Abstract
Purpose
Despite the life-threatening character of allogeneic hematopoietic stem cell transplantation (allogeneic HSCT), very few longitudinal research exists on posttraumatic stress disorder (PTSD) symptomatology in this patient group. We investigated prevalence, temporal course and predictors of PTSD symptomatology in this population.
Methods
Patients were assessed before conditioning (T0), 100 days (T1), and 12 months after HSCT (T2). PTSD symptomatology was measured with the PTSD Checklist—Civilian Version. We conducted multilevel modeling and multiple regression analyses.
Results
Two hundred thirty-nine patients participated at baseline, 150 at T1, and 102 at T2. Up to 15 % met the criteria for PTSD at least once during the course of assessment. Fifty-two percent showed diagnostic relevant levels of intrusion, 30 % of avoidance, and 33 % of arousal at least once. Apart from arousal, which increased between T0 and T1 (γ = 0.56, p = 0.03), no other severity score significantly differed between time points. Being impaired by pain (γ = 2.89, p < 0.01), pain level (γ = 0.63, p = 0.02), and being female (γ = 3.81, p < 0.01) emerged as significant predictors of PTSD symptomatology when taking into account all time points. Acute plus chronic graft-versus-host-disease and longer hospital stay predicted PTSD symptomatology at T2 (γ = 3.39, p = 0.04; γ = 0.1, p = 0.03).
Conclusions
A considerable number of patients undergoing allogeneic HSCT met the criteria for PTSD. PTSD symptomatology is prominent at all assessment points. Burden of pain, being female, and medical complications are risk factors for elevated levels of PTSD symptomatology.
Implications for cancer survivors
Psychological support should be offered not only after treatment but also in the long-term and even before HSCT. Professionals should be aware of the psychological consequences accompanied by pain and complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Allogeneic hematopoietic stem cell transplantation (allogeneic HSCT) is the treatment of choice for many hematological diseases [1, 2]. However, it can have wide-ranging adverse consequences: For example, complications such as graft-versus-host-disease (GvHD) or immunosuppressive medication have been found to negatively influence quality of life [3]. More important, even though the treatment is rapidly improving, toxicity and invasiveness still lead to a relatively high mortality rate [2]. As a result, (the anticipation of) undergoing allogeneic HSCT has a high potential of causing severe psychological stress responses [1, 4, 5]. Many patients even exhibit symptoms of posttraumatic stress disorder (PTSD), a syndrome which is characterized by intrusion (re-experiencing the trauma), avoidance (with regard to cues of the traumatic event), and arousal (e.g., sleeping disturbances) [6].
Concerning prevalence rates, previous studies (all cross-sectional) showed that between 5 and 19 % of patients treated with HSCT reached the criteria for PTSD [1, 7–12].
Regarding the temporal course, a longitudinal study among (autologous) HSCT patients showed a significant decline after HSCT of disease-related intrusive thoughts, but not for symptoms of avoidance [13]. Among non-HSCT cancer patients, a study by Voigt et al. [14] found an increase in intrusion and arousal within the first year after diagnosis, but not for avoidance. Another study among non-HSCT patients did not find any significant change in PTSD symptomatology between first assessment and 5-year follow-up [15].
With respect to predictors, gender was shown to be unrelated to PTSD symptomatology among HSCT populations [8, 10, 11], whereas physical functioning was repeatedly shown to be a predictor for PTSD symptomatology [10, 12, 16]. In a study by Hefner et al. [1], neither acute nor chronic GvHD had an effect on PTSD symptomatology. Inconsistent results were found regarding the impact of hospital stay on PTSD symptomatology [11, 12]. The association between pain and PTSD was only discussed among war veterans so far: Tan et al. [17] found that pain intensity and PTSD were not associated with each other, while Asmundson et al. [18] showed a correlation between pain interference (i.e., impairment by pain) and PTSD symptomatology.
To date, two longitudinal PTSD studies among HSCT patients exist [13, 19]. However, only one is prospective [13] and both have a small baseline sample (N = 17 and N = 20). Furthermore, they solely included autologous HSCT patients and therefore could not investigate the impact of specific features of allogeneic HSCT such as GvHD or myeloablative conditioning. The present study combines a prospective design with a relatively large sample among allogeneic HSCT patients and obtained detailed medical and treatment-related variables. Our research questions are as follows:
-
1.
To what extent do patients suffer from PTSD symptomatology?
-
2.
How does PTSD symptomatology change in the course of treatment?
-
3.
What illness- or treatment-related factors predict severity of PTSD symptomatology?
Answering these questions could raise awareness in health care professionals for high-risk patients and help to develop adequate prevention and intervention strategies.
Methods
Sample and procedure
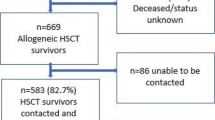
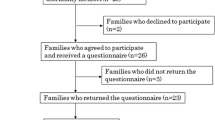
We collected the data within a study on psychological impairments in patients receiving allogeneic HSCT [20]. Participants were recruited from six German university medical centers (i.e., their respective institutions for stem cell and bone marrow transplantation). Patients meeting the inclusion criteria (minimum age of 18, diagnosed with a hematological disease, and scheduled for allogeneic HSCT) were assessed before conditioning (T0), 100 ± 20 days after HSCT (T1) and 12 ± 1 months after HSCT (T2). Data was collected over a 3-year period from June 2, 2005 to July 15, 2008. The research was approved by the local ethics committees or the institutional review boards. Prior to participation, all patients provided written informed consent. For further details about the procedure, see a previous publication [20].
Measures
Medical variables
Physical performance status was assessed by the respective examiner via the Karnofsky Index, a widely used measure for cancer patients which is rated on a ten-percent-step-scale ranging from 0 % (dead) to 100 % (no evidence of disease) [21]. Trained research assistants transferred all illness-, treatment- and complication-related variables from the medical records. The medical records in turn represent the official documents containing all medical data of the patients.
Posttraumatic stress disorder symptomatology
We measured PTSD symptomatology with the Posttraumatic Stress Disorder Checklist—Civilian Version (PCL-C) [22, 23]. This self-report questionnaire contains 17 items that are based on the DSM-IV criteria. Each item can be rated from 1 (not at all) to 5 (extremely). In the validated German version [22], the term event was replaced by cancer or treatment. The PCL-C encompasses the symptom clusters intrusion, avoidance, and arousal. PTSD can be diagnosed in two different ways: According to the symptom-based method, at least 1 intrusion item, 3 avoidance items, and 2 arousal items must be rated as moderately or above (i.e., 3–5). Another way is to sum up all items (range 17–85) and to determine a certain cut-off point above which PTSD is diagnosed (sum score method). For better comparability with previous studies among HSCT patients [1, 7–12], we decided upon a cut-off value of ≥50. In addition, the sum score can be used as a continuous variable that indicates severity of PTSD symptomatology [9].
Pain
We assessed pain experience by using adapted questions based on the Brief Pain Inventory [24]. Patients rated their current pain intensity on a scale from 0 (no pain) to 10 (strongest imaginable pain), their frequency of pain within the last 2 weeks on a scale from 0 (no pain) to 5 (always pain), and their impairment caused by pain on a scale from 0 (no pain) to 5 (very strongly impaired). Moreover, participants specified whether they received any pain medication.
Statistical analyses
We first provided descriptive statistics for all relevant variables. Dropouts were compared to the patients at T2 via t tests (continuous variables) and chi-square tests (binominal variables). Prevalence rates for PTSD were calculated via sum score and symptom-based method. Prevalence rates for each symptom cluster (i.e., intrusion, arousal and avoidance) were determined by the respective diagnostic criteria according to the symptom-based method (for definition see the “Measures” section or Table 2). Severity scores were defined as the sum score across all variables (total value) and across the variables for each symptom cluster. To test for differences between time points and to extract predictors when taking into account all time points, we conducted multilevel modeling (MLM) using random intercept models with time as fixed factor. For extraction of predictors of PTSD symptomatology, we calculated four MLM models with the respective severity score as dependent variables (i.e., total value and the symptom clusters). Independent variables (for definition see Table 1 and the “Measures” section) were pre-structured in hierarchic groups and added to each of the models in the following sequence: socio-demographic (gender, age), previous impacts (pre-diagnosis, whether and what pre-treatment), current status (diagnosis, time since diagnosis), current treatment (conditioning, total body irradiation, matched donor, related donor), physical performance status (Karnofsky Index), and pain (level, frequency, impairment, medication). Variables being significant (p < 0.05) were kept for the next step (i.e., the adding of the next variable group). Only variables that showed significance in all subsequent steps were kept in the four final models. Since variables indicating complications (i.e., GvHD and hospital stay) did not appear until T1, we conducted additional multiple regression analyses at T2 analog to the four multilevel models described above. In each of these regression models at T2, we controlled for the respective predictors extracted via MLM. Whenever independent variables were confounded (e.g., acute GvHD vs. acute plus chronic GvHD), separate models were run. Multinomial and ordinal data was dichotomized (diagnosis: AML vs. others, impairment by pain: impaired vs. not impaired, frequency of pain: less than half of days vs. more than half of days), metric data in MLM was grand-mean centered. Significance levels (two-tailed) were set at p = 0.05. Overall missing data on the PCL-C was relatively low (T0 2–6 %; T1 5–6 %; T2 0–1 %). Concerning descriptive data, only patients who completed more than 50 % of the PCL-C were included, leading to final sample sizes of n = 231 (T0), n = 142 (T1), and 102 (T2). In the regression models, listwise exclusion was used. Analyses were performed by using SPSS [25].
Results
Sample characteristics
Of 394 patients approached, 155 (39 %) did not participate due to not being interested, psychological burden, or physical problems, leading to a response rate of 61 %. The response rates at T1 and T2 were 74 % (30 patients deceased) and 75 % (19 patients deceased), respectively. Finally, 239 patients participated at T0, 150 at T1, and 102 at T2, leading to an overall dropout rate of 57 % (33 % due to death or being too ill). Compared to the patients at T2, dropouts were significantly older, scored worse in physical functioning and pain (level, frequency, and impairment), and were more often treated with TBI in the course of conditioning. Further details about patient enrollment and dropout reasons can be taken from a previous publication [20]. For sample characteristics, see Table 1.
Burden of PTSD symptomatology
Among the 239 participants, between 6 % (sum score method) and 15 % (symptom-based method) met the criteria for PTSD at least once. Fifty-two percent showed diagnostic relevant levels of intrusion, 30 % of avoidance, and 33 % of arousal at least once. Information about severity scores for each time point is shown in Table 2.
Temporal course of PTSD symptomatology
With the exception of intrusion (peak at T0), severity scores peaked at T1 (see Table 2). Apart from severity of arousal, which significantly increased between T0 and T1, no other score significantly differed between time points. The results of the tests for differences between time points can be taken from Table 3.
Predictors of severity of PTSD symptomatology
We firstly extracted significant predictors when taking into account all time points (using MLM). In doing so, pain level, impairment by pain, and gender were shown to be significant predictors for the total value. Impairment by pain was the only variable to predict severity of both the total value and each symptom cluster. For significant predictors for each of the four models (total value, intrusion, avoidance, and arousal) see Table 4.
To test the influence of complication variables (hospital stay and GvHD), we conducted cross-sectional multiple regression analyses at T2. Each model (total value, intrusion, avoidance and arousal) was controlled for the respective predictors in Table 4 and was run twice: One including acute and chronic GvHD as single variables (n = 99) and one including a combined variable, i.e., acute plus chronic GvHD (n = 100).
In the first run, no significance was found for acute and chronic GvHD, whereas hospital stay significantly predicted avoidance (γ = 0.06, SE = 0.02, p = 0.01). In the second run, acute plus chronic GvHD and longer hospital stay significantly predicted severity of the total value (γ GvHD = 3.39, SE = 1.62, p = 0.04; γ hospital stay = 0.1, SE = 0.05, p = 0.03) as well as avoidance (γ GvHD = 1.66, SE = 0.78, p = 0.04; γ hospital stay = 0.06, SE = 0.02, p < 0.01).
Several variables which were predictive when taking into account all time points (in particular pain level and impairment by pain) did not always reach significance in our regression models at T2.
Discussion
Main findings
In the course of assessment, almost every sixth patient met the criteria for PTSD at least once. PTSD symptomatology was prominent at all assessment points. Patients who were female, bothered by different aspects of pain, or suffering from medical complications were at high risk for elevated levels of PTSD symptomatology.
Comparison with previous research
Our study is one of the few PTSD studies exclusively focusing on allogenic HSCT patients and, to our knowledge, the first longitudinal study in this specific population. Cross-sectional studies assessed PTSD symptomatology post-HSCT and did not take into account pre-HSCT levels. Furthermore, the wide ranges regarding time since HSCT among and between study samples are supposed to influence descriptive and inferential results.
Given the novelty of our study design, comparability with previous research is limited. Nevertheless, looking at our prevalence rates 100 days and 1 year after HSCT, symptom-based prevalence largely corresponded with results from previous studies among HSCT patients, whereas sum score-based prevalence was slightly lower [1, 7–12]. Given the methodological advantages of our study, our prevalence rates and severity scores provide important information about allogeneic HSCT patients before and up to 1 year after transplantation.
The increase in arousal between pre-HSCT and post-HSCT illustrates the stressful effect of undergoing the transplantation process. However, it has to be noted that many arousal items could also be explained as physical side effects of HSCT and immune suppressive medication [26–28]. As a result, this increase could be partly explained by physical reactions. Our finding that no other score significantly differed between pre- and post-HSCT fits to assumptions that PTSD is not caused by the transplantation itself [7, 19]. Concerning the high levels of PTSD symptomatology before HSCT, two explanations are possible: First, it has been suggested that in the course of cancer, ruminating about events in the future might serve as a traumatic experience [29, 30]. Following that assumption, it was the process of attending HSCT which caused the elevated levels pre-HSCT. Second, as 80 % of patients underwent any pre-treatment, it is also possible that the elevated PTSD symptomatology before HSCT is a reaction to an enduring, psychologically, and physically distressing episode. Since intrusion (i.e., imagination of the trauma) peaked before HSCT, we conclude the first hypothesis to be more adequate.
In contrast to previous studies [8, 10, 11], gender (being female) was found to be an important predictor of PTSD symptomatology. Our finding, however, is very reasonable as it fits to studies among the general population that identify women as having a higher risk to develop PTSD after a traumatic event [31]. Physical performance did not predict PTSD symptomatology, which also contradicts all previous results [10, 12, 16]. Looking at the measures, this discrepancy could be explained by different assessment (Karnofsky Index in our study vs. SF-36 in the other studies). As shown by Asmundson et al. [18], impairment by pain were found to be an important predictor in our study. The predictive importance of pain intensity, however, contrasts with the study by Tan et al. [17], which could not show such an association. Since both cited studies investigated war veterans, our study provide first results regarding this relationship among HSCT patients, which needs to be further validated. Longer hospital stay predicted the severity of PTSD symptomatology, corresponding with a study by Jacobsen et al. [12], but contrasting with results of Widows et al. [11]. In light of very similar methods across the three studies, further research is needed to investigate these inconsistencies. Similarly to Hefner et al. [1], we found no effect for acute and chronic GvHD as single variables. However, combining both GvHD types led to a significant effect. This in turn indicates that the physiologically independent types of GvHD accumulate with regard to psychological strain.
Limitations
Given that dropouts and patients with missing data scored significant lower in physical functioning, there might be a sample bias towards the physically better functioning patients. This in turn could have resulted in underestimating PTSD symptomatology. As conditioning regimes and the indication for HSCT is changing rapidly, generalizability is also reduced by the fact that our data collection dates back to 2008.
Predictors were selected in a hierarchical/stepwise procedure and only significant predictors were left in the final models. This selection process could have missed potentially moderating effects of non-significant variables. However, in light of scarceness and inconsistencies of previous research, this exploratory approach seemed most appropriate as it enabled us to test for many potential predictors. Furthermore, dividing our selection in two parts (MLM when taking into account all time points and multiple regression analyses at T2) might seem cumbersome, but was chosen in order to both extract time robust predictors and test for important variables that developed at later time points.
With respect to assessment, the PCL-C is a self-rated questionnaire with all its inherent methodologic disadvantages [29]. Therefore, the PCL-C should only serve as a screening tool and cannot provide definite PTSD prevalence rates [10]. Moreover, an established cut-off value for the sum score based prevalence method is still lacking [29]. For better comparability with all previous HSCT studies, we used a cut-off of ≥50. Choosing the cut-off on the basis of the goal of the study and the expected prevalence [32], it would have been about 30. Together with the fact that symptom-based prevalence was up to four times higher than the sum score method, we suggest to downgrade the cut-off value in future HSCT studies. By adapting the questionnaire for cancer patients (i.e., replacement of the term event by cancer or treatment), it could not specify the exact content and time point of the potentially traumatic event. Furthermore, our study used the PCL-C version in accordance with the DSM-IV, which has, in the meantime, been replaced by the PCL-5 according to the DSM-5 [32].
Finally, we did not assess disease risk, which is supposed to play an important role in the development of PTSD symptomatology.
Further research
Further research should focus on improving assessment of PTSD symptomatology and controlling for confounding variables. PTSD symptomatology should be differentiated from other (neuro-) psychological symptoms that go along with disease and treatment, e.g., irritability or fear of a realistic danger [4, 27, 29]. History of traumatic events [33–34] as well as premorbid personality [11, 35] were shown to be strongly associated with stress responses and, therefore, should be assessed in future research. Since we hypothesized that the wide range concerning time since HSCT could be partly responsible for inconsistent results, this variable should be better controlled in further studies.
Conclusions and practical implications
PTSD symptomatology was prominent at all assessment points. Therefore, psychological support should not only be offered in the acute phase, but already before HSCT and in the long-term. Impairment by pain and pain intensity were risk factors for elevated levels of PTSD symptomatology. This highlights the importance of informing patients early enough that pain might occur and to teach techniques for dealing with it. Since medical complications predicted severity of PTSD symptomatology 1 year after HSCT, medical professionals should be aware of psychological strain among patients suffering from long-term medical complications.
References
Hefner J, Kapp M, Drebinger K, et al. High prevalence of distress in patients after allogeneic hematopoietic SCT: fear of progression is associated with a younger age. Bone Marrow Transplant. 2014;49:581–4.
Copelan EA. Hematopoietic stem-cell transplantation. N Engl J Med. 2006;354:1813–26.
Kurosawa S, Yamaguchi T, Mori T, et al. Patient-reported quality of life after allogeneic hematopoietic cell transplantation or chemotherapy for acute leukemia. Bone Marrow Transplant. 2015;50:1241–9.
Mosher CE, Redd WH, Rini CM, Burkhalter JE, DuHamel KN. Physical, psychological, and social sequelae following hematopoietic stem cell transplantation: a review of the literature. Psychooncology. 2009;18:113–27.
Cooke L, Gemmill R, Kravits K, Grant M. Psychological issues of stem cell transplant. Semin Oncol Nurs. 2009;25:139–50.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. DSM-IV. 4th ed. Washington, DC: American Psychiatric Association; 1994.
Lee SJ, Loberiza FR, Antin JH, et al. Routine screening for psychosocial distress following hematopoietic stem cell transplantation. Bone Marrow Transplant. 2005;35:77–83.
DuHamel KN, Ostrof J, Ashman T, et al. Construct validity of the posttraumatic stress disorder checklist in cancer survivors: analyses based on two samples. Psychol Assess. 2004;16:255–66.
Jacobsen PB, Sadler IJ, Booth-Jones M, Soety E, Weitzner MA, Fields KK. Predictors of posttraumatic stress disorder symptomatology following bone marrow transplantation for cancer. J Consult Clin Psychol. 2002;70:235–40.
Smith MY, Redd W, DuHamel K, Vickberg SJ, Ricketts P. Validation of the PTSD checklist—civilian version in survivors of bone marrow transplantation. J Trauma Stress. 1999;12:485–99.
Widows MR, Jacobsen PB, Fields KK. Relation of psychological vulnerability factors to posttraumatic stress disorder symptomatology in bone marrow transplant recipients. Psychosom Med. 2000;62:873–82.
Jacobsen PB, Widows MR, Hann DM, Andrykowski MA, Kronish LE, Fields KK. Posttraumatic stress disorder symptoms after bone marrow transplantation for breast cancer. Psychosom Med. 1998;60:366–71.
Wettergren L, Langius A, Bjorkholm M, Bjorvell H. Post-traumatic stress symptoms in patients undergoing autologous stem cell transplantation. Acta Oncol. 1999;38:475–80.
Voigt V, Neufeld F, Kaste J, et al. Clinically assessed posttraumatic stress in patients with breast cancer during the first year after diagnosis in the prospective, longitudinal, controlled COGNICARES study. Psychooncology. 2016.
Smith SK, Zimmerman S, Williams CS, et al. Post-traumatic stress symptoms in long-term non-Hodgkin’s lymphoma survivors: does time heal? J Clin Oncol. 2011;29:4526–33.
DuHamel KN, Smith MY, Vickberg SM, et al. Trauma symptoms in bone marrow transplant survivors: the role of nonmedical life events. J Trauma Stress. 2001;14:95–113.
Tan G, Fink B, Dao TK, et al. Associations among pain, PTSD, mTBI, and heart rate variability in veterans of Operation Enduring and Iraqi Freedom: a pilot study. Pain Med. 2009;10:1237–45.
Asmundson GJ, Wright KD, Stein MB. Pain and PTSD symptoms in female veterans. Eur J Pain. 2004;8:345–50.
Mundy E, Blanchard E, Cirenza E, Gargiulo J, Maloy B, Blanchard C. Posttraumatic stress disorder in breast cancer patients following autologous bone marrow transplantation or conventional cancer treatments. Behav Res Ther. 2000;38:1015–27.
Scherwath A, Schirmer L, Kruse M, et al. Cognitive functioning in allogeneic hematopoietic stem cell transplantation recipients and its medical correlates: a prospective multicenter study. Psychooncology. 2013;22:1509–16.
Buccheri G, Ferrigno D, Tamburini M. Karnofsky and ECOG performance status scoring in lung cancer: a prospective, longitudinal study of 536 patients from a single institution. Eur J Cancer. 1996;32:1135–41.
Höcker A, Mehnert A. Posttraumatische Belastung bei Krebspatienten: Validierung der deutschen Version der Posttraumatic Stress Disorder Checklist–Civilian Version (PCL-C). Z Med Psychol. 2012;68:79.
Weathers FW, Huska JA, Keane TM. PCL-C for DSM-IV. Boston: National Center for PTSD – Behavioral Science Division; 1991.
Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singap. 1994;23:129–38.
IBM Corporation. SPSS statistics for windows. Armonk, NY: IBM Corporation; 2011.
Andrykowski MA, Bishop MM, Hahn EA, et al. Long-term health-related quality of life, growth, and spiritual well-being after hematopoietic stem-cell transplantation. J Clin Oncol. 2005;23:599–608.
Silberfarb PM, Oxman TE. The effects of cancer therapies on the central nervous system. Adv Psychosom Med. 1988;18:13.
Diez-Campelo M, Perez-Simon JA, Gonzalez-Porras JR, et al. Quality of life assessment in patients undergoing reduced intensity conditioning allogeneic as compared to autologous transplantation: results of a prospective study. Bone Marrow Transplant. 2004;34:729–38.
Gurevich M, Devins GM, Rodin GM. Stress response syndromes and cancer: conceptual and assessment issues. Psychosomatics. 2002;43:259–81.
Mehnert A, Berg P, Henrich G, Herschbach P. Fear of cancer progression and cancer-related intrusive cognitions in breast cancer survivors. Psychooncology. 2009;18:1273–80.
Breslau N. Gender differences in trauma and posttraumatic stress disorder. J Gend Specif Med. 2002;5:34–40.
National Center for PTSD. Using the PTSD Checklist for DSM-IV(PCL). 2014. http://www.ptsd.va.gov/professional/pages/assessments/assessment-pdf/PCL-handout.pdf. Accessed 30 Nov 2015.
Yehuda R, Kahana B, Schmeidler J, Southwick SM, Wilson S, Giller EL. Impact of cumulative lifetime trauma and recent stress on current posttraumatic stress disorder symptoms in holocaust survivors. Am J Psychiatry. 1995;152:1815–8.
Breslau N, Chilcoat HD, Kessler RC, Davis GC. Previous exposure to trauma and PTSD effects of subsequent trauma: results from the Detroit Area Survey of Trauma. Am J Psychiatry. 1999;156:902–7.
Tjemsland L, Søreide JA, Malt UF. Posttraumatic distress symptoms in operable breast cancer III. Breast Cancer Res Treat. 1998;47:141–51.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The research was approved by the local ethics committees or the institutional review boards. Prior to participation, all patients provided written informed consent.
Funding
This study was funded by the José Carreras Leukämie-Stiftung e.V. (grant nos. DJCLS R 04/29pf and DJCLS R 07/37pf).
Conflict of interest
The funding source was not involved in any stage of the research process. The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Esser, P., Kuba, K., Scherwath, A. et al. Posttraumatic stress disorder symptomatology in the course of allogeneic HSCT: a prospective study. J Cancer Surviv 11, 203–210 (2017). https://doi.org/10.1007/s11764-016-0579-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-016-0579-7