Abstract
The purpose of this review is to evaluate whether some risk factors in childhood work as significant predictors of the development of obesity and the metabolic syndrome in adulthood. These factors include exposures to risk factors in the prenatal period, infancy and early childhood, as well as other socio-demographic variables. We searched articles of interest in PubMed using the following terms: ‘predictors AND obesity OR Metabolic syndrome AND (children OR adolescents) AND (dyslipidemia OR type 2 diabetes OR atherosclerosis OR hypertension OR hypercholesterolemia OR cardiovascular disease)’ AND genetic OR epigenetic. Maternal age, smoking and weight gain during pregnancy, parental body mass index, birth weight, childhood growth patterns (early rapid growth and early adiposity rebound), childhood obesity and the parents’ employment have a role in early life. Furthermore, urbanization, unhealthy diets, increasingly sedentary lifestyles and genetic/epigenetic variants play a role in the persistence of obesity in adulthood. Health promotion programs/agencies should consider these factors as reasonable targets to reduce the risk of adult obesity. Moreover, it should be a clinical priority to correctly identify obese children who are already affected by metabolic comorbidities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity in children and adults has become one of the most important public health problems worldwide [1]. As reported by the World Health Organization (WHO), the number of overweight infants and children in Europe rose steadily from 1990 to 2008 [2], and the proportion of overweight and obesity in childhood increased by 47.1 % between 1980 and 2013 worldwide [3]. Over 60 % of children who are overweight before puberty may be overweight in early adulthood. According to the current estimates, more than 700 million individuals worldwide will be obese by 2015. Childhood obesity is strongly associated with risk factors for cardiovascular disease, type 2 diabetes (T2DM), orthopedic problems, mental disorders, underachievement in school and lower self-esteem. The obesity-associated comorbidities increase as the prevalence of obesity increases, and it has become critical that overweight and obese children be appropriately identified and enrolled in appropriate counseling and treatment programs [4]. Recommendations, guidelines and consensus statements have been issued in this respect, and all are focused on the importance of behavioral, pharmacological, and surgical treatments in the population at high risk [5–11] (Table 1). Obese children are highly prone to becoming obese in adulthood, and this long time-span puts subjects at high risk for developing severe comorbidities such as the metabolic syndrome (MS), T2DM, cardiovascular disease [12–14], dysfunctional gastrointestinal motility and cholesterol gallstone disease [15, 16]. The burden of adult obesity can also be reflected in social, economic, educational and psychological factors [17]. Proneness to obesity depends on a complex interplay among genetic, epigenetic and environmental factors. Environmental changes have occurred over the last 30 years, which include the wide availability of energy dense foods and frequently a sedentary lifestyle. Despite such changes being associated with an increase in obesity prevalence, many individual variations in body weight exist among populations sharing a similar environment. Other factors such as short sleep duration [18], low dietary calcium intake [19], inadequate eating behaviors [20], also have a significant impact on body weight.
One important but still unanswered question is: are obesity and MS in adulthood the result of alterations existing in childhood, or whether obesity and MS in adulthood are separate entities determined by the onset of further alterations that are absent in childhood? In this review, we examine the most significant prenatal, infant, childhood predictors of the development of obesity and MS in adulthood.
Literature search
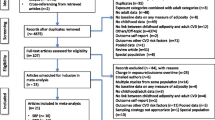
We searched articles of interest in PubMed using the following terms: ‘predictors AND obesity OR Metabolic syndrome AND (children OR adolescents) AND (dyslipidemia OR type 2 diabetes OR atherosclerosis OR hypertension OR hypercholesterolemia OR cardiovascular disease)’ AND genetic OR epigenetic. A total of 113 full-text articles published from 2000 to 2015 in English language were examined, based on their topic, scientific quality and currency.
Obesity and overweight in childhood and adulthood: criteria for definition according to age, gender, and ethnic differences
Obesity is defined as an accumulation of excess body fat that adversely affects health. Obesity results from a long-term positive energy balance, and is routinely measured as body mass index (BMI) that is equal to body weight (in kg) divided by height (in meters) squared. BMI is the standard measure of overweight and obesity in adults [21]. The WHO classifies a person with a BMI ≥25 kg/m2 as overweight, a BMI ≥30 kg/m2 as obese and a BMI ≥40 kg/m2 as extremely obese. Overestimation or underestimation of obesity can occur with BMI when muscle mass is increased in athletes or decreased in people prone to a sedentary life. BMI correlates with adiposity [21] and complications of childhood overweight and obesity [22]. In children and adolescents, BMI has to be referred to percentile tables, and obesity and overweight are defined according to the Centers for Disease Control (CDC) and Prevention Growth Charts [23]. For children, the use of BMI is still the common basis for defining weight status, and standard deviation scores for BMI (BMI-SDS), also referred to as z scores, have become widely accepted. BMI-SDS is very useful, particularly at the epidemiologic level, for describing how a child’s weight can be seen in the context of the general pediatric population. z-Scores correspond directly to percentiles. The z score for BMI is expressed as the number of standard deviations by which a child differs from the mean in a specific country or ethnic group for his or her age and gender [24]. However, BMI is not sensitive enough to assess increased fat mass in a pediatric population with moderate overweightness [24]. Cole et al. suggest measuring changes in weight using BMI percentages [25]. Another parameter that is increasingly used in the pediatric population is the waist-to-height-ratio (WHtR), and a value of ≥0.5 is associated with increased cardiometabolic risk [26]. This measure has comparable predictive value to BMI for obesity-associated morbidity [26]. More specifically, it is a fairly sensitive and specific marker of visceral obesity during childhood and adolescence.
Gender and age are associated with differences in body fat distribution and body composition. For example, women tend to store more fat in the gluteo-femoral subcutaneous adipose tissue depots rather than in the visceral adipose depots. Nonetheless, at the same BMI, women tend to carry more body fat than men [1]. Two general patterns of fat distribution have been observed: abdominal type or central obesity (adipose accumulation in the abdominal visceral area) and gluteo-femoral or gynoid type (adipose deposition around the hips). Abdominal fat mass is strongly correlated with waist circumference, which is the strongest predictor of most cardiovascular variables in men, whereas the ratio of abdominal to gluteo-femoral fat mass (waist-to-hip ratio) is the strongest predictor in women [27]. Gluteo-femoral fat mass is positively associated with impaired glucose tolerance, hypertriglyceridemia, and hypertension in men, whereas the ratio of hip circumference to total fat mass shows a negative association with hypertriglyceridemia and hypertension. Increased body adiposity contributes to the development of a low-grade chronic proinflammatory state in childhood and adults, thereby contributing to the obesity-associated cardiovascular disease [28]. In this respect, interventions targeted at insulin resistance are required to prevent cardiometabolic risk in adolescence [28].
Throughout the developed world, childhood overweightness is increased in ethnic minority groups. In the USA, the prevalence of childhood overweightness is higher among Blacks and Hispanics than among Caucasians [29]; and in the UK, overweightness prevalence is higher among South-Asian and African-Caribbean children, although contradictions arise when different definitions of overweightness are used [30]. Studies from Australia, Germany and the Netherlands also report that certain ethnic groups have a higher prevalence of childhood overweightness [31, 32]. Ethnic differences in overweight people have been reported to be present from preschool age onwards [31, 32]. This suggests that factors responsible for ethnic differences in overweightness have a role in early life. Ethnic differences in overweight preschool children seem to have their origins in factors that operate before (maternal educational level), during (parental BMI), and after (infant weight change) pregnancy [33]. After birth, BMI development is fairly similar between ethnic groups. Maternal educational level, parental BMI, and infant weight change may partly explain the ethnic differences in childhood overweightness. Therefore, in order to reduce ethnic inequalities in childhood overweightness, prevention programs should start in the earliest stage of pregnancy.
Prenatal, infant, childhood predictors of adult obesity
Prenatal risk factors are associated with increased risk for obesity later in life (Fig. 1). A relationship has been shown between maternal BMI, maternal smoking and maternal weight gain during pregnancy and adult obesity [34, 35]. Maternal obesity affects peri-conception events such as oocyte and embryo quality [36]. Intrauterine growth restriction with early catch-up growth during infancy is related to the development of central adiposity and the risk of cardiovascular disease [37]. Moreover, early adiposity rebound is a risk factor for greater fatness in adolescence and adulthood [38], because it identifies children with a BMI high or crossing upwards. Socioeconomic conditions in childhood influence the development of obesity in adulthood [39]. Furthermore, there is evidence of a link between childhood intelligence and adult obesity [40]. A recent study shows that a set of poor neurological functions (poor hand control, poor coordination, clumsiness) in 7-year-old children are significantly associated with obesity in adulthood [41]. Education, trait consicousness, and the amount of exercise in childhood have been significantly and independently associated with adult obesity [42].
Prenatal, infant, and childhood predictors of adult obesity. Following the gestational exposure with associated conditions influencing the epigenetic regulation, events depending on birth weight may affect early catch up growth and early adiposity rebound. During early childhood and subsequent adulthood, additional factors include socioeconomic conditions, neurological functions and physical exercise. BMI body mass index, IUGR intrauterine growth restriction
Genetic and epigenetic determinants
During intrauterine life, several factors such as maternal and paternal genes, maternal BMI, maternal smoking, maternal alcohol consumption, maternal drug use, exercise during pregnancy, and birth weight, vary depending on the epigenetics of an individual, and can predispose to obesity and other phenotypes during later stage of life [43]. In addition, after birth, gene–environment interactions may lead to modifications in DNA methylation patterns.
It has been observed that during the early years of life, monozygotic twins are epigenetically indistinguishable from each other, but, with increasing age, remarkable differences in their overall content and genomic distributions of 5-methylcytosine DNA and histone acetylations become evident [43]. It has also been observed that microRNAs (miRNAs) expand their roles in epigenetic regulation [44]. Thus, dietary intake of methyl groups (choline, methionine, genistein and folate) during critical periods of developmental stages alters promoter DNA and histone methylation, thereby resulting in lifelong changes in gene expression, and alteration of the epigenome towards obesity in adulthood [45].
Does the obese child become an obese adult with health consequences?
In addition to hereditary tendencies and environmental factors, abnormal lifestyles may cause obesity in childhood and adolescence, leading to a high obesity prevalence in adulthood.
High television screen time exposure, short sleep duration, a sedentary lifestyle, and increased intake of trans fatty acids, high sugars and salt, are associated with childhood obesity [46].
Since 1973, major changes have been occurred in the composition of macronutrients in the childhood diet. Energy has originated more from protein and carbohydrate than from fat, whereas the percentage of energy from polyunsaturated fatty acid has increased. Children became more prone to consume lower amounts of fat/oil, vegetables/soups, breads/grains, mixed meats, desserts, candy, and eggs. By contrast, increasing amounts of fruits/fruit juices, beverages, poultry, snacks, condiments, and cheese have been consumed. Moreover, a marked increase in the consumption of soft drinks and foods containing high fructose corn syrups has been observed [47]. By contrast, fruit and vegetable consumption is lower in obese children than in non-obese subjects, suggesting a low incindence of compliance of obese children with the recommendations of the food guide pyramid as adopted by the US Department of Food and Agriculture and the Department of Health and Human Services [48].
The condition of high BMI in childhood predisposes to obesity in adulthood and increased risks for obesity-related morbidities and mortality in adulthood, and this risk rises with age. In a systematic review including 34 studies, the effects of childhood obesity on the cardiovascular system is confirmed by the strong association between obesity (BMI >85th or 95th centiles) and several cardiovascular risk factors (i.e., dyslipidemia, high blood pressure, abnormalities in left ventricular mass or function, abnormalities in endothelial function, hyperinsulinemia, or insulin resistance) [49]. The analysis of data from four longitudinal cohort studies (including Bogalusa, Muscatine, CDAH, and YFS studies) shows that subjects who are overweight or obese in childhood have an increased risk of developing dyslipidemia, T2DM, hypertension, and high-risk carotid intima-media thickness in adulthood. Moreover, children with a normal BMI who become obese in adulthood display adverse risk-factor profiles. By contrast, the cardiovascular-risk profile of overweight or obese children who become non-obese in adulthood is similar to the risk of subjects who are never obese [50].
In the Kaunas cardiovascular risk cohort study with over 35 years of follow-up, an increased childhood BMI and skinfold thicknesses is associated with an increased risk of developing adult obesity, hyperglycemia or T2DM, MS, and an elevated level of high-sensitivity C reactive protein. By contrast, childhood obesity does not influence arterial hypertension and serum levels of triglycerides and HDL cholesterol. Furthermore, an increased odds of the overall mentioned risk factors is observed when BMI is increased from childhood to adulthood [51].
It is difficult to address all the progressive mechanisms that lead to the long-term adverse effects of childhood or adolescent obesity on cerebrovascular and cardiovascular diseases and accidents in adulthood. We speculate that early obesity occurring in childhood will expose subjects to the long-term effects of metabolic disturbances with further consequences during adulthood.
In fact, high blood pressure and high blood cholesterol lead to atherosclerotic lesions, which antedate severe clinical manifestations by years and even decades. Also, insulin resistance has been identified as a major precursor of T2DM and cardiovascular disease in adulthood. Moreover, a greater degree of adiposity is reported to be strongly associated with concentric left ventricular remodeling in midlife, while the cumulative effects of a longer duration of overall obesity during young adulthood contribute to concentric remodeling predominantly by increasing left ventricular mass [52]. In addition, longer duration of overall and abdominal obesity is associated with subclinical coronary heart disease and its progression through midlife independent of the degree of adiposity.
The metabolic syndrome: which differences between children and adults?
The MS, once regarded as an “adult problem”, has become increasingly common in children because of the ever growing prevalence of childhood obesity. The MS in adults is defined as a cluster of cardiovascular and diabetes risk factors including abdominal obesity, dyslipidemia, glucose intolerance, and hypertension [53]. Recently, the International Diabetes Federation (IDF) guidelines have rationalized the existing multiple definitions of the MS in adults [53]. However, to date, there has not been a unified definition that can be used to assess risk in children and adolescents, and existing adult-based definitions of the MS may not be appropriate to address the problem in this age group. The risk factors associated with clustering of components of the MS have been demonstrated in adults, where the presence of three or more components significantly increases the risk for coronary heart disease, and non-fatal myocardial infarction and the onset of diabetes [54]; however, few, if any, outcome data in children are available. Blood pressure, serum lipid levels, and anthropometric variables change with age and pubertal development. Puberty influences fat distribution, and causes a decrease in insulin sensitivity by ~30 % with a complementary increase in insulin secretion, and in adiponectin levels. Therefore, single cut off points cannot be used to define abnormalities in children.
Risk factors for the metabolic syndrome
Although it is well recognized that early-onset obesity is associated with an increased risk for developing metabolic and cardiovascular disease [55], there is still debate about the utility of MS as a cardiovascular predictor in children and adolescents. Population-based studies highlight that the presence of MS during adolescence is not predictive of adult MS and T2DM or increased carotid intima-media thickness (cIMT) [56]. Obese children and adolescents who recover from their obesity seem to have the same risk of presenting adult T2DM, hypertension, dyslipidemia or increased cIMT as children and adolescents who are never obese [57]. On the other hand, childhood MS, unless it resolves, represents a real cardiovascular risk factor [58]. While cardiovascular risk associated with childhood BMI and MS has been shown to be reversible in the case of obesity and MS recovery, childhood low-density lipoprotein (LDL) cholesterol, blood pressure and, in particular, a triglyceride/high-density lipoprotein (HDL) ratio <3 are associated with adult cardiovascular risk, irrespective of their tracking into adulthood [59]. On the other hand, a precise risk score to identify obese children who are likely to develop T2DM is still lacking. An impaired glucose tolerance (IGT), a traditional pre-diabetic condition, is not a fully precise predictor of future T2DM. Notably, IGT during childhood and adolescence is a cardiovascular risk factor per se, independent of the development of diabetes, as it is associated with an increased rate of cardiovascular events in adults and increased cIMT in youth [60].
Among risk factors predisposing to the development of MS in childhood, genetic factors, low birth weight, and early adiposity rebound may all contribute to a child’s future risk. Several other risk factors have been emerging as potential predictors of MS at a general population level. Among lifestyle risk factors, infrequent fruit consumption and low physical activity in childhood are associated with accelerated 6-year IMT progression in adulthood. However, data on the predictive value of lifestyle variables in obese youth are not available. The predictive utility of circulating biomarkers such as C-reactive protein, adiponectin, leptin, homocysteine and asymmetric dimethylarginine has been explored [58], even if only high adiponectin has been shown to protect against adult MS. Among comorbidities of childhood and adolescent obesity, polycystic ovary syndrome, low sex hormone binding globulin and nonalcoholic fatty liver disease (NAFLD) are known to be strong risk factors for severe obesity and MS during early adulthood [61].
Conclusions and perspectives
Obesity is a common problem in children and adolescents worldwide, which influences public health. Obesity causes adverse effects on health in childhood, which perpetuate and amplify the metabolic disturbances in adulthood, thereby leading to a high risk of mortality.
Although still preliminary, there is important evidence from human and animal studies demonstrating that already in early life, epigenetic states may contribute, in part, to the occurrence of obesity and the metabolic syndrome in adults.
The importance of the early identification of children at risk of developing the MS, and subsequently progressing to T2DM and cardiovascular disease in later life must not be underestimated. Current initiatives include school-based programs addressing physical activity and diet, which have been conducted with mixed success in reducing adiposity. However appropriate algorithms specific for childhood obesity are needed to allow more realistic predictions of intervention effects. Only recently such an algorithm has been proposed in adults to estimate the weight outcomes of clinical health interventions accounting for compensatory changes in energy intake or expenditure.
There are limited safety data supporting the use of drugs for the treatment of obesity and related conditions, and noncompliance in this population suggests that pharmacotherapy is unlikely to be effective long term.
References
Ogden CL, Yanovski SZ, Carroll MD, Flegal KM (2007) The epidemiology of obesity. Gastroenterology 132:2087–2102
Obesity. In: World Health Organization (WHO) Regional Office for Europe, 2015
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C et al (2014) Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the global burden of disease study 2013. Lancet 384:766–781
Fruhbeck G (2000) Childhood obesity: time for action, not complacency. Definitions are unclear, but effective interventions exist. BMJ 320:328–329
Baker S, Barlow S, Cochran W, Fuchs G, Klish W, Krebs N et al (2005) Overweight children and adolescents: a clinical report of the North American society for pediatric gastroenterology, hepatology and nutrition. J Pediatr Gastroenterol Nutr 40:533–543
Daniels SR, Arnett DK, Eckel RH, Gidding SS, Hayman LL, Kumanyika S et al (2005) Overweight in children and adolescents: pathophysiology, consequences, prevention, and treatment. Circulation 111:1999–2012
Speiser PW, Rudolf MC, Anhalt H, Camacho-Hubner C, Chiarelli F, Eliakim A et al (2005) Childhood obesity. J Clin Endocrinol Metab 90:1871–1887
Barlow SE, Expert C (2007) Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics 120:S164–S192
Krebs NF, Himes JH, Jacobson D, Nicklas TA, Guilday P, Styne D (2007) Assessment of child and adolescent overweight and obesity. Pediatrics 120:S193–S228
Force USPST, Barton M (2010) Screening for obesity in children and adolescents: US preventive services task force recommendation statement. Pediatrics 125:361–367
Young KL, Demeule M, Stuhlsatz K, Janzen D, Porter RM, Pomettio M et al (2011) Identification and treatment of obesity as a standard of care for all patients in children’s hospitals. Pediatrics 128:S47–S50
Park MH, Falconer C, Viner RM, Kinra S (2012) The impact of childhood obesity on morbidity and mortality in adulthood: a systematic review. Obes Rev 13:985–1000
Faienza MF, Acquafredda A, Tesse R, Luce V, Ventura A, Maggialetti N et al (2013) Risk factors for subclinical atherosclerosis in diabetic and obese children. Int J Med Sci 10:338–343
Nacci C, Leo V, De Benedictis L, Carratu MR, Bartolomeo N, Altomare M et al (2013) Elevated endothelin-1 (ET-1) levels may contribute to hypoadiponectinemia in childhood obesity. J Clin Endocrinol Metab 98:E683–E693
Portincasa P, Moschetta A, Palasciano G (2006) Cholesterol gallstone disease. Lancet 368:230–239
Di Ciaula A, Wang DQ, Portincasa P (2012) Gallbladder and gastric motility in obese newborns, pre-adolescents and adults. J Gastroenterol Hepatol 27:1298–1305
Viner RM, Cole TJ (2005) Adult socioeconomic, educational, social, and psychological outcomes of childhood obesity: a national birth cohort study. BMJ 330:1354
Chaput JP, Despres JP, Bouchard C, Tremblay A (2012) Longer sleep duration associates with lower adiposity gain in adult short sleepers. Int J Obes 36:752–756
Zemel MB, Thompson W, Milstead A, Morris K, Campbell P (2004) Calcium and dairy acceleration of weight and fat loss during energy restriction in obese adults. Obes Res 12:582–590
Chaput JP, Leblanc C, Perusse L, Despres JP, Bouchard C, Tremblay A (2009) Risk factors for adult overweight and obesity in the Quebec family study: have we been barking up the wrong tree? Obesity 17:1964–1970
Deurenberg P, Weststrate JA, Seidell JC (1991) Body mass index as a measure of body fatness: age- and sex-specific prediction formulas. Br J Nutr 65:105–114
Freedman DS, Dietz WH, Srinivasan SR, Berenson GS (1999) The relation of overweight to cardiovascular risk factors among children and adolescents: the Bogalusa heart study. Pediatrics 103:1175–1182
Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z et al (2002) 2000 CDC growth charts for the United States: methods and development. Vital Health Stat 11(246):1–190
Javed A, Jumean M, Murad MH, Okorodudu D, Kumar S, Somers VK et al (2015) Diagnostic performance of body mass index to identify obesity as defined by body adiposity in children and adolescents: a systematic review and meta-analysis. Pediatr Obes 10:234–244
Cole TJ, Faith MS, Pietrobelli A, Heo M (2005) What is the best measure of adiposity change in growing children: BMI, BMI %, BMI z-score or BMI centile? Eur J Clin Nutr 59:419–425
Savva SC, Lamnisos D, Kafatos AG (2013) Predicting cardiometabolic risk: waist-to-height ratio or BMI. A meta-analysis. Diabetes Metab Syndr Obes 6:403–419
Wiklund P, Toss F, Weinehall L, Hallmans G, Franks PW, Nordstrom A et al (2008) Abdominal and gynoid fat mass are associated with cardiovascular risk factors in men and women. J Clin Endocrinol Metab 93:4360–4366
Sakou II, Psaltopoulou T, Sergentanis TN, Karavanaki K, Karachaliou F, Ntanasis-Stathopoulos I et al (2015) Insulin resistance and cardiometabolic risk factors in obese children and adolescents: a hierarchical approach. J Pediatr Endocrinol Metab 28:589–596
Anderson SE, Whitaker RC (2009) Prevalence of obesity among US preschool children in different racial and ethnic groups. Arch Pediatr Adolesc Med 163:344–348
Shaw NJ, Crabtree NJ, Kibirige MS, Fordham JN (2007) Ethnic and gender differences in body fat in British schoolchildren as measured by DXA. Arch Dis Child 92:872–875
de Wilde JA, van Dommelen P, Middelkoop BJ, Verkerk PH (2009) Trends in overweight and obesity prevalence in Dutch, Turkish, Moroccan and Surinamese South Asian children in the Netherlands. Arch Dis Child 94:795–800
Lynch J, Wang XL, Wilcken DE (2002) Body mass index in Australian children: recent changes and relevance of ethnicity. Arch Dis Child 82:16–20
van Rossem L, Hafkamp-de Groen E, Jaddoe VWV, Hofman A, Mackenbach JP, Raat H (2014) The role of early life factors in the development of ethnic differences in growth and overweight in preschool children: a prospective birth cohort. BMC Public Health 14:722
Williams S (2001) Overweight at age 21: the association with body mass index in childhood and adolescence and parents’ body mass index. A cohort study of New Zealanders born in 1972–1973. Int J Obes Relat Metab Disord 25:158–163
Gaillard R, Steegers EA, Franco OH, Hofman A, Jaddoe VW (2015) Maternal weight gain in different periods of pregnancy and childhood cardio-metabolic outcomes. The generation R study. Int J Obes 39:677–685
Depalo R, Garruti G, Totaro I, Panzarino M, Vacca MP, Giorgino F et al (2007) Oocyte morphological abnormalities in overweight women undergoing in vitro fertilization cycles. Gynecol Endocrinol 27:880–884
Singhal A, Lucas A (2004) Early origins of cardiovascular disease: is there a unifying hypothesis? Lancet 363:1642–1645
Papadimitriou A (2015) Timing of adiposity rebound and prevalence of obesity. J Pediatr 167:498
Power C, Manor O, Matthews S (2003) Child to adult socioeconomic conditions and obesity in a national cohort. Int J Obes Relat Metab Disord 27:1081–1086
Chandola T, Deary IJ, Blane D, Batty GD (2006) Childhood IQ in relation to obesity and weight gain in adult life: the national child development (1958) study. Int J Obes 30:1422–1432
Osika W, Montgomery SM, Longitudinal Birth Cohort S (2008) Physical control and coordination in childhood and adult obesity: longitudinal birth cohort study. BMJ 337:a699
Cheng H, Furnham A (2013) Personality traits, education, physical exercise, and childhood neurological function as independent predictors of adult obesity. PLoS One 8:e79586
Stoger R (2008) Epigenetics and obesity. Pharmacogenomics 9:1851–1860
Lodygin D, Tarasov V, Epanchintsev A, Berking C, Knyazeva T, Korner H et al (2008) Inactivation of miR-34a by aberrant CpG methylation in multiple types of cancer. Cell Cycle 7:2591–2600
Zeisel SH (2009) Epigenetic mechanisms for nutrition determinants of later health outcomes. Am J Clin Nutr 89:1488S–1493S
Bornhorst C, Wijnhoven TM, Kunesova M, Yngve A, Rito AI, Lissner L et al (2015) WHO European childhood obesity surveillance initiative: associations between sleep duration, screen time and food consumption frequencies. BMC Public Health 15:442
Ludwig DS, Peterson KE, Gortmaker SL (2001) Relation between consumption of sugar-sweetened drinks and childhood obesity: a prospective, observational analysis. Lancet 357:505–508
Garipagaoglu M, Sahip Y, Budak N, Akdikmen O, Altan T, Baban M (2008) Food types in the diet and the nutrient intake of obese and non-obese children. J Clin Res Pediatr Endocrinol 1:21–29
Reilly JJ (2003) Health consequences of obesity. Arch Dis Child 88:748–752
Juonala M, Magnussen CG, Berenson GS, Venn A, Burns TL, Sabin MA et al (2011) Childhood adiposity, adult adiposity, and cardiovascular risk factors. N Engl J Med 365:1876–1885
Petkeviciene J, Klumbiene J, Kriaucioniene V, Raskiliene A, Sakyte E, Ceponiene I (2015) Anthropometric measurements in childhood and prediction of cardiovascular risk factors in adulthood: Kaunas cardiovascular risk cohort study. BMC Public Health 15:218
Reis JP, Allen N, Gibbs BB, Gidding SS, Lee JM, Lewis CE et al (2014) Association of the degree of adiposity and duration of obesity with measures of cardiac structure and function: the CARDIA study. Obesity 22:2434–2440
Alberti KG, Zimmet P, Shaw J (2006) Metabolic syndrome—a new world-wide definition. A consensus statement from the international diabetes federation. Diabet Med 23:469–480
Sattar N, Gaw A, Scherbakova O, Ford I, O’Reilly DS, Haffner SM et al (2003) Metabolic syndrome with and without C-reactive protein as a predictor of coronary heart disease and diabetes in the West of Scotland coronary prevention study. Circulation 108:414–419
Franks PW, Hanson RL, Knowler WC, Sievers ML, Bennett PH, Looker HC (2010) Childhood obesity, other cardiovascular risk factors, and premature death. N Engl J Med 362:485–493
Magnussen CG, Koskinen J, Chen W, Thomson R, Schmidt MD, Srinivasan SR et al (2010) Pediatric metabolic syndrome predicts adulthood metabolic syndrome, subclinical atherosclerosis, and type 2 diabetes mellitus but is no better than body mass index alone: the Bogalusa heart study and the cardiovascular risk in young Finns study. Circulation 122:1604–1611
Magnussen CG, Koskinen J, Juonala M, Chen W, Srinivasan SR, Sabin MA et al (2012) A diagnosis of the metabolic syndrome in youth that resolves by adult life is associated with a normalization of high carotid intima-media thickness and type 2 diabetes mellitus risk: the Bogalusa heart and cardiovascular risk in young Finns studies. J Am Coll Cardiol 60:1631–1639
Morrison JA, Glueck CJ, Woo JG, Wang P (2012) Risk factors for cardiovascular disease and type 2 diabetes retained from childhood to adulthood predict adult outcomes: the Princeton LRC follow-up study. Int J Pediatr Endocrinol 2012:6
Urbina EM, Khoury PR, McCoy CE, Dolan LM, Daniels SR, Kimball TR (2013) Triglyceride to HDL-C ratio and increased arterial stiffness in children, adolescents, and young adults. Pediatrics 131:e1082–e1090
Reinehr T, Wunsch R, Putter C, Scherag A (2013) Relationship between carotid intima-media thickness and metabolic syndrome in adolescents. J Pediatr 163:327–332
Morandi A, Maffeis C (2014) Predictors of metabolic risk in childhood obesity. Horm Res Paediatr 82:3–11
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of human and animal rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Not required.
Rights and permissions
About this article
Cite this article
Faienza, M.F., Wang, D.Q.H., Frühbeck, G. et al. The dangerous link between childhood and adulthood predictors of obesity and metabolic syndrome. Intern Emerg Med 11, 175–182 (2016). https://doi.org/10.1007/s11739-015-1382-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-015-1382-6