Abstract
Background
We designed, implemented and assessed an interactive musculoskeletal teaching module for fourth-year medical students. Over a 2-week period, students followed a programme of alternating lectures, interactive tutorials, case discussions, clinical examination and ‘how to do’ sessions using patients and clinical models.
Methods
Over a 4-month period, 140 fourth-year medical students rotated for 2 weeks through a new interactive musculoskeletal teaching module in an elective orthopaedic hospital. To assess the impact of our module, a basic-competency examination in musculoskeletal medicine was developed and validated. Each student completed the examination on the first and last days of the module. We also assessed musculoskeletal basic knowledge in students from a different medical school, receiving a classic lecturing programme.
Results
In the pre-course assessment, only 20 % of students achieved an overall pass rate. The pass rate increased to 85 % in post-course examination. Students found particularly beneficial the interactive tutorial approach, with 48 % finding this to be the single most effective teaching method. When compared with students who completed a classic lecturing programme, students attending our interactive module scored higher in all aspects of musculoskeletal knowledge.
Significance
This study highlights the benefits and need for more interactive teaching of musculoskeletal medicine in medical schools.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Musculoskeletal problems rank first as a reason to seek medical care, and they consume a large proportion of medical resources [1]. It has been reported that musculoskeletal conditions constitute 10–28 % of all presentations to general practitioners and emergency departments in North America and Europe [2–8]. It would seem intuitive that all graduating medical students should possess a basic competency in musculoskeletal medicine.
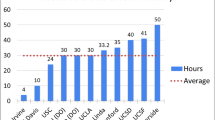
Available evidence suggests however that medical schools fail to deliver adequate musculoskeletal education in the time allocated in undergraduate programs. Undergraduate teaching in core musculoskeletal subjects is under-resourced with inadequate curriculum time allocated to the teaching of musculoskeletal conditions [8, 9]. Less than 50 % of US medical schools require students to undertake a specific preclinical course in musculoskeletal medicine, less than 25 % a clinical course, and almost 50 % have no required pre-clinical or clinical musculoskeletal course. [10, 11]. Comparable figures elsewhere show that only 12 % of Canadian medical schools have mandatory teaching in musculoskeletal medicine [12]. In the UK, time allocated to musculoskeletal education has fallen from 6 to 4 % for the decade 1990–2000. In 1990, Booth and Wise [13] reported that 6 % of undergraduate time in the UK was devoted to musculoskeletal teaching. A study by Williams in 1999 concluded that a mean of 2.7 weeks was spent teaching trauma and orthopaedic education at UK medical schools, representing 2 % of available teaching time [9]. When rheumatology and emergency medicine were included, this accounted for just 4 % of available clinical teaching time. In Canada, just over 2 % of curricular time is spent on musculoskeletal medicine [8].
This provides concrete evidence that musculoskeletal education has been ‘squeezed out’ of many expanding medical school curricula during the 1990s.
Medical students report a lower level of confidence in diagnosing and treating musculoskeletal patients when compared with confidence level in dealing with non-musculoskeletal patients [14]. This prompted an initiative as part of the ‘Bone and Joint’ Decade to “influence the training program in medical schools to include at least 6 months of exposure to musculoskeletal disorders with the aim of improving the diagnostic skills of general practitioners” [15].
At our institution, the interactive musculoskeletal module is a newly designed compulsory clinical rotation delivered in an elective orthopaedic teaching hospital setting over a 2-week period in the first 6 months of intensive clinical attachment (fourth medical year). This recognizes that students will benefit most if they have been taught basic science and have already been exposed to clinical medicine. Various basic science and clinical aspects of musculoskeletal medicine have been taught to our students in the medical school prior to attending our module: anatomy, exercise physiology and physiopathology. Some students were exposed to rheumatology as part of their medical clinical rotation before attending our programme. Students at our medical school start clinical rotations in hospital in their fourth year and, although they may have had formal teaching on history taking and clinical examination, their interaction with the real patients is minimal during their first 3 years of medical education.
The focus of the module is to initiate and enhance students’ knowledge in four main aspects: history taking, clinical examination, diagnosis and treatment of musculoskeletal pathology. Using a previously validated basic-competency examination, we prospectively assessed the efficacy of this new interactive teaching module in musculoskeletal medicine.
Materials and methods
Course development
Our basic teaching strategy was to use different formats to present the core content, following a logical progression from lectures to clinical case presentations and finally to hands-on learning in small group sessions.
Our theory and clinical teaching are student centred and delivered through interactive problem and task-based learning, supported with electronic learning (e-learning) techniques. In problem-based learning, students learn by solving problems derived from real practice, in this context, patient cases. This encourages student participation, ensures variety and maximizes the learning experience for the student. The e-learning aspect is delivered via Moodle (Moodle Trust, Perth, Western Australia), an open course management system familiar to students and also used in the delivery of other undergraduate modules at our institution. All lectures are presented in PowerPoint format (Microsoft Office 2000; Microsoft, Redmond, Washington) and uploaded on the Web via Moodle prior to commencement of the course. In line with the best recommendations, we teach students using practical simulator models, where possible, to help students acquire basic skills in performing procedures (e.g. joint aspiration and injection) [16]. To facilitate these initiatives, students are divided into groups of 20 for attendance at the course at any given time. Two full-time orthopaedic lecturers, a course coordinator and the professor of trauma and orthopaedic surgery, RCSI deliver the module over a 4-month period.
The paradigm in our course is that all medical consultations have two essential components: ‘what the patient says’ and ‘what the doctor says’ (Fig. 1). This doctor–patient encounter model is presented to students during an introductory lecture and it is explained that this case-based approach will be used for all group discussions throughout the module.
Classroom teaching is based on pre-selected classical presentations of common cases from within the hospital. This system ensures systematic rather than opportunistic exposure to clinical presentations, as would be the case if ‘real’ patients were used for all teaching sessions. We focus on teaching the student to elicit the patient’s symptoms through leading questions, ask what signs they would look for on physical examination and to formulate a differential diagnosis. Students are taught to select investigations based on their chosen differential diagnosis. Students are presented with the results of correct investigations and they must provide an interpretation appropriate to the differential diagnosis. The concept of using the information that students know is emphasized. Students are encouraged to examine his or her knowledge (internal) or search other sources (external) such as journal articles, e-learning resources or textbooks to arrive at an answer. Finally, students must suggest what they would say to the patient by way of a basic treatment or management plan, providing a rational explanation for the patient’s presenting symptoms. Arrival at this point completes the ‘journey’ from ‘what the patient says’ to ‘what the doctor says’ using the stepping stones of history, physical examination, investigation and differential diagnosis (Fig. 1). We believe that this method best gives students the confidence and competency ultimately required for a real patient encounter. Students are taught with a bias towards the initial history taking and selection of appropriate clinical examination (‘what the patient says’) side of our model. This ensures that all students can formulate a differential diagnosis for the key presenting musculoskeletal signs and symptoms as a minimum at the end of their course. Cases are selected to trigger elaboration of basic science and musculoskeletal anatomy and pathophysiology within a clinical context. Physical examination is taught by example, using volunteering hospital inpatients, with an emphasis on students recognizing normal from abnormal musculoskeletal signs.
Course structure
Each day of the 2-week programme is allocated to a specific area (Table 1). One day is allocated to trauma and musculoskeletal emergencies. For this, small groups are used rotating through a series of teaching stations, each structured to address a pre-determined competency [17]. Teaching stations include trauma management, cervical spine evaluation and immobilization, and limb immobilization. Two further curricular days are allocated to sports medicine, again with an emphasis on teaching practical skills. Recognizing the multidisciplinary management of musculoskeletal conditions, lectures are also provided on orthotics and prosthetics, and physiotherapy in a collaborative approach with the relevant departments.
After teaching sessions, students have ample time to practice our teaching model at the bedside and work on their skills in history taking, physical examination and formulating a differential diagnosis. They also have an opportunity to attend theatre and outpatient sessions. The taught components of our course are illustrated in Fig. 2.
Our educational efforts are also directed towards initiating and enhancing our students’ proficiencies in constructing and delivering of short PowerPoint presentations on common musculoskeletal conditions. In order to promote team spirit and collaborating attitudes among students, groups of three to four students are given on the first day of their attendance a topic to present at the end of the module in front of their colleagues in a conference format. Confidence and team building are enhanced through use of a mixed, interactive, general and musculoskeletal table quiz during the course. This is delivered in a contest format, with each student from the winning team receiving a prize (under a format of a non-medical book, picture or music CD) from the faculty.
Students are encouraged to suggest areas for improvement as part of the ongoing assessment of the course by both students and lecturers with dynamic adjustment and refinement made in response to criticism and identified deficiencies.
Course assessment
The primary outcomes of the new module were the gains in knowledge, changes in level of confidence and acquisitions of new skills by the students when dealing with the four taught aspects of the course: history taking, clinical examination, diagnosis and treatment of musculoskeletal pathology. Secondary outcomes consisted of student enhancement of inter-personal skills, presentation skills and attitude towards patient, and student preference of teaching method. To assess the above primary and secondary outcomes of the module, a newly designed questionnaire was administered to 140 students attending the new course, both on the first and the last day of the module. We developed our new questionnaire starting from the previously validated basic-competency examination in musculoskeletal medicine developed by Freedman and Bernstein [4] (Table 2). We also validated our new questionnaire by sending it to 20 consultant orthopaedic surgeons and 20 general practitioners, who were asked to rate each question for importance and to suggest a passing score. Each question was weighted based on the average rating. We set the passing rate for our new questionnaire to above 60 %. In addition to assessing knowledge, confidence and acquisition of skills in students dealing with common musculoskeletal problems, we added ten closed questions in our new questionnaire to assess the secondary outcomes of the new module (i.e. improvement of presentation skills, team work, attitude towards the patient and learning expectations).
In our effort to identify the best teaching method for the students, we asked them before and after participation in our module what would be, in their opinion, the most appropriate teaching method: lecture, interactive tutorial, bedside or bedside interactive tutorial.
To compare the efficacy and relevance of this new teaching method with the classic musculoskeletal teaching, we administered our new questionnaire to students in their final year in a different medical teaching institution in Dublin who were attending our hospital for a week’s lecturing program. Lectures were delivered to 2 groups of 60 students at one time for 1 week by orthopaedic consultants and orthopaedic specialist registrars. The questionnaire was administered to the students on their last day of the lecturing programme.
Statistical methods
The mean scores of each group were compared with the use of a two-tailed Student’s t test. Comparisons of multiple means were performed with a one-way analysis of variance. Specific groups were then compared with the use of the Bonferroni multiple-comparisons adjustment. All proportions were compared with the use of the Chi-square test or the Fisher exact test (when indicated). The level of significance was set at 0.05. Statistical analysis was performed with the use of MINITAB, version 13.1 statistical analysis software.
Results
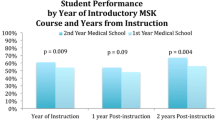
From 140 students enrolled in our module, 120 students completed our pre- and post-course questionnaire. In the pre-course assessment, only 20 % of students achieved an overall pass rate (>60 %) with an average score of 136 out of a maximum of 280. The pass rate increased to 85 % in the post-course examination with the average score increasing to 201 out of 280. The students’ knowledge about musculoskeletal problems in all four areas (history taking, clinical examination, diagnosis and treatment) had increased significantly at the conclusion of the course. The pass rate in the ‘History Taking’ module doubled from 42 to 84 %. The pass rate in the ‘Clinical Examination’ module increased from 7.3 to 63 %, in the ‘Diagnosis’ module from 39 to 79 % and that in the ‘Treatment’ section from 24 to 84 % (Fig. 3).
After completing our interactive module, the majority of students (98/121) felt that the course improved their ability to work in a team for completion of a given project. At the end of the module, the majority of the students (103/121) felt more comfortable giving a presentation on a medical topic to their colleagues or peers and 91 students (75 %) stated that the module improved their presentation skills. Attitude towards patients improved in 71 % (86/121) of the attending students. Most of the students (111/121) found the extracurricular activities (i.e. table quiz, presentations, tasks, etc.) helpful as a learning tool throughout the module.
When asked about the preferred teaching method, prior to attending our module, 46 % of the students believed that seeing patients on the ward would be most beneficial for their learning experience. After experiencing our interactive module, students found the interactive tutorial teaching approach particularly beneficial, with 48 % finding this to be the single most effective teaching method. After completing our module, only 3 % of the students believed that seeing patients on the ward was mostly beneficial (Fig. 4).
A total of 101 (from 120) final year medical students from a different medical school, who received the classical musculoskeletal teaching, the 1-week lecturing programme, responded to our new questionnaire. When compared with the students who were exposed to the two different teaching methods, classic lecturing programme versus interactive module, despite the difference in years, final year versus third year, students who were exposed to our 2-week interactive musculoskeletal module did better in all four aspects. The overall score was higher in students who completed the 2-week interactive musculoskeletal programme (Fig. 3).
Discussion
Educating medical students in musculoskeletal medicine requires an organized programme, conscientious teachers and adequate dedicated curriculum time. Foundation in musculoskeletal knowledge must stem from appropriate medical school teaching. Given the high prevalence of musculoskeletal problems that are encountered in clinical practice, the importance of basic competency in musculoskeletal medicine for all doctors cannot be disputed.
Recently, two other medical teaching institutions in the USA introduced and assessed the impact of a structured musculoskeletal teaching course on preclinical medical students. Both institutions provide evidence that the development of an integrated musculoskeletal curriculum within the medical school curriculum can be an effective way to address the need for newly trained physicians to be knowledgeable about the growing demand and burden of musculoskeletal conditions on society [18, 19].
At our institution, we designed, implemented and evaluated an interactive musculoskeletal module to teach cognitive and process-based skills necessary to achieve an adequate level of competency in musculoskeletal medicine. We did not explicitly seek to test any particular hypothesis.
The module was designed to provide comprehensive training in the basic science and clinical aspects of the musculoskeletal system at an instructional level appropriate to year 4 medical students. Further in their undergraduate training, these students will rotate through clinical divisions of rheumatology, emergency medicine and trauma and orthopaedic surgery. We saw this module as an opportunity to equip the students with basic knowledge and clinical skills when dealing with patients with musculoskeletal problems. The core element of our programme is the patient–doctor encounter model. We structured our module around our course paradigm that all medical consultations have two essential components: ‘what the patient says’ and ‘what the doctor says’. Our main cognitive objective was to teach students to think like physicians and to make them feel comfortable in establishing and managing a doctor–patient relationship. We used our programme as an opportunity to enhance students’ inter-personal skills, presentation and collaborative skills. It was noted by the faculty of this programme from discussion with all students that formal teaching of the above-mentioned skills was not delivered in their previous 3 years of undergraduate medical training.
Assessment of our programme was performed using the basic-competency examination, which is a useful tool for measuring basic cognitive competency in musculoskeletal medicine [18, 20–22]. We modified the existing basic-competency examination by adding ten new closed questions to assess the secondary outcomes of our new module (i.e. improvement of presentation skills, team work, attitude towards the patient and learning expectations).
The reported results of our programme assessment using pre- and post-course questionnaires confirm the positive impact that such interactive musculoskeletal module has on students’ basic musculoskeletal knowledge. When we compared our fourth-year medical students with more senior, final year medical students who received the classic lecture format teaching from a different medical school, we found that the level of knowledge was significantly improved in students who completed our interactive module.
We recognize the weaknesses of our study. The newly designed module is a practical, hands-on programme and assessing students’ performance by MCQ paper alone may not fully cover all the expected learning outcomes. We are considering introducing a short station, clinical-style examination in the future. The significant difference when testing the two groups (Fig. 3) could be explained by the fact that the faculty delivering the interactive module was not blinded to the final assessment questionnaires and therefore could have been biased towards emphasizing the importance of the topics that were tested. The faculty delivering the 1-week lecture programme to the final medical year students in the comparative group was blinded to the topics to be tested by the questionnaire. It could be argued that the achieved levels of cognitive knowledge and clinical skills might not be maintained throughout medical school and that, even if maintained, they might not translate into adequate clinical performance later.
We received very positive feedback from our students on the impact that the interactive module had on the development of their interpersonal skills, presentation and collaborative skills. After completion of our module, the majority of students (over 75 %) found that that the course improved their presentation skills and their ability to work in a team. They felt more comfortable giving a presentation on a medical topic to their colleagues or peers and they considered that their attitude towards patients improved. Most of our students (111/121) found the extracurricular activities (i.e. table quiz, presentations, tasks, etc.) helpful as a learning tool throughout the module. After experiencing our interactive module, students found particularly beneficial the interactive tutorial teaching approach, with 48 % finding this to be the single most effective teaching method. Although prior to starting the course, 46 % of students preferred the bedside teaching, after completing our module only 3 % of students believed that seeing patients on the ward was mostly beneficial (Fig. 4).
Since this study was conducted, we are proud to say that one other medical school (the same school that allowed us to use their final year students as the comparative group for our students) in Ireland started implementation of our interactive module for their year 3 medical students.
Conclusion
We developed, validated and used a basic-competency examination in musculoskeletal medicine to assess the efficacy of a new interactive teaching module in musculoskeletal medicine.
This study shows that an interactive teaching module may be very successful in enhancing basic musculoskeletal knowledge for the medical students.
This study highlights the benefits and need for more interactive teaching of musculoskeletal medicine in medical schools.
References
Yelin E, Herrndorf A, Trupin L, Sonneborn D (2001) A national study of medical care expenditures for musculoskeletal conditions: the impact of health insurance and managed care. Arthritis Rheum 44:1160–1169
Carr AJ, Harnden A (1997) Orthopaedics in primary care. Butterworth-Heinemann, Oxford
De Lorenzo RA, Mayer D, Geehr EC (1990) Analyzing clinical case distributions to improve an emergency medicine clerkship. Ann Emerg Med 19:746–751
Freedman KB, Bernstein J (1998) The adequacy of medical school education in musculoskeletal medicine. J Bone Joint Surg Am 80-A:1421–1427
Kahl LE (1987) Musculoskeletal problems in the family practice setting: guidelines for curriculum design. J Rheumatol 14:811–814
Marsland DW, Wood M, Mayo F (1976) Content of family practice. Part I. Rank order of diagnoses by frequency. Part II. Diagnoses by disease category and age/sex distribution. J Fam Pract 3:37–68
Mulhall KJ, Masterson E (2005) Relating undergraduate musculoskeletal medicine curricula to the needs of modern practice. Ir J Med Sci 174:46–51
Pinney SJ, Regan WD (2001) Educating medical students about musculoskeletal problems. Are community needs reflected in the curricula of Canadian medical schools? J Bone Joint Surg Am 83-A:1317–1320
Williams JR (2000) The teaching of trauma and orthopaedic surgery to the undergraduate in the United Kingdom. J Bone Joint Surg Br 82:627–628
Bernstein J, Alonso DR, DiCaprio M et al (2003) Curricular reform in musculoskeletal medicine: needs, opportunities, and solutions. Clin Orthop Relat Res 415:302–308
DiCaprio MR, Covey A, Bernstein J (2003) Curricular requirements for musculoskeletal medicine in American medical schools. J Bone Joint Surg Am 85-A:565–567
Craton N, Matheson GO (1993) Training and clinical competency in musculoskeletal medicine. Identifying the problem. Sports Med 15:328–337
Booth A, Wise DI (1990) General practice training in musculoskeletal disorders. Br J Gen Pract 40:390
Reznick RK, Brewer ML, Wesley RM, Stauffer ES (1987) Orthopaedic teaching: the practicing family doctor’s perspective. Orthop Rev 16:529–535
Editorial Guest (1998) The Bone and Joint Decade 2000–2010. Acta Orthop Scand 69:219–220
Reznick RK, MacRae H (2006) Teaching surgical skills—changes in the wind. N Engl J Med 355:2664–2669
Hill D, Stalley P, Pennington D et al (1997) Competency-based learning in traumatology. Am J Surg 173:136–140
Bilderback K, Eggerstedt J, Sadasivan KK, Seelig L, Wolf R, Barton S, McCall R, Chesson AL Jr, Marino AA (2008) Design and implementation of a system-based course in musculoskeletal medicine for medical students. J Bone Joint Surg Am 90(10):2292–2300
Day CS, Yu YR, Yeh AC, Newman LR, Arky R, Roberts DH (2009) Musculoskeletal preclinical medical school education: meeting an underserved need. J Bone Joint Surg Am 91(3):733–739
Freedman KB, Bernstein J (2002) Educational deficiencies in musculoskeletal medicine. J Bone Joint Surg Am 84:604–608
Matzkin E, Smith EL, Freccero D, Richardson AB (2005) Adequacy of education in musculoskeletal medicine. J Bone Joint Surg Am 87:310–314
Stockard AR, Allen TW (2006) Competence levels in musculoskeletal medicine: comparison of osteopathic and allopathic medical graduates. J Am Osteopath Assoc 106:350–355
Conflict of interest
All authors state that there is no conflict of interest in the submitted manuscript; there are no financial and personal relationships with other people or organisations that could inappropriately influence (bias) the submitted work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vioreanu, M.H., O’Daly, B.J., Shelly, M.J. et al. Design, implementation and prospective evaluation of a new interactive musculoskeletal module for medical students in Ireland. Ir J Med Sci 182, 191–199 (2013). https://doi.org/10.1007/s11845-012-0855-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-012-0855-0