients as is done internationally is more useful as it focuses solely on the older, frailer population of patients, and excludes those who may have been in excellent physical condition prior to their amputation for trauma-related injuries.
Survival
LEA is associated with high rates of mortality with 1-year mortality ranging from 13.7 to 48.3% in previously reported studies [9, 12, 22,23,24,25]. Perioperative mortality rates internationally are better for TTA (0.9% to 14%) than TFA (2.8% to 35%) [9]. This likely reflects morbidity burden in patients with a higher level of amputation [26]. Our morbidity burden was not significantly different between the two groups when stratified through the CCI index score but a larger cohort may demonstrate statistical significance.
In-hospital mortality in our study was 13.2% in keeping with internationally reported data [27]. Increased short-term (30-day) mortality has been shown to be associated with older age and greater numbers of comorbidities [12, 23]. With advances in diagnostics and therapeutics in PVD, the ultimate aim for clinicians treating those at risk of limb loss should be to reduce the number of LEA where possible. Jones et al. analysed Medicare data from 2000 to 2008 and found that patients who underwent LEA had mortality rates that were nearly twice as high as those who did not undergo LEA [12].
With 3-year survival rates of less than 35% regardless of amputation and a 5-year survival dropping further as far as 19% in TFA in our study, post-amputation mortality is on par with or worse than many cancers. Of the top 21 most commonly diagnosed cancers in the UK, only 5 have worse survival rates: oesophagus, lung, brain, lung, and pancreas [11].
Morbidity
This high level of mortality more than likely reflects the frailty of our patient population who may be very susceptible to opportunistic infections and deconditioning. High-quality pre- and post-amputation multi-disciplinary care constitutes best practice. This requires input from physiotherapy, occupational therapy, social work, and rehabilitation services.
Ortho-geriatric physicians are a well-established element of many acute orthopaedic units and their participation has been shown to significantly improve outcomes. Their involvement is now regarded as a basic standard of care under NICE guidelines [28]. We should now also consider the inclusion of dedicated physicians routinely in the acute and follow-up care of these patients in order to maximise outcomes and minimise further morbidity.
Level of amputation
One of the areas where our study differed in comparison to the international literature was the ratio of TFA to TTA. In our study the ratio of TFA to TTA was nearly 3:1. Studies focusing specifically on non-traumatic LEA have shown higher rates of TFA compared to TTA, and higher ratios of TFA to TTA are found among nursing home residents overall [9, 16]. Our high TFA rate is likely a reflection of our patient population, which include a large number of elderly males from nursing homes. TFA in these patients is often more appropriate due to the level of comorbidity and the fact that many of these patients are already immobile prior to presentation.
When determining the level of amputation, a number of factors are taken into account. TTA is the procedure of choice where possible in order to reduce energy expenditure and improve functional and mobility outcomes. Conversion to TFA occurs in 15–20% [29, 30]; preoperative factors such as age > 70 years, dementia, end-stage renal failure, history of stroke, and limited preoperative mobility have been identified as markers of poor performance post-amputation [31, 32]. In our study, 10.4% (20/192) of amputations performed were done as secondary procedures. In this cohort of patients, studies have suggested that primary TFA is preferable to TTA to avoid the need for revision surgery. The low rate of subsequent conversion in this study cohort, combined with the higher proportion of TFA overall, suggests our decision process for opting for primary TFA in the more frail and bed-bound successfully prevents most patients returning to theatre at a later date to have a higher revision.
The discrepancy in length of stay between TTA and TFA suggests that the mean LOS may reflect waiting times for transfer to rehabilitation rather than true recovery time. Our median LOS was 28 days (25 for TFA and 41 for TTA). These figures are comparable to figures from the UK published during the same time period [33]. Healthcare strategies may not always prioritise home adaptations when a nursing home is more readily available. A patient with a lower level of amputation is more likely to return to remain mobile and in independent living after their hospital stay, but would require home adaptations to be facilitated before discharge. Waiting for these can significantly delay discharge, increasing the median LOS; thus, the LOS is not necessarily reflective of clinical status. In recent years, our centre has improved it assisted discharge facilities allowing for step-down care out of the acute hospital setting until their home is ready.
Mobility and rehabilitation
Predicting post-amputation mobility in a vascular population is difficult. Factors such as older age, preoperative mobility, poor baseline cognition, and poor baseline activities of daily living (ADL) have been identified as predictors of poor functional outcome and rates of mobility after amputation [31, 32, 34]. Those who were living at home preoperatively were found to be most likely to be ambulatory post-LEA [35]. While ambulation is one of the primary aims following amputation this is not always possible and setting of realistic post-amputation goals is important. In our study, 76% of amputees achieved some level of ambulation on discharge from rehabilitation (SIGAM C to F). It is well recognized that preoperative MDT assessment is important. In our institution, where possible, all prospective amputees are referred and seen by all relevant allied healthcare professionals and the medical rehabilitation team prior to amputation.
Stump revision
Interestingly, revision rates for TFA and TTA were equivalent. Those requiring revision were much more likely to have had previous surgical revascularization or another amputation (Table 4). This is likely reflective of the pattern of underlying disease progression in PVD compared to other causes such as diabetic foot infection.
Public health
Increasing awareness of PVD and diabetes is important in reducing LEA. Public knowledge of PVD is poor and greater public/patient education is needed to improve the recognition of the signs and symptoms of PVD [5]. More than 85% of LEA in diabetics are precipitated by a foot ulcer [36]. Dedicated diabetic foot clinics have been shown to reduce amputation rates as well as leading to substantial savings [37, 38].
In the current series, those patients undergoing TTA were more likely to have diabetes than the TFA group. Many of these amputations could have potentially been avoided. With a rising level of diabetes in the general population, this should remain a high priority for healthcare outcomes in minimising healthcare needs and retaining independence among these patients for as long as possible. Fortunately, in recent years, the morbidity associated with diabetic feet has been acknowledged, and the diabetic foot model of care has been implemented. This provides for ongoing review and clear escalation protocols in the at risk foot [39]. To further achieve this effectively, a national prospective LEA database in the Republic of Ireland would help guide service planning going forward. This could then be used for further multi-centre analysis similar to this study for more comprehensive service provision and improvement.
Limitations
The time period for data collection was 2000–2009 to enable adequate follow-up for survival analysis. Changes may have occurred in the interim to improve outcomes. Pre amputation level of mobility was not included in our analysis as recording was not consistent across hospital records. Therefore, we cannot comment on the comparative level of retained independence or mobility after amputation. Furthermore, routine recording of SIGAM outcome scores, which were first described in a 2003 publication, increased during the study period, but the study included patients since 2000. While the SIGAM scores are very good, this represents a small cohort (n = 35) (Table 5). Those that are accepted to the NRH are typically the best candidates, thus most likely to succeed. Our rehabilitation numbers remain comparatively low due to capacity constraints, and thus may not be a fair comparison to other jurisdictions.
Due to the retrospective nature of data collection, data on comorbidities may also be underreported. Our population did not demonstrate a statistical difference between the TTA and TFA groups, yet international literature would indicate otherwise, perhaps reflecting an underpowered metric in this cohort. Other data we would have liked to assess was the effect of patency of revascularised limbs on subsequent stump revision; data on prior revascularisation was gathered, but whether they remained patent was not known. The study also only looked at rehabilitation outcomes from patients who were referred to the National Rehabilitation Hospital (NRH). Patients who were referred from other hospitals may have been sent to rehabilitation elsewhere; this data was not available.
Conclusion
As the incidence of diabetes and PVD increases so too do the numbers of those at risk of LEA. Previous Irish studies have rarely assessed this subgroup of patients, grouping them with oncology and trauma patients making this study all the more relevant to planning their care. This study confirms the significant impact of diabetes on limb loss. This is becoming an increasing problem in Ireland with a rapid rise in the number of diabetic foot infections in younger patients. The current data also illustrates the relationship of LEA on outcome and survival in this group of patients, likely as a surrogate indicator of frailty. This highlights the need to sustain these patients’ quality of life during their remaining months and years by minimising the time spent in the acute hospital setting. Improving timely access to rehabilitation and step-down services is essential to maximise quality of life and functional outcomes. This data is important to consider in healthcare planning, and provides a benchmark from which to assess our services into the future.
References
Fowkes FG, Rudan D, Rudan I et al (2013) Comparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: a systematic review and analysis. Lancet 382(9901):1329–1340. https://doi.org/10.1016/S0140-6736(13)61249-0
Guariguata L, Whiting DR, Hambleton I et al (2014) Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract 103(2):137–149. https://doi.org/10.1016/j.diabres.2013.11.002
Balanda KP, Buckley CM, Barron SJ et al (2013) Prevalence of diabetes in the Republic of Ireland: results from the National Health Survey (SLAN) 2007. PLoS One 8(10):e78406. https://doi.org/10.1371/journal.pone.0078406
Ogurtsova K, da Rocha Fernandes JD, Huang Y et al (2017) IDF Diabetes Atlas: global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Res Clin Pract 128:40–50. https://doi.org/10.1016/j.diabres.2017.03.024
Hirsch AT, Murphy TP, Lovell MB et al (2007) Gaps in public knowledge of peripheral arterial disease: the first national PAD public awareness survey. Circulation 116(18):2086–2094. https://doi.org/10.1161/CIRCULATIONAHA.107.725101
Lovell M, Harris K, Forbes T et al (2009) Peripheral arterial disease: lack of awareness in Canada. Can J Cardiol 25(1):39–45
Cronin CT, McCartan DP, McMonagle M et al (2015) Peripheral artery disease: a marked lack of awareness in Ireland. Eur J Vasc Endovasc Surg 49(5):556–562. https://doi.org/10.1016/j.ejvs.2014.12.017
Buckley CM, O'Farrell A, Canavan RJ et al (2012) Trends in the incidence of lower extremity amputations in people with and without diabetes over a five-year period in the Republic of Ireland. PLoS One 7(7):e41492. https://doi.org/10.1371/journal.pone.0041492
Aulivola B, Hile CN, Hamdan AD et al (2004) Major lower extremity amputation: outcome of a modern series. Arch Surg 139(4):395–399; discussion 399. https://doi.org/10.1001/archsurg.139.4.395
Humphries MD, Brunson A, Hedayati N et al (2016) Amputation risk in patients with diabetes mellitus and peripheral artery disease using statewide data. Ann Vasc Surg 30:123–131. https://doi.org/10.1016/j.avsg.2015.04.089
Quaresma M, Coleman MP, Rachet B (2015) 40-year trends in an index of survival for all cancers combined and survival adjusted for age and sex for each cancer in England and Wales, 1971-2011: a population-based study. Lancet 385(9974):1206–1218. https://doi.org/10.1016/S0140-6736(14)61396-9
Jones WS, Patel MR, Dai D et al (2013) High mortality risks after major lower extremity amputation in Medicare patients with peripheral artery disease. Am Heart J 165(5):809–815, 815 e801. https://doi.org/10.1016/j.ahj.2012.12.002
Nelson MT, Greenblatt DY, Soma G et al (2012) Preoperative factors predict mortality after major lower-extremity amputation. Surgery 152(4):685–694; discussion 694-686. https://doi.org/10.1016/j.surg.2012.07.017
Ismail K, Winkley K, Stahl D et al (2007) A cohort study of people with diabetes and their first foot ulcer: the role of depression on mortality. Diabetes Care 30(6):1473–1479. https://doi.org/10.2337/dc06-2313
Turner AP, Meites TM, Williams RM et al (2015) Suicidal ideation among individuals with dysvascular lower extremity amputation. Arch Phys Med Rehabil 96(8):1404–1410. https://doi.org/10.1016/j.apmr.2015.04.001
Cruz CP, Eidt JF, Capps C et al (2003) Major lower extremity amputations at a Veterans Affairs hospital. Am J Surg 186(5):449–454
Fisher SV, Gullickson G Jr (1978) Energy cost of ambulation in health and disability: a literature review. Arch Phys Med Rehabil 59(3):124–133
O'Loughlin A, Kellegher E, McCusker C, Canavan R (2017) Diabetic charcot neuroarthropathy: prevalence, demographics and outcome in a regional referral centre. Ir J Med Sci 186(1):151–156. https://doi.org/10.1007/s11845-016-1508-5
Forde H, Wrigley S, O'Murchadha LT et al (2019) Five-year outcomes of patients attending a diabetic foot clinic in a tertiary referral Centre. Ir J Med Sci. https://doi.org/10.1007/s11845-019-02108-2
Ireland East Hospital Group Operational Plan: HSE (2018) Available from: https://www.hse.ie/eng/services/publications/serviceplans/service-plan-2018/operational-plans-2018/ireland-east-hospital-group-operational-plan-2018.pdf
Ryall NH, Eyres SB, Neumann VC et al (2003) The SIGAM mobility grades: a new population-specific measure for lower limb amputees. Disabil Rehabil 25(15):833–844. https://doi.org/10.1080/0963828021000056460
Pohjolainen T, Alaranta H (1998) Ten-year survival of Finnish lower limb amputees. Prosthetics Orthot Int 22(1):10–16. https://doi.org/10.3109/03093649809164452
Kristensen MT, Holm G, Kirketerp-Moller K et al (2012) Very low survival rates after non-traumatic lower limb amputation in a consecutive series: what to do? Interact Cardiovasc Thorac Surg 14(5):543–547. https://doi.org/10.1093/icvts/ivr075
Kulkarni J, Pande S, Morris J (2006) Survival rates in dysvascular lower limb amputees. Int J Surg 4(4):217–221. https://doi.org/10.1016/j.ijsu.2006.06.027
Basu NN, Fassiadis N, McIrvine A (2008) Mobility one year after unilateral lower limb amputation: a modern, UK institutional report. Interact Cardiovasc Thorac Surg 7(6):1024–1026. https://doi.org/10.1510/icvts.2008.180422
Dillon MP, Quigley M, Fatone S (2017) Outcomes of dysvascular partial foot amputation and how these compare to transtibial amputation: a systematic review for the development of shared decision-making resources. Syst Rev 6(1):54. https://doi.org/10.1186/s13643-017-0433-7
Moxey PW, Hofman D, Hinchliffe RJ et al (2010) Epidemiological study of lower limb amputation in England between 2003 and 2008. Br J Surg 97(9):1348–1353. https://doi.org/10.1002/bjs.7092
Hip fracture: management clinical guideline [CG124] (2011) vol Clinical guideline [CG124], May 2017 edn. National Institute of Clinical Excellence. Available from: https://www.nice.org.uk/guidance/cg124
Dormandy J, Heeck L, Vig S (1999) Major amputations: clinical patterns and predictors. Semin Vasc Surg 12(2):154–161
Nehler MR, Coll JR, Hiatt WR et al (2003) Functional outcome in a contemporary series of major lower extremity amputations. J Vasc Surg 38(1):7–14
Taylor SM, Kalbaugh CA, Blackhurst DW et al (2005) Preoperative clinical factors predict postoperative functional outcomes after major lower limb amputation: an analysis of 553 consecutive patients. J Vasc Surg 42(2):227–235. https://doi.org/10.1016/j.jvs.2005.04.015
Vogel TR, Petroski GF, Kruse RL (2014) Impact of amputation level and comorbidities on functional status of nursing home residents after lower extremity amputation. J Vasc Surg 59(5):1323–1330 e1321. https://doi.org/10.1016/j.jvs.2013.11.076
Vamos EP, Bottle A, Majeed A, Millett C (2010) Trends in lower extremity amputations in people with and without diabetes in England, 1996-2005. Diabetes Res Clin Pract 87(2):275–282. https://doi.org/10.1016/j.diabres.2009.11.016
Sansam K, Neumann V, O'Connor R, Bhakta B (2009) Predicting walking ability following lower limb amputation: a systematic review of the literature. J Rehabil Med 41(8):593–603. https://doi.org/10.2340/16501977-0393
Suckow BD, Goodney PP, Cambria RA et al (2012) Predicting functional status following amputation after lower extremity bypass. Ann Vasc Surg 26(1):67–78. https://doi.org/10.1016/j.avsg.2011.07.014
Apelqvist J, Larsson J (2000) What is the most effective way to reduce incidence of amputation in the diabetic foot? Diabetes Metab Res Rev 16(Suppl 1):S75–S83. https://doi.org/10.1002/1520-7560(200009/10)16:1+<::AID-DMRR139>3.0.CO;2-8
Nason GJ, Strapp H, Kiernan C et al (2013) The cost utility of a multi-disciplinary foot protection clinic (MDFPC) in an Irish hospital setting. Ir J Med Sci 182(1):41–45. https://doi.org/10.1007/s11845-012-0823-8
Canavan RJ, Unwin NC, Kelly WF, Connolly VM (2008) Diabetes- and nondiabetes-related lower extremity amputation incidence before and after the introduction of better organized diabetes foot care: continuous longitudinal monitoring using a standard method. Diabetes Care 31(3):459–463. https://doi.org/10.2337/dc07-1159
Model of care for the diabetic foot (2011) National Diabetes Programme Working Group, Dublin. Available from: http://hdl.handle.net/10147/326403
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval was granted by the local hospital board. No unique patient identifiers were gathered.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Maguire, S.C., Mohan, H.M., Fenelon, C. et al. Trends and outcomes of non-traumatic major lower extremity amputations in an Irish tertiary referral hospital. Ir J Med Sci 189, 1351–1358 (2020). https://doi.org/10.1007/s11845-020-02231-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-020-02231-5