Abstract
Objective
We present a novel strategy in cardiac surgery with a cardiopulmonary bypass with low-dose heparin and Nafamostat mesylate as an anticoagulant (NM-CPB), which reduces postoperative neurological complications.
Method and results
19 patients with a mean age of 63.6 ± 20.2 years (range 24–91) and an indication of early cardiac surgery with intracranial complication (ICC) underwent surgery with NM-CPB. The preoperative diagnoses included seven cases of infective endocarditis and six of left atrial appendage thrombosis. ICC were noticed in seven cases with hemorrhages (hemorrhagic infarction: n = 4, subarachnoid hemorrhage: n = 3) and 12 without hemorrhage (large infarction: n = 10, small-multiple infarction at the risk for hemorrhagic transformation: n = 2). The mean interval between a diagnosis and cardiac surgery was 1.1 ± 1.5 days in the ICH cases and 1.4 ± 1.4 days otherwise.
In-hospital mortality was 5.3%. The mean CPB time was 146.7 ± 66.03 min, the mean dose of NM, heparin were 2.23 ± 1.59 mg/kg/hr and 56.8 ± 20.3 IU/kg, respectively. The mean activated clotting time (ACT) was 426.8 ± 112.4 s. No further intracranial bleeding and no new hemorrhages were observed after surgery.
Conclusions
In early cardiac surgery with ICC, especially with hemorrhage, NM-CPB reduced postoperative neurological complications. We plan to use NM-CPB to expand the indications and to establish an early aggressive treatment.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Intracranial complication (ICC) is a severe and difficult to manage side effect of acute cardiac surgery. Especially in cases of intracranial hemorrhages (ICH), there is always a risk that cardiopulmonary bypass (CPB) and heparinization may induce serious complications. For instance, in the field of infective endocarditis (IE), a delay in cardiac surgery is recommended in the presence of ICC as long as 4 weeks, and there is still no satisfactory alternative method in the acute phase even if in fatal condition [1]. Even in cases of non-IE, such as residual intracardiac thrombosis with brain complications, the standard response is according to the recommendation for IE 2, 3, and it is still debated whether operating with CPB using normal heparin actually improves or worsens the situation of the patient.
Nafamostat mesylate (NM; 6-amino-2 naphthalene-p-guanidinobenzoate dimethanesulfonate) is a synthetic protease inhibiting agent with particularly intense inhibitory activity on various proteases in the coagulo-fibrinolytic system [4]. Sakamoto et al. [5] and Ota et al. [6] reported that cardiac surgery using NM as an alternative anticoagulant during CPB was performed successfully, reducing perioperative blood loss. There are also reports on the usage of NM as an anticoagulant during CPB in cardiac surgery for IE with ICC; however, its detailed mechanism is still largely unknown. Needless to say, it is unclear for patients with ICH.
In this study, we report on a novel CPB strategy with low-dose heparin and NM as an anticoagulant, which leads to the reduction of perioperative and postoperative intracranial bleeding and neurological complications for early cardiac surgery patients with ICC.
Patients and methods
Patient characteristics
Between May 2017 and April 2021, a total of 608 patients underwent cardiac surgery at our institution. Among them, 19 patients presented indications of emergent surgery with CPB with low-dose heparin and NM as an anticoagulant (NM-CPB) because of ICC. Mean age was 63.6 ± 20.2 years (range 24–91). Twelve patients (63%) were male. In neurological findings, there were 10 cases of hemiplegia, 3 of dizziness, 3 of disorder of consciousness, 2 of headache, and 1 of aphasia. Regarding ICC, it was roughly divided into ICH group (n = 7) and non-ICH group (n = 12). Non-ICH was divided into three types, large infarction (30–49 mm) (n = 5), large one (> 50 mm) (n = 5), and small-multiple infarction (< 30 mm) at the risk for hemorrhagic transformation (n = 2). There were 2 cases, the detail of which are 22 × 15 mm, 18 × 12 mm, multiple one and 13 × 17 mm, 13 × 12 mm, 12 × 7 mm multiple one. In such cases, we refer to a discussion with a neurological team on its risk for hemorrhagic transformation. ICC data was detected by diffusion-weighted magnetic resonance imaging (MRI) or computed tomography (CT) scanning. The size of the infarct and bleeding area was measured at maximal length on the axial plane of CT or MRI. Written informed consent was obtained from the patient for publication of this article and accompanying images. The patient characteristics are listed in Table 1.
Criteria of using NM-CPB under emergent surgery
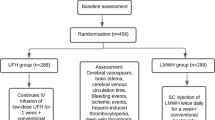
The strategy and methods of NM-CPB were shown in Fig. 1. The indication of NM is for early cardiac surgery using CPB for patients with ICH. In non-ICH cases, the indication is for acute cerebral infarction if the lesion is larger than 30 mm or at the risk for hemorrhagic transformation. Regarding the size of 30 mm, the size of infarction which could be treated safely by early surgery was 15–20 mm [7, 8]. There are some case reports, which stated that the size of it, when less than 30 mm, was treated safely with normal CPB [9]. When the infarction area was smaller than 30 mm or older than 4 weeks, we also considered cardiac surgery with CPB with normal dosage of heparin. Contraindication for NM-CPB was the cases of coma and needed hypothermic surgery.
Strategy and method of cardiopulmonary bypass using nafamostat mesylate (NM-CPB) were shown. Image of below is the pump circuit of NM-CPB. Nafamostat mesylate was infused continuously to the cardiotomy reservoir and venous reservoir at a 0.8 mg/kg/h and 1.0 mg/kg/h, respectively. The rate of injection changed according to activated clotting time (ACT)
Anticoagulation protocol during NM-CPB
As stated in the literature [5], NM (1.0 mg/kg) was administered intravenously to assess for any allergic reaction after induction of anesthesia. Heparin (50 IU/kg; 25% of normal dosage) was then administrated to achieve the activated clotting time (ACT; measured by HemocronTM, Instrumentation Laboratory, USA) of > 400 s after induction of general anesthesia. When measured antithrombin activity was not reached 70%, we added 1500 IU of antithrombin concentrate before CPB. If ACT did not exceed the valid area at an initiation of CPB, an additional dose of heparin (30 IU /kg) was administrated. The CPB circuit consisted of a motor pump (Terumo APS 1, negative pressure drainage), a silicon-heparin-coated hollow-fiber polypropylene Oxygenator (Terumo CX-FX25RE), and a heparin-coated bypass circuit. After connecting the patient to the pump circuit, NM was infused continuously through the venous line of the pump circuit at 1.8 mg/kg/h. ACT was maintained at 350–500 s by a fine titration of the NM dose, which was added at 0.8 mg/kg/hr to the cardiotomy reservoir and at 1.0 mg /kg/hr. ACT was measured every 15 min. When insufficiency or excess of ACT during CPB was observed, the NM dose was adjusted in 0.2 mg/kg/hr increments. There is no upper limit on the amount of NM dose. All patients were cooled to mild hypothermia (33℃–34℃). The target mean systemic pressure was 40–50 mmHg to protect a brain perfusion. The cerebral oxygenation was monitored with a near-infrared oxygen monitor (INVOS. 4100; Somanethics Corporation, Troy, Mich). Concerning brain protection, we set a targeted systemic blood pressure of 50 mmHg and a partial pressure of atrial carbon dioxide (PaCO2) of 30 mmHg during CPB. Monitoring the optimal cerebral oxygenation, we reduced excessive reflex to the injured brain by low systolic blood pressure and PaCO2, which might be part of the explanation of the lack of adverse neurological events. After weaning from CPB and decannulation, no pump suction was allowed and protamin was not usually administrated. If re-CPB is needed after NM-CPB at the same operation, we consider cardiac surgery with a normal dosage of heparin for safety. This protocol was approved by the Ethics committee of our institution (No 22, Jun 29, 2017).
Operative timing and surgical procedure
Their preoperative diagnoses were as follows: 7 cases of IE (native valve endocarditis, NVE: 6, prosthetic valve endocarditis, PVE: 1), 6 cases of left atrial appendage (LAA) thrombosis, and others. The details of patients with unknown reasons are 2 cases of left ventricle thrombus, root abscess, traumatic ascending aortic rupture, left atrial tumor (myxoma), and aortic valve calcification. All diagnoses of IE were made according to the modified Duke criteria. All cases of LAA thrombosis were diagnosed by detailed examination at the time of stroke. The indications of early cardiac surgery were mobile and repeated embolus in 16 patients, septic shock, heart failure and aortic rupture in 1 patient, respectively (Table2). There were 4 patients with stoke underwent surgery with usual CPB. 3 patients were very small and asymptomatic infarction. 1 patient was more than 2 weeks passed from the onset. The mean interval between diagnosis and cardiac surgery was 1.2 ± 1.3 days (range 0–4 days) in the ICH cases and 1.5 ± 1.3 days (range 0–5 days) in the non-ICH cases. All cases underwent cardiac surgery urgently. The employed surgical procedures covered a wide range. In cases of IE, mitral valve plasty was performed for all NVE patients. Re-aortic valve replacement for PVE and patch plasty for aortic annulus was performed after enough vegetectomy and debridement. In cases of LAA thrombosis, thrombectomy with LAA closure was performed with partial sternotomy. Among these cases, procedures, such as mitral valve replacement (MVR) for MS, re-MVR (mechanical to bioprosthetic valve), and Maze operation, were performed concomitantly to avoid anticoagulation therapy in perioperative period. We extracted and examined its details of patients with ICH. The perioperative data and findings were listed in Table 3.
Results
Intraoperative date
The mean CPB time was 146.7 ± 66.03 min (range 68–331 min), and the mean doses of NM and heparin were 347.5 ± 279.3 mg (range 315–700; 2.23 ± 1.59 mg/kg/hr) and 3778 ± 1556 IU (range 2300 to 8000 IU; 56.8 ± 20.3 IU/kg), respectively. One case required additionally 3000 IU (31 IU/Kg) of heparin for achieving a valid ACT, and another case required 3500 IU (50 IU/kg) for a second CPB. The mean ACT was 426.8 ± 112.4 s, and it was generally controlled within the target zone during CPB (Fig. 2). The mean platelet count (× 104/μl) were 25.2 ± 14.2 as pre- CPB, 11.9 ± 6.8 as CPB 30 min, and 12.1 ± 5.4 as post- CPB.
Outcome
In-hospital mortality was 5.3% (n = 1), which was a case of multiple trauma with ICH, dead on day 8 after surgery due to repeated lethal arrhythmia and disseminated intravascular coagulation. For all patients CT was performed on postoperative day 1. There was no further deterioration of intracranial bleeding or any new hemorrhage or stroke (Table 4). There are no thrombotic events in postoperative periods. The average observation period was 18.1 ± 14.4 months (range 0–44 months), and the follow-up rate was 94%. The mortality rate after 3 years was 5.3%, and no deterioration of neurological findings has been established.
The perioperative findings and images of ICH were listed in Fig. 3. Although it was suspected that enlargement of the hemorrhagic infarction in case 5 and increasing edematous change of brain in case 7 on postoperative CT images, these findings would be within the range of normal clinical course after acute cerebral hemorrhage according to the neurological team. There were also no worsen neurological findings in all ICH cases.
Emergent surgical indication, surgical findings, pre- and post- operative brain computed tomography (CT) of cases with intracranial hemorrhages (n = 7) were shown. Allows shows mobile vegetation or thrombus. White circle of third column shows surgical findings of vegetation, thrombus, abscess, and rupture site. Another white circle of fourth, fifth column shows intracranial hemorrhage site. Forth column is preoperative CT and fifth column is postoperative one. Ao, Aorta; LA, left atrium; RA, right atrium; LV, left ventricle; LAA, left atrial appendage
Discussion
Cardiac surgery with cerebral complications especially in cases of IE with cerebral complication, has been only hesitatingly operated on with normal CPB until now. A multicenter study suggests that open cardiac surgery in case of cerebral complications can be performed safely 4 weeks after onset [10]. In the recently revised guideline for IE [11], cardiac surgery should be considered without any delay in cases of heart failure, uncontrolled infection, abscess, or persistent high embolic risk as long as coma is absent and the presence of ICH has been excluded. However, for IE with ICH it is still recommended to delay cardiac surgery for 4 weeks [12, 13].
Garcia-Cabrera et al. [14] and Ruttmann et al. [15] reported that the mortality of early surgery in IE patients with ICH was 66–75%. Okita et al. [16] reported that the mortality of IE patients who underwent surgery within 7 days was higher than that underwent between days 8 and 21. These studies indicate thus that mortality decreases as cardiac surgery in case of ICH is delayed. Contrarily, there are some reports on early surgery of IE with ICH as well. Note also that in case of difficult situations, such as shock, uncontrolled infection, or high embolic risk in patients with ICH, the current guidelines recommend delaying the surgery not to aggravate the situation of the patients.
In the case of non-IE patients, especially with residual LAA thrombosis after ICC, in our institution, cardiac surgery with NM-CPB is usually performed. Because there is no clear guideline for emergent operations of residual LAA thrombosis after ICC, the indication and timing of surgery remain unclear. There are reports of successful anticoagulant therapy in such cases [15,16,17,18,19], however, cases of re-ICC with disastrous results are also known [20, 21]. As we experienced two cases of re-ICC in patients under anticoagulant therapy in our institution, we extended the indication of emergent surgery to LAA thrombosis with ICC. The indication in such cases was a thrombus size > 10 mm and the fact that it was mobile. The cases of coma were excluded. When a cardiogenic stroke was suspected, we checked for the presence of thrombosis by ultrasound or CT within 48 h, and surgery with NM-CPB was performed as soon as possible if indicated. This has been successfully done for six cases of ICC with or without hemorrhage, without mortality cases or worsening of neurological findings.
We performed cardiac surgery using NM-CPB on IE patients with recent cerebral infarction. Though the target was IE with non-hemorrhage infarction in the early stage, we expanded the indication to ICH, multiple trauma. The anticoagulation protocol was based on the one issued by the Department of Cardiovascular Surgery of the Kobe University. Early surgery for IE with ICH using the same anticoagulation protocol was reported to produce successful outcomes. Sakamoto et al. and Ota et al. reported that the timing of surgery was 2.1–2.3 days from onset, with a mortality of 33.3% and no worse hemorrhages [5, 6]. In both cases, mortality was not explicitly associated with surgery. There were some reports of NM-CPB surgery from other facilities, too. Yamamoto et al. reported a surgical case of left atrial myxoma with hemorrhagic cerebral infarction on day 5 from onset using NM (1.0 mg/kg/hr) as an anticoagulant, whereas the total dose of heparin sodium was 150 IU/kg [22]. Yasuda et al. reported on a surgical case of left atrial thrombus with hemorrhagic cerebral infarction on day 5 from onset using NM (2.0 mg/kg/h) as an anticoagulant while the total dose of heparin sodium was 100 IU/kg [23]. In the seven cases of cardiac surgery with ICH performed by the authors of this study, the timing of surgery was 1.1 days from onset, and the mortality reached 14.2%.
ACT is not a good parameter for NM as anticoagulation during CPB: However, it is good for heparin. We measured ACT by HemocronTM, which was Celite-measured ACT (Celite; World Minerals Inc, Santa Barbara, Calif). The Celite-ACT is total ACT which reflects the activity of anticoagulation of both heparin and NM. Kaolin-measured ACT reflects the only heparin activity in the blood under the combined use of NM because kaolin absorbs NM [24]. Although we should measure both Celite and Kaolin ACT for all cases, it was difficult to measure and analyze both ACT each 15 min in a limited situation for all cases. Besides, we gradually became possible to perform surgery with NM-CPB safely by close monitoring the surgical site and pump-circuit visually with concerning to celite-ACT. Although it is difficult to measure directly the effect of NM only by ACT, we should consider measuring the anticoagulation of NM by other testing tools, such as thromboelastography (TEG).
NM has also been used as an anticoagulant in substitution for heparin for extracorporeal membrane oxygenation and hemodialysis. Although its exact action mechanism has not been clarified yet, the advantages of NM consist of its very short half-time and successful application in inactive coagulation, fibrinolysis, and platelet aggregation. Miyamoto et al. reported that fibrinolysis was inhibited during CPB when using NM [25]. Tanaka et al. reported that NM preserves the platelet function and that heparin sodium enhances fibrinolysis activity during CPB [26, 27]. Therefore, it was necessary to perform cardiac surgery under severe circumstances of ICH, wherein the inhabitation of fibrinolysis and preservation of the platelet function were stressed as advantages brought by NM.
Other studies noted that blood loss during CPB was reduced while employing NM, although this happened after the administration of a normal dose of heparin [28, 29]. Although Fukata et al. presented the successful study on the timing of using NM during CPB, the problem of identifying the optimal dose of NM and analysis of its safety are still open [30]. Several contributions suggested that the dose of NM should be about 1.0–2.0 mg/kg/h for 100–150 IU/kg of heparin sodium. Contrarily, in our study we worked with an NM dose of 2.23 ± 1.59 mg/kg/h for 56.8 ± 20.3 IU/kg of heparin sodium, showing that more effective positive results of cardiac surgery could be achieved with smaller amounts of heparin sodium by maximizing the benefits of NM. Further research on the optimal dosage of NM and heparin sodium is necessary.
Regarding safety concerns during CPB, there were no reports of blood coagulation in the pump circuit in our study group. When we observe coagulation tendency in the circuit or the filter of the reservoir regardless of usual protocol, we plan to add a full dose of heparin and transfer to the usual CPB. As clots in the heart sac were reported during CPB in the literature, we sprinkled directly the clot in the heart sac when necessary.
Despite the significant contributions of our study, several limitations have to be addressed as well. First, because the study was performed on a very small number of patients, further research on larger cohorts are necessary for confirming our findings. Second, our study was not based on basic research while approved by the Ethics committee of our institution. Third, we could not assign patients with acute ICC to ECC with normal dosage heparin group as a control from an ethical perspective. Fourth, no laboratory data about coagulation and fibrinolysis were used as none was available to us.
In this study, we have shown that NM can be a useful option as an anticoagulant in critical situations of cardiac surgery with ICC involving cardiopulmonary bypass.
In emergent cases of open heart surgery with ICC, especially with hemorrhage, the approach we proposed turned out to significantly reduce postoperative neurological complications. Further investigations are necessary to identify the optimal dosage of NM in surgery with cardiopulmonary bypass and to find further possible useful effects of its employment.
References
Habib G, Lancellotti P, Antunes MJ, Bongiorni MG, Casalta JP, Del Zotti F, et al. 2015 ESC Guidelines for the management of infective endocarditis. Eur Heart J. 2015;36(44):3075–128.
Kernan WN, Ovbiagele B, Black HR, Bravata DM, Chimowitz MI, Ezekowitz MD, et al. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45(7):2160–226.
Nakamura M, Uzuka T, Sato H, Kondo M, Sakta J, Kodama F. Early surgery with aggressive surgical approach to improve 6-month outcomes in patients with active infective endocarditis: contribution of cerebral preoperative magnetic resonance imaging. Gen Thorac Cardiovasc Surg. 2019;67(5):427–35.
Hitomi Y, Ikari N, Fujii S. Inhibitory effect of a new synthetic protease inhibitor (FUT-175) on the coagulation system. Haemostasis. 1985;15(3):164–8.
Sakamoto T, Kano H, Miyahara S, Inoue T, Izawa N, Gotake Y. Efficacy of nafamostat mesilate as anticoagulation during cardiopulmonary bypass for early surgery in patients with active infective endocarditis complicated by stroke. J Heart Valve Dis. 2014;23(6):744–51.
Ota T, Okada K, Kano H, Okita Y. Cardiopulmonary bypass using nafamostat mesilate for patients with infective endocarditis and recent intracranial hemorrhage. Interact Cardiovasc Thoracic Surg. 2007;6(3):270–3.
Miura T, Eishi K. Current treatment of active infective endocarditis with brain complications. Gen Thorac Cardiovasc Surg. 2013;61(10):551–9.
Hosono M, Sasaki Y, Hirai H, et al. Considerations in timing of surgical intervention for infective endocarditis with cerebrovascular complications. J Heart Valve Dis. 2010;19(3):321–5.
Shang E, Forrest GN, Chizmar T, Chim J, Brown JM, Zhan M. Mitral valve infective endocarditis: benefit of early operation and aggressive use of repair. Ann Thorac Surg. 2009;87(6):1728–34.
Eishi K, Kawazoe K, Kuriyama Y, Kitoh Y, Kawashima Y, Omae T. Surgical management of infective endocarditis associated with cerebral complications. Multi-center retrospective study in Japan. J Thorac Cardiovasc Surg. 1995;110(6):1745–55.
Nakatani S, Ohara T, Ashihara K, et al. JCS 2017 guideline on prevention and treatment of infective endocarditis. Circ J. 2019;83(8):1767–809.
Pettersson GB, Coselli JS, Pettersson GB, Coselli JS, Hussain ST, Griffin B, et al. 2016 The American Association for Thoracic Surgery (AATS) consensus guidelines: surgical treatment of infective endocarditis: executive summary. J Thorac Cardiovasc Surg. 2017;153(6):1241–58.
Baddour LM, Wilson WR, Bayer AS, Fowler VG, Tleyjeh IM, Rybak MJ. Infective endocarditis in adults: Diagnosis, antimicrobial therapy, and management of complications: a scientific statement for healthcare professionals from the American Heart Association. Circulation. 2015;132(15):1435–86.
García-Cabrera E, Fernández-Hidalgo N, Almirante B, Ivanova-Georgieva R, Noureddine M, Plata A. Neurological complications of infective endocarditis risk factors, outcome, and impact of cardiac surgery: a multicenter observational study. Circulation. 2013;127(23):2272–84.
Ruttmann E, Willeit J, Ulmer H, Chevtchik O, Höfer D, Poewe W. Neurological outcome of septic cardioembolic stroke after infective endocarditis. Stroke. 2006;37(8):2094–9.
Okita Y, Minakata K, Yasuno S, Uozumi R, Sato T, Ueshima K, et al. Optimal timing of surgery for active infective endocarditis with cerebral complications: A Japanese multicentre study. Eur J Cardiothorac Surg. 2016;50(2):374–82.
Saito S, Shindo S, Tsudaka S, Uchida K, Shirakawa M, Yoshimura S. Resolving thrombus in the left atrial appendage by edoxaban treatment after acute ischemic stroke: report of 2 cases. J Stroke Cerebrovasc Dis. 2016;25(10):e188–91.
Saito S, Tomita H, Kimura Y, Shiroto H, Hagii J, Metoki N, et al. Reduced smoke-like echo and resolved thrombus in the left atrium with rivaroxaban therapy in an acute cardioembolic stroke patient. J Stroke Cerebrovasc Dis. 2014;23(6):1747–9.
Yasaka M, Yamaguchi T, Miyashita T, Tsuchiya T. Regression of intracardiac thrombus after embolic stroke. Stroke. 1990;21(11):1540–4.
Fang BR, Kuo LT. Recurrent cerebral embolism and impending detachment of a previous nonmobile left atrial thrombus following initiation of anticoagulant therapy in a patient with nonvalvular atrial fibrillation. Echocardiography. 2001;18(6):527–9.
Tabata E, Yasaka M, Wakugawa Y, Komori M, Mori K, Tsurusaki Y, et al. Increase in the size of an intracardiac thrombus during dabigatran therapy (110 mg b.i.d.) in an acute cardioembolic stroke patient. Cerebrovasc Dis Extra. 2013;3(1):78–80.
Yamamoto S. Left atrial myxoma surgically resected in acute phase of hemorrhagic cerebral infarction: report of a case. Kyobu Geka. 2007;60(3):237–41.
Yasuda S, Tokunaga S, Matsuki Y, Okamoto H, Machida D, Masuda M. Left atrium ball thrombus in a patient with hemorrhagic cerebral infarction. Ann Thorac Surg. 2013;96(6):2236–8.
Despotis GJ, Gravlee G, Filos K, Levy J. Anticoagulation monitoring during cardiac surgery: a review of current and emerging techniques. Anesthesiology. 1999;91:1122–51.
Miyamoato Y, Nakano S, Kaneko M, Takano H, Matsuda H. Clinical evaluation of a new synthetic protease inhibitor in open heart surgery effect on plasma serotonin and histamine release and blood conservation. ASAIO J. 1992;38(3):395–8.
Tanaka K, Takao M, Yada I, Yusas M, Kusagawa M, Deguchi K. Alterations in coagulation and fibrinolysis associated with cardiopulmonary bypass during open heart surgery. J Cardiothorac Anesth. 1989;3(2):181–8.
Sato S, Tanaka K, Kondo C, Morimoto T, Yada I, Yuasa H, et al. Nafamostat mesilate administration during cardiopulmonary bypass decreases postoperative bleeding after cardiac surgery. ASAIO Trans. 1991;37(3):194–5.
Tanaka K, Kondo C, Takagi K. Effects of nafamostat mesilate on platelets and coagulofibrinolysis during cardiopulmonary bypass surgery. ASAIO J. 1993;39(3):545–9.
Murase M, Usui A, Tomita Y, Maeda M, Koyama T, Abe T. Nafamostat mesilate reduces blood loss during open heart surgery. Circulation. 1993;88(5):432–6.
Fukata Y. Reduction in dose of heparin by combined use of nafamostat mesilate for the control of cardiopulmonary bypass. Iryo. 1994;48(3):196–201.
Acknowledgements
The authors would like to thank Prof. Emeritus Yutaka Okita and the department of cardiovascular surgery Kobe University for their kind guidance and continuous support.
Funding
The authors declare no grants, and sources of funding related to the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest related to the manuscript.
Institutional review board approval
All procedures used in this research were approved by the Ethical Committee of Okinawa Nanbu Prefectural Medical Center and Childrenʼs Medical Center, (No 22, Jun 29, 2017).
Informed consent
Written informed consent was obtained from the patient for publication of this article and accompanying images.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yamazato, T., Oyama, N., Fujii, T. et al. Aggressive early surgical strategy in patients with intracranial hemorrhage: a new cardiopulmonary bypass option. Gen Thorac Cardiovasc Surg 70, 602–610 (2022). https://doi.org/10.1007/s11748-021-01743-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-021-01743-w