Abstract
Within the visual system, docosahexaenoic acid (DHA, 22:6n−3) is an important structural component for retinal photoreceptors and cortical gray matter. There is a marked decrease in neural DHA accumulation in the face of DHA deficiency. DHA is accumulated at an accelerated rate during pregnancy, especially in the third trimester. However, pregnant women in the US and Canada have dietary DHA intakes that are significantly below the optimal level. The main objective of this study was to determine whether a DHA-functional food during pregnancy would benefit infant visual acuity at four and six months of age measured behaviorally using the acuity card procedure (ACP). In a randomized, longitudinal, double-blinded, and placebo-controlled trial, 30 pregnant women received either the DHA-functional food (n = 16) or the placebo (n = 14). There were significant main effects for visual acuity at four months of age (P = 0.018). The mean acuity scores were 3.8 ± 1.1 cycles/degree in the DHA group versus 3.2 ± 0.7 cycles/degree in the placebo group. At six months there were no group differences. Based on our results, we conclude that DHA supplemented during pregnancy plays a role in the maturation of the visual system.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The visual system comprises a complex signaling system involving the retina, thalamus and primary visual cortex. In addition, multiple other cortical regions are involved in the cognitive integration of visual information. Previous studies focused on the impact of long-chain polyunsaturated fatty acids (LCPUFA) on infant visual development have assessed two main aspects of the visual system: retinal development using electroretinogram (ERG), and visual processing at the level of the primary visual cortex. Cortical measures of resolution include sweep visual evoked potential (VEP) and behavioral assessments like the acuity card procedure (ACP). Of the resolution (grating) acuity measures, VEP measures cortical response directly and has less variability [1]. However, behavioral acuity measures provide a different measure of what an infant actually perceives, and normative data are well established for this procedure [1, 2]. Behavioral acuity measured with ACP is dependent on different brain regions controlling eye movements, attention, and other processes involved in generating the behavioral response [1].
Compared to other cells of the body, retinal photoreceptors have the highest docosahexaenoic acid (DHA, 22:6 n−3) content. The gray matter in the visual cortex and multiple other cortical regions also have high levels of DHA. In an animal model, a diet deficient in LCPUFA during pregnancy impeded accumulation of DHA in these tissues [3]. A 50% reduction of DHA in retinal tissue and a 25% reduction in cerebral cortex DHA was reported for the offspring of rhesus monkeys fed a diet deficient in α-linolenic acid (ALA, 18:3n−3) during pregnancy compared to controls [3]. Deficient animals also had lower visual acuity using behavioral measures and a prolonged recovery time of the dark-adapted ERG after a saturating flash.
In full-term infants, improved visual function related to the provision of n−3 fatty acids during the postnatal period has been repeatedly reported based on the application of methods of visual acuity assessment [4–9]. There are no reports of improved infant visual acuity assessed using the ACP related to maternal dietary DHA intake. Malcolm et al. [10, 11] used VEP and ERG to assess visual acuity and retinal function after maternal DHA supplementation. In these studies, no significant treatment effect was reported for ERG in the first postnatal week [8] or VEP at 2.5 or 6.5 months of age [7].
Pregnant women in the US and Canada have DHA intakes well below the 300 mg/day recommended by the National Institutes of Health Workshop on the Essentiality of and Recommended Dietary Intakes for Omega-6 and Omega-3 Fatty Acids [12–17]. As the developing fetus has an extremely limited capacity to derive DHA from the 18-carbon precursor, the fetus is clearly at risk of a relative deficiency of DHA.
In the current study, we hypothesized that infants of mothers who consumed the DHA-functional food during pregnancy would have better visual acuity when assessed with ACP at four and six months of age compared to infants of mothers consuming a placebo.
Methods
Study Design
In a randomized, longitudinal, double-blinded, and placebo-controlled trial, 30 pregnant women 18–35 years of age and <20 weeks gestation were recruited. The cohort used to assess visual acuity was derived from a larger study (unpublished data) focused on the impact of maternal DHA supplementation on infant sleep patterning in the first two postnatal days. Ten ACP assessments were lost initially due to a delay in implementing the ACP. Once implemented, 50% of the infants of women originally recruited were assessed for vision. Colored marbles representing each study group were selected at random for group assignments by an individual who did not work directly on the project. All other personnel involved with the project were blinded to group assignments. The placebo bars were packaged in exactly the same manner as the intervention bars, making detection of group assignments impossible for investigators or participants. Study groups received: (1) the DHA-containing cereal-based bars, n = 16 (300 mg DHA as low EPA fish oil: EPA:DHA, 1:8, per 92 kcal bar) or (2) the cereal-based placebo bars containing corn oil, n = 14. Within each group, women consumed three, five or seven bars weekly from 24 weeks of pregnancy to delivery. The consumption of an average of five bars per week provided 214 mg DHA/day via the functional food. The cereal-based bars did not differ in energy, carbohydrate, protein or total fat content (Table 1).
The initial blood draw and 24-h recall were collected at 20–22 weeks gestation prior to starting the intervention at 24 weeks. Women were instructed to consume bars beginning at 24 weeks gestation and continue until delivery. Bars were delivered to women once monthly. Women were given logs to record bar intakes and these were collected monthly. Four times throughout the pregnancy the women were interviewed using 24-h dietary recalls by a trained researcher. All maternal dietary data were evaluated using the Nutrition Data System for Research (NDS, 2005). Infant medical history and diet histories of infants’ intakes were obtained at four and six months of age from the mother or primary caregiver. Visual assessments were conducted only on healthy infants and appointments were rescheduled if infants became ill prior to their scheduled appointments. Care was also taken to schedule appointments during the time of day that the infant was most alert/active.
Subjects
Subject recruitment was conducted in accordance with IRB guidelines at Hartford Hospital and the University of Connecticut. Women with a history of drug/alcohol addiction, smoking, hypertension, hyperlipidemia, renal disease, liver disease, diabetes or psychiatric disorder were excluded from study participation.
Infant Visual Acuity Testing
Visual acuity assessments were conducted at four and six months of age by an individual trained in the ACP using Teller acuity cards [18, 19]. These rectangular cards each contain a square patch of black and white stripes; the cards are arranged from high to low stripe width or grating. One black and white stripe is referred to as one cycle and the frequency of the stripes is given in cycles per centimeter. The spatial frequency doubles stepwise every other card, and this increase in spatial frequency is referred to as an octave. Cards were presented to infants on a stage starting with 0.32 cycles/cm for the four-month assessment and 0.64 cycles/cm for the six-month assessment. Infants were seated 38 cm from the test stage at four months and 55 cm at six months of age. The distances from the stage based upon infant age were set according to the standard ACP procedure. Both groups were tested at identical distances from the stage at four and then at six months. A light meter was used to ensure that the lighting was consistent and adequate for all infants (minimum level of 10 candelas/m2).
The test administrator stood on the opposite side of the stage and observed the infants through a peephole in the cards. As the cards were presented to the infants, the tester was unaware of the location of the striped patch on the rectangular card, i.e., left or right. The high visual contrast of the black and white striped square provides a great deal of visual interest for young infants, causing them to look toward the grating pattern if it can be seen by the infant. The observer watched the infant’s response to the card and made an assessment regarding whether the striped patch was located on the right or left side of the card based upon the infant’s behavioral response. Cards were presented to infants from low to high visual frequency in 0.5 octave steps, and an assessment was made with each step as to whether the infant was able to see the stripes reliably. The observer repeated the presentation of each card; after the first presentation the card was typically flipped so that the stripes were on the opposite side (i.e., left versus right). If the infant could see the stripes, the observer expected the infant to look to the opposite side on alternate trials. The observer presented each card a sufficient number of times to reliably answer the question, “Can the infant see the stripes?” (answer: yes or no). The card with the finest grating that the infant could see was defined as the threshold.
A single individual who was trained and validated in the procedure performed all visual assessments. All ACP assessments were completed at Hartford Hospital, ensuring that controlled conditions were used, e.g., lighting, sound, distance. Lastly, acuity scores in cycles/degree were converted to octaves, log (base 2), for all statistical analyses as a standard procedure associated with the ACP [18].
Previous studies of infants with diets supplemented with DHA demonstrated that significant differences between mean acuities were ≥0.40 octaves [20]. Because in the current study we were assessing dietary intake of pregnant mothers, rather than infants, we anticipated greater group differences (0.50 octaves). Using α = 0.05 and power = 0.80, the calculated sample size was 16 subjects per group.
Statistical Analyses
All statistical analyses were conducted using the Statistical Analysis System (SAS) software [21]. The PROC GLM procedure was used for group comparisons of the log-transformed acuity scores. Analyses of baseline characteristics included the Student’s t-test for numeric and chi-square for categorical variables. The Proc Mixed procedure was used to evaluate changes over time between four and six-month assessments.
Results
Overall, groups were well randomized, as most group characteristics were similar between groups (Table 2). Total weight gain during pregnancy, infant gender and APGAR score at 5 min were significantly different between groups.
Information regarding maternal ethnicity and risk of depression was collected via a review of medical records, and there were no differences between groups. Incidence of venereal disease during pregnancy was low in both groups and there were no differences between groups.
The mean dietary DHA intake was not significantly different between groups, and the mean average DHA intake for our entire cohort was 80 mg/day. Thus, subjects in the intervention group received an average of 294 mg DHA/day with intervention and dietary intakes combined.
Mode of infant feeding was categorized as: formula with DHA; formula containing no DHA; breast milk only; combination breast milk and formula no DHA; breastfed for 1–2 months, then changed to formula containing no DHA; breastfed for 2–4 months, then changed to formula containing no DHA. There were no differences between study groups for infant feeding type.
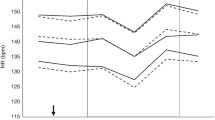
Groups were not different for timing of the ACP assessment at the four or six-month time points (133.2 ± 16.3 days, DHA intervention versus 126.7 ± 6.0 days, placebo at four months; 187.9 ± 7.5 days, DHA intervention versus 190.9 ± 9.6 days, placebo at six months of age). Mean visual acuity scores at four and six months of age for the DHA group compared to the placebo group are presented in Table 3.
The same regression model was used to evaluate infant visual acuity by group at four and six months. The main fixed factor was group (intervention, placebo). Independent and potentially confounding variables for the model were: infant gender, weight gain during pregnancy, APGAR score at 5 min, maternal hematocrit, participation in the WIC program and infant feeding type. Of these independent variables, infant gender and maternal weight gain were not significant within the model (with significant group differences) and were therefore excluded. There was a significant group difference in visual acuity at four months of age after adjusting for potential confounding variables (P = 0.018). Using the same model, there was no significant group difference at six months of age.
There was an increase in ACP score over time for both groups between four and six months (P ≤ 0.0001); however, change over time was not significantly different between the DHA and placebo groups.
Discussion
Our findings demonstrate that infants of mothers who consumed the DHA-functional food during pregnancy had higher ACP visual acuity scores at four months of age compared to controls. In principle, higher acuity scores indicate that the infant is able to resolve a finer grating and therefore demonstrate more mature sensory visual processing. Our finding suggests that the infants of mothers who consumed the DHA food during pregnancy had better visual development at four months than infants of women consuming the placebo, regardless of what the infants were fed postnatally. Group differences were not significant at six months of age.
Visual acuity improved from four to six months for both the DHA and placebo groups. An improvement in visual acuity from the four to the six-month time point was expected, as this is the pattern seen in normative ACP data [2]. These data can be interpreted from the standpoint that infants of mothers who consumed DHA during pregnancy had accelerated development of the visual system that occurred some time prior to four months of age, when we assessed it.
Although ACP has inherent subjectivity not associated with ERG and VEP, it provides an opportunity to evaluate the behavioral responses that require more integrated processing associated with the visual stimulus. As far as we know, this is the first report of the impact of DHA supplementation during pregnancy on infant visual acuity assessed with ACP.
Dietary DHA deficiency during pregnancy reduces the DHA content of photoreceptor membranes of the retina and induces subnormal visual acuity in offspring of nonhuman primates compared to controls [3]. In the absence of DHA, retinal tissue accumulated higher levels of n−6 derived docosapentaenoic acid (DPA, 22:5n−6), altering membrane characteristics [22]. Such changes in membrane properties interfere with cellular signaling pathways, leading to deficits in function. More specifically, impairment in the G protein-coupled receptor (GPCR) signal transduction was demonstrated in association with DHA deficiency in retinal rod outer segment membranes isolated from rats [22].
Alteration in GPCR signal transduction in the rat model provides a plausible mechanism for our findings of better visual acuity in those infants whose mothers consumed DHA during pregnancy. GPCR signal transduction also has been suggested as a likely basis for alterations in cortical processes related to suboptimal DHA status [23]. Like ACP, VEP is considered a functional measure, but it is a measure that is specific to the primary visual cortex. The ACP elicits a behavioral response, which requires integrative cortical processing. Future work should focus on evaluating (1) the maternal DHA status and the ability of infants to integrate visual stimuli, as in face and object recognition, and (2) the relationship of acuity assessed during infancy to vision at a later age, as well as to cognitive processes [24].
References
Neuringer M (2000) Infant vision and retinal function in studies of dietary long-chain polyunsaturated fatty acids: methods, results and implications. Am J Clin Nutr 71:256S–267S
Salomao SR, Ventura DF (1995) Large sample population age norms for visual acuities obtained with vistech-teller acuity cards. Invest Opthalmol Vis Sci 36:657–670
Neuringer M, Connor WE, Barstad L, Luck S (1986) Biochemical and functional effects of prenatal and postnatal n−3 fatty acid deficiency on retina and brain in rhesus monkeys. Proc Natl Acad Sci 83:4021–4025
Carlson SE, Ford AJ, Werkman SH, Peeples JM, Koo WK (1996) Visual acuity and fatty acid status of term infants fed human milk and formulas with and without docosahexaenoate and arachidonate from egg yolk lecithin. Pediatr Res 39:882–888
Jorgensen HM, Hernell O, Lund P, Holmer G, Michaelsen KF (1996) Visual acuity and erythrocyte docosahexaenoic acid status in breast-fed and formula-fed term infants during the first four months of life. Lipids 31:99–105
Birch E, Birch DG, Hoffman DR, Hale L, Everett M, Uauy RD (1993) Breast feeding and optimal visual development. J Pediatr Ophthalmol Strabismus 30:33–38
Hoffman DR, Birch EE, Castaneda YS, Fawcett SL, Wheaton DH, Birch DG, Uauy R (2003) Visual function in breast-fed term infants weaned to formula with or without long-chain polyunsaturates at 4 to 6 months: a randomized clinical trial. J Pediatr 142:669–677
Makrides M, Simmer K, Goggin M, Gibson RA (1993) Erythrocyte docosahexaenoic acid correlates with the visual response of healthy, term infants. Pediatr Res 33:425–427
Makrides M, Neumann M, Simmer K, Pater J, Gibson R (1995) Are long-chain polyunsaturated fatty acids essential nutrients in infancy? Lancet 345:1463–1468
Malcolm CA, McCulloch DL, Montgomery C, Shepherd A, Weaver LT (2003) Maternal docosahexaenoic acid supplementation during pregnancy and visual evoked potential development in term infants: a double blind, prospective, randomized trial. Arch Dis Childhood Fetal Neonatal Ed 88:F383–F390
Malcolm CA, Hamilton R, McCulloch DL, Montgomery C, Weaver LT (2003) Scotopic electroretinogram in term infants born of mothers supplemented with docosahexaenoic acid during pregnancy. Invest Opthalmol Vis Sci 44:3685–3691
Simopoulos AP, Leaf A, Salem N (2000) Workshop statement on the essentiality and recommended dietary intakes for omega-6 and omega-3 fatty acids. Prostaglandins Leukot Essent Fatty Acids 83:119–21
Lewis NM, Widga AC, Buck JS, Frederick AM (1995) Survey of omega-3 fatty acids in diets of midwest low-income pregnant women. J Agromed 2:49–56
Judge MP, Loosemore ED, DeMare CI, Keplinger MR, Mutungi G, Cote S, Ryan M, Ibarolla B, Lammi-Keefe CJ (2003) Dietary docosahexaenoic acid (DHA) intake in pregnant women. J Am Diet Assoc 103:A82
Judge MP, Loosemore ED, Farkas SL, DeMare CI, Keplinger MR, Mutungi G, Cote S, Ryan M, Ibarolla B, Lammi-Keefe CJ (2003) Dietary DHA intake across four ethnic groups. FASEB J 17:71–72
Innis SM, Elias SL (2003) Intakes of essential n−6 and n−3 polyunsaturated fatty acids among pregnant Canadian women. Am J Clin Nutr 77:473–478
Denomme J, Stark KD, Holub BJ (2005) Directly quantitated dietary (n−3) fatty acid intakes of pregnant Canadian women are lower than current dietary recommendations. J Nutr 135:206–211
Teller D (1990) Teller acuity cards (Tac) manual. Vistech Consultants, Inc., Dayton, OH
Hartmann EE, Ellis GS, Morgan KS, Love A, May JG (1990) The acuity card procedure: longitudinal assessments. J Pediatr Opthalmol Strabismus 27:184–187
Mayer LD, Dobson V (1997) Grating acuity cards: validity and reliability in studies of human visual development. Academic, New York, pp 253–292
Freund RJ, Littell RD, Spector PC (2003) SAS System, v9 (TS M0). SAS Institute, Inc., Cary, NC
Nui SL, Mitchell DC, Lim SY, Wen ZM, Kim HY, Salem N, Litman BJ (2004) Reduced G protein-coupled signaling efficiency in retinal rod outer segments in response to n−3 fatty acid deficiency. J Biol Chem 279:31098–31104
Salem N Jr, Litman B, Kim HY, Gawrisch K (2001) Mechanisms of action of docosahexaenoic acid in the nervous system. Lipids 36:945–959
Neuringer M, Jeffrey BG (2003) Visual development: neural basis and new assessment methods. J Pediatr 143:S87–S95
Acknowledgments
We are grateful to so many who were instrumental in making this project a success: the staff at Hartford Hospital (Women’s Ambulatory Health Services) especially, Brunella Ibarrola, Griselle Corcino, Lynn Deasy and Dr. John Greene who appreciated the importance of this work and supported us in establishing subject recruitment and follow-up procedures and provided us with an examination room to conduct our assessments; E. Eugenie Hartmann who provided us with the training and background necessary to establish reliability for the ACP procedures, interpreted results, and who kindly reviewed our manuscript; University of Connecticut graduate students Amber Courville, Charlotte DeMare, Melissa Keplinger, and Elizabeth McArthur, who worked collaboratively in recruitment and follow-up activities. A special thanks to the families from the greater Hartford area who took time from their busy lives to commit to participation in this longitudinal project. Supported in part by USDA IFAFS, Nestec, Ltd., the Hatch Act, the National Fisheries Institute and the American Dietetic Association Foundation.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Judge, M.P., Harel, O. & Lammi-Keefe, C.J. A Docosahexaenoic Acid-Functional Food During Pregnancy Benefits Infant Visual Acuity at Four but not Six Months of Age. Lipids 42, 117–122 (2007). https://doi.org/10.1007/s11745-006-3007-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11745-006-3007-3