Abstract
Background
While most children with cancer survive their initial disease, cancer therapy places them at risk for late effects (LE). Knowledge of their diagnosis, treatment, and LE risk may motivate survivors to attend long-term follow-up care. The aims of this study were to examine knowledge of cancer history and future risks, and to identify factors associated with such knowledge, in a cohort of childhood cancer survivors.
Methods
Survivors (i.e., patients finished cancer treatment, regardless of time since completion) aged 15 to 26 years from three Canadian cancer centers were invited to complete a questionnaire that assessed knowledge of cancer history and potential LE of treatments, including five specific LE known to have considerable long-term health impact. Clinical data were extracted from hospital records and used to validate participants’ answers.
Results
Of 250 participants, 16 (6 %) were unable to name their cancer, 79 (32 %) had partial or no knowledge of their therapy, and 83 (33 %) were unaware of at least some of their risks for LE. Decreasing age (OR for increase in age = 1.2 (1.1–1.4)), having had a renal tumor compared to leukemia (OR = 0.3 (0.1–0.9)), and lacking knowledge about treatment (OR = 0.4 (0.2–0.9)) were associated with lack of knowledge of LE. Of the five, the most and least familiar LE was LE associated with impaired pulmonary function and risk of second malignancy, respectively.
Conclusion
This study highlights knowledge deficits in survivors, specifically regarding their risk for LE.
Implications for Cancer Survivors
Findings can be utilized to target survivors at risk for knowledge deficits.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
From 1975 to 2006, the 5-year overall survival rate for pediatric cancer patients increased from 59 to 85 % [1], primarily due to increases in cancer treatment intensity and better supportive care. Unfortunately, these survival improvements have been accompanied by risk of long-term health-related complications in survivors, which has had an impact on outcomes such as health status [2], morbidity [3, 4], and mortality [5]. Survivors of childhood cancer have been shown to be at increased risk for developing chronic health conditions or late effects (LE) that affect pulmonary, auditory, reproductive, cardiac, and neurocognitive functions, among others [4]. In addition, survivors have been shown to have an overall eleven-fold increase in mortality rates compared to the general United State (US) population [5], with second malignant neoplasms and cardiac and pulmonary disease being the largest contributors to non-relapse-related mortality.
Given the detrimental effects of cancer treatment, long-term follow-up (LTFU) care by a knowledgeable health care provider has been recommended for survivors of cancer in childhood and adolescence in order to monitor and prevent occurrence of LE and to provide psychosocial support and cancer education [6, 7]. However, many childhood cancer survivors drop out of LTFU care as they get older [8]. Non-attendance in LTFU has been associated with multiple patient, provider, and health system issues, but lack of survivor knowledge regarding their cancer history and risk for LE has been shown to be a substantial barrier to seeking appropriate LTFU care [7, 9, 10].
Although several studies have identified important knowledge deficits in childhood cancer survivors regarding diagnosis and treatment history [11–14], there is a paucity of literature about survivors’ knowledge of their specific risks for LE. A study by Hudson et al. [15] assessed knowledge of cancer treatment history and late effects. This study represented health knowledge as a composite score, but did not present the findings for specific LE, especially those prevalent among childhood cancer survivors. Also, the study did not evaluate factors associated with knowledge. As such, there is little known about childhood and adolescent cancer survivors’ awareness of the most commonly occurring LE and factors associated with such knowledge.
The aims of this study were to examine the extent of knowledge regarding diagnosis, treatment, and LE, including five specific LE that have been shown to have considerable impact on survivors long-term health and quality of life (i.e., second malignancy, pulmonary, cardiac, reproductive, and neurocognitive dysfunction) and to identify factors associated with lack of such knowledge in childhood and adolescent cancer survivors.
Methods
The analysis was a component of a larger study to understand barriers and facilitators experienced by survivors as they transition from pediatric to adult LTFU care [16, 17]. In the larger study, qualitative interviews were conducted with childhood cancer survivors to identify barriers and facilitators to transition. The analysis of transcript data led to the identification of three primary constructs for which scales were subsequently developed, namely cancer worry, self-management skills, and expectation about adult LTFU care [16, 17]. In order to assess cancer-related knowledge, a set of 13 items (see Box 1) with accompanying open-ended questions (see Box 2) were developed by the research team and included in a questionnaire booklet along with the three scales. Subsequently, a field test was undertaken to validate these scales, with the results described in detail elsewhere [17]. Research ethics board approval was obtained from participating centers prior to the start of the study.
Box 1 Scale

Box 2 – Selected open-ended questions from the survey


Recruitment of childhood cancer survivors to assess knowledge occurred between July 2011 and January 2012 from children’s hospitals located in Hamilton, Toronto, and Vancouver. Except for minor differences, LTFU care is delivered in a similar manner at all three centers. In Toronto and Hamilton, pediatric cancer survivors are generally transferred to LTFU care at the later of 2 years from completion of therapy and 4 years from diagnosis. In Toronto, survivors are transitioned to an adult LTFU program at a separate regional cancer center at age 18 years, while patients in Hamilton remain in the same clinic for life. In Vancouver, all patients who complete treatment are transferred to LTFU care approximately 6 months after completion of treatment. Patients considered to be at low to moderate risk for LE remain in the clinic until age 25 years when they are transitioned to a family physician. In contrast, survivors at high risk for LE are transferred to an adult cancer center between ages 18 and 21 years. At all centers, survivors are usually seen once per year. Attendance at LTFU clinics is generally excellent prior to age 18 years. However, some young adults are lost to follow-up, particularly if they move away for school or employment. At all centers, survivors receive a treatment summary and counseling from a physician or nurse practitioner based on the Children’s Oncology Group Long-term Follow-up Guidelines. All patients receive annual counseling about their exposures, risk for LE, and surveillance and lifestyle modifications required to optimize their health.
Survivors were defined as patients who had completed treatment for their cancer and were attending a LTFU care clinic at the time of recruitment. There were no limitations on the length of time survivors could be off treatment. Inclusion criteria were survivors currently aged between 15 and 26 years who had been diagnosed with cancer before 18 years of age. We excluded survivors with a neurocognitive disability that would prevent independent completion of the questionnaire. Survivors who agreed to participate were asked to sign consent or assent forms as appropriate.
Participants were recruited in-person at hospital clinics and by mail. For clinic recruitment, patients were approached by a research assistant (RA) prior to their appointment and invited to participate. Patients not scheduled for a clinic visit during the recruitment period were included in a postal survey. To maximize the response rate, up to three reminders were sent to potential participants as needed, spaced 2 to 3 weeks apart. All potential participants were given a five-dollar gift card to thank them for considering the study.
In addition to the survey, a chart review was performed to collect clinical information on diagnosis and treatment. One RA conducted the chart extraction, and a second RA checked the extracted data for accuracy. These data were considered the “gold standard” and used to compare with the self-report answers provided in the questionnaire. Finally, information about non-respondents (age, gender, age at diagnosis, and cancer type) was extracted from the charts to determine response bias.
Dependent variables
Cancer knowledge of diagnosis, treatment, and LE were determined by comparing participant responses from the respective open-ended questions (Box 2) to the information available from hospital records.
For knowledge of diagnosis, all those who correctly identified major type of cancer (e.g., leukemia) and/or correctly identified sub-type of cancer (e.g., acute lymphoblastic leukemia—ALL) were categorized as “knowledgeable”. Those who incorrectly identified major type of cancer and/or sub-type of cancer or left the question blank were categorized as “not knowledgeable”.
Knowledge of four cancer treatment options (i.e., chemotherapy, radiation therapy, surgery and transplant) was also determined. Participants who correctly identified whether or not they received all four treatments, three of four treatments, and less than three of four treatments were categorized as “knowledgeable”, “partially knowledgeable,” and “not knowledgeable”, respectively. We also specifically looked at knowledge of exposure to anthracycline in survivors who had received this chemotherapy drug according to their hospital records. In this sub-group, those who listed anthracycline agent for Box 2-question 3 were considered “knowledgeable”.
Knowledge of LE was assessed in two ways: overall knowledge of potential LE and knowledge of five specific LE with known long-term health impact. For overall knowledge of LE, an ordinal measurement, diagnosis, and treatment history for each participant was reviewed by an LE expert (PN) and assessed against participant’s response (Box 2-question 4). Those who correctly identified that they were not at risk for any LE or only listed LE for which they were at risk were deemed “knowledgeable”. It was not important for participants to have listed all LE for which they were at risk to be considered “knowledgeable”. Participants were categorized as “partially knowledgeable” if they correctly listed one or more LE, but also incorrectly listed LE for which they were not at risk. Moreover, participants were considered “not knowledgeable” if they failed to list any LE when they were at risk or listed LE when they were not at risk. For analysis of each of the five specific LE, participants “at risk” for the specific LE were considered “knowledgeable” if they had listed that LE in Box 2-question 4, and “not knowledgeable” if they did not. Conversely, participants “not at risk” were “knowledgeable” if they did not list the specific LE, but were considered “not knowledgeable” if they did list the specific LE.
Independent variables
Selection of independent variables was based on previous studies in this area of research and expert feedback. Patient factors included current age, gender, and race. Family factors included mother’s and father’s highest level of education and marital status. Cancer-related factors including age at diagnosis, diagnostic era (dichotomized at midpoint), and type of cancer were extracted from hospital records. Cancer type was categorized according to the International Classification of Childhood Cancer (ICCC) [18]. Treatment factors were obtained from hospital records, including receipt of chemotherapy, surgery, and transplant, site of radiation therapy, and relapse status. Treatment variables were used to categorize treatment intensity using the intensity treatment rating scale 2.0 (ITR-2) [19]. The scale ranges from one to four, with four being most intensive.
The cancer worry scale [17] was also included. This six-item scale measures thoughts and feelings related to cancer and LE (e.g., I worry about my cancer every day; I worry my cancer will come back). For each item, four options were provided, ranging from “strongly disagree” to “strongly agree”. Scores ranged from 0 to 100 and lower scores indicated more cancer worry.
In order to determine whether knowledge of cancer treatment could impact knowledge of LE, “Knowledge of treatment”, as categorized in this study, was used as an independent variable of interest. This was included as a factor for the multivariable analysis of factors associated with knowledge of LE.
Control variables
Since the sample size varied by center, and response rate by method of recruitment, we included these variables in the analysis.
Analysis
To address the first objective, the number and percentage of participants knowledgeable about their diagnosis, treatment, and overall LE were calculated. Additionally, logistic regression models were used to address the second objective, which was to identify factors associated with cancer knowledge regarding diagnosis, treatment, and LE. A step-wise approach was undertaken to identify variables associated with cancer knowledge. First, univariable logistic regressions were conducted to screen for potential associations between dependent and independent variables. Variables significantly related to cancer knowledge in the univariable analysis were included in multivariable logistic regressions alongside the two control variables. An odds ratio of greater than one indicated more knowledge. For factors associated with specific LE in the “at risk” population, only univariable analyses were conducted as exploratory analysis to identify potential associations. An odds ratio of greater than one indicated less knowledge.
A binary logistic regression was conducted for dichotomous dependent variables, whereas ordinal logistic regression was conducted for ordinal dependent variables. Regression models were tested for fit and assumptions by conducting Pearson’s goodness-of-fit or Hosmer-Lameshow tests and test of parallel lines, respectively. SPSS Statistics 20 ® was used to perform all analyses. Significance level was set to 0.05 for two-sided tests. For logistic regressions, odds ratio (OR) and 95 % confidence intervals (CI) were reported where appropriate. Multiple imputations [20] were used to deal with the missing data.
Results
Of 331 patients invited to participate, 250 (75.5 %) agreed and completed the questionnaire. The response rate was significantly higher for clinic (1114/118 = 96.6 %) versus mail (136/213 = 63.8 %) recruitment (p < 0.01). Non-respondents were younger than respondents (p < 0.01), but did not differ in terms of age at diagnosis, gender, and type of cancer. Table 1 shows sample characteristics. The sample included more males (54.0 %) than females; the average age was 18.1 years (median = 17.0; interquartile range = 16 to 20), with the majority of participants aged between 15 and 17 years (53.6 %).
Knowledge of diagnosis, treatment, and LE
Of 250 participants, 234 (93.6 %) were “knowledgeable” and 16 (6.4 %) were “not knowledgeable” about their diagnosis. Of 244 participants who indicated responses for all four types of treatment, 165 (67.6 %) were “knowledgeable”, 54 (22.1 %) were “partially knowledgeable,” and 25 (10.3 %) were “not knowledgeable” about their treatment. Additionally, the following number of participants correctly identified whether they had received these specific types of treatment: chemotherapy—240 of 250 (96.0 %), radiation therapy—217 of 248 (87.5 %), surgery—213 of 249 (85.5 %), and transplant—206 of 249 (82.7 %). Out of 249 participants who had associated information in their charts, only 20 (8.0 %) had a transplant, as part of their cancer treatment, and all were “knowledgeable” about having received this modality. Out of 191 participants who received anthracycline(s), 144 (75.4 %) were “not knowledgeable” of having received this drug. Of 248 participants who had sufficient information in their charts for ascertaining the risk of late effects, 134 (54.0 %) were “knowledgeable”, 31 (12.5 %) were “partially knowledgeable” and 83 (33.5 %) were “not knowledgeable” about their risk for overall LE.
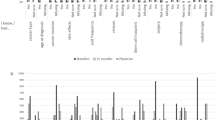
Table 2 reports the number and proportion of patients “knowledgeable” and “not knowledgeable”, stratified by risk status, of the five specific LE considered in this study.
Factors associated with knowledge
Since only 16 out of 250 participants did not know their diagnosis, an insufficient number of cases to conduct multivariable analysis [21], we could not assess the factors associated with this lack of knowledge. Table 3 presents results from the univariable and multivariable analyses for knowledge of treatment and LE. In the multivariable model for knowledge of treatment, “white” cancer survivors compared to “non-white” (OR = 2.7; 95 % CI = 1.5–5.0) and those who received radiation therapy to sites other than the head and neck compared to those who did not receive radiation therapy (OR = 2.5; 95 % CI = 1.02–6.0), were found to have higher knowledge regarding their cancer treatment. In the multivariable model for knowledge of LE, younger survivors (OR as coded for increasing age = 1.2; 95 % CI = 1.1–1.4), renal cancer survivors (OR = 0.3; 95 % CI = 0.1–0.9) compared to leukemia survivors, and those who were “not knowledgeable” (OR = 0.4; 95 % CI = 0.2–0.9) of their treatment compared to “knowledgeable” were found to lack knowledge regarding their risk for LE. Table 4 presents results from the univariable analyses for knowledge of specific LE in those at risk for that LE.
Discussion
Putting study findings in context
This study revealed that most survivors knew their cancer diagnosis (94 %) and the vast majority was aware of whether or not they had received chemotherapy, radiation therapy, surgery, and transplant. We found a lack of knowledge regarding the receipt of anthracyclines, with 75 % of participants not able to name an anthracycline agent when asked to write names of chemotherapy drugs they had received. It is important to note that participants were not specifically probed for information about anthracycline agents per se, but rather to name any chemotherapy drug they had received. A previous study by Kadan-Lottick et al. [14] reports similar findings when participants were not probed specifically for anthracyclines. However, knowledge of whether the participants had received doxorubicin or daunorubicin and anthracycline agents increased when prompted for these drugs.
Our study revealed important knowledge deficits regarding LE. Almost half of the participants either did not list a LE for which they were at risk or they listed a LE for which they were not at risk. Lack of knowledge regarding LE was more common in participants who were younger, had a renal tumor, and lacked knowledge about the cancer treatments they received.
Among the five specific LE explored in this study, participants were most familiar with their risk of LE associated with pulmonary function, but the majority of participants lacked knowledge about their risk status for second malignancy (55 %). Furthermore, almost all of those (99 %) who lacked such knowledge were in fact at risk for this LE. In those at risk of second malignancy, younger age at diagnosis was associated with lack of knowledge.
It is recommended that childhood cancer survivors at risk for LE be screened for potential risks to reduce the impact of cancer treatment on long-term health [22]. However, studies looking at surveillance practices in survivors of childhood cancer reported low rates of screening for second malignancies, despite recommendations by current guidelines. A study looking at adherence to surveillance guidelines by low- and high-risk survivors for second malignancies reported low rates of mammography (46 %) in women at high risk for breast cancer and low rates of colonoscopy (11 %) and skin examination (27 %) among both men and women at high risk for colorectal and skin cancer, respectively [23]. Another study looking at breast cancer screening practices among female survivors of childhood cancer who received chest radiation showed lack of screening mammograms, especially in younger subjects; only 36.5 % of those aged 25–39 compared to 76.5 % aged 40–50 reported having had a screening mammogram in the last two years [24].
As previously believed, simply changing perceptions regarding screening practices may not be a sufficient facilitator for improving screening practices. Among female survivors of childhood cancer at risk for breast cancer, it was found that physician recommendation was associated with mammography, regardless of the patient’s perspective on the benefits of screening [25]. However, a recent survey of oncologists’ attitudes and knowledge of childhood cancer survivor care showed lack of knowledge of LTFU guidelines, combined with deficiency in surveillance for LE [26]. Additionally, knowledge of such information has been found to be lower in family physicians taking care of childhood cancer survivors [27]. Overall, knowledge deficits of guidelines may lead to lack of physician recommendation of screening for potential LE.
Thus, it is pertinent that adult survivors of childhood cancer be knowledgeable of risks and empowered to advocate for themselves in LTFU care regarding screening practices. In addition to educating survivors, educating oncologists and family physicians about guidelines related to LTFU care, especially with regard to specific screening practices, is crucial. Moreover, awareness of potential risks of LE could help to motivate survivors to attend LTFU care and may influence them to avoid risky behavior (e.g., smoking cigarettes); a study investigating perceptions related to tobacco use in adolescent survivors of cancer found that those who were aware of tobacco-related health risks also reported lower intentions to smoke [28].
Strategies to improve knowledge in childhood cancer survivors
Emerging literature and LTFU guidelines outline approaches that could be taken to ensure that childhood cancer survivors are properly educated about their cancer history. One such approach includes providing survivors with a comprehensive, but concise, written summary of their diagnosis, treatment, and LE, called the survivorship care plan (SCP) mandated by the American College of Surgeons [29]. The purpose of this plan is to provide the survivor with a summary of their cancer treatment, overview of physical and psychosocial effects of treatment, surveillance practices for potential LE, and ways to mitigate the risk of such LE by modifying behavior and resources for needs that a survivor may have regarding their physical and psychosocial health [29]. The SCP will be implemented by all programs accredited by the American College of Surgeons Commission on Cancer by 2015 and will likely be delivered in survivorship clinics or during routine oncology care process [29].
In addition to the SCP, targeted interventions can also be designed to further educate survivors about their LE and surveillance of these risks. In an intervention looking at whether or not a telephone counseling session with a nurse added to SCP increases cardiomyopathy-screening practices showed that at risk survivors of pediatric cancer in the intervention group were more than twice as likely to complete the screening than those in the control group [30]. Moreover, with the widespread adoption of online technology by adolescents and young adults, educational strategies that take advantage of technology to educate survivors, such as SCP delivered over e-mail or through an interactive website, should be developed and evaluated.
Limitations of current study
There were several limitations to this study. Firstly, the small numbers of participants in some of the cancer type categories (e.g., CNS tumors) made it difficult to detect reliable differences versus random variation. In addition, although information mailed to potential participants stressed the importance of completing the questionnaire independently, there was no way of ensuring that these instructions were strictly followed (e.g., parents may have helped). However, the method of recruitment was included in the analyses to control for potential confounding variables. Finally, the cross-sectional design of this study presents limitations for causality and temporality, which cannot be determined.
Conclusion
This study showed that important knowledge deficits exist in many survivors of childhood and adolescent cancer, especially regarding LE. Based on these findings, further research and clinical interventions should be implemented to address knowledge deficits related to treatment and LE prior to and during LTFU care. A longitudinal study is needed to test interventions that may help to increase knowledge in survivors and their LTFU attendance.
References
Howlader N, Noone AM, Krapcho M, Garshell J, Neyman N, Altekruse SF, et al., editors. SEER Cancer Statistics Review, 1975–2010, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2010/, based on November 2012 SEER data submission, posted to the SEER web site, April 2013.
Hudson MM, Mertens AC, Yasui Y, et al. Health status of adult long-term survivors of childhood cancer : a report from the Childhood Cancer Survivor Study. JAMA. 2003;290(12):1583–92.
Oeffinger KC, Mertens AC, Sklar CA, et al. Chronic health conditions in adult survivors of childhood cancer. N Engl J Med. 2006;355(15):1572–82.
Hudson MM, Ness KK, Gurney JG, et al. Clinical ascertainment of health outcomes among adults treated for childhood cancer. JAMA. 2013;309(22):2371–81.
Mertens AC, Yasui Y, Neglia JP, et al. Late mortality experience in five-year survivors of childhood and adolescent cancer: the Childhood Cancer Survivor Study. J Clin Oncol. 2001;19(13):3163–72.
Nathan PC, Hayes-Lattin B, Sisler JJ, Hudson MM. Critical issues in transition and survivorship for adolescents and young adults with cancers. Cancer. 2011;117(10S):2335–41.
Oeffinger KC. Longitudinal risk-based health care for adult survivors of childhood cancer. Curr Probl Cancer. 2003;27(3):143–67.
Oeffinger KC, Mertens AC, Hudson MM, et al. Health care of young adult survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. Ann Fam Med. 2004;2(1):61–70.
Zebrack BJ, Eshelman DA, Hudson MM, et al. Health care for childhood cancer survivors: insights and perspectives from a Delphi panel of young adult survivors of childhood cancer. Cancer. 2004;100(4):843–50.
Schwartz LA, Tuchman LK, Hobbie WL, Ginsberg JP. A social-ecological model of readiness for transition to adult-oriented care for adolescents and young adults with chronic health conditions. Child Care Health Dev. 2011;37(6):883–95.
Byrne J, Lewis S, Halamek L, Connelly RR, Mulvihill JJ. Childhood cancer survivors’ knowledge of their diagnosis and treatment. Ann Intern Med. 1989;110(5):400–3.
Bashore L. Childhood and adolescent cancer survivors’ knowledge of their disease and effect of treatment. J Pediatr Oncol Nurs. 2004;21(2):98–102.
Hess SL, Johannsdottir IM, Hamre H, Kiserud CE, Loge JH, Fossa SD. Adult survivors of childhood malignant lymphoma are not aware of their risk of late effects. Acta Oncol. 2011;50(5):653–9.
Kadan-Lottick NS, Robinson LL, Gurney JG, et al. Childhood cancer survivors’ knowledge about their past diagnosis and treatment: Childhood Cancer Survivor Study. JAMA. 2002;287(14):1832–9.
Hudson MM, Tyc VL, Srivastava DK, Gattuso J, Quargnenti A, Crom DB, et al. Multi-component behavioural intervention to promote health protective behaviors in childhood cancer survivors: the protect study. Med Pediatr Oncol. 2002;39(1):2–1.
Rosenberg-Yunger Z, Klassen AF, Amin L, et al. Barriers and facilitators of transition from pediatric to adult long-term follow-up care in childhood cancer survivors. J Adolesc Young Adult Oncol. 2013;2(3):104–11.
Klassen AF, Rosenberg-Yunger Z, D’Agostino N, et al. The development of scales to measure childhood cancer survivors’ readiness for transition to long-term follow-up care as adults. Accepted Health Expect. 2014.
Steliarova-Foucher E, Stiller C, Lacour B, Kaatasch P. International classification of childhood cancer, third edition. Cancer. 2005;103(7):1457–67.
Werba BE, Hobbie W, Kazak AE, Ittenbach RF, Reilly AF, Meadows AT. Classifying the intensity of pediatric cancer treatment protocols: the intensity of treatment rating scale 2.0 (ITR-2). Pediatr Blood Cancer. 2007;48(7):673–7.
Acock AC. Working with missing values. J Marriage Fam. 2005;67:1012–28.
Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996;49(12):1373–9.
Children’s Oncology Group. Long-term follow-up guidelines for Survivors of Childhood, Adolescent and Young Adult Cancer, Version 4.0. Monrovio: Children’s Oncology Group; 2013. Available on-line: www.survivorshipguidelines.org.
Nathan PC, Ness KK, Mahoney MC, et al. Screening and surveillance for second malignant neoplasms in adult survivors of childhood cancer: a report from the childhood cancer survivor study. Ann Intern Med. 2010;153(7):442–51.
Oeffinger KC, Ford JS, Moskowitz CS, et al. Breast cancer surveillance practices among women previously treated with chest radiation for a childhood cancer. JAMA. 2009;301(4):404–14.
Smith SM, Ford JS, Rakowski W, et al. Inconsistent mammography perceptions and practice among women at risk of breast cancer following a pediatric malignancy: a report from the Childhood Cancer Survivor Study. Cancer Causes Control. 2010;28(10):1585–95.
Henderson TO, Hlubocky FJ, Wroblewski KE, Diller L, Daughtery CK. Physician preferences and knowledge gaps regarding the care of childhood cancer survivors: a mailed survey of pediatric oncologists. J Clin Oncol. 2010;28(5):878–83.
Nathan PC, Daughtery CK, Wroblewski KE, et al. Family physician preferences and knowledge gaps regarding the care of adolescent and young adult survivors of childhood cancer. J Cancer Surviv. 2013;7(3):275–82.
Tyc VL, Hadley W, Crockett G. Predictors of intentions to use tobacco among adolescent survivors of cancer. J Pediatr Psychol. 2001;26:117–21.
Stricker CT, O’Brien M. Implementing the commission on cancer standards for survivorship care plans. Clin J Oncol Nurs. 2014;18(Suppl):15–22.
Hudson MM, Leisenring W, Stratton KK, et al. Increasing cardiomyopathy screening in at-risk adult survivors of pediatric malignancies: a randomized controlled trial. J Clin Oncol. 2014;32(35):3974–81.
Acknowledgments
This study received grants from the Canadian Institutes of Health Research Institute of Cancer Research and the Innovation Fund of the Hamilton Academic Health Sciences Organization Alternate Funding Plan under the auspices of the Ontario Ministry of Health and Long Term Care and the Ontario Medical Association. Anne Klassen is funded by a Canadian Institutes of Health Research Mid-Career Award.
Conflict of interest
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Syed, I.A., Klassen, A.F., Barr, R. et al. Factors associated with childhood cancer survivors’ knowledge about their diagnosis, treatment, and risk for late effects. J Cancer Surviv 10, 363–374 (2016). https://doi.org/10.1007/s11764-015-0482-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-015-0482-7