Abstract
Introduction
Sedation uptake rates for oesophagogastroduodenoscopy (OGD) vary greatly. Issues concerning adequate information and consent have been raised. Additionally, patient comprehension of sedation options is inconsistent.
Methods
A closed ended questionnaire was created and delivered to assess patient understanding regarding sedation prior to OGD. The questionnaire was based on British Society of Gastroenterology guidelines.
Results
One hundred and eleven patients were recruited. 90 % of the sedated and 73 % of the unsedated patients were satisfied with their respective decisions (OR 0.283, *p = 0.01). 65 % were unaware of basic differences between conscious sedation and general anesthesia, and 37 % were unaware that driving is permitted after having throat spray alone. The most informed of the age groups had the lowest uptake of sedation and the least informed had the highest uptake.
Conclusion
The decision to undergo gastroscopy with or without sedation is not a sufficiently informed one. This study highlights the need for the widespread dissemination of good quality information to inform patients better regarding sedation prior to OGD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Due to its ability to reduce anxiety and improve patient tolerance [1], the use of conscious sedation in upper gastro-intestinal endoscopy has resulted in the widespread acceptance for this commonly performed procedure [2]. However, with the administration of sedation there is an added responsibility placed on the endoscopist [3]. Additionally, it slows patient turnover increasing overall healthcare costs and can result in significant complications and morbidities [4, 5]. Reports of fatal cardio-pulmonary complications, though rare, have been reported [6, 7]. Unsurprisingly, with these contrasting attributes sedation uptake rates vary substantially across the world [8].
In recent years, demands placed on endoscopy services have increased significantly. As a result, emphasis has been placed on protocol developments for the use of sedation. A 2001 United Kingdom (UK) study demonstrated a shift towards non-sedation gastroscopy over a 10-year period [9] with the suggestion that eliminating conscious sedation would be beneficial, particularly in terms of patient safety and cost containment [10]. However, an important determining factor in such practices is patient choice. In countries like Ireland the choice to receive sedation often lies with the patient themselves, unless there are substantial clinical reasons to negate its use. This highlights the importance of the informed decision making process. Providing patients with this information in writing prior to invasive procedures is an accepted and common practice in the delivery of healthcare [11]. Yet, inconsistencies in the content and delivery of this information have been identified. A study conducted in Northern Ireland in 2003, showed that despite clear guidelines only one of seven clinical units informed patients that there was a choice between sedation and anesthetic throat spray [11]. Subsequently in 2008, the British Society of Gastroenterology (BSG) guidelines were updated to encourage clearer, more factual and informative Oesophagogastroduodenoscopy (OGD) information leaflets [12]. Despite this, significant differences in content are still noticeable today across the UK and Ireland.
Ultimately, in some instances patients make choices despite lacking relevant information. Therefore, it is reasonable to suggest that patient satisfaction may also be affected in the absence of clear and factual information. Consequently the aim of this study was to evaluate patient understanding as to what sedation entails, assess patient satisfaction with their choice regarding sedation and to determine if possible, the key factors that play a role in this decision making process.
Methods
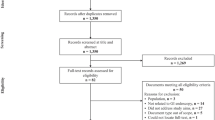
A prospective audit of patients undergoing OGD was performed at a regional district hospital over an 8-week period (November–December 2013). All patients who were having their first ever OGD were asked to participate. As the premise of this study focused on patient choices, any acutely unwell patients who required urgent OGD or those having a colonoscopy on the same day were excluded. All patients included in this study received a comprehensive information leaflet outlining all aspects of the procedure and the option for sedation at the time of booking. All patients included in this study had their OGD performed by one of three surgical consultants to reduce inter-operator variability. Xylocaine® 10 mg/delivery mucosal spray (4 sprays) was administered to all patients prior to OGD.
All patients who agreed to participate were recorded and contacted within 48-h post-procedure via phone-call to complete the survey. The survey included questions relating to patient demographics (age, gender), whether sedation was given, and their post-procedure satisfaction ratings. To assess patient understanding regarding the procedure, seven informative statements were included (“Appendix”). These statements were based on the BSG guidelines [3, 8] and the example BSG information leaflet [12]. Finally, to assess the impact of this information, patients were asked if they would change their decision with regards to sedation if they were to have the procedure again.
To ensure consistency, standardized statements and questions were read to the participant with the same wording on each occasion. Additionally, the same researcher was involved in all phone calls to reduce any variation in wordings and/or explanations. Ethical approval to conduct all aspects of this study was granted by the local research ethics committee. Odds ratio (OR) was calculated using MedCalc® to evaluate satisfaction ratings with and without general sedation. Basic descriptive analysis was performed using Microsoft Excel Software®.
Results
Study demographics
Initially, 113 patients agreed to enroll in this study prior to OGD. However, at the time of phone-call interview 111 patients agreed to participate. 68 patients (61.2 %) were female and 43 patients (38.8 %) were male. 12 % of participants were aged <30 years old, 22 % aged between 30 and 44 years, 32 % aged between 45 and 59 years and 35 % aged 60 years or older.
Sedation versus non-sedation
More than half (56.8 %) of the participants (n = 63) chose to be sedated for OGD. Mean (range) sedation was 4 mg (2–6 mg) of midazolam. The decision to receive sedation was more popular among women in comparison to males (68 vs. 40 %). Additionally, sedation was also more frequently opted for in both the youngest and oldest age cohorts (62 % of under 30 year olds and 77 % of over 60 s). In contrast 57 % of the 45–59 years cohort and only 13 % of the 30–44 years cohort opted for sedation.
Patient satisfaction
The majority of patients (82.8 %, n = 92) stated that they were satisfied with their decision regarding sedation. The association between sedation dose and satisfaction rating was not evaluated. However, on comparing the sub-groups (local anesthetic spray alone and general sedation), there were higher satisfaction rates in those receiving general sedation (90 vs. 73 %, OR 0.283, 95 % CI 0.09–0.81, *p = 0.01) (Fig. 1).
Patient understanding
Interestingly, the largest discrepancy in understanding for both the sedated and non-sedated group was relating to the level of consciousness with sedation. Two-third of patients (n = 36/48) in the non-sedated group were aware that receiving sedation does not put you to sleep, but has amnesic qualities. In contrast, less than half (n = 31/63) of the sedated group was aware of this.
In addition, 81 % of patients stated that they knew that anesthetic spray alone was a viable alternative to sedation. Only a quarter of participants were cognizant that patients can now tolerate OGD without sedation largely due to the endoscopes being narrower, while 63 % understood that when anesthetic throat spray alone was used, they could go home unaccompanied. 72 % were mindful that a delay of approximately 1 h is necessary before eating after local anesthetic spray administration.
On assessing overall awareness, it was observed that the sedated group had a lower average awareness score (55 %) compared with the non-sedated group (65 %). Accordingly, the age groups with the highest uptake of sedation had the least overall awareness: <30 years (56 %), 30–44 years (65 %), 45–59 years (62 %), >59 years (55 %). Conversely, though females had a higher uptake of sedation, their awareness was also higher (62 vs. 56 %).
On further examination of the 30–44 years old age group (least frequent requesters and most knowledgeable age category), we noted that their awareness was particularly high surrounding the role and benefits of anesthetic throat spray. They were especially aware that they could drive home unaccompanied (75 %) and eat within 1 h after receiving it (88 %) (Fig. 2).
Finally, when all participants were asked if they were to have the procedure repeated, 52 % of overall participants stated they would request sedation, down from 57 % who had sedation on this occasion.
Discussion
This study’s appraisal of patient understanding regarding sedation practices for OGD observed that there were three categories more likely to opt for sedation; females, extremes of the age and those patients who were the least informed regarding the types and mechanisms of sedation. Overall elderly patients were the least informed group and the most frequent requesters of sedation. This is quite concerning as this group is the most susceptible to the potential risks surrounding sedation [13]. Additionally, it was noted that those who chose to be sedated had a poorer understanding of the risks of sedation, despite all being provided comprehensive information leaflets at outpatient consultation and procedure booking. One-third of patients were not aware of the limits of sedation and one-fifth did not realize that anesthetic throat spray alone was an alternative to sedation. This highlights that a significant proportion of patients consent to this invasive procedure without thoroughly understanding their options and the risks that accompany them.
This study highlights the need for clearer and more understandable information regarding sedation practices and their associated risks. It also reinforces the fact that sedation must be assessed and tailored on a case-by-case basis [14, 15]. For example, females in our study tended to be more knowledgeable than their male counterparts, but they were also more likely to opt for sedation. This would suggest that comprehension regarding sedation and OGD is not the only factor influencing patient choice and despite its disadvantages, it must be respected that sedation may be the most appropriate option for many patients.
Overall general satisfaction rates amongst participants in this study are similar to those reported in other studies [4]. The provision of information prior to endoscopy has been shown to reduce patient anxiety and improve patient satisfaction, which may be a confounding factor [16]. It is also reasonable to suggest that the amnesic quality of sedation may significantly skewer results to favorable outcomes, and therefore incentivize a shift towards sedated gastroscopy in the future.
Interestingly, after our phone-interview with patients regarding their own experience, we noted that there would be a tendency towards a lower uptake of sedation if the procedure was to be repeated (57–52 %). This may be underestimated as patients may still be influenced from their recent experience. However, evidence suggests that patients retrospectively wish they had been compos mentis immediately after OGD so that they can attain and understand the findings of the procedure and any necessary treatment if required [16].
We acknowledge that this study has some limitations that may impact on the results. The forty-eight delay in contacting patients to assess understanding and satisfaction rates may have affected the results, but we wanted to provide patients time to reflect on their experience. In addition, we accept that sedation with its amnesic qualities may also distort patient satisfaction ratings, and therefore future choices. Finally, future studies are required to highlight if improved pre-procedure information leaflets affect patients choices regarding sedation practices.
Conclusion
Patient understanding of sedation in upper gastrointestinal endoscopy has been shown to be suboptimal. Although those who opt to have sedation have a high post-procedure satisfaction rate, they tend to be in general the least informed. This highlights the need for improved patient education pre-gastroscopy so that a balanced decision can be made. This will overall improve patient safety, understanding and satisfaction.
References
Trevisani L, Sartori S, Gaudenzi P et al (2004) Upper gastrointestinal endoscopy: are preparatory interventions or conscious sedation effective? A randomized trial. World J Gastroenterol 10(22):3313–3317
Aljebreen AM (2010) Unsedated endoscopy: Is it feasible? Saudi J Gastroenterol 4:243–244
Teague R (2003) Guidelines on safety and sedation during endoscopic procedures. The British Society of Gastroenterology (BSG). http://www.bsg.org.uk/clinical-guidelines/endoscopy/guidelines-on-safety-and-sedation-during-endoscopic-procedures.html
Watson JP, Goss C, Phelps G (2011) Audit of sedated versus unsedated gastroscopy: do patients notice a difference? J Qual Clin Pract 21:26–29
Sachdeva A, Bhalla A, Sood A et al (2010) The effect of sedation during upper gastrointestinal endoscopy. Saudi J Gastroenterol 16(4):280–284
Ben-Menachem T, Decker GA, Early DS, ASGE Standards of Practice Committee et al (2012) Adverse events of upper GI endoscopy. Gastrointest Endosc 76(4):707–718
Green J (2006) Complications of gastrointestinal endoscopy. The British Society of Gastroenterology (BSG). http://www.bsg.org.uk/pdf_word_docs/complications.pdf
Ladas SD, Satake Y, Mostafa I et al (2010) Sedation practices for gastrointestinal endoscopy in Europe, North America, Asia, Africa and Australia. Digestion 82:74–76
Mulcahy HE, Hennessy E, Connor P et al (2001) Changing patterns of sedation use for routine out-patient diagnostic gastroscopy between 1989 and 1998. Aliment Pharm Ther 15(2):217–220
Abraham N, Barkun A, Larocque M et al (2002) Predicting which patients can undergo upper endoscopy comfortably without conscious sedation. Gastrointest Endosc 56(2):180–189
Parahoo K, Ridley T, Thompson K et al (2003) A qualitative evaluation of information leaflets for gastroscopy procedure. J Eval Clin Pract. 9(4):423–431
Shepherd H, Hewett D (2008) Guidance for obtaining a valid consent for elective endoscopic procedures. The British Society of Gastroenterology (BSG). http://www.bsg.org.uk/pdf_word_docs/consent08.pdf
Lord DA, Bell GD, Gray A et al (2006) Sedation for gastrointestinal endoscopic procedures in the elderly: getting safer but still not nearly safe enough. The British Society of Gastroenterology (BSG). http://www.bsg.org.uk/clinical-guidance/endoscopy/sedation-for-gastrointestinal-endoscopic-procedures-in-the-elderly-getting-safer-but-still-not-nearly-safe-enough.html
Harewood GC, Clancy K, Engela J et al (2011) Randomised clinical trial: a ‘nudge’ strategy to modify endoscopic sedation practice. Aliment Pharm Ther 34(2):229–234
Ristikankare M, Hartikainen J, Heikkinen M et al (2004) Is routine sedation or topical pharyngeal anesthesia beneficial during upper endoscopy? Gastrointest Endosc 60(5):686–694
Van ZFJ, Grypdonck M, Crevits E et al (2006) The effect of an information brochure on patients undergoing gastrointestinal endoscopy: a randomized controlled study. Patient Educ Couns 64:173–182
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflicts of interest.
Appendix
Appendix
Statement 1 The alternative to sedation is throat spray; this is similar to having your teeth numbed at the dentist. Were you made aware of this at any stage?
Statement 2 Because the scope tubes are now much thinner, the majority of people can manage this procedure with throat spray alone, and 2 out of 3 patients in the UK undergo this procedure without sedation. Were you made aware of this at any stage?
Statement 3 One of the benefits of throat spray is that you can go home unaccompanied almost immediately after the procedure and are permitted to drive. Were you made aware of this at any stage?
Statement 4 The main constraint of throat spray is that you must not eat or drink until the sensation in your mouth has returned to normal, which usually takes about an hour. Were you made aware of this at any stage?
Statement 5 If you have had sedation you must not drive, take alcohol, operate heavy machinery, look after children on our own, or sign any legally binding documents for 24 h following the procedure. Additionally you will need someone to take you home. Were you made aware of this at any stage?
Statement 6 Sedation makes you slightly drowsy and relaxed, but it does not put you to sleep. Additionally you are unlikely to remember anything about the procedure. Were you made aware at any stage?
Statement 7 Had you known the information outlined in the above statements, if you were to have this procedure again would you request sedation?
Rights and permissions
About this article
Cite this article
Quinn, L., Kelly, M.E., Khan, A. et al. Sedation for gastroscopy: Is it an adequately understood and informed choice?. Ir J Med Sci 185, 785–789 (2016). https://doi.org/10.1007/s11845-015-1354-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-015-1354-x