Abstract
Background
Nasal foreign body(-ies) (FB) cause local irritation, inflammation, and mucosal erosion and carry a potential risk of aspiration. The aim is to describe the management of nasal FBs in our Emergency Department (ED).
Method
A retrospective study of 100 sequential suspected nasal FB presentations to a tertiary paediatric ED. Patient age, gender, FB typology, doctor/nurse seniority, sedation/analgesia usage, removal method, ENT referral rate, extraction time and disposition were collected. Data was inputted to Microsoft Excel®.
Results
One hundred cases were encountered over 16 months: 51 males and 49 females. Median age was 3.4 years (range 0.8–10). Of the 73 FB visualised in the ED, 78% (57/73) were successfully removed by ED staff. Sixteen visualised in ED required ENT removal. Of those 16 FBs, 7 were removed at OPD while 9 were removed by ENT in ED.
Discussion
The ED physician/advanced nurse practitioner successfully managed most children with a nasal FB in the ED. The goal of the management should be to minimise complications/repeated attempts. Formation of a national guideline to assist in ED removal and timely care will hopefully improve patient’s experience. It will include guidance on topical anaesthetic use, performing radiographs for radiopaque objects not initially visualised and limiting ED staff extraction attempts.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nasal foreign bodies (FBs) make up roughly 0.1% of presentations to paediatric emergency departments (PED) [1]. Children present with orifice FBs due to various age-related or developmental stage-related factors such as curiosity, imitation, boredom, playing, intellectual disability (older children) and availability of relatively small objects [2]. Nasal FBs can be difficult to deal with and occasionally life threatening [1]. They have the potential to damage nasal mucosa and cause life-threatening respiratory distress should they dislodge and obstruct the airway [3]. Importantly, the nasal button battery warrants emergent removal [4, 5].
Nasal FBs come in many shapes and sizes. They are divided into organic and non-organic materials. Studies report children’s toys as the most commonly encountered FB present in 23–46% of cases and food-related FBs in 12–27% of cases [3, 6, 7].
Given that there is such a wide variety of objects that can be found lodged in the nasal cavity, it is important that physicians are comfortable with multiple removal methods [2, 5]. Methods of removal include positive pressure, suctioning, forceps removal, use of catheter devices and ENT hook [2, 5]. One method of positive-pressure removal is commonly termed “the parental kiss” [8]. This is where the parent covers the unaffected nostril and blows into their child’s mouth. It has been shown to be safe and a useful first-line method of removal [8]. The vast majority of intranasal FBs are removed on first presentation and do not require specialist skills [9]. Failure of removal in the ED leads to increased use of resources.
Primary aim of this study was to describe the management of 100 consecutive children with suspected nasal FB, who presented to our ED. Secondary outcomes included time to removal, need for specialist ENT assistance, need for sedation/anaesthetic, and method of removal.
Methods
This is a retrospective descriptive review of patients presenting with a suspected nasal FB to a tertiary PED. We decided, a priori, to analyse 100 consecutive cases. Patients were identified using their presenting complaint/discharge diagnosis on the ED information system. The identifying discharge diagnosis used was “Nasal foreign body”. The following presenting complaint terms were screened: “nose”, “nostril”, “nasal”, “ENT” and “foreign body”. There is no age limit in this study.
Patient’s electronic, paper and radiological assessments were reviewed. Demographics, type of FB, doctor/nurse experience, sedation/analgesia usage, removal method, referral rate and time to discharge were collected. This data was inputted in a Microsoft Excel® spreadsheet.
Descriptive statistical analysis was performed using Microsoft Excel 2010 software®. By using this programme, mean, median and inter-quartile ranges (IQR) were determined for relevant data points.
Results
Results included 100 consecutive patients with a suspected nasal FB who presented to the PED over the 16-month period (January 2016–April 2017). ED census for this time period was 50,563 patient episodes of care. The frequency of suspected nasal FB was 0.2% (100/50563) of all attendances. There were 49 females and 51 males. The age range was 10 months–10 years, median age of 3 years 4 months (IQR 2 years 5 months to 4 years 6 months). Detailed age breakdown was as follows: 1 patient under 1 year (10 months old), 39 patients between 1 and 3 years, 39 patients between 3 and 5 years and 21 patients ≥ 5 years. The eldest patient encountered was 10 years old.
An advanced nurse practitioner (ANP) delivered care in 13 cases, consultant in 8, registrar in 36 and senior house officer (SHO) in 43 cases. Of the 100 charts analysed, 11 had no nasal FB identified after ED clinician review, no ENT consultation and were discharged home. None of these patients represented to the ED within the study period. FBs were identified on direct visualisation in 73; 57 of these were successfully removed by ED staff. The exact location within the nasal cavity was documented in only 3 cases. In total, 27 cases had no FB visualised by ED staff and 16/27 (59.2%) were referred to ENT colleagues.
The total number referred to ENT was 32. ENT referral rates varied by clinician grade: ANPs referred 5/13 (38.5%), consultants 3/8 (37.5%), registrars 12/36 (33.3%) and SHOs 12/43 (27.9%) cases.
There were 16 patients that had no visible FB on initial ED review and were then referred to ENT. Ultimately, 6/16 had FBs removed (5 in ENT OPD and 1 in theatre under general anaesthetic). The remainder had no FBs visualised. Radiographs were performed in 2/27 cases where FBs were not visualised on initial ED review. One radiograph demonstrated a piece of Lego™ in the nasopharynx which was subsequently removed by ENT in the ED (Fig. 1).
Children presented with a history of self-inserted FB, parental visualisation of the FB or symptoms of localising pain, unilateral discharge or epistaxis. A single child had a background of autism, attention-deficit hyperactivity disorder and global developmental delay.
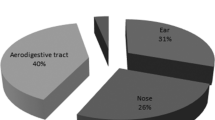
In total, 81 FBs were identified (73 identified by ED, 6 removed by ENT and 2 sneezed out prior to review). Of the 81 FBs identified, food and beads were the most commonly removed items. Organic items were seen in 22 cases and non-organic items accounted for the remaining 56. The most common food types were nuts and raisins. Beads were the second most common FB, 22.2% (18/81). Lego™ was seen in 16% of cases (13/81). Pieces of jewellery, most commonly the back of an earring, accounted for 8.6% (7/81). Miscellaneous items (24.6%; 20/81) included objects such as paper, toy cars, teddy bear’s eye and cotton wool, amongst others. There were no cases of button battery or magnet insertion (Fig. 2).
Previous unsuccessful attempts at removal, prior to ED attendance, were noted in 19 cases: 7/19 by parents and 12/19 by GPs or rapid access clinics. Method of removal in ED was only documented in 6 cases: 3 cases by ENT hook and the remaining with ENT forceps or suctioning.
No major complications, such as septal perforation, were observed. Nasal epistaxis occurred in 8 children (8/100). This was managed conservatively in all the children. Only two out of the 8 children with epistaxis had pre-hospital removal attempts.
Of the 73 that had FB’s visualised in ED, successful removal rate by ED staff was 78% (57/73). Of those referred to ENT, 7 were removed in ENT OPD the following day while 9 were removed by ENT in the ED during the same visit. One patient underwent removal of FB in theatre under general anaesthetic. This patient presented with unilateral purulent discharge without a visible FB and was brought to theatre for endoscopic examination. A plastic bead was subsequently removed. One patient underwent procedural sedation, using inhaled nitric oxide, in the ED to assist removal. No patients were given analgesia (oral/ topical) to facilitate removal.
The procedure duration was not documented in any case. When a FB was successfully removed by an ED physician, the mean duration of consultation was 63.6 min (IQR 19–100 min). The need for ENT opinion/removal extended the mean duration of consultation to 123.6 min (IQR 64–174 min).
The number of attempts at removal in the ED was documented in 70 of the cases; 21 had no attempts by PED staff, of which 15 were referred to ENT; 40 had one attempt, with 4 subsequently referred (10%); 5 had two attempts, 4 of which referred to ENT (80%). Three attempts was the maximum documented and all four patients were subsequently referred to ENT.
Discussion
This study describes current management of nasal FBs in a tertiary PED. The majority of nasal FBs can be successfully removed by PED staff [7, 10]. Mackle et al. quote successful removal of nasal FBs in ED in 65% of cases [10]. Our review found a successful removal rate by ED staff of 78% when the FB was visible at presentation (57/73). Successful removal by PED staff of total number of FBs in our review was 70.4% (57/81). A review in the USA demonstrated a greater incidence of ENT intervention within the ED [9]. While 64.7% of the children had their nasal FBs removed in the ED, nearly half of these were removed by otolaryngology residents/attending physicians [9]. An Australian study has quoted a higher success rate of 84%, within a mixed cohort of adult and paediatric patients [11]. Successful removal by ED staff reduced patient ED experience time.
There were no identified incidences of serious complications in any of the patients in this review. Serious complications of nasal FBs include posterior dislodgement and aspiration, trauma caused by the object itself/removal attempts, infection and choanal stenosis [5, 6]. Epistaxis was the only reported complication in this study and managed conservatively in all cases. Number of removal attempts was documented in 70% of the cases. Those that had > 2 removal attempts were nearly always referred to ENT. This emphasises the need for early expertise with appropriate equipment/environment to maximise success and minimise patient distress. Epistaxis occurred in three of the patients that had one removal attempt in hospital and one patient that had two. We are unsure of the number of removal attempts in the other children that had epistaxis.
No clinical practice guideline existed in our ED during the study period. The greatest variation in management identified was in patients with a clear history of nasal FB insertion but without direct visualisation in the ED. The literature supports performing radiographs in these cases [12]. If concern exists, radiographs should be performed to rule out button batteries, which would ultimately lead to emergent removal [12]. This was only performed in 2 of the cases where the foreign body was not seen on direct vision. Local anaesthesia before foreign body removal may facilitate efficient, effective retrieval [7]. No patients within our study received local anaesthetic prior to removal. The majority of our patients did not require sedation for FB removal with only two children requiring sedation/general anaesthetic. This is a much lower frequency than previously reported in other studies. Awad et al. quoted a rate of general anaesthetic use of 14.06% [5]. Use of topical local anaesthetic is recommended in the literature and its use in our department may potentially improve rates of successful removal [7].
Typology of nasal foreign objects included food, toys and common household items [3, 7]. Due to the variability, emergency physicians should be competent in several techniques for removing the different types of FB. There are various methods of removal, including the use of positive pressure, direct removal with forceps and balloon catheter devices [2, 5]. Literature suggests that most nasal FBs can be removed with direct visualisation using forceps, hook or suction catheters [5, 13]. Knowledge of the type of foreign body assists in a physician’s decision on the removal method chosen, e.g. forceps are commonly used for sponge and hooks for beads/hard items [14, 15]. Removal method in this study was poorly documented making it difficult to report the most frequently used tools or which pieces of equipment have improved success rates and for which types of FB. Timely removal is important to prevent local damage and infection.
There were several limitations to this study. The review was retrospective, using written documentation and not all parameters of interest were recorded in every case. The procedural time for removing the FB was not documented in any of the cases and the patient consultation time was derived from the ED information system. Presenting history was only documented in a handful of cases and pre-existing complications at presentation were not differentiated from complications resulting from FB removal (e.g. epistaxis). Mean times were not weighted by significant variables such as ED overcrowding.
Conclusion
This review documented a higher than expected incidence of suspected nasal FBs, at 0.2%, relative to previously published data [16].
The ED clinician successfully managed most children with a nasal FB. The goal of management should be to minimise complications and distress, which often occurs from repeated attempts at removal. Use of a clinical guideline, topical anaesthetic and restricting initial attempts may increase success rates further and minimise distress. ENT opinion should be sought whenever there is concern that an attempt may result in trauma. Urgent referral to ENT was not required in most cases and a follow-up in the ENT outpatient clinic the following day was adequate. Following this review, a clinical guideline was developed to direct management of ENT and inhaled foreign bodies [8].
References
Kiger JR, Brenkert TE, Losek JD (2008) Nasal foreign body removal in children. Pediatr Emerg Care 24:785–792. https://doi.org/10.1097/PEC.0b013e31818c2cb9
Nandapalan V, Mcilwain JC (1994) Removal of nasal foreign bodies with a Fogarty biliary balloon catheter. J Laryngol Otol 108(9):758–760. https://doi.org/10.1017/S0022215100128038
Baker MD (1987) Foreign bodies of the ears and nose in childhood. Pediatr Emerg Care 3(2):67Y70
Guidera AK, Stegehuis HR (2010) Button batteries: the worst case scenario in nasal foreign bodies. N Z Med J 123(1313):68–73
Awad AH, Eltaher M (2017) ENT foreign bodies: an experience. Int Arch Otorhinolaryngol 22:146–151. https://doi.org/10.1055/s-0037-1603922
Tong MC, Ying SY, van Hasselt CA (1996) Nasal foreign bodies in children. Int J Pediatr Otorhinolaryngol 35(3):207–211
Kadish HA, Corneli HM (1997) Removal of nasal foreign bodies in the pediatric population. Am J Emerg Med 15(1):54–56. https://doi.org/10.1016/S0735-6757(97)90049-8
Ui Bhrian S, Blackburn C (2018) Irish Association for Emergency Medicine. Foreign bodies: the emergency department management of inhaled and inserted objects in children. IAEM CG12
Scholes MA, Jensen EL (2016) Presentation and management of nasal foreign bodies at a tertiary children’s hospital in an American metro area. Int J Pediatr Otorhinolaryngol 88:190–193. https://doi.org/10.1016/j.ijporl.2016.07.016
Mackle T, Conlon B (2006r) Foreign bodies of the nose and ears in children. Should these be managed in the accident and emergency setting? Int J Pediatr Otorhinolaryngol 70(3):425–428
Gupta R, Nyakunu RP, Kippax JR (2016) Ear Nose Throat J 95(3):113–116
Glynn F, Amin M, Kinsella J (2008) Nasal foreign bodies in children: should they have a plain radiograph in the accident and emergency? Pediatr Emerg Care 24(4):217–218. https://doi.org/10.1097/PEC.0b013e31816a9f1b
Chan TC, Ufberg J, Harrigan RA, Vilke GM (2004) Nasal foreign body removal. J Emerg Med 26:441–445. https://doi.org/10.1016/j.jemermed.2003.12.024
Davies PH, Benger JR (2000) Foreign bodies in the nose and ear: a review of techniques for removal in the emergency department. Emerg Med J 17:91–94
Shrestha I, Shrestha BL, Amatya RCM (2012) Analysis of ear, nose and throat foreign bodies in Dhulikhel hospital. Kathmandu Univ Med J 10(38):4–8
Fox JR (1980) Fogarty catheter removal of nasal foreign bodies. Ann Emerg Med 9(1):37–38. https://doi.org/10.1016/S0196-0644(80)80439-2
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dann, L., Doody, J., Howard, R. et al. Nasal foreign bodies in the paediatric emergency department. Ir J Med Sci 188, 1401–1405 (2019). https://doi.org/10.1007/s11845-019-02000-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-019-02000-z