Abstract
A 32-year-old male patient was initially diagnosed with fibrosing mediastinitis. The patient subsequently developed severe dyspnea and was further diagnosed with constrictive pericarditis due to the extent of fibrosing mediastinitis around the heart. Therefore, the patient underwent surgical resection of the fibrotic tissue in the anterior mediastinum including the pericardium and the pleura. Postoperative histological and immunohistochemical analyses revealed angiosarcoma. Seven years after the diagnosis, he is still alive. Herein, we report a case of atypical primary angiosarcoma of the anterior mediastinum causing constrictive pericarditis and restrictive pulmonary dysfunction.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
An angiosarcoma is the most common primary malignant tumor of the heart with poor prognosis. However, primary angiosarcoma of the anterior mediastinum is extremely rare with a limited number of case reports. We reported a case of primary mediastinal angiosarcoma atypically causing constrictive pericarditis and restrictive pulmonary dysfunction.
Case
A 32-year-old male physician developed worsening fatigue and severe dyspnea. He first recognized exertional dyspnea 4 years ago. One year prior to this presentation, a chest computed tomography (CT) showed bilateral pleural effusion and diffuse enlargement of the anterior mediastinum. Pleural effusion was found to be chylous, and no malignancy was observed on cytological examination. Thoracoscopic biopsy revealed inflammatory fibrous tissue of the anterior mediastinum. Thus, he was diagnosed with fibrosing mediastinitis and subcutaneous administration of sandostatin was effective against chylothorax [1]. At this point, his pulmonary function test (PFT) revealed that vital capacity (VC) and forced expiratory volume in 1 s (FEV1.0) had decreased from 2.51 to 1.00 L and from 2.04 to 0.96 L, respectively during a 3-year interval. Arterial blood gas (ABG) analysis revealed pH 7.36, PaO2 60.8 mmHg, and PaCO2 73.7 mmHg on room air. Although noninvasive positive pressure ventilation (NPPV) was initiated with high inspiratory positive airway pressure (IPAP: 28 cmH2O), his dyspnea worsened.
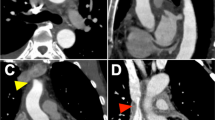
At the time of this presentation, a chest CT revealed thickness of the pericardium and the left pleura (Fig. 1a). Cardiac catheterization was consistent with constrictive physiology as follows: systemic blood pressure (SBP) 104/75 (80) mmHg, pulmonary artery pressure (PAP) 44/25 (32) mmHg, pulmonary capillary wedge pressure (PCWP) 24 mmHg, right atrial pressure (RAP) 26 mmHg, and cardiac index (CI) 1.36 L/min/m2. Right ventricular pressure tracing showed 46/~ 24 mmHg with dip and plateau pattern. FDG-PET/CT showed a significant FDG uptake in the mediastinal adipose tissue. Moreover, this adipose tissue was accumulated unevenly in the right side of the heart, suggesting the presence of active pericarditis. MRI showed neoplastic lesions from the bilateral supraclavicular fatty tissue to the mediastinum. In addition, thickening of the pleura, between the bilateral lobes, fluid retention, especially along the left pleura, and pulmonary edema, which could have been caused by pleural fibrosis, were observed in the lung.
Computed tomography scan a before he initial operation. b 1 month after the initial operation: residual thickened left pleura; no residual pericardial thickening and improvement in congestive lung. c 6 years after the initial operation. Operative findings: d arrows indicate vestige of thickened pericardium. The pericardium was removed from the epicardium (asterisk). e The thickened pleura (arrows) was dissected from the lung (asterisk). S sternum, H heart
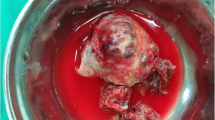
The patient underwent surgical resection of the fibrotic anterior mediastinal tissue. Because of a high risk for circulatory collapse, the patient was placed on cardiopulmonary bypass via cannulation of the femoral artery and the vein at the time of general anesthesia induction. After median sternotomy, we found that the thickened fibrous tissue of the anterior mediastinum was whitish in color and elastic hard without hemorrhage, apparently causing restriction of both lungs and the heart. The anterior mediastinal tissue along with the pericardium had moderate adhesion to the epicardial surface on the cardiac structure (Fig. 1d) and did not seem to invade the cardiac muscle. We removed the anterior-to-lateral pericardium between the phrenic nerves of both sides and the inferior pericardium facing the diaphragm. The thickened anterior aspect of the pleura was also removed bilaterally. Postoperatively, cardiac catheterization showed improvement as follows: SBP 93/57 (65) mmHg, PAP 31/18 (23) mmHg, PCWP 16 mmHg, RAP 11 mmHg, and CI 1.90 L/min/m2. The ABG also improved: pH 7.46, PaO2 94.5 mmHg and PaCO2 63.7 mmHg under O2 at 2 L/min via nasal cannula. Histological examination revealed angiosarcoma with atypical vascular proliferation in both the pericardium and the pleura (Fig. 2a, b). Immunohistochemical studies revealed positivity for factor VIII and CD31 (Fig. 2c). Because Ki-67 labeling index was less than 1%, adjuvant chemotherapy was not given (Fig. 2d).
a Histological study showed invasive growth of irregularly shaped and anastomosing vascular channels (Hematoxylin–eosin stain), b solid nodules of endothelial cells, c immunohistochemical staining for CD31 showed anastomosing vascular channels lined with positive endothelial cells. d Ki-67 labeling index was less than 1%
However, the respiratory condition gradually worsened again. Seven months after surgery, PFT showed only 0.66 L of VC, and 0.66 L of FEV1.0. Hence, he again became dependent on NPPV (25 cmH2O) throughout the day. We suspected that the residual thickened left side pleura had caused respiratory deterioration (Fig. 1b), and thus decided the reoperation to remove the left pleura. During the second operation via redo median sternotomy under cardiopulmonary bypass, we dissected and removed the left side pleura with dense fibrotic tissue of the left lower lobe of the lung (Fig. 1e). The pathological analyses were the same as before. Postoperatively, the PFT and ABG improved slightly (VC 0.72 L, pH 7.408, PaO2 81.9 mmHg, and PaCO2 68.4 mmHg under O2 at 1 L/min); however, he still required IPAP (20 cmH2O) intermittently. One year after reoperation, he returned to work as an internal medicine physician with daytime and nocturnal NPPV usage. Without any additional treatment against angiosarcoma, he has been alive for seven years since the first operation, using NPPV almost all day long. His heart failure has been gradually worsened, leading to NYHA class IV, although chest CT revealed the thickening of pericardium and left pleura has been almost unchanged (Fig. 1c).
Discussion
Angiosarcoma is an uncommon tumor representing less than 1% of all sarcomas [2]. Particularly, primary angiosarcomas arising in the anterior mediastinum are extremely rare [3]. Most of the cases revealed typical symptoms of anterior mediastinal masses; namely, chest pain, dyspnea, and cough [3, 4]. To the best of our knowledge, this is the first report of primary angiosarcoma of the anterior mediastinum causing congestive pericarditis and restrictive pulmonary dysfunction.
Angiosarcomas have a poor prognosis with reported 5-year survival rates ranging from 12 to 35% [2]. The mainstay of treatment has traditionally been wide-margin surgical resection. However, in our case, the patient is still surviving for 7 years postoperatively. His initial diagnosis was fibrosing mediastinitis. We observed no masses in the mediastinum, but there was a thick layer of angiosarcoma around the heart which resulted in constrictive pericarditis. Moreover, because of the rarity of mediastinal angiosarcoma, these neoplasms must be differentiated from various other tumors that can occur in this location. In the present case, histological analysis showed invasive growth of irregularly shaped, anastomosing vascular channels lined with CD31-positve endothelial cells. Some solid nodules of endothelial cells were also seen. The nuclear atypia was mild; however, some of them were plump. Taken together, mediastinal angiosarcoma was diagnosed.
Weissferdt et al. [4] reported that primary angiosarcoma of the anterior mediastinum appeared to follow a more protracted clinical course. Angiosarcomas are a heterogeneous group of tumors and apart from the stage at diagnosis, an important prognostic factor is the primary site. Although the angiosarcoma of the heart, liver, and bone have poor outcome with 5-year survival rates between 0 and 36%, the tumors of the breast, soft tissue, and skin demonstrate a slightly better prognosis with 5-year survival rates between 43 and 74% [5]. Moreover, histological grade was also found to be prognostic factor for survival [6]. In the present case, Ki-67 labeling index which is a marker of rapid growth was less than 1%. This result indicates that the angiosarcoma of this case has slow progression potential in nature, and supports a favorable clinical course with relatively longer survival.
Conclusion
In this report, we described a rare case of angiosarcoma of the anterior mediastinum that atypically presented with constrictive pericarditis and restrictive pulmonary disease. Successful surgical resection has played a significant role in symptom relief and provides longer survival.
References
Togashi Y, Kim YH, Miyahara R, et al. Octreotide, a somatostatin analogue, in the treatment of chylothorax associated with idiopathic fibrosing mediastinitis. Tohoku J Exp Med. 2010;222:51–3.
Young RJ, Brown NJ, Reed MW, Hughes D, Woll PJ. Angiosarcoma. Lancet Oncol. 2010;11:983–91.
Dainese E, Pozzi B, Milani M, et al. Primary pleural epidermoid angiosarcoma. A case report and review of literature. Pathol Res Pract. 2010;206:415–9.
Weissferdt A, Kalhor N, Suster S, Moran CA. Primary angiosarcoma of the anterior mediastinum: a clinicopathologic and immunohistochemical study of 9 cases. Hum Pathol. 2010;41:1711–7.
Fayette J, Martin E, Piperno-Neumann S, et al. Angiosarcomas, a heterogeneous group of sarcomas with specific behavior depending on primary site: a retrospective study of 161 cases. Ann Oncol. 2007;18:2030–6.
Anderson T, Zhang L, Hameed M, Rushch V, Travis WD, Antonescu CR. Thoracic epithelioid malignant vascular tumors: a clinicopathorogic study of 52 cases with emphasis on pathologic grading and molecular studies of WWTR1-CAMTA1 fusions. Am J Surg Pathol. 2015;39:132–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yamazaki, K., Minakata, K., Nakane, T. et al. A rare case of primary angiosarcoma of the anterior mediastinum. Gen Thorac Cardiovasc Surg 69, 766–769 (2021). https://doi.org/10.1007/s11748-020-01551-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-020-01551-8