Abstract
Background
The Acute Medical Admission Unit (AMAU) model of care has been associated with improved short- and medium-term outcomes; whether these improvements are sustained remains unclear. We report on the 15-year outcomes of an AMAU in our institution.
Methods
All emergency medical admissions between 2002 and 2016 were examined and 30-day in-hospital mortality, admission rates, readmission rates and length of stay (LOS) assessed. We used logistic and Poisson regression and margin statistics to evaluate outcomes.
Results
There were 96,305 admissions in 50,612 patients. By admission, the 30-day in-hospital mortality averaged 5.6% (95% CI 5.4 to 5.7%); there was a relative risk reduction (RRR) of 33.9% between 2002 and 2016, from 7.0 to 4.6% (p = 0.001), number need to treat (NNT) 41.9. By unique patient the 30-day in-hospital mortality averaged 10.5% (95% CI 10.3 to10.8%); there was a RRR of 61.7% between 2002 and 2016, from 15.1 to 5.8% (p = 0.001), NNT 10.7. The median LOS was 5.0 days (IQR 2.1, 9.8) and was unaltered over time. Deprivation status strongly influenced the admission rate/1000 population increasing from Q1 7.7 (95% CI 7.6 to 7.8) to Q5 37.8 (95% CI 37.6 to 38.0); this showed a slight trend to increase over time. Total readmissions increased as a function of time; early readmissions (< 4 weeks) remained constant 10.5% (95% CI 9.6 to 11.3).
Conclusion
The 30-day in-hospital mortality showed a linear trend to reduce over the 15 years following the institution of an AMAU; other key parameters were unaltered.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Acute Medicine is that part of hospital medicine concerned with the immediate and early specialist management of adult patients suffering from a wide range of medical conditions requiring urgent or emergency care [1]. The continued rise in demand for emergency care together with spiralling healthcare costs has led to increased investigation into identifying service effectiveness [2, 3]. Demographic changes combined with the complex medical needs of an ageing population necessitate investment in acute care delivery; increased life expectancy has been coupled with an increased time spent living with chronic disabling conditions [4]. Consequently, the complexity and costs of acute healthcare delivery can be anticipated to increase. Clinical services are therefore under scrutiny in an attempt to achieve greater healthcare cost-efficiency and ultimately to try to reduce healthcare costs [5].
The process of care delivery influences patient outcomes—formerly, it was not uncommon for patients to be admitted and dispersed widely around the hospital with little regard for coordination of investigations or therapy. A body of evidence subsequently emerged indicating that the consequences of the inefficiencies described resulted in longer hospital stays [6] and an increase in direct patient risk such as medical error, complications and avoidable death [7]. Thus, Acute Medicine developed in the UK as a result of changes in the demographic and clinical environment. Specifically, the recognition that the admission of acutely unwell medical patients represented the major source of work for most hospitals coupled with the drive to improve clinical governance standards was important. Improved outcomes have occurred with reforms such as care delivery via an acute medical admission unit (AMAU) [8, 9], other structural reforms [10, 11] and the presence of senior consultant interventions [12,13,14].
The AMAU was the natural development of this process, and as such, it represented as much a philosophy of care as being a physical entity. It propelled a significant growth in a new discipline of acute medicine in the UK as evidenced by a 63% increase in the number of consultants in acute medicine between 2002 and 2007, whilst also highlighting that 92% of hospitals were admitting sick medical patients to an AMAU [15]. AMAUs were also established in Australia and Ireland, and the hospitalist movement has been gaining in popularity in North America [16]. The unifying feature being the recognition that traditional models of hospital care were not patient centred delivered poor outcomes and offered bad value for money, in conjunction with the recognition that standardising aspects of medical management of many conditions can improve outcomes [17, 18]. In this paper, we report 15-year outcomes following the introduction of an AMAU to our institution.
Materials and methods
Background
St. James’s Hospital Dublin serves as a secondary care centre for emergency admissions in a catchment area with a population of 270,000 adults. All emergency medical admissions are admitted from the Emergency Department to an AMAU opened in 2003, the operation and outcome of which have been described elsewhere [9, 8, 19].
Data collection
An anonymous patient database was employed, collating core information of clinical episodes from the Patient Administration System (PAS), the national hospital in-patient enquiry (HIPE) scheme, the patient electronic record, the Emergency Department and laboratory systems. HIPE is a national database of coded discharge summaries from acute public hospitals in Ireland [20, 21]. The International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) has been used for both diagnosis and procedure coding from 1990 to 2005 with ICD-10-CM used since then. Data included parameters such as the unique hospital number, admitting consultant, date of birth, sex, area of residence, principal and up to nine additional secondary diagnoses, principal and up to nine additional secondary procedures and admission and discharge dates. Additional information cross-linked and automatically uploaded to the database includes physiological, haematologic and biochemical parameters.
Deprivation index
Irish census returns reports are based on electoral divisions, the smallest administrative areas for which population statistics are reported. Using principle components analysis (PCA), a weighted combination of four indicators was derived, relating to unemployment, social class, type of housing tenure and car ownership, as described by the SAHRU investigators [22]. The methodology has previously been described in greater detail [23]; the deprivation index scores were ranked from low (least deprived) to high (most deprived) and divided into quintiles according to their ranked raw scores. We utilised the registered address on our patient administration system to allocate each address to a divisional area, with a corresponding matched SAHRU deprivation index raw score and quintile rank. This attribute data were joined to the small area polygon geometries based upon their relative geographic positions, using the ArcGS Geographic Information System software implementation of the point-in-polygon algorithm [24].
From the 2006 census returns information, the total population within each unit area and a range of local area statistics were available. The incidence rate for emergency medical admissions for our catchment area was calculated by summing admissions for each electoral division over 15 years and calculating an average for each (numerator) and dividing by the total population within each area (divisor). The quintiles of deprivation were based on the national calculation rather than the local catchment population. There are a total of 74 electoral divisions in the catchment area with a total population of 210,443 persons. The median population per electoral division was 2845 (IQR 2020, 3399). The electoral divisions in our catchment area have a high proportion of deprivation, ranked nationally as quintile I (n = 13), quintile III (n = 5), quintile IV (n = 4) and quintile V (n = 49), but by chance, there are none rated as quintile II.
Statistical methods
Descriptive statistics were calculated for background demographic data, using means/standard deviations (SD), medians/interquartile ranges (IQR) or percentages, as appropriate. Comparisons between categorical variables were made using chi-squared tests. Analyses were performed on either per admission or per patient basis. For the latter, one admission only per patient was permissible; the last admission was used if the patient had more than one admission. The ‘medical’ length of stay (LOS) was estimated using a ‘trimmed’ data set; a shortage of nursing home beds and resources means that 50% of all acute bed utilisation is attributable to just 11% of episodes. Patients remaining in hospital awaiting long-term care were excluded from LOS analyses.
We derived and applied an acute illness severity score [25, 26], predicting 30-day in-hospital mortality from parameters recorded in the Emergency Department [27,28,29]. We adjusted for previously demonstrated outcome predictors the Charlson comorbidity index [30], chronic disabling disease score [31] and blood culture status (a surrogate for sepsis) [32].
We employed a logistic model with robust estimate to allow for clustering; the correlation matrix thereby reflected the average dependence among the specified correlated observations. We used the margins command in Stata to estimate and interpret adjusted predictions for interactions of key predictors, whilst controlling for other variables, using computations of average marginal effects. Margins are statistics calculated from predictions of a previously fitted model at fixed values of some covariates and averaging or otherwise over the remaining covariates. Computed are the levels of margins for different covariate values or the differences in levels of margins if covariate values are changed (marginal effects). For a continuous covariate, margins compute the first derivative of the response with respect to the covariate. For a discrete covariate, margins compute the effect of a discrete change of the covariate (discrete change effects).
For hospital admission rates, we employed a truncated Poisson regression model, including predictive outcome categorical variables in the model as a series of indicator variables. The dependent variable of the admission rate is restricted to certain values; the predictor variables are therefore regressed against admission rates using the truncated Poisson model. We used robust standard errors for the parameter estimates, as recommended by Cameron and Trivedi [33]. Using the truncated Poisson regression model, we can interpret the coefficients in terms of incidence rate ratios (IRR). In the multivariable model (logistic or Poisson), we adjusted univariate estimates of effect, using the previously described outcome predictor variables.
Adjusted odds ratios (OR) and 95% confidence intervals (CI) or IRRs were calculated for those predictors that significantly entered the model. Statistical significance at p < 0.05 was assumed throughout. Stata v.13.1 (Stata Corporation, College Station, TX) statistical software was used for analysis.
Results
Patient demographics
A total of 96,305 admissions in 50,612 patients over the 15-year study period were included. These represented all emergency medical admissions, including patients admitted directly into the intensive care unit or high dependency unit. The proportion of males was 48.7%. The median (IQR) length of stay (LOS) was 5.2 (2.0, 13.1) days. The median (IQR) age was 62.1 (40.3, 78.4) years, with the upper 10% boundary at 86.1 years. Of the total, 70,543 admissions in 33,343 patients were resident within the catchment area and used for admission rate incidence calculations.
Admission characteristics related to illness severity
The data in Table 1 contrasts the demographics of the emergency admissions based on the calculated acute illness severity score. Those with high illness severity were more likely to be female, 51.8 vs 48.3% (p < 0.001), and to be older, mean age 69.7 years (95% CI 54.1 to 80.1) vs 35.0 years (95% CI 26.5 to 45.8) (p < 0.001). They had higher Charlson comorbidity indices and chronic disabling disease scores. They were also more likely to die, 5.7 vs 0.2% (p < 0.001), or to have an extended hospital stay, mean LOS 5.8 days (95% CI 2.5 to 10.9) vs 3.2 days (95% CI 1.4 to 6.2) (p < 0.001).
Impact on mortality and hospital length of stay
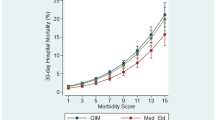
By admission, the 30-day in-hospital mortality over the 15-year period averaged 5.6% (95% CI 5.4 to 5.7%); there was a relative risk reduction (RRR) of 33.9% between 2002 and 2016, from 7.0 to 4.6% (p = 0.001), with a number needed to treat (NNT) of 41.9 (Fig. 1). Considering the 2002–2006, 2007–2011 and 2012–2016 timeframes, the respective 30-day in-hospital mortality rates were 6.4% (95% CI 6.2 to 6.7%), 5.3% (95% CI 5.1 to 5.6%) and 4.9% (95% CI 4.7 to 5.2%) (Scheffe multiple comparison overall p < 0.001, last two time comparisons p = 0.07).
By patient, the 30-day in-hospital mortality averaged 10.5% (95% CI 10.3 to 10.8%); there was a RRR of 61.7% between 2002 and 2016, from 15.1 to 5.8% (p = 0.001), NNT 10.7 (Fig. 2). Considering the time periods of 2002–2006, 2007–2011 and 2012–2016, the respective mortalities were 13.7% (95% CI 13.1 to 14.2%), 11.0% (95% CI 10.5 to 11.5%) and 8.1% (95% CI 7.7 to 8.4%) (p < 0.001 for each comparison).
The median LOS was 5.0 days (IQR 2.1, 9.8); the median LOS for the three time periods was 5.1 (IQR 2.1, 9.8), 5.0 (IQR 2.0, 9.7) and 5.1 (IQR 2.2, 9.8).
Multivariable model with adjustment for risk categories
In the full multivariable model, we included adjustment for acute illness severity score, Charlson comorbidity index, chronic disabling disease score, sepsis status, a weekend admission and the effects of time. Each of these was independently predictive of the risk of 30-day in-hospital mortality (Table 2). By patient, there was a significant reduction in the mortality rate over time—OR 0.95 (95% CI 0.95, 0.96); mortality declined from 14.8% (95% CI 14.1 to 15.4) to 9.3% (95% CI 8.9 to 9.8). By admission, there was also a significant reduction in mortality over time OR 0.98 (95% CI 0.97, 0.98); mortality declined from 6.7% (95% CI 6.4 to 7.0) to 5.0% (95% CI 4.8 to 5.3).
Admission rate incidence, age profile and social factors
We calculated the admission incidence rates (/1000 population) for the three time periods; 2002–2006, 2007–2011 and 2012–2016. The predicted probabilities for each were derived from the zero truncated regression multiple variable model, adjusted for age profile and deprivation index. Between 2002 and 2011, there was little evidence in any change in the admission rate incidence. The admission incidence increased as a function of the social deprivation from 6.9 to 36.2/1000 between 2002 and 2006 and from 6.9 to 38.1/1000 between 2007 and 2011. For the period 2012–2016, the admission rate incidence were for Q1 10.2 (95% CI 10.0 to 10.3), Q3 19.8 (95% CI 19.7 to 20.0), Q4 27.6 (95% CI 27.5 to 27.7) and Q5 38.6 (95% CI 38.5 to 38.6) (Fig. 2). These admission rates were somewhat increased compared with the earlier 5-year periods at lesser degrees of deprivation (p < 0.001). However as the respective frequency distribution of admissions, related to a deprivation index of 1, 3, 4 and 5, was 5.2, 4.7, 4.8 and 85.3%, the small differences in admission rate incidences would not be expected to have materially influenced the total number of hospital emergency medical admissions over the 15-year study period.
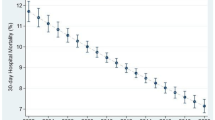
Readmissions and time
The total number of readmissions between 2002 and 2016 was examined and predicted probabilities derived from the truncated Poisson regression model, adjusted for acute illness severity score, Charlson comorbidity index, chronic disabling disease score and a weekday or weekend admission. All these were significant predictors of a readmission. The number of readmissions increased over time from 2.9 (95% CI 2.8 to 2.9) after 1 year to 18.1 (95% CI 17.1 to 19.1) by 15 years (Fig. 3a). However, early readmissions within 4 weeks were unchanged over time, averaging 10.5% (95% CI 9.6 to 11.3) (Fig. 3b).
Discussion
There has been much debate about the value of reform of acute care delivery when implemented via an AMAU [8, 9]. As previously stated, the AMAU represents as much a philosophy of care as a physical entity. Over the 15 years following the implementation of an AMAU at our institution, there was a relative risk reduction of 33.9% in 30-day in-hospital mortality by admission from 7.0 to 4.6% and when calculated per patient of 61.7% from 15.1 to 5.8%. As is evident from the graphical depiction of mortality over time, mortality essentially declined as a linear function. This mortality reduction must not be emphasised representing the crude annual mortality rates, but rather that adjusted for major outcome predictors such as acute illness severity score [25], Charlson comorbidity index [30], chronic disabling disease score [31], blood culture status [32] and the ‘weekend effect’. Therefore, the fall in mortality was not due to a change in admission policy or lower risk categories, but rather represented the outcome figure adjusted for major risk factors [25].
The AMAU model has theoretical advantages in terms of system organisation and delivery at a number of levels. The concentration of acute medical admissions in a single location within a large hospital facilitates urgent medical care in the critical initial hours and days following an emergency admission. In the design of our AMAU, we had several strategic objectives. Accessibility for staff and patient flow were important design considerations. As the bulk of patients were to be admitted from the Emergency Department (rather than general practice referrals), the AMAU needed to be proximate to the Emergency Department. Diagnostic imaging was likely to be necessary for the majority of patients, and a small number (4–5%) would require transfer to the intensive care unit. We wished senior staff (60–70 separate consultant teams) to prioritise requests from the AMAU; therefore, it had to be in a central location. All of these requirements were fulfilled in that the AMAU area chosen was located equidistant between the Emergency Department and the hospital main entrance, along the hospital ground floor corridor. It was on the opposite side of the corridor to the ground floor Diagnostic Imaging Department, with the intensive care units and the high dependency units almost overhead on the first floor.
These factors were under the control of the design team. However, the increased future capacity of the AMAU in terms of bed numbers required was not adequately envisaged at the time of development. The average emergency 24-h ‘take’ was less than 20 patients in 2002; patients could not remain in the AMAU longer than 5 days (an explicit design limit), but there was an aspirational LOS target of 3 days for the majority. Therefore, the two 30-bedded central general medical wards that were to be reconfigured into the AMAU were thought sufficient or even to provide an excess of the capacity required. Of course, the hospital capacity constraints were not perhaps adequately considered or taken into account when making these determinations. Ireland has 3.1 acute hospital beds versus a European average of 5.3/1000; for a population of 4.7 million, this implies a deficit of acute capacity just over 10,000 beds. An Irish Department of Health strategy document (the Codd report) recognised the immediate need in 2001 for 1500 new beds with 6000 further beds before 2006 [34]. At that time, 23 hospitals were found to have occupancy levels of greater than the functionally ideal occupancy rate of 85% with an average occupancy level of 95%. In effect, this meant that movements into the AMAU and transfer out were always going to be problematic with a negative impact on outcomes [35]. It could be argued that the AMAU capacity in any event is an academic number in relationship to systematic capacity constraints. However, patients could not always be admitted to the AMAU, and those admitted to outlying wards due to space constraints appeared to have worse outcomes [9].
We have previously reported that more experienced physicians (more than 20-year experience) achieved better mortality outcomes over the AMAU operation period [14]. The latter phenomenon is of interest because the only time constant of the medical team over the entire period was the presence of the consultant. The system was a consultant directed rather than a consultant-delivered service. For most of the time, treatment was delivered by a team consisting of an intern (< 1-year experience), senior house officer (< 3-year experience) and a senior registrar (5–10-year experience) with a supervising consultant (at least 15-year experience prior to consultant appointment). The patients admitted might be discussed with the consultant when admitted, if urgent, but ordinarily, the consultant review of each emergency would occur initially on the ‘post-take’ ward round (8 a.m. onwards on the morning after the 24-h take period). The medical staff typically would work a 40-h week plus the ‘on-call’ element. This was typically from 9 a.m. on the day of the take until perhaps 12 a.m. the following day—a 30-h on-call period would not be deemed unusual, often with limited sleep. However, the fact that teams of more experienced consultants experienced better outcomes suggest that the mentoring process resulted in superior performance [36]. The implementation of the AMAU model in our country has, broadly speaking, resulted in an increasing proportion of the acute medical take being cared for by consultant physicians with less years of experience; the younger newly appointed AMAU consultants have taken over a significant proportion of the care of acutely admitted medical patients. The data would suggest that this may not be the optimum approach to patient care and that there is still an important role for more experienced physicians within the department. The EU established the European Working Time Directive (EWTD) in 2003 to avoid the exploitation of employees, with a limit on the number of working hours, 4-week paid annual leave and mandatory rest periods in every 24-h shift. In 2004, junior doctors came under the EWTD remit and their working week was limited to 58 h, and further reduced to 48 h in 2009. The rostering system for the AMAU altered in 2014 as a direct result of this process; we found no evidence of a detrimental impact on training or patient outcomes to date despite the implied reduction in training time and experiential learning [37, 38].
A number of previous studies have reported on outcomes following the introduction of either an AMAU or a similar initiative. Our group has previously reported improvements in outcomes consistent with the trend seen here at both 5 and 10 years following the introduction of our AMAU [8, 39]. It would be natural to assume that the substantial initial improvements achieved after the introduction of the AMAU may have plateaued as experience and competency in acute medicine progressed; however, even after 15 years, a threshold level does not appear to have been reached and better outcomes continue to be achieved. A study from Liverpool reported a similar significant reduction in mortality following the introduction of an AMAU, but this appeared to be confined to the subgroup of younger patients [40]. A number of other studies assessing AMAU performance have reported positive effects on outcome metrics such as readmission rates and duration of hospital stay but in contrast have found only no or minor effects on mortality [41,42,43]. Some of these differences may be related to study power although the potential importance of the characteristics of the individual AMAUs cannot be out ruled.
As with any study and methodology, there are limitations to our work. There have been improvements in mortality over time in the population as a whole. The extent and significance of these are difficult to estimate, and therefore, there is some difficulty in disentangling the proportion of the improvements in mortality we have observed following the introduction of the AMAU from those which would have occurred regardless of this reform. There are no studies estimating the reductions in inpatient mortality over a similar time period in Ireland. The Global Burden of Disease Study 2015 estimated that male and female life expectancy in Ireland increased by 1.6 and 2.5 years respectively over the 10-year period to 2015 [44]. Of course, it is difficult to draw comparisons between such disparate data; however, the overall reductions in population mortality do not appear to be as dramatic as those which we have reported over a similar time period. In addition, we have previously shown that patients admitted to other wards in our institution when the AMAU capacity was exceeded have a significantly worse outcome [9]. Therefore, whilst there undoubtably have been general improvements in mortality over the 15 years of the study, a significant degree of the mortality improvements are likely to be attributable to the implementation of the AMAU model. Finally, whilst this study covers all admissions under general medicine, our hospital has a number of other admitting services including cardiology and surgical specialties. The results we report here therefore are limited by the patient cohort available and may not be applicable to other services and diseases.
In conclusion, our study demonstrates sustained benefits in mortality over the 15-year period following the introduction of an AMAU. This demonstrates the potential improvements achievable through systems reform in the provision of acute medical care.
References
Langlands A, Dowdle R, Elliott A et al (2009) RCPE UK Consensus Statement on Acute Medicine, November 2008. British J Hospital Medicine London, England 2005(70):S6–S7
Litvak E, Bisognano M (2011) More patients, less payment: increasing hospital efficiency in the aftermath of health reform. Health Aff (Millwood) 30:76–80
Moses HI, Matheson D, Dorsey E et al (2013) The anatomy of health care in the United States. JAMA 310(18):1947–1963
Lynch C, Holman C, Arcy J et al (2007) Use of Western Australian linked hospital morbidity and mortality data to explore theories of compression, expansion and dynamic equilibrium. Australian Health Review : a Publication Australian Hospital Assoc 31:571–581
Curfman G, Morrissey S, Drazen J (2013) High-value health care—a sustainable proposition. N Engl J Med 369:1163–1164
Liew D, Kennedy MP (2003) Emergency department length of stay independently predicts excess inpatient length of stay. Med J Aust 179:524–526
Sprivulis PC, Da Silva JA, Jacobs IG et al (2006) The association between hospital overcrowding and mortality among patients admitted via Western Australian emergency departments. Med J Aust 184:208–212
Conway R, O’Riordan D, Silke B (2014) Long-term outcome of an AMAU—a decade’s experience. QJM 107:43–49. https://doi.org/10.1093/qjmed/hct199
Coary R, Byrne D, O’Riordan D, Conway R, Cournane S, Silke B (2014) Does admission via an acute medical unit influence hospital mortality? 12 years’ experience in a large Dublin hospital. Acute medicine 13:152–158
Scott I, Vaughan L, Bell D (2009) Effectiveness of acute medical units in hospitals: a systematic review. Int J Qual Health Care 21:397–407
Byrne D, Silke B (2011) Acute medical units: review of evidence. Eur J Intern Med 22:344–347
Bell D, Lambourne A, Percival F, Laverty AA, Ward DK (2013) Consultant input in acute medical admissions and patient outcomes in hospitals in England: a multivariate analysis. PLoS One 8:e61476
Conway R, O’Riordan D, Silke B (2013) Consultant volume, as an outcome determinant, in emergency medical admissions. QJM 106:831–837. https://doi.org/10.1093/qjmed/hct119
Conway R, O’Riordan D, Silke B (2014) Consultant experience as a determinant of outcomes in emergency medical admissions. Eur J Intern Med 25:151–155. https://doi.org/10.1016/j.ejim.2013.12.012
Kingdom TFotRCoPotU (2008) Census of consultant physicians in the UK: data and commentary. London
Peterson MC (2009) A systematic review of outcomes and quality measures in adult patients cared for by hospitalists vs nonhospitalists. Mayo Clin Proc 84:248–254
Indredavik B, Bakke F, Solberg R, Rokseth R, Haaheim LL, Holme I (1991) Benefit of a stroke unit: a randomized controlled trial. Stroke 22:1026–1031
Rogers AM, Ramanath VS, Grzybowski M et al (2007) The association between guideline-based treatment instructions at the point of discharge and lower 1-year mortality in Medicare patients after acute myocardial infarction: the American College of Cardiology’s Guidelines Applied in Practice (GAP) initiative in Michigan. Am Heart J 154:461–469
Conway R, Byrne D, O’Riordan D et al (2015) Patient risk profiling in acute medicine: the way forward? QJM 108:689–696. https://doi.org/10.1093/qjmed/hcv014
O’Loughlin R, Allwright S, Barry J et al. (2005) Using HIPE data as a research and planning tool: limitations and opportunities. Ir J Med Sci 174:40–45; discussion 52–47
O’Callaghan A, Colgan MP, McGuigan C, Smyth F, Haider N, O’Neill S, Moore D, Madhavan P (2012) A critical evaluation of HIPE data. Ir Med J 105:21–23
Kelly A, Teljeur C (2007) SAHRU National Deprivation Index. http://www.sahru.tcd.ie/services/ deprivation/DeprivationFiles/WebReport07.pdf
Conway R, Galvin S, Coveney S, O’Riordan D, Silke B (2013) Deprivation as an outcome determinant in emergency medical admissions. QJM 106:245–251. https://doi.org/10.1093/qjmed/hcs233
Shimrat M (1962) Algorithm 112: position of point relative to polygon. Commun ACM 5:434
Silke B, Kellett J, Rooney T, Bennett K, O’Riordan D (2010) An improved medical admissions risk system using multivariable fractional polynomial logistic regression modelling. Q J Med 103:23–32. https://doi.org/10.1093/qjmed/hcp149
O’Sullivan E, Callely E, O’Riordan D et al (2012) Predicting outcomes in emergency medical admissions—role of laboratory data and co-morbidity. Acute Medicine 2:59–65
Courtney D, Conway R, Kavanagh J et al (2014) High-sensitivity troponin as an outcome predictor in acute medical admissions. Postgrad Med J:1–7
Conway R, Creagh D, Byrne DG, O’Riordan D, Silke B (2015) Serum potassium levels as an outcome determinant in acute medical admissions. Clinical Medicine (London, England) 15:239–243. https://doi.org/10.7861/clinmedicine.15-3-239
Conway R, Byrne D, O’Riordan D, Silke B (2014) Hyponatraemia in emergency medical admissions—outcomes and costs. J Clinical Medicine 3:1220–1233. https://doi.org/10.3390/jcm3041220
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Chotirmall SH, Picardo S, Lyons J, D’Alton M, O’Riordan D, Silke B (2014) Disabling disease codes predict worse outcomes for acute medical admissions. Intern Med J 44:546–553
Chotirmall SH, Callaly E, Lyons J, O’Connell B, Kelleher M, Byrne D, O’Riordan D, Silke B (2016) Blood cultures in emergency medical admissions: a key patient cohort. European J Emergency Medicine : official J European Soc Emergency Medicine 23:38–43. https://doi.org/10.1097/MEJ.0000000000000192
Cameron A, Trivedi P (2009) Microeconometrics using Stata. Stata Press, College Station, TX
Children DoH (2002) Acute hospital bed capacity. http://health.gov.ie/wp-content/uploads/2014/04/Acute-Hospital-Bed-Capacity.pdf
Plunkett PK, Byrne DG, Breslin T, Bennett K, Silke B (2011) Increasing wait times predict increasing mortality for emergency medical admissions. Eur J Emerg Med 18:192–196
Conway R;Riordan D, Silke B (2014) Consultant experience as a determinant of outcomes in emergency medical admissions. European Journal of Internal Medicine. doi:https://doi.org/10.1016/j.ejim.2013.12.012, Consultant experience as a determinant of outcomes in emergency medical admissions
Paice E, Reid W (2004) Can training and service survive the European working time directive? Med Educ 38:336–338. https://doi.org/10.1111/j.1365-2929.2004.01834.x
Maybury C (2014) The European working time directive: a decade on. Lancet 384:1562–1563
Rooney T, Moloney ED, Bennett K, O’Riordan D, Silke B (2008) Impact of an acute medical admission unit on hospital mortality: a 5-year prospective study. QJM 101:457–465. https://doi.org/10.1093/qjmed/hcn025
Moore S, Gemmell I, Almond S, Buchan I, Osman I, Glover A, Williams P, Carroll N, Rhodes J (2006) Impact of specialist care on clinical outcomes for medical emergencies. Clinical Medicine (London, England) 6:286–293
Vork JC, Brabrand M, Folkestad L et al (2011) A medical admission unit reduces duration of hospital stay and number of readmissions. Dan Med Bull 58:A4298
Li JY, Yong TY, Bennett DM, O’Brien LT, Roberts S, Hakendorf P, Ben-Tovim DI, Phillips PA, Thompson CH (2010) Outcomes of establishing an acute assessment unit in the general medical service of a tertiary teaching hospital. Med J Aust 192:384–387
St Noble VJ, Davies G, Bell D (2008) Improving continuity of care in an acute medical unit: initial outcomes. QJM 101:529–533. https://doi.org/10.1093/qjmed/hcn042
Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death (1980-2015) a systematic analysis for the Global Burden of Disease Study 2015 (2016). Lancet 388:1459–1544. https://doi.org/10.1016/s0140-6736(16)31012-1
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
This study utilised routinely collected anonymous data and involved no direct patient contact. The requirement for informed consent was waived by the institutional review board.
Rights and permissions
About this article
Cite this article
Conway, R., Byrne, D., Cournane, S. et al. Fifteen-year outcomes of an acute medical admission unit. Ir J Med Sci 187, 1097–1105 (2018). https://doi.org/10.1007/s11845-018-1789-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-018-1789-y