Abstract
It is well known that tobacco smoking worsens asthma. Conversely, few data are currently available in the literature on the effects of vaping in asthmatic patients. This work aims to investigate the effects of vaping on asthmatic patients and in asthmatic patients that switched from tobacco smoking to electronic cigarette (e-cig), in particular focusing on quality of life, asthma control, and pulmonary function. We designed a two-group study. One group encompassed vapers with asthma selected through a web survey with questions on quality of life and symptoms worsening; the other group encompassed vapers that switched from tobacco smoking to e-cig, and that volunteered to undergo clinical visits at our outpatient clinic. 2787 people responded to the web survey, including 631 asthmatics. In the second group, 55 volunteers, including 15 asthmatics, were enrolled after a visit. The visit included physical examination and pulmonary function tests (PFT). Internationally validated questionnaires were administered to all subjects: Asthma Control Test (ACT), Asthma Control Questionnaire (ACQ), 36-Item Short Form Survey (SF-36) and Asthma Quality of Life Questionnaire (AQLQ). The 382 asthmatic vapers-only in the web survey were mainly males (86.9%), 31–65 years old. 90% of them declared that vaping did not worsen asthma symptoms and would recommend asthmatic smokers to switch to vaping (98.4%). There was worsening of asthma symptoms due to the actual asthma therapy used by the participants, while no relationship was found with other aspects analysed. In the second group, the analysis of variance in the questionnaires administered to the 10 asthmatics showed a significant improvement in ACQ, ACT and SF-36 for asthmatics that switched from tobacco to vaping, while PFT remained stable throughout the three visits. Almost all of the asthmatics who previously smoked would recommend switching to e-cig, and vaping did not worsen their asthma symptoms. Furthermore, switching from tobacco smoking to e-cigs showed a significant improvement in asthma control and quality of life, not showing, in the period studied, to affect pulmonary function tests.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Asthma is a worldwide problem with more than 300 million affected people [1]. Its prevalence ranges between 1 and 16% of the population in different countries [1, 2]. The World Health Organization (WHO) has estimated that about 15 million years of total life are lost each year for asthma, adjusted for disability, and 350,000 asthma deaths a year are reported worldwide [3]. Asthmatic patients who smoke tobacco have a worse asthma control, have more frequent exacerbations and more hospitalizations, experience a more rapid decline in lung function and an increased risk of death compared to asthmatic patients who are not smokers [4].
Furthermore, asthmatic smokers may have a predominance of neutrophilic inflammation in the airways, therefore poorly responsive to corticosteroid treatment [5, 6].
Usually the liquid used in electronic cigarettes (e-cigs) is a blend, in different proportions, of vegetable glycerol (VG) and propylene glycol (PG) normally 50/50%, but some devices, designed to increase the vapour production, work at their best if powered with liquids composed 70/30, 80/20 or even 99% by VG. Generally, this vapour appears more dense than cigarette smoke, but it dissolves more quickly in the air and proves to be strongly aromatic. It usually contains aromas such as fruit, candies, mint, or other flavours. The e-cigs are marketed in different typologies and configurations, making the vaping market very heterogeneous [7]. However, the basic structure remains common to all the devices and consists of an electrical power supply plus an atomizer. There are mainly two types of atomizers: mouth-to-lung (MTL), whose puff feels like that of a traditional cigarette, with a restricted airflow and usually a single coil, a small chamber and an higher resistance value, and direct-lung-hit (DLH), with a larger airflow, a bigger chamber, one or more coils and a lower resistance value.
The use of e-cigs is growing: the latest report from the United Kingdom estimates the number of users in 2.8 millions [8]. This finding is in keeping with a decrease of the prevalence of traditional cigarette smoke [9]. E-cigs have been recognized as a new technology helpful to reduce traditional cigarettes consumption: in fact, the attempts of smoking cessation through the e-cig increased [10, 11], and e-cigs have been perceived as a gateway to improve the quality of life and life expectation [12, 13]. In the United Kingdom, about 850,000 cigarettes smokers switched to vaping, and other 650,000 “dual users”, which were used to both smoke and vape, have now interrupted both these habits [13, 14].
At present, the number of studies designed to evaluate the security profile of vaping among the population is increasing [13, 14]. Nevertheless, studies on specific population groups, like asthmatics, are still scant [15, 16]. There is an approved trial, which is not recruiting yet, ongoing in Ottawa Hospital Research Institute [17].
Therefore, our work aims to investigate on how the use of e-cig is perceived in asthmatics by a web survey and on how e-cig affects asthma control, quality of life and, as a second aim, pulmonary function tests in a small group of asthmatic vapers.
Methods
Subjects
We designed a two-group study. One group encompassed vapers with asthma selected through a web survey with questions on quality of life and symptoms worsening; the other group encompassed vapers that switched from tobacco smoking to e-cig, and that volunteered to undergo clinical visits at our outpatient clinic. A total of 2842 consecutive volunteers (age range 16–65 years) have been evaluated. 2787 replied to the online questionnaire; furthermore, 55 other adult participants have been examined at our centre. All declared to be active vapers. We included in our analysis from the web survey group, only the questionnaires where the volunteers met the following inclusion criteria: living in Italy, continuous and exclusive e-cigs use, diagnosis of bronchial asthma.
We included in our analysis from the patients seen at our Centre, only the volunteers that met the following inclusion criteria: previous documented asthma diagnosis, exclusive and regular use of e-cig for the entire duration of the study.
Out of 2787 survey participants, 631 stated to be affected by bronchial asthma, 2156 stated to be e-cig users, but not asthmatics, and therefore have been excluded from the study.
Among the 631 participants with asthma, 249 declared to use traditional cigarettes too (“dual users”), and thus have been excluded from the study. All the remaining participants declared to be former smokers. Of the 55 consecutive volunteers examined at our centre, 15 resulted affected by bronchial asthma. Between these 15 vapers with asthma there were 5 dual users that have been excluded from the study.
The remaining 10 patients with asthma agreed to enter in the study protocol. This small group served to reinforce and confirm our survey data.
Thus, in total, 392 asthmatic patients have been examined (382 online questionnaire, 10 online questionnaire and lung function test) (Fig. 1).
Study design
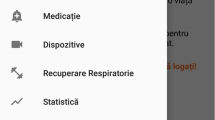
The online questionnaire was created through the modular platform of Google data collection (Google®-Google Forms®), spread on the web through the main social networks (Facebook®, Twitter®). The questionnaires employed are Asthma Control Questionnaire® (ACQ) [18], 36-Item Short Form Survey (SF-36) [19], Asthma Control Test (ACT) [20], Asthma Quality of Life Questionnaire (AQLQ) and a set of questions that aims to differentiate and stratify the patients. The ACQ and ACT are simple questionnaires to measure the adequacy of asthma control and change in asthma control. Instead, the SF-36 and the AQLQ are questionnaires for administered quality-of-life measures: the first one a set of generic, coherent, and easily administered the second an asthma-specific health-related quality of life instrument. All questionnaires are reproducible and validate.
Clinical data have been obtained from the evaluation of volunteers attending the Center for Allergic Respiratory Physiopathology (Department of Internal Medicine) at the University Hospital of Cagliari during the period June 2017–July 2018, immediately prior to the first of the two consecutive follow-ups (check-ups 1 and 2). Follow-ups 1 and 2 have been performed at 3 (± 1) and 6 (± 1) months after the preliminary examination. Informed consent was obtained from all individual participants included in the study.
At each check-up, participants have been re-evaluated through clinical examination, smoking history review, re-evaluation of the compliance and effectiveness of the treatment. Furthermore, the patients have been re-evaluated using the previously mentioned questionnaires, in addition to ACT [20], taking notes of the number of exacerbations since the previous follow-up [21]; spirometry with parameters of forced expiratory flow in 1 s (FEV1), forced vital capacity (FVC), Tiffeneau index (% FEV1/FVC), and forced expiratory flow in the FVC average (FEF 25–75%), spirometry with evaluation of the residual volume through helium dilution technique [22], and carbon monoxide transfer (DLCO) [23] with a Biomedin® spirometer, single membrane filter Spirometry Filter 59 Mada®. Furthermore, the level of exhaled nitric oxide (FeNO) [24] has been evaluated by Vivatmo pro® by Bosch® with mouthpieces Vivatmo pro® Oxycap® by Bosch®.
Statistical analysis
The data collected underwent statistical analysis via IBM SPSS® software version 23.0 and MedCalc version 18.6 [25]. In each case the statistical significance level of the differences observed has been set at a value “p” equal to or less than 0.05 for the two-tailed hypothesis (p ≤ 0.05). It has been decided to compare the nominal data through the use of Contingency tables, based on the evaluation of Pearson χ2 (Chi-square) test and Fisher exact text, in order to adapt the statistical analysis to the sample size; the data expressed as continuous variables have been treated through the Student’s “t” test for independent samples and ANOVA for repeated measures with Bonferroni correction.
Results
Survey
The 382 volunteers from the survey were mainly males 86.9% (n = 332), 47.9% (n = 183) were between 31 and 65 years old. Most of the subjects (70.2%, n = 268) have been using the e-cig for more than a year, with heterogeneous concentration of nicotine and quantity of e-juice vaped per day. The number of volunteers who used a MTL atomizer 44.2% (n = 169) and those who vaped with a DLH atomizer 55.8% (n = 213) (Table 1).
More than half of the participants 61.8% (n = 236) said they had not performed a spirometry in the last year while most of them 81.4% (n = 311) did not take asthma medications at the moment of filling in the questionnaire. A total of 350 volunteers reported no vaping-related worsening of their asthmatic symptoms (91.6%). The majority of them 98.4% (n = 376) would recommend an asthmatic smoker to switch to vaping, claiming in 89.3% (n = 341) of cases to feel better in comparison with the time when they were cigarette smokers (Table 2).
A worsening of respiratory symptoms was reported by 32 participants only: 5.9% (n = 10) of E-Cig MTL users and 10.3% (n = 22) of E-Cig DLH users.
Of these volunteers with symptoms worsening, 31.3% (n = 10) used liquids with 0 mg/ml of nicotine while 65.6% of them (n = 21) used liquids containing 3 mg/ml of nicotine; only one person (3.1%) used liquids with 6 mg/ml of nicotine, none has used liquids with 1.5, 9 and 12 mg/ml of nicotine. These values showed a statistically significant difference (p = 0.025).
Among the 32 volunteers with worsening of respiratory symptoms after using e-cig, 7 (21.9%) used an amount of e-liquid lower than 5 ml/day, 14 (43.8%) used between 5 and 10 ml/day while 11 (34.4%) used an amount between 10 and 30 ml/day, no participant used more than 30 ml/day (Supplementary Table 1). This difference was not statistically significant (p = 0.759).
Furthermore, 15.6% (n = 5) used more than one drug per day for asthma, 12.5% (n = 4) took only one drug per day, 62.5% (n = 20) was not regularly taking therapy (they were using drugs as needed), 9.4% (n = 3) never took any asthma medication. This difference was highly significant (p < 0.001) (Supplementary Table 2). Regarding e-juice aromas, 31.3% (n = 10) used creamy aromas, 28.1% (n = 9) used fruity aromas, 18.8% (n = 6) used tobacco-flavoured liquids and 21.9% (n = 7) used different aromatized liquids (creamy, fruity, tobacco). This difference was not statistically significant (p = 0.305) (Supplementary Table 3).
Outpatients
Concerning the ten asthmatic patients visited at our Centre, the analysis of the AQLQ Score carried out during the three examinations [T0 (baseline visit), T1 (at 3 (± 1) months from the baseline visit) and T2 (at 6 (± 1) months from the baseline visit)] showed a statistically significant positive difference of asthma-related quality of life (p = 0.0041; ANOVA for repeated measures), with an average value per item that highlights the absence of exacerbations in the period evaluated. Globally there is an improvement of the AQLQ score from the baseline visit to the last of 0.44 points. (Table 3, Supplementary Figure 1).
In the same way, the analysis of the variance between the points of ACQ and ACT in the three visits highlights a statistically significant difference (p = 0.0204 for ACQ and p = 0.0021 for ACT) (Figs. 2, 3). Decrease in ACQ score means an improvement in asthma control as an increase in ACT score.
As regards ACT, the comparison between the three examinations highlights a strong statistical difference between T0 and T2 (p = 0.0063) and between T1 and T2 (p = 0.0202), whereas between T0 and T1 it does not reach the statistical significance (p = 0.0529).
Concerning the quality of life, the analysis of the SF-36 highlights a positive trend from T0 to T2, with a progressive increase of the total points and per item. The analysis of the variance for repeated measures on the average of the three examinations points shows a statistically significant change (p = 0.0022). Comparing the single examinations there is a significant difference both between T0 and T1 (p = 0.0233) and between T1 and T2 (p = 0.0194), just like between T0 and T2 (p = 0.0066) (Table 4, Supplementary Figure 2).
Analysis of the variance for repeated measures (ANOVA) for respiratory function tests (FEV1, FVC, PEF, DLCO, FeNO) in the study period did not show any statistically significant difference between the three visits (from the T0 baseline to the T2 6 months) (Supplementary Table 4, Supplementary Figures 3, 4).
Discussion
It is well known that cigarettes smoke contributes to a worsening of bronchial asthma natural history [5, 6, 26], with a decrease in respiratory flows and volumes, a declining responsivity to bronchodilators and an increase in the number of exacerbations in 1 year. On the other hand, recent scientific literature has progressively begun to highlight how vaping proves to be a safe method to quit smoking without showing any alteration in the respiratory function or in the acute phase (i.e. C-reactive protein, erythrocyte sedimentation rate, etc.) in healthy volunteers that use e-cigs [27].
Given the even higher prevalence of cigarette smoking among asthmatic subjects, compared to the general population (21% vs 17%) [28], it is important to find a safe method for the reduction of smoking-related risks in these subjects.
In reading our data there are potential limitations that should be taken into consideration.
As for the survey participants declared themselves asthmatics, but is not medically certified, also there was a greater representation of male volunteers than females (this data could be secondary to the increased spread of vaping among the males).
Instead, outpatient data are limited to a very small group and we wanted to report them into the study as suggestive data. In this group, the “single e-cig user” status was attested by a volunteer statement.
Against this background out of the 382 that filled in the survey, 97.3% declared having perceived an improvement of their “breath” in comparison with the period when they were traditional cigarettes smokers, and the 98.4% would recommend to an asthmatic subject the switch to e-cigs.
The difference among the device employed (“MTL” or “DLH”) and the worsening of symptoms, was not statistically significant. The choice of the two types of atomizers among the asthmatic subjects of our records (44.4% for MTL and 56.6% for DLH) is similar; however, among the 32 that experienced a worsening of the asthmatic symptoms, those using atomizers with pulmonary inhaling (DLH type) are indeed twice than MTL users (22 vs 10). This data, even if not statistically significant, could be explained by the greater quantity of vapour produced by DLH atomizers compared to MTL atomizers, or by the fact that these devices need more elevated wattages compared to the mouth-to-lung setup [29]. This is an interesting data, which surely needs further studies (Supplementary Table 5).
The association between the amount of nicotine present in the liquid used and the worsening of the symptoms appeared strongly significant; however this could be in part altered by the small number of asthmatics that declared a worsening of their symptoms after the e-cigs use (n = 32; 8.4%). Among this 32 participants that claimed to have a symptoms worsening, it is important to consider the possibility that other confounding factors (i.e. environmental or psychological factors) could have had an influence on that [30].
No participants reported worsening of symptoms from the groups with 12 mg/ml, surprisingly, the two groups complaining worsening of symptoms were the users of 3 mg/ml and 0 mg/ml (respectively n = 21 and n = 10 people). Therefore, it appears that minor concentrations of nicotine in this study are linked to an increase in asthma symptoms, but we underline that the groups do not have a homogeneous distribution and 65% of the analysed vapers used 3 mg/ml of nicotine, so although a statistically significant difference is present, definitive conclusions cannot be drawn. Further studies in this regard are undoubtedly necessary (Supplementary Table 6). To our knowledge, this finding has not yet been reported in the literature and needs larger studies to confirm it. As regards the correlation between the type of asthma therapy taken and the symptoms worsening, there was a strong association between the absence of a controller therapy and the exacerbation rate (a flare-up or exacerbation is an acute or sub-acute worsening in symptoms and lung function from the patient’s usual status; occasionally it may be the initial presentation of asthma [31]), which is an expected result. It is well known from the literature that asthmatic patients are often non-compliant to the proposed treatments [32, 33] and this could explain the high percent of volunteers we found that not take medications.
Out of the ten outpatients analysed at our clinic during the period of the study, no changes in respiratory function parameters have been noted, that is probably linked to the quite short period of observation for this study. The values of exhaled nitric oxide (FeNO) is reduced in some of the subjects; this finding, although not statistically significant, in our opinion, is probably related to both the absence of an irritating agent such as smoke and to a better compliance, probably also related to the commitment to our study.
The analysis of the questionnaires showed an improvement in the quality of life perception and of breath which is strongly statistically significant, with a trend of the AQLQ, ACQ, ACT and SF-36 points showing a clear improvement during the three follow-ups.
It is interesting to see how the subjective perception of the e-cigs users on their breath and on their quality of life is positive compared to their past as smokers; also in the analysis of the questionnaires given to the outpatients, it can be noticed how asthma control and quality of life had both a statistically significant improvement during the 6 months period of this study.
In conclusion, our data are in agreement with the few studies already present in literature about vaping, which today proves to be one of the most effective methods to quit smoking and thus reduce smoke-related damages [27, 34].
Asthma control, asthma-related quality of life and general health perception are improved in asthmatic vapers, compared to their previous tobacco smoker life.
A total of 350 volunteers reported no vaping-related worsening of their asthmatic symptoms (91.6%). The majority of them would recommend an asthmatic smoker to switch to vaping, claiming in about 90% of cases to feel better in comparison with the time when they were cigarette smokers.
Analysing the AQLQ score in the ten asthmatic patients visited at our Centre during the three examinations there was a statistically significant positive trend, with an improvement of the asthma-related quality of life. In the same way we saw a positive trend on the asthma control between the three visits, with no modifications on lung function tests. Results of our study agree with previous researches on asthma and vaping present in medical literature [16].
Our preliminary data, together with the lack of studies on vaping in asthmatic patients, suggest continuing with further studies on this topic, with longer follow-up to determine with more certainty the security profile of vaping in general and in cohorts of more “at-risk” patients, such as asthmatics.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Matthew M, Denise F, Shaun H, Richard B (2004) The global burden of asthma: executive summary of the GINA Dissemination Committee Report. Allergy 59(5):469–478. https://doi.org/10.1111/j.1398-9995.2004.00526.x
Lai CKW, Beasley R, Crane J, Foliaki S, Shah J, Weiland S (2009) Global variation in the prevalence and severity of asthma symptoms: Phase Three of the International Study of Asthma and Allergies in Childhood (ISAAC). Thorax 64(6):476–483. https://doi.org/10.1136/thx.2008.106609
Bateman ED, Hurd SS, Barnes PJ, Bousquet J, Drazen JM, FitzGerald JM, Gibson P, Ohta K, O'Byrne P, Pedersen SE, Pizzichini E, Sullivan SD, Wenzel SE, Zar HJ (2008) Global strategy for asthma management and prevention: GINA executive summary. Eur Respir J 31(1):143–178. https://doi.org/10.1183/09031936.00138707
Thomson NC, Chaudhuri R, Livingston E (2004) Asthma and cigarette smoking. Eur Respir J 24(5):822–833. https://doi.org/10.1183/09031936.04.00039004
Chalmers GW, Macleod KJ, Little SA, Thomson LJ, McSharry CP, Thomson NC (2002) Influence of cigarette smoking on inhaled corticosteroid treatment in mild asthma. Thorax 57(3):226–230
Chaudhuri R, Livingston E, McMahon AD, Thomson L, Borland W, Thomson NC (2003) Cigarette smoking impairs the therapeutic response to oral corticosteroids in chronic asthma. Am J Respir Crit Care Med 168(11):1308–1311. https://doi.org/10.1164/rccm.200304-503OC
Barrington-Trimis JL, Gibson LA, Halpern-Felsher B, Harrell MB, Kong G, Krishnan-Sarin S, Leventhal AM, Loukas A, McConnell R, Weaver SR (2018) Type of e-cigarette device used among adolescents and young adults: findings from a pooled analysis of eight studies of 2166 vapers. Nicotine Tob Res 20(2):271–274. https://doi.org/10.1093/ntr/ntx069
Bauld L, MacKintosh AM, Eastwood B, Ford A, Moore G, Dockrell M, Arnott D, Cheeseman H, McNeill A (2017) Young people’s use of e-cigarettes across the United Kingdom: findings from five surveys 2015–2017. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph14090973
Brown J, West R, Beard E, Michie S, Shahab L, McNeill A (2014) Prevalence and characteristics of e-cigarette users in Great Britain: findings from a general population survey of smokers. Addict Behav 39(6):1120–1125. https://doi.org/10.1016/j.addbeh.2014.03.009
Brown J, Beard E, Kotz D, Michie S, West R (2014) Real-world effectiveness of e-cigarettes when used to aid smoking cessation: a cross-sectional population study. Addiction (Abingdon, England) 109(9):1531–1540. https://doi.org/10.1111/add.12623
Rahman MA, Hann N, Wilson A, Mnatzaganian G, Worrall-Carter L (2015) E-cigarettes and smoking cessation: evidence from a systematic review and meta-analysis. PLoS ONE. https://doi.org/10.1371/journal.pone.0122544
Tombor I, Shahab L, Herbec A, Neale J, Michie S, West R (2015) Smoker identity and its potential role in young adults' smoking behavior: a meta-ethnography. Health Psychol 34(10):992–1003. https://doi.org/10.1037/hea0000191
Etter JF (2017) Electronic cigarette: a longitudinal study of regular vapers. Nicotine Tob Res. https://doi.org/10.1093/ntr/ntx132
Farsalinos KE, Poulas K, Voudris V, Le Houezec J (2016) Electronic cigarette use in the European Union: analysis of a representative sample of 27 460 Europeans from 28 countries. Addiction (Abingdon, England) 111(11):2032–2040. https://doi.org/10.1111/add.13506
Polosa R, Caponnetto P, Niaura R, Abrams D (2017) Analysis of E-cigarette use in the 2014 Eurobarometer survey: calling out deficiencies in epidemiology methods. Intern Emerg Med 12(6):733–735. https://doi.org/10.1007/s11739-017-1667-z
Polosa R, Morjaria J, Caponnetto P, Caruso M, Strano S, Battaglia E, Russo C (2014) Effect of smoking abstinence and reduction in asthmatic smokers switching to electronic cigarettes: evidence for harm reversal. Int J Environ Res Public Health 11(5):4965–4977. https://doi.org/10.3390/ijerph110504965
Institute OHR (2019) E-Cigarette Inner City RCT [ClinicalTrials.gov Identifier: NCT03249428]. https://clinicaltrials.gov/ct2/show/NCT03249428?term=e-cig&cond=Asthma&rank=1
Juniper EF, Svensson K, Mork AC, Stahl E (2005) Measurement properties and interpretation of three shortened versions of the asthma control questionnaire. Respir Med 99(5):553–558. https://doi.org/10.1016/j.rmed.2004.10.008
Ware JE Jr, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30(6):473–483
Schatz M, Sorkness CA, Li JT, Marcus P, Murray JJ, Nathan RA, Kosinski M, Pendergraft TB, Jhingran P (2006) Asthma Control Test: reliability, validity, and responsiveness in patients not previously followed by asthma specialists. J Allergy Clin Immunol 117(3):549–556. https://doi.org/10.1016/j.jaci.2006.01.011
Chung KF, Wenzel SE, Brozek JL, Bush A, Castro M, Sterk PJ, Adcock IM, Bateman ED, Bel EH, Bleecker ER, Boulet LP, Brightling C, Chanez P, Dahlen SE, Djukanovic R, Frey U, Gaga M, Gibson P, Hamid Q, Jajour NN, Mauad T, Sorkness RL, Teague WG (2014) International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur Respir J 43(2):343–373. https://doi.org/10.1183/09031936.00202013
Patroniti N, Bellani G, Manfio A, Maggioni E, Giuffrida A, Foti G, Pesenti A (2004) Lung volume in mechanically ventilated patients: measurement by simplified helium dilution compared to quantitative CT scan. Intensive Care Med 30(2):282–289. https://doi.org/10.1007/s00134-003-2109-0
Macintyre N, Crapo RO, Viegi G, Johnson DC, van der Grinten CP, Brusasco V, Burgos F, Casaburi R, Coates A, Enright P, Gustafsson P, Hankinson J, Jensen R, McKay R, Miller MR, Navajas D, Pedersen OF, Pellegrino R, Wanger J (2005) Standardisation of the single-breath determination of carbon monoxide uptake in the lung. Eur Respir J 26(4):720–735. https://doi.org/10.1183/09031936.05.00034905
Dweik RA, Boggs PB, Erzurum SC, Irvin CG, Leigh MW, Lundberg JO, Olin AC, Plummer AL, Taylor DR (2011) An official ATS clinical practice guideline: interpretation of exhaled nitric oxide levels (FENO) for clinical applications. Am J Respir Crit Care Med 184(5):602–615. https://doi.org/10.1164/rccm.9120-11ST
Schoonjans F, Zalata A, Depuydt CE, Comhaire FH (1995) MedCalc: a new computer program for medical statistics. Comput Methods Progr Biomed 48(3):257–262
Groneberg DA, Quarcoo D, Frossard N, Fischer A (2004) Neurogenic mechanisms in bronchial inflammatory diseases. Allergy 59(11):1139–1152. https://doi.org/10.1111/j.1398-9995.2004.00665.x
Polosa R, Cibella F, Caponnetto P, Maglia M, Prosperini U, Russo C, Tashkin D (2017) Health impact of e-cigarettes: a prospective 3.5-year study of regular daily users who have never smoked. Sci Rep 7(1):13825. https://doi.org/10.1038/s41598-017-14043-2
Prevention, C.f.D.C.a., Percentage of people with asthma who smoke. Published January 31, 2013. Accessed January 14, 2017
Adam (2018) Mouth to lung (MTL) vs direct to lung (DTL) vaping: a full guide on different vaping styles. Ecigology
Beatriz GF, Isabel V, Pertega-Diaz S (2019) The relationship of psychological factors and asthma control to health-related quality of life. J Allergy Clin Immunol Pract. https://doi.org/10.1016/j.jaip.2019.07.009
Asthma GIf (2017) Global strategy for asthma management and prevention (2017 update). https://www.ginasthma.org
Cochrane MG, Bala MV, Downs KE, Mauskopf J, Ben-Joseph RH (2000) Inhaled corticosteroids for asthma therapy: patient compliance, devices, and inhalation technique. Chest 117(2):542–550. https://doi.org/10.1378/chest.117.2.542
Gamble J, Stevenson M, McClean E, Heaney LG (2009) The prevalence of nonadherence in difficult asthma. Am J Respir Crit Care Med 180(9):817–822. https://doi.org/10.1164/rccm.200902-0166OC
Polosa R, Caponnetto P (2016) The health effects of electronic cigarettes. N Engl J Med 375(26):2608
Funding
None to declare from all of the authors relevant to this work.
Author information
Authors and Affiliations
Contributions
All the authors have contributed in the preparation of this paper and have approved its final version and submission.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest.
Human and animal rights
All human and animal studies have been approved by the appropriate ethics committee and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Solinas, A., Paoletti, G., Firinu, D. et al. Vaping effects on asthma: results from a web survey and clinical investigation. Intern Emerg Med 15, 663–671 (2020). https://doi.org/10.1007/s11739-019-02247-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-019-02247-5