Abstract
Hemoptysis is a life-threatening complication of Behcet’s disease that is likely related to pulmonary artery aneurysm (PAA). Vascular interventional radiology may offer effective emergency therapeutic option, but has not been thoroughly investigated in this setting. A case series of a French referral center for hemoptysis combined with a literature review of case reports was conducted. Between 1995 and 2016, 12 patients were referred to our center for hemoptysis revealing or complicating the course of Behcet’s disease. Pulmonary artery aneurysm (PAA) was the mechanism of hemoptysis in ten patients, nine of whom were treated by a transcatheter embolotherapy. Combining an additional 8 case reports from the literature, 17 patients treated by transcatheter embolotherapy for PAA were analyzed. The duration of the course of Behcet’s disease was 22 months [IQR 3–45] at the time of PAA diagnosis. Transcatheter embolotherapy of PAA was successful for immediately controlling hemoptysis in all patients, without major complication except for one. Hemoptysis recurred in seven patients (41%) within 5 months [IQR 1–12]. The use of coils for transcatheter embolotherapy was associated with hemoptysis recurrence. A bronchosystemic hypervascularization related to the previously occluded PAA was the main mechanism of bleeding recurrence, leading to bronchosystemic artery embolization in four patients and surgery in two patients. Behcet’s disease-related hemoptysis is mainly due to PAA. Transcatheter embolotherapy should be considered as the first-line emergency treatment for PAA-related hemoptysis, in association with the immunosuppressive regimen. Hemoptysis may recur in half of the cases, involving preferentially a bronchosystemic arterial mechanism.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Vascular arterial and venous involvement may occur in up to 40% of patients with Behcet’s disease [1,2,3,4,5] and is the most common cause of mortality [2]. Arterial lesions including thrombosis and aneurysm formation are described in 1–12% of patients [5,6,7,8,9], but their prevalence may be underestimated considering postmortem findings [10]. The prevalence of pulmonary artery aneurysm (PAA) during Behcet’s disease averages 1% [11, 12]. Behcet-related PAAs are almost always associated with hemoptysis [2, 12,13,14,15], whereas other Behcet-related pulmonary vascular lesions, including pulmonary artery thrombosis or small size vessels, are less frequently associated with such events [12, 16]. PAAs are associated with a high mortality rate, exceeding 20% at 1 year [11,12,13, 17]. Prompt treatment should be considered. Emergency surgery may be a therapeutic option, but may be challenging owing to technical difficulty as well as to a high mortality rate when performed during active bleeding [18, 19]. Transcatheter embolotherapy of PAA may be a suitable option, but the published experiences remain limited to a few case reports.
We aim to describe the clinical spectrum, the management and the short- and long-term outcomes of consecutive Behcet patients admitted to the intensive care unit for severe hemoptysis treated with transcatheter embolotherapy of PAA. We also review the case reports issued from the literature. This study was conducted in accordance with the French law, which does not require approval of an institutional review board or the consent of patients for such a retrospective analysis of medical records.
Methods
Selection of patients
We conducted a single-center analysis of a prospective registry of consecutive patients with severe hemoptysis admitted to the intensive care unit (ICU) of Tenon Hospital, a tertiary teaching hospital and referral center for hemoptysis in Paris, France, between May 1995 and March 2016. All consecutive patients admitted to the ICU for Behcet’s disease-related hemoptysis were included.
Behcet’s disease diagnosis
Behcet’s disease was diagnosed according to the International Criteria for Behcet’s Disease (ICBD), which uses a point score system [20]. Patients having a Hughes–Stovin syndrome were also included [21, 22].
Data collection
Demographic data included age, gender and country of origin. The dates of Behcet and PAA diagnoses were recorded. The diagnostic circumstances of the pulmonary aneurysmal disease (hemoptysis, general signs or fortuitously) were assessed. Times from the onset of Behcet’s disease to the diagnosis of PAA and from the diagnosis of PAA to the embolization procedure were considered. Initial CT scans were reviewed by a radiologist (AK, MFC); the number of PAA was assessed; ground-glass opacities around PAA or air bubble within the aneurismal sac located the bleeding site; the presence of a bronchosystemic hypervascularization was sought, particularly in the area of PAA. Modalities of PAA transcatheter embolotherapy were collected, including the type of embolic agent, the site of occlusion (aneurysmal sac or neck) and the number of embolized PAA. The immunosuppressive regimens and anticoagulant and antiplatelet therapies were collected. Follow-up data included recurrence of hemoptysis, time from transcatheter embolotherapy to recurrence, need for additional interventional radiology procedure, need for surgical lung resection and death. Lung resection pieces were stained with hematein–safran–eosin and examined under a light microscope.
Literature review
We undertook a literature review regarding other cases of PAA complicating Behcet’s disease for which a transcatheter embolotherapy has been performed, using computerized Medline and Web of Science searches. The terms used included “Behcet’s syndrome”, “Behcet syndrome”, “Behcet’s disease”, “Behcet disease”, “Hughes–Stovin syndrome”, “hemoptysis” and “embolization”. This search was restricted to English language articles. Data using the above standardized procedure were extracted.
Statistical analysis
Continuous and categorical variables were expressed as median [interquartile range 25–75] and number (percentage), respectively. Comparisons of continuous variables were made using the Mann–Whitney U test. Comparisons of proportions were made using the Chi2 test. The level of significance for all statistical tests was 2-sided, p < 0.05.
Results
Case series from Tenon Hospital
During the study period, 1761 patients were referred to our ICU for hemoptysis (Fig. 1). Among them, 12 patients had a Behcet’s disease (n = 10) or a Hughes–Stovin syndrome (n = 2) (Supplementary Table 1). A PAA was present in all patients at the time of initial management. Three patients did not undergo transcatheter embolotherapy. The first one suffered a massive hemoptysis related to a unique left inferior PAA, which was complicated by a cardiac arrest. Despite an emergent surgical lobectomy, the patient developed an anoxic encephalopathy and died. The two other patients had multiple and bilateral PAA, with no radiological sign of bleeding from PAA. Hemoptysis was related to a systemic hypervascularization and was controlled by bronchial artery embolization. Altogether, PAA was present in all patients at ICU referral and was involved in the mechanism of bleeding in ten patients (83%), leading to a transcatheter embolotherapy in nine of them (Fig. 1).
Case reports form the literature
Altogether, 17 patients with Behcet’s disease and hemoptysis treated with PAA transcatheter embolotherapy were identified from the literature review [9, 12, 14, 23,24,25,26,27,28,29,30,31,32]. Among them, nine were excluded because of the limited information regarding the transcatheter embolotherapy procedure [9, 12, 14, 23, 31] and two were excluded because of the use of a promising, but still restricted technique [24, 32] (Fig. 1). Clinical data were missing for two patients (Supplementary Table 2).
Pulmonary artery aneurysms
Overall, 17 patients were analyzed (Table 1). Sixteen were men, aged 32 years [IQR 24–41]. Ten patients (59%) had a previous history of venous thrombus disease, including deep vein thrombosis and superficial vein thrombophlebitis of lower and upper extremities, and large vein thrombosis (Supplementary Table 2). The median duration of Behcet’s disease before the diagnosis of PAA was 22 months [IQR 3–45]. Hemoptysis was the inaugural symptom of PAA in 14 patients (82%). Most patients (n = 11; 65%) exhibited more than one PAA, with a median number of 3 PAA [IQR 1–5]. The time elapsed from the diagnosis of PAA to the transcatheter embolotherapy was 1 month [IQR 0–12] and was significantly shorter in our series, as compared to the published cases (0 month [IQR 0–1] vs. 9 months [IQR 0–33]; p = 0.04).
Ten of the 17 patients (59%) received immunosuppressive regimens before TCE: four of our nine patients (44%) received corticosteroids with cyclophosphamide, whereas six of the eight patients (75%) found in the literature were treated by corticosteroids plus cyclophosphamide (n = 4) or corticosteroids alone (n = 2). Six of those ten patients were treated with immunosuppressive drugs for more than 12 months before TCE; the size of all the PAA decreased in three of them, based on iterative CT examinations performed in the months before TCE.
Transcatheter embolotherapy of pulmonary artery aneurysm
A PAA transcatheter embolotherapy was performed in all patients (Figs. 2, 3). In our center, the preferential technique of embolization used coils and was based on the occlusion of the aneurismal sac, in the absence of identification of the aneurismal neck (Table 2), in contrast to the literature case reports in which the neck was more frequently occluded. Three complications occurred after the procedure, including worsening of a preexisting pulmonary hypertension (n = 1) and pulmonary infarct (n = 2). Bronchial arteries were hypertrophic in two patients who underwent a concomitant bronchial artery embolization using coils. Immediate control of bleeding was achieved in all patients.
Pulmonary artery aneurysm occlusion: case report illustration. A 24-year-old was admitted to our department for hemoptysis. Twelve months earlier, he was diagnosed with Behcet's disease. A combination of immunosuppressive drugs (cyclophosphamide, corticosteroids and colchicine) was initiated. A CT scan was performed. a The axial CT scan on mediastinal windows showed multiple pulmonary artery aneurysms associated with a pulmonary artery wall thickening (arrowheads). b Sagittal reconstructions with parenchymal windows showed ground-glass opacities (arrow) beyond the pulmonary artery aneurysm. c Sagittal reconstructions with mediastinal windows at the same level showed the rupture of the pulmonary artery aneurysm (arrow) and the thickening of the pulmonary artery parietal walls (arrowheads). A pulmonary angiography was performed. d The selective pulmonary artery angiogram showed the pulmonary artery aneurysm (arrow) and its rupture within the pulmonary parenchyma (arrowhead). e A control pulmonary artery angiogram after pulmonary artery aneurysm occlusion showed the pulmonary artery aneurysm exclusion. The bleeding stopped. Nine months later, a CT scan was performed. f The axial CT scan showed the disappearance of both the pulmonary artery aneurysm and the pulmonary artery wall thickening
Surgical lung resection for bleeding recurrence: case report illustration. A 27-year-old patient was admitted to our department for massive hemoptysis. Seven years earlier, he was diagnosed with Behcet’s disease. Several combinations of immunosuppressive therapy were successively used, the last one combining colchicine, corticosteroids and oral cyclophosphamide. A CT scan was performed. a Sagittal reconstructions with parenchymal windows showed ground-glass opacities (asterisk) beyond a pulmonary artery aneurysm with an air bubble within the pulmonary artery aneurysm wall (arrow). b Sagittal reconstructions with mediastinal windows at the same level clearly showed pulmonary artery aneurysm (asterisk), the air bubble within the pulmonary artery aneurysm wall (arrow) and the thickening of the pulmonary artery aneurysm wall (arrowhead) related to the inflammation process. A pulmonary artery angiography was performed. c The superselective angiogram revealed a pulmonary artery aneurysm arising from the posterior segmental artery from the right lower pulmonary artery. d The pulmonary artery aneurysm sac was occluded with coils. Nineteen months later, hemoptysis recurred and was related to a systemic hypervascularization. e A CT scan with sagittal reconstructions showed artifacts related to coils (black arrows) and ground-glass opacities related to the bleeding (white arrow). f The axial slices with maximum intensity projection showed the enlargement of the bronchial arteries (arrows). Two procedures of bronchial artery embolization did not control the bleeding, leading to performing a right lower lobectomy. The patient is still alive without recurrence at 19 months post-surgery
Follow-up after transcatheter embolotherapy
The follow-up duration after PAA transcatheter embolotherapy was 12 months [IQR 10-33]. Fifteen patients (88%) received a long-term immunosuppressive treatment after transcatheter embolotherapy: 13 patients were treated by monthly pulse of cyclophosphamide and daily pulse of corticosteroids followed by oral daily prednisone, in addition to daily colchicine for two patients; the remaining two patients received corticosteroids and colchicine. The PAA decreased in size in five patients and disappeared in one. Conversely, the PAA showed an increase in size despite immunosuppressive treatment in one patient, who underwent a right inferior lobectomy to prevent the risk of fatal bleeding recurrence.
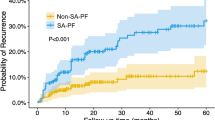
Hemoptysis recurred after 5 months [IQR 1–12] in seven patients, including three of our series and four of the literature review. The mechanism of the recurrence was neither related to the erosion nor the rupture of PAA, but to the development of a bronchosystemic hypervascularization. A bronchial artery embolization was performed in four patients and was successful in two. Surgery was considered necessary for the remaining two patients: the first patient underwent a right inferior lobectomy (Fig. 3); the other one underwent a right middle lobectomy, but died because of the abnormal origin of the right coronary artery between the pulmonary artery trunk and the aortic root [33].
The overall 1-year mortality rate was 24% (4/17). Two deaths were related to hemoptysis. The other deaths were related to surgery (n = 1) and to worsening pulmonary hypertension (n = 1).
Risk factors of recurrence of hemoptysis after transcatheter embolotherapy
We searched the literature to identify the factors associated with the recurrence of hemoptysis (Table 3). The following cases were excluded to achieve a consistent analysis: (1) incomplete data on the location of PAA embolization (n = 1) [28]; (2) initial management including straightaway a bronchial artery embolization (n = 2); (3) follow-up duration of less than 1 month after transcatheter embolotherapy (n = 1). Overall, 13 patients were included in the analysis. Six of them (46%) experienced at least one episode of bleeding recurrence during follow-up. The use of coils for PAA transcatheter embolotherapy was significantly associated with the recurrence of hemoptysis (p = 0.025). Moreover, we noted a trend to a higher frequency of multi-site aneurismal disease in patients with at least one bleeding recurrence (p = 0.18).
Lung pathology
Finally, we aim to describe the mechanisms involved in the recurrence of hemoptysis after transcatheter embolotherapy of PAA using coils, by examining lung surgical resection in two patients. The first patient had a bleeding recurrence 19 months after embolotherapy (Fig. 3). Two procedures of bronchial artery embolization failed to control hemoptysis, leading to carrying out a right lower lobectomy. The removed lobe was examined. The pulmonary artery was thrombosed and repermeabilized. The material of embolization was observed close to the pulmonary artery parietal wall, which displayed a marked fibrosis (Supplementary Fig. 1). The second patient had a bleeding recurrence 1 month after transcatheter embolotherapy of a PAA located in the right middle lobe using 2.07 m of coils. A bronchial artery embolization effected control of hemoptysis transiently, but the bleeding recurred 4 months later. Two additional procedures of systemic artery embolization failed to control the bleeding, leading to a right middle lobectomy. The removed lobe was examined. The pulmonary artery was thrombosed. Materials of systemic artery embolization were observed in the lumens of both the pulmonary artery and the adjacent systemic arteries. A marked systemic hypervascularization was observed around the thrombosed pulmonary artery. Macrophage infiltrates were observed within the pulmonary artery thrombus; lymphocytes and macrophage infiltrates were observed within the pulmonary artery parietal wall (Supplementary Fig. 2).
Discussion
We describe the clinical spectrum, the management and the outcomes of 17 patients with Behcet’s disease and severe hemoptysis during a 20-year period, combining a case series from a referral center and literature case reports. Hemoptysis revealed PAA in 14 patients (82%). More than half of the patients had at least two PAAs. Transcatheter embolotherapy achieved an initial control of bleeding in all patients. An acute exacerbation of a preexisting pulmonary hypertension was the unique major complication. Hemoptysis recurred in 41% of the patients during a median follow-up of 12 months and was mainly related to a bronchosystemic mechanism that might be linked to the embolization technique (coils).
Behcet’s disease is a vasculitis usually affecting large vessels of the lungs [13, 34]. Mechanisms of hemoptysis during Behcet’s disease may involve either the alveolar–capillary unit (specific capillaritis) or the bronchial tract that may be related to the erosion of PAA into the bronchi or to the development of a systemic arterial hypervascularization. Because the mechanisms and the therapeutic approaches may strongly differ, the first challenge is to locate the bleeding and to assess its mechanism. PAA is the main mechanism of hemoptysis. We also show that a primary bronchosystemic hypervascularization is rarely involved (Supplementary Table 1). No case of hemoptysis due to a diffuse alveolar hemorrhage was recorded [35].
Consistently with previous series [2, 12,13,14], PAA affects mainly young men and is often revealed by hemoptysis. Two-thirds of the patients have more than one PAA, highlighting the fact that a CT scan evaluation is essential to identify the number and the location of PAAs, as well as to determine which PAA is involved in the bleeding process [36]. In our patients, air bubbles were present within the wall of PAA in three patients and ground-glass opacities within the area of PAA in six.
The recommended specific medical treatment of Behcet’s disease-related hemoptysis is a combination of intravenous pulse of methylprednisolone and cyclophosphamide [37, 38]. Regression in size or disappearance of PAA after this drug combination is well established, but may require several months [12, 39]. However, immunosuppressive regimens do not protect against a fatal bleeding recurrence. Therefore, vascular interventional radiology or surgical lung resection should be considered in an emergency. There are several arguments against emergency surgical lung resection in that setting: (1) first, thoracic surgery should be avoided during active bleeding [18]; (2) second, surgery may lead to a large pulmonary amputation in patients with a recurrent disease affecting both lungs and at risk of infectious complications [19, 40]; (3) third, anastomotic dehiscence and recurrence of aneurysm at anastomotic vascular sites have been reported [39, 41]. Therefore, emergency vascular interventional radiology should be considered as the technique of choice in that setting. In our study, PAA transcatheter embolotherapy, in association with a bronchial artery embolization in two patients, allowed an immediate control of bleeding in all cases.
The technique of transcatheter embolotherapy may vary from a center to another. Some may use coils, while others favor liquid agents (n-butyl-cyanoacrylate, NBCA or ethylene-vinyl-alcohol copolymer, onyx). During the procedure, the location of embolic agents drop may depend of the PAA anatomic features. A superselective neck embolization is not always achievable, especially when the neck is short or absent, or when the catheter is unstable. In the present series, coils were used in nine patients (7 patients from our center and 2 patients from literature), and the embolization of the aneurismal neck was performed in seven patients (2 patients from our center and 5 patients from literature). The differences observed in the techniques of embolization might be explained by the PAA anatomical features or by the local technical practices.
Several mechanisms may be involved in the recurrence of hemoptysis after PAA transcatheter embolotherapy: incomplete procedure, rupture of another PAA, pulmonary embolism, or alveolar diffuse hemorrhage. A bronchosystemic hypervascularization should be considered as well [29]. PAA occlusion may cause a local ischemia of the downstream pulmonary parenchyma, leading to the opening of physiological bronchosystemic to pulmonary artery precapillary shunts. This is illustrated in Supplementary Fig. 2(A, B), which shows materials of bronchosystemic embolization within pulmonary artery. The healing process associated with the decrease in size of PAAs, particularly under immunosuppressive regimen, may also be involved [42]. This is illustrated in Supplementary Fig. 1, which shows a marked fibrosis of the pulmonary artery parietal wall. Our study raises a third hypothesis related to the abundant material used in fulfilling the aneurysmal sac during PAA embolotherapy, i.e., more than 200 cm of coils for two patients in our series, which may have promoted a local inflammatory process with the development of neovessels. This is illustrated in Supplementary Fig. 2 (B, C, D, E), which shows a marked systemic hypervascularization around the thrombosed pulmonary artery and leucocytes infiltrates within the pulmonary artery parietal wall. In our series, hemoptysis recurred in seven patients after 5 months. The recurrence of hemoptysis was mainly related to a bronchosystemic arterial hypervascularization, and was significantly associated with the use of coils for PAA transcatheter embolotherapy. All recurrences were managed with bronchosystemic artery embolization. However, an emergency surgery was necessary to control the bleeding in two cases.
Our study suffers from several limitations. First, some clinical data were unavailable, especially from cases reported in the literature. Second, the inclusion of patients with Hughes–Stovin syndrome might be criticized, since this entity does not fulfill the diagnosis criteria of Behcet’s disease. However, both entities display numerous similarities, regarding clinical, radiological and histopathological features, leading some authors to describe Hughes–Stovin syndrome as an incomplete form of Behcet’s disease [13, 21, 22, 43, 44]. Moreover, Hughes–Stovin syndrome and Behcet’s disease are the only vasculitides associated with the development of pulmonary artery aneurysms [22]. Elsewhere, some authors included patients with Hughes–Stovin syndrome in studies describing Behcet-related vascular lesions [9, 13]. Third, the retrospective nature of our study over a long time period could bring confounding problems. Diagnosis procedures and treatments might have evolved. Finally, the number of patients is small, preventing any firm conclusions.
In summary, PAA is by far the main mechanism of hemoptysis during Behcet’s disease. Transcatheter embolotherapy should be considered as the key therapeutic option for PAA-related hemoptysis, in association with the administration of immunosuppressive regimen. Hemoptysis recurs frequently, involving a bronchosystemic mechanism that might be related to the occlusion technique.
Abbreviations
- BAE:
-
Bronchial artery embolization
- BD:
-
Behcet’s disease
- BHV:
-
Bronchial hypervascularization
- F:
-
Female
- GS:
-
Gelfroam sponge
- HSS:
-
Hughes–Stovin syndrome
- ICU:
-
Intensive care unit
- IQR:
-
Interquartile range
- M:
-
Male
- NA:
-
Not available
- Nb:
-
Number
- NBCA:
-
n-Butyl-cyanoacrylate
- PAA:
-
Pulmonary artery aneurysm
- PE:
-
Pulmonary embolism
- TCE:
-
Transcatheter embolotherapy
References
Tunaci A, Berkmen YM, Gokmen E (1995) Thoracic involvement in Behcet’s disease: pathologic, clinical, and imaging features. AJR Am J Roentgenol 164(1):51–56
Kural-Seyahi E, Fresko I, Seyahi N, Ozyazgan Y, Mat C, Hamuryudan V et al (2003) The long-term mortality and morbidity of Behcet syndrome: a 2-decade outcome survey of 387 patients followed at a dedicated center. Medicine (Baltim) 82(1):60–76
Ideguchi H, Suda A, Takeno M, Ueda A, Ohno S, Ishigatsubo Y (2011) Behcet disease: evolution of clinical manifestations. Medicine (Baltim) 90(2):125–132
Sarica-Kucukoglu R, Akdag-Kose A, KayabalI M, Yazganoglu KD, Disci R, Erzengin D, Azizlerli G (2006) Vascular involvement in Behçet’s disease: a retrospective analysis of 2319 cases. Int J Dermatol 45(8):919–921
Emmi G, Silvestri E, Squatrito D, Amedei A, Niccolai E, D’Elios MM, Della Bella C, Grassi A, Becatti M, Fiorillo C, Emmi L, Vaglio A, Prisco D (2015) Thrombosis in vasculitis: from pathogenesis to treatment. Thromb J 13:15
Hamza M (1987) Large artery involvement in Behcet’s disease. J Rheumatol 14(3):554–559
Calamia KT, Schirmer M, Melikoglu M (2005) Major vessel involvement in Behcet disease. Curr Opin Rheumatol 17(1):1–8
Houman MH, Neffati H, Braham A, Harzallah O, Khanfir M, Miled M et al (2007) Behcet’s disease in Tunisia. Demographic, clinical and genetic aspects in 260 patients. Clin Exp Rheumatol 25(4 Suppl 45):S58–S64
Saadoun D, Asli B, Wechsler B, Houman H, Geri G, Desseaux K et al (2012) Long-term outcome of arterial lesions in Behcet disease: a series of 101 patients. Medicine (Baltim) 91(1):18–24
Lakhanpal S, Tani K, Lie JT, Katoh K, Ishigatsubo Y, Ohokubo T (1985) Pathologic features of Behcet’s syndrome: a review of Japanese autopsy registry data. Hum Pathol 16(8):790–795
Hamuryudan V, Yurdakul S, Moral F, Numan F, Tüzün H, Tüzüner N et al (1994) Pulmonary arterial aneurysms in Behcet’s syndrome: a report of 24 cases. Br J Rheumatol 33(1):48–51
Seyahi E, Melikoglu M, Akman C, Hamuryudan V, Ozer H, Hatemi G et al (2012) Pulmonary artery involvement and associated lung disease in Behcet disease: a series of 47 patients. Medicine (Baltim) 91(1):35–48
Uzun O, Akpolat T, Erkan L (2005) Pulmonary vasculitis in Behcet disease: a cumulative analysis. Chest 127(6):2243–2253
Hamuryudan V, Er T, Seyahi E, Akman C, Tüzün H, Fresko I et al (2004) Pulmonary artery aneurysms in Behcet syndrome. Am J Med 117(11):867–870
Gebitekin C, Yilmaz M, Senkaya I, Saba D, Sağdiç K, Ozer G (1997) Fatal haemoptysis due to pulmonary artery aneurysm in Behçet’s disease. Eur J Vasc Endovasc Surg 13(2):233–236
Uzun O, Erkan L, Akpolat I, Findik S, Atici AG, Akpolat T (2008) Pulmonary involvement in Behcet’s disease. Respiration 75(3):310–321
Raz I, Okon E, Chajek-Shaul T (1989) Pulmonary manifestations in Behcet’s syndrome. Chest 95(3):585–589
Andréjak C, Parrot A, Bazelly B, Ancel PY, Djibré M, Khalil A et al (2009) Surgical lung resection for severe hemoptysis. Ann Thorac Surg 88(5):1556–1565
Tuzun H, Hamuryudan V, Yildirim S, Beşirli K, Yörük Y, Yurdakul S et al (1996) Surgical therapy of pulmonary arterial aneurysms in Behcet’s syndrome. Ann Thorac Surg 61(2):733–735
International Team for the Revision of the International (2014) Criteria for Behçet’s Disease (ITR-ICBD). The International Criteria for Behçet’s Disease (ICBD): a collaborative study of 27 countries on the sensitivity and specificity of the new criteria. J Eur Acad Dermatol Venereol 28(3):338–347
Erkan D, Yazici Y, Sanders A, Trost D, Yazici H (2004) Is Hughes–Stovin syndrome Behcet’s disease? Clin Exp Rheumatol 22(4 Suppl 34):S64–S68
Khalid U, Saleem T (2011) Hughes–Stovin syndrome. Orphanet J Rare Dis 6:15
Kim JT, Oh TY, Chang WH (2007) Rare case of multiple pulmonary artery aneurysms with caval thrombosis–Hughes–Stovin syndrome. Eur J Cardiothorac Surg 31(3):561–562
Tzilalis VD, Vourliotakis G, Tsironis IA, Tsiligiris VD, Brountzos EN (2011) Use of an Amplatzer vascular plug in embolization of a pulmonary artery aneurysm in a case of Hughes–Stovin syndrome: a case report. J Med Case Rep 5:425
Cil BE, Geyik S, Akmangit I, Cekirge S, Besbas N, Balkanci F (2005) Embolization of a giant pulmonary artery aneurysm from Behcet disease with use of cyanoacrylate and the “bubble technique”. J Vasc Interv Radiol 16(11):1545–1549
Cil BE, Turkbey B, Canyigit M, Kumbasar OO, Celik G, Demirkasik FB (2006) Transformation of a ruptured giant pulmonary artery aneurysm into an air cavity after transcatheter embolization in a Behcet’s patient. Cardiovasc Interv Radiol 29(1):151–154
Cantasdemir M, Kantarci F, Mihmanli I, Akman C, Numan F, Islak C et al (2002) Emergency endovascular management of pulmonary artery aneurysms in Behcet’s disease: report of two cases and a review of the literature. Cardiovasc Interv Radiol 25(6):533–537
Lacombe P, Frija G, Parlier H, Lang F, Hamza M, Hamza R et al (1985) Transcatheter embolization of multiple pulmonary artery aneurysms in Behcet’s syndrome. Report of a case. Acta Radiol Diagn 26(3):251–253
Lacombe P, Qanadli SD, Jondeau G, Barré O, Mesurolle B, Mouas H et al (1997) Treatment of hemoptysis in Behcet syndrome with pulmonary and bronchial embolization. J Vasc Interv Radiol 8(6):1043–1047
Durieux P, Bletry O, Huchon G, Wechsler B, Chretien J, Godeau P (1981) Multiple pulmonary arterial aneurysms in Behcet’s disease and Hughes–Stovin syndrome. Am J Med 71(4):736–741
Bennji SM, du Preez L, Griffith-Richards S, Smit DP, Rigby J, Koegelenberg CFN, Irusen EM, Allwood BW (2017) Recurrent pulmonary aneurysms: Hughes–Stovin syndrome on the spectrum of Behçet disease. Chest 152(5):e99–e103
Kably IM, Reveron C (2015) Multimodal endovascular management of a Jehovah’s Witness patient with Hughes–Stovin syndrome presenting with ruptured pulmonary artery aneurysm and cardiopulmonary thromboembolism. Eur J Cardiothorac Surg 47(4):e158–e161
Khalil A, Parrot A, Fartoukh M, Marsault C, Carette MF (2006) Images in cardiovascular medicine. Large pulmonary artery aneurysm rupture in Hughes–Stovin syndrome: multidetector computed tomography pattern and endovascular treatment. Circulation 114(10):e380–e381
Emmi G, Silvestri E, Squatrito D, D’Elios MM, Ciucciarelli L, Prisco D, Emmi L (2014) Behçet’s syndrome pathophysiology and potential therapeutic targets. Intern Emerg Med 9(3):257–265
De Prost N, Parrot A, Picard C, Ancel PY, Mayaud C, Fartoukh M et al (2010) Diffuse alveolar haemorrhage: factors associated with in-hospital and long-term mortality. Eur Respir J 35(6):1303–1311
Khalil A, Parrot A, Nedelcu C, Fartoukh M, Marsault C, Carette MF (2008) Severe hemoptysis of pulmonary arterial origin: signs and role of multidetector row CT angiography. Chest 133(1):212–219
Erkan F, Gul A, Tasali E (2001) Pulmonary manifestations of Behcet’s disease. Thorax 56(7):572–578
Hatemi G, Silman A, Bang D, Bodaghi B, Chamberlain AM, Gul A et al (2008) EULAR recommendations for the management of Behcet disease. Ann Rheum Dis 67(12):1656–1662
Tunaci M, Ozkorkmaz B, Tunaci A, Gül A, Engin G, Acunas B (1999) CT findings of pulmonary artery aneurysms during treatment for Behcet’s disease. AJR Am J Roentgenol 172(3):729–733
de Montpreville VT, Macchiarini P, Dartevelle PG, Dulmet EM (1996) Large bilateral pulmonary artery aneurysms in Behcet’s disease: rupture of the contralateral lesion after aneurysmorrhaphy. Respiration 63(1):49–51
Tuzun H, Besirli K, Sayin A, Vural FS, Hamuryudan V, Hizli N et al (1997) Management of aneurysms in Behcet’s syndrome: an analysis of 24 patients. Surgery 121(2):150–156
Hirohata S, Kikuchi H (2009) Histopathology of the ruptured pulmonary artery aneurysm in a patient with Behcet’s disease. Clin Exp Rheumatol 27(2 Suppl 53):S91–S95
Emad Y, Ragab Y, Shawki A-H, Gheita T, El-Marakbi A, Salama MH (2007) Hughes–Stovin syndrome: is it incomplete Behçet’s? Report of two cases and review of the literature. Clin Rheumatol 26(11):1993–1996
Slavin RE, de Groot WJ (1981) Pathology of the lung in Behçet’s disease. Case report and review of the literature. Am J Surg Pathol 5(8):779–788
Funding
None.
Author information
Authors and Affiliations
Contributions
GV had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis, including and especially any adverse effects. GV participated in the conception and the design of the study, participated in the data acquisition, analysis and interpretation, and the statistical analysis, and drafted the manuscript. AP participated in the conception and the design of the study, participated in the data acquisition, analysis and interpretation, and helped to revise the manuscript critically for intellectual content. MA participated in the conception and the design of the study, performed the histological analysis, participated in the data acquisition and analysis, and helped to revise the manuscript critically for intellectual content. AG participated in the data acquisition, analysis and interpretation, and helped to revise the manuscript critically for intellectual content. SH participated in the data acquisition, analysis and interpretation, and helped to revise the manuscript critically for intellectual content. MFC participated in the conception and the design of the study, performed the interventional radiology procedures and helped to revise the manuscript critically for intellectual content. MF participated in the conception and design of the study, the data analysis and interpretation, and the statistical analysis, and revised the manuscript critically for intellectual content. AK designed the study, performed the interventional radiology procedures, participated in the data analysis and interpretation, and revised the manuscript critically for intellectual content. All authors read and approved the final version to be submitted.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Availability of supporting data
Data and materials supporting the findings of this study can be entirely shared on asking.
Ethical approval
This study was conducted in accordance with the French law, which does not require approval of an institutional review board.
Informed consent
None.
Statement of human and animal rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Figure 1.
Pathological findings: pulmonary artery thrombosis. A 27-year-old patient was admitted to our department for massive hemoptysis (see legend of Figure 3). Seven years earlier, he was diagnosed a Behçet’s disease. A pulmonary artery angiography revealed a pulmonary artery aneurysm, which was occluded with coils. Nineteen months later, hemoptysis recurred and was related to a systemic hypervascularization. Two procedures of bronchial artery embolization did not allow to control the bleeding, leading to perform a right lower lobectomy. The removed lobe underwent staining with hematein-safran-eosin, and examination under a light microscope. The pulmonary artery (Pa) was thrombosed and repermeabilized. The material of embolization (arrow) was observed close to the pulmonary artery parietal wall, which displayed a marked fibrosis. Magnification X2.5. (TIFF 612 kb)
Supplementary Figure 2.
Pathological findings: systemic hypervascularization and inflammatory process. A 42-year-old patient with a history of recurrent pulmonary embolism was admitted to our department for massive hemoptysis. Hughes–Stovin syndrome (HSS) was diagnosed on the basis of the association of multiple pulmonary arteries aneurysms, pulmonary embolism, and thrombus into the right atrium. Only one pulmonary artery aneurysm (located in the right middle lobe) displayed signs of recent bleeding (air bubble and ground-glass opacities around the pulmonary artery aneurysm). The sac of this pulmonary artery aneurysm was occluded using a total of 2.07 meters of coils. The bleeding stopped. Immunosuppressive therapy was started. One month later, hemoptysis recurred and was related to a systemic hypervascularization. A bronchial artery embolization allowed to control the bleeding transiently, but the bleeding recurred 4 months later. Two additional procedures of systemic artery embolization failed to control the bleeding, leading to perform a right middle lobectomy. The removed lobe underwent staining with hematein-safran-eosin, and examination under a light microscope. (A, B) The pulmonary artery (Pa) was thrombosed; materials of bronchosystemic artery embolization (arrows) were observed in lumens of both the pulmonary artery and the adjacent systemic arteries (Sv). (C, D) A marked systemic hypervascularization (Sv) was observed around the thrombosed pulmonary artery (Pa) and its satellite bronchus (Br). (E, F) Macrophage (Mp) infiltrates were observed within the pulmonary artery thrombus; lymphocytes (Ly) and macrophage infiltrates were observed within the pulmonary artery parietal wall. Magnification X2.5 (A, C, E) and X10 (B, D, F). (TIFF 5090 kb)
Rights and permissions
About this article
Cite this article
Voiriot, G., Parrot, A., Antoine, M. et al. Transcatheter embolotherapy of pulmonary artery aneurysms as emergency treatment of hemoptysis in Behcet patients: experience of a referral center and a review of the literature. Intern Emerg Med 13, 491–500 (2018). https://doi.org/10.1007/s11739-018-1817-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-018-1817-y