Abstract
Laparoscopic elective splenectomy is considered as a safe surgical treatment of spleen non-traumatic blood disorders. However, robotic assisted splenectomy is becoming a promising alternative, although there are scarce studies in pediatric patients. Our aim is to compare the effectiveness and associated costs of both procedures in children. A single-institution retrospective study was performed among consecutive children undergoing splenectomy between 2004 and 2021, who were divided according to the surgical approach: LAS group (laparoscopic splenectomy) and RAS group (robotic assisted splenectomy). Demographics, clinical features, intraoperative blood loss, surgery time, length of hospital stay (LOS), postoperative complications, need for postoperative blood transfusion, readmission rate and economic data were compared. A total of 84 patients were included (23 LAS group; 61 RAS group), without demographic or clinical differences between them. RAS patients presented lower intraoperative blood loss (42 ± 15 vs. 158 ± 39 ml; p < 0.021) and shorter surgery time (135 ± 39 vs. 182 ± 68 min; p = 0.043), with no differences in median LOS (3 days in both groups). No intraoperative complications or conversion was reported. Five postoperative complications were observed: 4 in LAS patients (17.4%) versus only one in RAS (1.6%; p = 0.021). One reintervention was required in LAS group due to hemoperitoneum 12 h after splenectomy. RAS patients had lower postoperative blood transfusion requirements (1.6% vs. 13.0%; p = 0.025) and lower readmission rate (3.3 vs. 17.4%; p = 0.042). No differences were observed when comparing the median economic costs ($25,645 LAS vs. $28,135 RAS; p = 0.215). Robotic assisted splenectomy may be considered as a safe and feasible option in children compared to the traditional laparoscopic approach. Level of evidence: III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Splenectomy is considered as the primary treatment approach for the consequences of various pediatric hereditary hematologic conditions, which encompass immune sickle cell disease (SCD), idiopathic thrombocytopenic purpura (ITP), and hereditary spherocytosis (HS) [1]. Since its initial description over 30 years ago, laparoscopic elective splenectomy has become the gold standard surgical treatment of both benign and malignant hematological conditions [2]. Nevertheless, in the last decade, robotic assisted splenectomy is becoming a promising alternative treatment for these cases [3]. Several meta-analyses in adult patients have demonstrated a reduction in the volume of intraoperative blood loss and postoperative complications of robotic splenectomy compared to laparoscopic procedures [4, 5]. However, adoption of robotic techniques within pediatric patients has been somewhat restricted, primarily due to constraints related to instrument size, reduced surgical domain, and a general shortage of technical expertise [6]. There are scarce studies in children comparing robotic and laparoscopic splenectomy, with low numbers of patients and controversial conclusions regarding outcomes and associated costs [7, 8]. The aim of this study is to compare the effectiveness, safety and associated costs of both procedures.
Methods
Study design
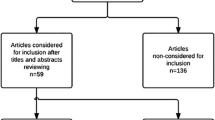
We conducted a single-institution retrospective cohort study among consecutive children undergoing splenectomy between from January 2004 to December 2021. These patients were divided in two groups according to the surgical approach: LAS group (laparoscopic splenectomy) and RAS group (robotic assisted splenectomy). Until 2011, all splenectomies were performed laparoscopically, and since then, with the start of the pediatric robotic surgery programme, these procedures were performed using the robotic approach. The indication for splenectomy was moderate to severe anemia and recurrent blood transfusions (> 2 per year). In those patients in whom symptomatic cholelithiasis was demonstrated, cholecystectomy was performed during the same operation. All patients were checked for adequate immunization against Streptococcus pneumonia, Haemophilus influenzae and Neisseria meningitidis, and in cases where vaccines had not been administered, they were immunized at least 1 month prior to splenectomy.
Data collected
Demographic data, clinical features (underlying hematological disease, spleen size, cholelithiasis-related symptoms, and need for pre-operative transfusion), intraoperative data (blood loss, surgery time, intraoperative complications and conversion to open surgery), length of hospital stay (LOS), postoperative complications and readmission rate (both within 30 days), need for postoperative blood transfusion, and economic associated cost were compared in both groups. Before surgery, ultrasound and/or computed tomography scans were used to measure the length of the spleen in all instances. Blood loss during surgery was assessed by measuring the amount of blood drawn into the suction system tube. Surgery time duration was defined as the time from the initial skin incision to the closure of the skin. For the RAS group, this duration encompassed the setup time, involving tasks such as positioning trocars and docking the robotic system. Postoperative complications were assessed and categorized using the Clavien–Dindo classification of surgical complications [9]. Prior to discharge, blood tests were performed in all patients. If hemoglobin values were below 9 g/dl, postoperative blood transfusion was indicated following the recommendations of the American Society for Hematology Education Program [10, 11]. After being discharged, all patients underwent regular follow-up appointments at the outpatient clinic. Overall costs associated to each group were calculated as the sum of the costs related to surgery, admission and readmissions/complications, and were computed based on itemized charges provided by the billing department. The study was conducted in accordance with the STROBE guidelines [12], and with the Declaration of Helsinki (as revised in 2013). Institutional Review Board approval (IRB number 1945724-1) was obtained for both study design and patient data collection authorization. Informed consent was not necessary due to the study’s retrospective design and the utilization of anonymized data management.
Procedural details
Robotic surgeries were carried out employing the DaVinci Si® double-console robotic system (Intuitive Surgical, Inc., Sunnyvale, CA, United States). All cases were performed under general anesthesia with the patient in supine reverse Trendelenburg position. Trocar placement replicated the configuration used for laparoscopic splenectomy, and the same steps were adhered to in both approaches. Peritoneal attachments and splenic ligaments were separated using electrocautery. The omental bursa was incised, and transection was performed, accompanied by the bipolar sealing of short gastric vessels. Both poles of the spleen were mobilized until the hilum was well exposed and could be effectively divided using a 10 mm endostapler (vascular cartridge).
Statistical analysis
Data were gathered using Microsoft Excel software version 2010 (Redmond, Washington, United States), and then analyzed using SPSS Statistic version 22 (Chicago, Illinois, United States). Continuous variables were presented as mean and standard deviation when they followed a normal distribution, or as median and interquartile range (Q1–Q3) if they did not. The normal distribution of variables was assessed using the Shapiro–Wilk test. For normally distributed continuous variables, the independent samples Student’s t test was utilized, while the Mann–Whitney test was employed for those not normally distributed. Categorical variables were expressed as frequency and percentage and were subjected to analysis through the Chi-square test or Fisher’s test when applicable. Odds ratios (OR) were calculated, accompanied by 95% confidence intervals. All statistical calculations were conducted with a two-tailed approach, and significance was determined by a p value of less than 0.05.
Results
We included a total of 84 patients (23 in LAS group and 61 in RAS group), with no differences in demographics, underlying hematological disease or spleen size between them. Sickle cell disease was the most frequent reason for splenectomy in both groups. Table 1 summarizes demographic data and patient characteristics.
For intraoperative features, RAS patients presented a significantly shorter surgery time (135 ± 39 vs. 182 ± 68 min; p = 0.043) and lower intraoperative blood loss (42 ± 15 vs. 158 ± 39 ml; p < 0.021) when compared to LAS patients. There were no intraoperative complications or conversions to open surgery in either group. Associated cholecystectomy was performed at the same operation in 18% of RAS patients and in 13% of LAS (p = 0.708). In most patients, the spleen was removed by endobag via the umbilical trocar. In large cases, a mini infra-umbilical laparotomy was performed to achieve complete removal. There was no difference in mean spleen weight between the two groups. Table 2 shows the intraoperative features in both groups.
Regarding postoperative features, no differences in median LOS were observed (3 days in both groups). When analyzing 30-day outcomes, five postoperative complications were reported: 4 in LAS patients (17.4%) versus only one in RAS (1.6%; p = 0.021). In the LAS group, one additional reintervention (Clavien–Dindo IIIb) was necessary due to hemoperitoneum occurring 12 h following splenectomy in a child who had been on long-term aspirin treatment and had a wound site infection. The decision for reoperation was prompted by escalating abdominal discomfort during examination, and the surgical exploration revealed a moderate accumulation of hematoma without any ongoing source of active bleeding. Three small bowel obstructions were reported (2 in the LAS group and 1 in RAS) which were managed conservatively with nasogastric tube and parenteral nutrition for several days, without the need for surgical reintervention (Clavien–Dindo II). RAS patients had significantly lower postoperative blood transfusion requirements (1.6 vs. 13.0%; p = 0.025) and lower readmission rate (3.3 vs. 17.4%; p = 0.042). Although the median surgery cost was higher in the RAS group ($5847 vs. $2155), robotic group patients had lower complications cost, so ultimately no differences were observed when comparing the median economic overall cost ($25,645 LAS vs. $28,135 RAS; p = 0.215). Postoperative results and economic data are provided in Table 3.
Discussion
This study compares the outcomes and costs of laparoscopic and robotic splenectomy in children with hematological disorders leading to splenomegaly, medically refractory cytopenia, and transfusion dependency. Clinical symptoms determine the indications and timing of intervention [1]. Splenectomy effectively resolves splenic sequestration and consequent splenomegaly, except in cases of ITP where the treatment’s efficacy lies in eliminating the splenic phagocytes responsible for platelet destruction [13]. The majority of patients in our study were black children with SCD, as this disease is more prevalent in this ethnicity. The second cause of splenectomy in both groups was HS, mainly in Caucasian patients. The absence of differences in demographic and clinical data between patients in both groups means that they can be considered comparable. As they were included in one group or the other consecutively (until 2011 laparoscopic and until 2021 robotic), there was no potential selection bias.
A few years ago, we described our preliminary experience with the first 30 cases of robotic splenectomy [14]. After re-analyzing the data including two times the initial number of patients, we have observed relevant findings. Robotic splenectomy operating time has been reduced by more than 30 min on average, which is probably due to the learning curve of both the surgeon and the rest of the team (anesthesia, nursing, etc.). Time loss in this procedure is mainly a result of the time-consuming positioning of the system and the delicate port placement, so the greater the number of procedures performed, the greater the reduction in surgery time achieved [15, 16]. The robot allowed for less operative time compared with standard laparoscopy even though some of the cases included cholecystectomies. In addition, the hospital stay has been reduced to 3 days, which is probably a consequence of the reduction of surgery time, intraoperative bleeding and the consequent lower need for postoperative transfusions. This aspect carries notable significance, especially for individuals affected by SCD, wherein extended anesthesia durations were previously believed to correlate with an increased occurrence of postoperative complications in this group of patients [17]. The results of our study are similar to those described by Giza et al. who noted improved operative time and blood loss when performing more complex splenectomies with the robotic assisted platform compared to laparoscopic splenectomy in adult patients [18].
The robotic system furnishes a stable camera platform that offers an enhanced view, owing to three-dimensional imaging, along with instruments featuring increased degrees of freedom and a more ergonomic positioning for the surgeon [19]. This is especially important in narrow or otherwise hardly accessible anatomical fields, such as the pelvis or the subdiaphragmatic regions [20, 21]. The use of tools with greater mobility allows for more precise hemostasis, thus reducing intraoperative bleeding and consequently decreasing the need of blood transfusion and the risk of postoperative complications compared to laparoscopy [21]. In our study, one LAS patient had to be reoperated due to bleeding at the surgical site, which caused pain and decrease in the patient’s hemoglobin values. There were no re-interventions in the robotic group. The lower need for blood transfusion observed in the ROB group may be due on the one hand to less intraoperative bleeding, and on the other hand to the shorter operative time, which reduces the surgical stress in this group of patients compared to the laparoscopic group.
Comparative studies between laparoscopic and robot-assisted splenectomy in children and adolescents are limited. Shelby et al. reported 24 splenectomies (14 laparoscopic and 10 robotic) with a lower LOS in the robotic group (2.1 days) compared to the laparoscopic group (3.2 days; p = 0.02), but with a higher associated cost in the robotic group ($44,724 vs $30,255; p = 0.01) [8]. However, they did not find a difference in operative time between the two cohorts (140.5 min in robotic group vs 154.9 min in laparoscopic). Recently, Belbahri et al. have reported 41 cases (26 laparoscopic and 15 robotic), with a median LOS higher than our results (6.5 days for laparoscopic group and 5 days for robotic), and with a robotic surgery time of 223 min [interquartile range 190–280], also higher than our study [7]. Both the authors conclude that robotic splenectomy in children remains safe, but offers no additional advantage compared to laparoscopy as the cost are higher.
Our study benefits from a 17-year-long evolving experience and encompasses a larger sample size compared to prior investigations. Our shorter operative time is probably due to the larger number of cases operated in our series (61 robotic splenectomies). The larger volume of surgeries has been shown to reduce the operative time per surgery and thus the cost of the intervention. Costs have repeatedly been one of the main criticisms of robotic surgery [21]. Comparing costs across different studies remains complex due to the inclination to report charges, variations in regional/market cost disparities, and the diverse methodologies employed to estimate expenses [22]. The fixed price of robotic and laparoscopic equipment should be excluded, as both costs are covered by the hospital and are not paid by the insurance companies or the patients. Given that robotic instruments can be reused up to ten times, a fraction of the initial purchase price, specifically one-tenth, was factored into the robotic assisted group. Despite this, the cost is still higher than single-use laparoscopic instruments. However, as the costs of instruments may decrease and both setup and operative times become shorter, the elevated expenses associated with robotic surgery might eventually become comparable to those of standard laparoscopy in the future.
In relation to the limitations of the study, it should be noted that most of them stem from its retrospective, single-institution design. The relatively small sample size is also a restriction, although given the small number of cases of splenectomy in children, our study constitutes the largest of those published to date. However, further multicenter studies with higher number of patients are still needed. This approach is essential for further cementing the role and applicability of robotic technology in the realm of pediatric surgery.
Conclusion
Robotic assisted splenectomy may be considered as a safe and feasible option in children compared to the traditional laparoscopic approach. The main benefits observed in this study were shorter surgery time, lower blood loss, less transfusion requirements, fewer postoperative complications and lower readmission rate. Nevertheless, additional research will be necessary to comprehensively grasp the optimal application of robot-assisted surgical methods within pediatric patients.
Data availability
Not applicable.
References
Iolascon A, Andolfo I, Barcellini W, Corcione F, Garçon L, De Franceschi L, Working Study Group on Red Cells and Iron of the EHA (2017) Recommendations regarding splenectomy in hereditary hemolytic anemias. Haematologica 102:1304–1313
Delaitre B, Maignien B, Icard P (1992) Laparoscopic splenectomy. Br J Surg 79:1334
Cavaliere D, Solaini L, Di Pietrantonio D, D’Acapito F, Tauceri F, Framarini M et al (2018) Robotic vs laparoscopic splenectomy for splenomegaly: a retrospective comparative cohort study. Int J Surg 55:1–4
Bhattacharya P, Phelan L, Fisher S, Hajibandeh S, Hajibandeh S (2022) Robotic vs. laparoscopic splenectomy in management of non-traumatic splenic pathologies: a systematic review and meta-analysis. Am Surg 88:38–47
Peng F, Lai L, Luo M, Su S, Zhang M, He K et al (2020) Comparison of early postoperative results between robot-assisted and laparoscopic splenectomy for non-traumatic splenic diseases rather than portal hypertensive hypersplenism-a meta-analysis. Asian J Surg 43:36–43
Pepper VK, Rager TM, Diefenbach KA, Raval MV, Teich S, Michalsky MP (2016) Robotic vs. laparoscopic sleeve gastrectomy in adolescents; reality or hype. Obes Surg 26:1912–1917
Belbahri I, Planchamp T, Ait Aissa D, Larcher C, Mouttalib S, Le Mandat A et al (2023) Pediatric mini-invasive splenectomy comparing laparoscopy with or without robotic approach: a single-center study. J Laparoendosc Adv Surg Tech A 33:703–706
Shelby R, Kulaylat AN, Villella A, Michalsky MP, Diefenbach KA, Aldrink JH (2021) A comparison of robotic-assisted splenectomy and laparoscopic splenectomy for children with hematologic disorders. J Pediatr Surg 56:1047–1050
Thompson H, Jones C, Pardy C, Kufeji D, Nichols E, Murphy F, Davenport M (2020) Application of the Clavien-Dindo classification to a pediatric surgical network. J Pediatr Surg 55:312–315
Han H, Hensch L, Tubman VN (2021) Indications for transfusion in the management of sickle cell disease. Hematology Am Soc Hematol Educ Program 2021(1):696–703
Linder GE, Chou ST (2021) Red cell transfusion and alloimmunization in sickle cell disease. Haematologica 106(7):1805–1815
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, STROBE Initiative (2007) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 370:1453–1457
Neunert CE, Cooper N (2018) Evidence-based management of immune thrombocytopenia: ASH guideline update. Hematol Am Soc Hematol Educ Program 2018:568–575
Mbaka MI, Robl E, Camps JI (2017) Laparoscopic versus robotic-assisted splenectomy in the pediatric population: our institutional experience. Am Surg 83:e358–e359
Bodner J, Kafka-Ritsch R, Lucciarini P, Fish JH 3rd, Schmid T (2005) A critical comparison of robotic versus conventional laparoscopic splenectomies. World J Surg 29:982–985
Bennett WE Jr, Whittam BM, Szymanski KM, Rink RC, Cain MP, Carroll AE (2017) Validated cost comparison of open vs. robotic pyeloplasty in American children’s hospitals. J Robot Surg 11:201–206
Ingle SS, Ubale P (2011) Anesthetic management of a patient with sickle cell disease for common bile duct exploration. J Anaesthesiol Clin Pharmacol 27:547–549
Giza DE, Tudor S, Purnichescu-Purtan RR, Vasilescu C (2014) Robotic splenectomy: what is the real benefit? World J Surg 38:3067–3073
Meehan JJ, Sandler A (2008) Pediatric robotic surgery: a single-institutional review of the first 100 consecutive cases. Surg Endosc 22:177–182
Delgado-Miguel C, Camps JI (2022) Robotic Soave pull-through procedure for Hirschsprung’s disease in children under 12-months: long-term outcomes. Pediatr Surg Int 38:51–57
Delgado-Miguel C, Camps JI (2023) Robotic-assisted versus laparoscopic redo antireflux surgery in children: a cost-effectiveness study. Int J Med Robot. 2023:e2541
O’Kelly F, Farhat WA, Koyle MA (2020) Cost, training and simulation models for robotic-assisted surgery in pediatric urology. World J Urol 38:1875–1882
Funding
The authors have not disclosed any funding.
Author information
Authors and Affiliations
Contributions
All the authors contributed to the study conception and design. Carlos Delgado-Miguel collected the patients’ data, analyzed and interpreted them, and wrote the manuscript. Juan Camps performed critical revision, reviewed and corrected the manuscript. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval
The protocol of the study obtained the approval of Prisma Health Children’s Hospital Institutional Review Board (IRB number 1945724-1) and complied with the guidelines of the Declaration of Helsinki (as revised in 2013).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Delgado-Miguel, C., Camps, J.I. Robotic-assisted versus laparoscopic splenectomy in children: a costeffectiveness study. J Robotic Surg 18, 51 (2024). https://doi.org/10.1007/s11701-023-01783-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11701-023-01783-9