Abstract
Introduction
General practitioners (GPs) require the necessary skills to identify potentially malignant skin lesions and refer patients in an appropriate and timely manner. We examined the impact of a single consultant delivered education session to GP trainees on their diagnosis of common skin lesions.
Methods
A prospective analysis of baseline knowledge was assessed using a photographic questionnaire. A dedicated education session was delivered by a consultant plastic surgeon. Their knowledge was re-assessed after 3 months.
Results
There were 23 participants. Baseline ability to correctly diagnose skin lesions improved significantly at 3 months following dedicated teaching (baseline mean 30.2%, 3-month mean 65.9%, p = 0.001). All trainees recommended that dedicated skin education should be incorporated into GP training curricula.
Conclusion
Dedicated education sessions on skin lesions can improve the diagnostic accuracy of GP trainees, and we suggest that they are incorporated into the GP training curriculum.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dermatological conditions account for 15% of presentations to primary practice [1]. GPs are the ‘gatekeepers’ to tertiary referral. Not only must they have the ability to examine the lesion for features consistent with malignancy, but they must also determine the degree of urgency when a referral is required.
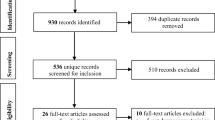
The Health Service Executive (HSE) in Ireland has recently published guidelines on the referral of non-melanoma skin cancers (NMSCs) to add to its existing melanoma referral guidelines (Fig. 1) [2]. With this however, adequate training must be in place for GPs in order for them to identify lesions that require referral.
This study examines the impact of a single dedicated teaching session to current GP trainees, by establishing baseline diagnostic abilities and reassessing at 3 months.
Methods
Standardised pre-op clinical photographs of 40 common skin lesions of patients presenting to a dedicated outpatient were taken by a professional clinical photographer. Photos were taken of typical common skin lesions with classical clinical appearances. Table 1 details each lesion included. In total, 18 lesions were malignant and 22 lesions were benign. Histological confirmation of the diagnosis was recorded post-operatively. Figure 2 is an example of a benign lesion, and Fig. 3 is an example of a malignant lesion included in the study. Patient demographical and clinical details were also collected. Written informed consent was obtained from all patients.
The GP trainees were shown a PowerPoint slide show of each clinical case. Figure 4 is an example of a slide show and the accompanying clinical details. A questionnaire was distributed to 23 independent GP trainees. The GP were undertaking general medical rotations at the time of the study. We asked the trainees to diagnose each lesion, in addition to asking them whether they thought the lesion was benign or malignant. The trainees were also asked whether each lesion should be referred urgently, soon or routinely. All participants were blinded to the actual disease state.
A dedicated interactive education session on common skin pathologies was then delivered to the GP trainees by a consultant plastic surgeon. This lasted for 1 h and consisted of education regarding the clinical appearance of various types of common skin lesions. PowerPoint images of typical lesions were shown to the group during the teaching session. The photos used in the teaching session differed from those used in the questionnaire.
Three months after the education session, a second PowerPoint slide show was shown of the same lesions and the questionnaire was re-administered to the GP trainees, with re-organisation of the sequence of the photograph series. The GP trainees were blinded to their initial assessment.
Statistical analysis was performed using SPSS (SPSS, Inc., Chicago, IL). Diagnostic accuracy, sensitivity, specificity, positive predictive value and negative predictive value were calculated for the GP trainees before and after the education session. Calculations were performed using SPSS version 21.
Results
Twenty-three GP trainees from the Trinity College regional training scheme participated in the study. The mean age was 29 years (range 24–37). No trainee had previous clinical experience in plastic surgery or dermatology. On questioning the trainees’ baseline ability to diagnose skin lesions, 58% of trainees rated their ability as poor, 37% as fair and 5% of trainees rated their ability as moderate. After the education session, all trainees reported that the session was useful and all reported that it should be incorporated into their training curriculum.
Baseline ability to correctly diagnose skin lesions was 30.2% (Table 2). At 3 months, there was a significant improvement in ability to correctly diagnose a skin lesion (p = 0.001). Their ability to differentiate between benign and malignant also improved.
Their ability to correctly identify a benign lesion as benign remained relatively constant (Table 2). Their false benign rate improved after the education session. Their overall ability to identify a malignant lesion also improved. On subgroup analysis of this, their ability to diagnose a malignancy in cases of melanoma improved from 30 to 60%. Unfortunately, their ability to diagnose malignancy in cases of SCC dis-improved from 70 to 61%, hence why the overall improvement was not statistically significant. The false diagnosis of a benign lesion as malignant did not change significantly.
A subgroup analysis of the BCC cases was performed (Table 3). The ability to correctly diagnose a BCC significantly improved from 29.2 to 44.2% (p = 0.016). The ability of the trainees to identify malignancy for the BCC subgroup of cases also improved. Their ability to identify that a lesion that was a BCC required urgent referral improved from 31.2 to 44.4%.
Discussion
Non-melanoma skin cancer is the most common form of cancer. The incidence of skin cancer in Ireland is 178 per 100,000 population per year [3]. With an ageing population, coupled with increasing public awareness, it is likely that this figure will continue to rise. Centralisation of cancer services is leading to growing demands on tertiary referral services [4]. The demand on outpatient plastic surgery and dermatology service can lead to considerable waiting periods; therefore, it is of great importance that patients with suspected malignant lesions are referred appropriately and seen in a timely manner.
Our study showed that a dedicated teaching session, delivered by an expert in the field, can improve GP trainees’ ability to diagnose common skin lesions and identify potentially malignant lesions. The GP trainees had low confidence in their baseline ability to diagnose skin lesions. The capacity of GP trainees to diagnose skin lesions was improved by 36% during the study period. They also improved their ability to identify a malignant lesion by 6.2%. Importantly, their ability to diagnose BCCs improved significantly by 51%, and their ability to identify that the lesion was malignant improved by 33%. The HSE guidelines suggest that SCCs and BCCs should be referred for early tertiary review [2]. Worryingly, at a baseline, 14.2% of BCCs were classified as a routine referral, but this improved to 7.4% after the education session, and reclassification as urgent referrals increased by 13.2%. Importantly, all trainees felt the education session was useful and improved their knowledge of skin lesions.
This study represents an important step towards recognising the need for a dedicated skin core curriculum sessions for GP trainees in Ireland. Simple education interventions may lead to improved triage of patients. The most effective way to train the identification of cancerous lesions is by repetition of clinical photographs [5, 6]. It has been shown in other studies that simple interventions such as visual case-based training of qualified GPs can improve their ability to detect malignancy [7]. If GPs improve their ability to diagnose conditions, a greater number of benign lesions could be managed in primary practice. This would reduce the burden on tertiary outpatient systems and may facilitate earlier review and treatment of malignant lesions. Time to treatment may be reduced for both benign and malignant conditions alike.
Other adjuncts can also be implemented to improve referral patterns of skin lesions. GPs with special interests (GPSIs) are being incorporated into many disciplines to aid tertiary healthcare services [8]. GPSIs in dermatology have been shown to be quite successful, with an improvement in outpatient waiting times, as well as being cost effective [9]. Teledermatology or simply including a photo of the lesion in the referral letter can also be used to improve triage and referral patterns for skin lesions [10, 11].
Distributing guidelines can help improve referral patterns; however, it is not sustainable without adequate ongoing education [12]. We suggest that not only should education on skin lesions be incorporated into the GP training curriculum, but it should also form part of their ongoing training.
Conclusion
Dedicated education sessions on skin lesions can improve the diagnostic accuracy of GP trainees. The ability for GPs to identify common skin lesions and have the confidence to differentiate between benign and malignant conditions may improve referral patterns to tertiary referral centres. Dedicated education sessions should be incorporated into the GP training curriculum, as well as to Continued Medical Education programmes.
References
Basarab T, Munn SE, Jones RR (1996) Diagnostic accuracy and appropriateness of general practitioner referrals to a dermatology out-patient clinic. Br J Dermatol 135(1):70–73
NCCP. National non-melanoma skin cancer GP referral guideline: HSE; 2015 [1:[accessed 18/12/15 2015
NCRI. Cancer in Ireland (2013) Annual report of the National Cancer Registry Cork. In: 2013
Beecher S, O’Leary D, McLaughlin R (2015) Increased risk environment for emergency general surgery in the context of regionalization and specialization. Int J Surg 21:112–114
Burge S (2004) Teaching dermatology. Clin Exp Dermatol 29(2):206–210
Speelman C, Martin K, Flower S, Simpson T (2010) Skill acquisition in skin cancer detection. Percept Mot Skills 110(1):277–297. https://doi.org/10.2466/pms.110.1.277-297 [published Online First: 2010/04/16]
Badertscher N, Braun RP, Held U, et al. Diagnostic competence of Swiss general practitioners in skin cancer. Swiss medical weekly 2013;143:w13834. doi: https://doi.org/10.4414/smw.2013.13834 [published Online First: 2013/07/31]
Beecher SM, Donlan C, O’Leary DP et al (2015) Clinical and economic benefit of general practitioner integration to a symptomatic breast service. Ir J Med Sci. https://doi.org/10.1007/s11845-015-1386-2 [published Online First: 2015/11/26]
Salisbury C, Noble A, Horrocks S et al (2005) Evaluation of a general practitioner with special interest service for dermatology: randomised controlled trial. BMJ (Clin Res ed) 331(7530):1441–1446. https://doi.org/10.1136/bmj.38670.494734.7C [published Online First: 2005/12/08]
Thind CK, Brooker I, Ormerod AD (2011) Teledermatology: a tool for remote supervision of a general practitioner with special interest in dermatology. Clin Exp Dermatol 36(5):489–494. https://doi.org/10.1111/j.1365-2230.2011.04073.x [published Online First: 2011/04/22]
Morton CA, Downie F, Auld S, Smith B, van der Pol M, Baughan P, Wells J, Wootton R (2011) Community photo-triage for skin cancer referrals: an aid to service delivery. Clin Exp Dermatol 36(3):248–254. https://doi.org/10.1111/j.1365-2230.2010.03960.x [published Online First: 2010/11/13]
Hill VA, Wong E, Hart CJ (2000) General practitioner referral guidelines for dermatology: do they improve the quality of referrals? Clin Exp Dermatol 25(5):371–376. https://doi.org/10.1046/j.1365-2230.2000.00665.x
Acknowledgements
Thank you to all the GP trainees who kindly participated in this study. We are grateful to their trainer, Dr. Frank O’Leary, for facilitating the education session. The authors would also like to thank Anthony Edwards, the clinical photographer, for performing the photography.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares that she has no conflict of interest.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Beecher, S.M., Keogh, C. & Healy, C. Dedicated general practitioner education sessions can improve diagnostic capabilities and may have a positive effect on referral patterns for common skin lesions. Ir J Med Sci 187, 959–963 (2018). https://doi.org/10.1007/s11845-018-1788-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-018-1788-z