Abstract
A social media group, the International Hernia Collaboration (IHC), facilitates professional development among surgeons interested in hernia disease. The purpose of this study was to assess practice pattern differences among IHC surgeon members regarding a ventral incisional hernia (VIH) scenario. A single multiple-choice question, posted for 1 month on the IHC, assessed which operation was preferred for a healthy patient with a symptomatic, reducible primary VIH (5 × 6 cm). Responses were compared by surgeon practice location (US vs. World). In total, 371 IHC surgeons completed the survey. More respondents practicing in the US completed the survey (57.1% vs. 42.9%, P < 0.01). Respondents in the US cohort would select a robotic-assisted approach more frequently than World colleagues (47.6% vs. 8.8%, P < 0.01). More IHC surgeons in the US cohort would offer a robotic-assisted approach for primary VIH repair compared to World colleagues. Studies are warranted to investigate practice pattern differences related to VIH repair.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adoption of social media across surgical disciplines continues to grow, reaching not only small groups but surgical societies at large, therefore, it is important to investigate the impact of this expansion on care delivery [1]. Social media allows large groups of similarly interested health care providers to dialogue about current preferred practices and strategies to improve patient outcomes. One such platform, the International Hernia Collaboration (IHC), a closed Facebook group established by Dr. Brian Jacob in 2012, is designed to allow surgeons and other contributors the opportunity to learn and improve through the concept of community, specifically the exchange of ideas, the provision of education, and networking with peers. As of January 2019, the IHC included almost 7000 members.
Social media can facilitate professional development and measure clinical opinions across generational, geographical, and personal distinctions. In a recent survey of 208 surgeons and trainees, 70% felt social media benefits professional development [2]. A growing number of social media groups support health care professionals across surgical disciplines including, but not limited to, General Surgery, Colon and Rectal Surgery, Plastic Surgery, Otorhinolaryngology/Head and Neck Surgery, Neurological Surgery plus sub-specialties such as bariatric, gastrointestinal, and hernia surgery [3,4,5,6,7,8,9]. Specifically, the IHC facilitates the professional growth and education of interested and informed surgeons, nurse practitioners, physician assistants, surgical first assistants, surgical technologists, and nurses within the sub-specialty of hernia surgery. Real-time, worldwide input from IHC members allows for timely understanding of current preferred practices in hernia disease, robust discussion about hernia management, and various types of hernia-related research.
In addition to the growth of social media as a means for surgeons to communicate and learn, the evolution of robotic-assisted ventral incisional hernia repair (R-VIHR) may be impacting how surgeons practice. The United States of America (USA) continues to see a move toward minimally invasive approaches for VIH repair. Some of what is transpiring in the USA is occurring in other countries at various rates. Recent data suggest that surgeons in the USA select a laparoscopic approach to VIH repair only 15–20% of the time, with no variability by geographic region [10]. On the other hand, adoption of robot-assisted hernia repair is increasing rapidly in the USA but less so in the European Union and other parts of the world. The consulting firm, Deloitte recently estimated that in 2016 robot-assisted hernia repair comprised 19% of all hernia repairs in the US. This increased use of robot-assisted hernia repair came at the expense of fewer open hernia repairs (unpublished data, Intuitive Surgical, Inc., Sunnyvale, CA, USA).
Considering the growing popularity and use of social media among surgeons who manage hernia disease, this survey of IHC members aimed to determine if surgeons practicing in the USA, given a specific clinical scenario, would choose different management strategies compared to colleagues practicing outside the USA. The hypothesis was that more surgeons practicing in the USA would consider and/or offer R-VIHR repair compared to colleagues practicing outside the USA for a specific clinical scenario.
Methods
Briefly, the IHC “is an international [social media] platform for [those] interested in the repair of hernia and optimizing outcomes to come together to collaborate, share, [and] discuss…” hernia as a disease process. The closed Facebook (Facebook Inc., Menlo Park, CA, USA) group is internally monitored for content and HIPAA compliance. The survey, conducted in September 2017, comprised a single multiple-choice question based on a hernia-related scenario.
A convenience sample of IHC members was queried about a scenario in which a 50-year-old healthy male [body mass index (BMI) of 29 kg/m2] presented electively with a symptomatic, periumbilical reducible incisional hernia (5 × 6 cm) resultant from uncomplicated laparoscopic cholecystectomy 1 year prior. At the time of laparoscopic cholecystectomy, a 12 mm trocar was inserted through the linea alba at the umbilicus. The resultant fascial defect was closed using 2-0 polyglactin 910 suture in a figure-of-eight fashion. Participants were notified that the patient qualified for operation based on symptoms, desired repair, and did not have a defect necessitating separation of components (or other myofascial advancement flaps).
In a single multiple-choice question, participants were presented, in horizontal response format with left alignment, ten different operative strategies to manage this VIH. The survey was designed such that respondents were restricted by Facebook software from choosing more than one option. The order of responses (operative approaches) was presented randomly and changed frequently and automatically to minimize selection and/or social desirability biases. Choices of operative approach to VIH repair included: open—primary repair; open—onlay mesh repair; open intra- or pre-peritoneal mesh repair; laparoscopic—subcutaneous onlay mesh repair; laparoscopic—intraperitoneal mesh (IPOM) repair; laparoscopic—transabdominal preperitoneal (TAPP) repair; laparoscopic—retromuscular/totally extraperitoneal (eTEP) repair; robotic—TAPP repair; robotic IPOM repair; robotic eTEP repair. If the respondent would offer a hybrid (combined laparoscopic and open technique) approach to VIH repair in this clinical scenario, they were told to select the laparoscopic technique that best identified the preferred mesh location.
Thirty days after the survey question was posed to the IHC group, responses were collected (Microsoft Excel, Microsoft Inc., Redmond, WA, USA) and analyzed for overall trends and compared based on respondent practice location. Two cohorts—USA and Outside USA—were used to group surgeon respondents based on geography. Responses of all surgeons currently practicing in the USA were compared to surgeons practicing outside the USA. Practice locations were confirmed by review of surgeons’ Facebook profile and, when necessary, comprehensive Internet search.
The primary outcome metric was the proportion of respondents in each cohort who would choose a robotic-assisted VIH repair in this clinical scenario. Secondary outcomes included the proportion of respondents who would offer laparoscopic and open operations, and what specific operative approaches they would prefer. A sample size of 355 respondents was determined based on a total population of 4500 potential respondents, 5% margin of error, and 95% confidence interval. Data are presented as proportions and compared using Chi-square test with Yates’ correction (α = 0.05). QuickCalcs (GraphPad Software, Inc., La Jolla, CA, USA) was used for statistical analysis.
Results
In total, 371 IHC surgeon members completed the survey. More respondents practicing in the USA compared to outside the USA completed the survey (57.1% vs. 42.9%, P < 0.01). Regarding the primary outcome metric, respondents practicing in the USA would select a robotic-assisted approach to repair this type of VIH more frequently than colleagues practicing outside the USA (47.6% vs. 8.8%, P < 0.01). However, similar proportions of respondents practicing in the USA or outside the USA would choose an open (11.3% vs. 22.6%, P = 0.12) or laparoscopic/hybrid (41.0% vs. 68.6%, P = 0.12) approach, respectively (Fig. 1).
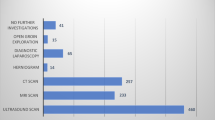
Many respondents (40.7%) would choose laparoscopic–intraperitoneal mesh (IPOM) repair for this clinical scenario. Respondents less frequently selected robotic–transabdominal preperitoneal (TAPP) repair (18.6%) or open–intra- or pre-peritoneal mesh repair (13.8%). When analyzing operative approaches with at least 10% response rate, the least frequent operation choices were laparoscopic–eTEP repair (10%) and robotic–IPOM repair (10.2%). Figure 2 depicts the number of respondents who selected each operative approach.
The responses of 371 surgeon members of the International Hernia Collaboration when asked about the operative approach they would select for a primary, reducible ventral incisional hernia. R robotic, L laparoscopic, O open, IPOM intraperitoneal onlay mesh, eTEP totally extraperitoneal, TAPP transabdominal preperitoneal, subq subcutaneous
Specifically, more respondents practicing in the USA would choose robotic–TAPP repair compared to those practicing outside the USA (29.7% vs. 3.8%, P < 0.01). Similarly, respondents in the USA cohort would perform robotic–IPOM repair more often than those in outside the USA cohort (15.6% vs. 2.5%, P < 0.01). There was a trend among respondents practicing outside the USA to select laparoscopic–TEP repair more often than those practicing in the USA, though it did not reach statistical significance (P = 0.07). All other comparisons of technique by practice location were not statistically significant (Fig. 3).
Responses of 371 surgeon members of the International Hernia Collaboration when asked about the operative approach they would select for a primary, reducible ventral incisional hernia. The USA cohort constitutes all surgeons currently practicing in the United States while World indicates surgeons practicing outside the United States. R robotic, L laparoscopic, O open, IPOM intraperitoneal onlay mesh, eTEP totally extraperitoneal, TAPP transabdominal preperitoneal, subq subcutaneous
Discussion
A convenience sample of IHC members was queried using social media. The overarching goal was to determine how responding surgeons would manage a 50-year-old healthy male with a symptomatic, primary periumbilical reducible incisional hernia (measuring 5 × 6 cm). Respondents chose from ten of the most common approaches to VIH repair.
VIH repair, especially abdominal wall reconstruction, requires a comprehensive, patient-centered management algorithm that enables matching of patient and repair technique to ensure optimum outcomes [11]. Principal management goals are to modify patient risk factors, minimize hospital length of stay and lower overall morbidity, reduce the risk of hernia recurrence, and improve patient quality of life. As hernia complexity and defect size increase, achievement of these patient-centered goals becomes more challenging.
A growing number of centers are investigating ways to accomplish these goals by shifting from open to minimally invasive techniques for complex VIH repair. Several comparative studies highlighted the utility of a robotic-assisted approach for complex abdominal wall reconstruction. In general, these studies showed that a robotic-assisted approach to complex abdominal wall reconstruction is feasible, safe, and yields at least equivalent short-term outcomes compared to an open approach. In similar and matched patient cohorts, the robotic-assisted approach significantly shortened hospital length of stay and lowered indirect hospital costs compared to the open approach [12,13,14].
Despite some shift toward selecting minimally invasive approaches for complex hernia repair, there is broad variability in practice patterns for VIH management. An expert panel convened to achieve consensus on preferred practices in VIH management. The panel and evidence support the preoperative modification of certain patient risk factors including obesity (BMI ≥ 30 kg/m2), tobacco use, and uncontrolled or poorly controlled diabetes mellitus (glycosylated hemoglobin ≥ 6.5%) [15]. In the clinical scenario created for this study, the patient was given a BMI of 29 kg/m2 with no history of tobacco use/dependence or diabetes mellitus to limit respondent bias toward non-operative management or a minimally invasive approach to VIH repair.
The present survey results echoed the conclusions of the expert consensus panel; operative management strategies for VIH vary appreciably [15]. The survey further highlighted the geographical differences in surgeons’ practice patterns. Specifically, the survey showed that IHC respondents practicing in the USA would more often choose a robotic-assisted VIH repair compared to colleagues practicing outside the USA. While this finding may be due to the greater availability of robotic surgical platforms or earlier adoption of robotic-assisted VIH repair in the USA, other important demographic, sociopolitical, and economic factors may impact the offering of robotic-assisted VIH repair [16].
Limitations of this survey study include a low response rate as well as respondent selection bias, non-response bias, and potentially social desirability bias (mitigated through use of forced-choice items and randomized response technique). The scenario and survey question were written to minimize leading bias but the question was not validated as neutral by pretesting. The list of ten different operative approaches offered as responses to the survey question is not exhaustive, but is representative of the most common hernia repair techniques worldwide. The convenience sample of IHC surgeon members may not reflect the opinions of all surgeons practicing in the USA or outside the USA. Respondents were not queried as to specific rationale for their choice of operation, which may be influenced not only by geographic location and robotic platform availability, but cost and quality metrics. If the survey was posted online for a longer period, at a different time, or for a second time, response frequency and results may change.
In conclusion, this survey of IHC surgeon members highlighted a difference in operative management of a generalizable clinical scenario between surgeons practicing in the USA and those practicing elsewhere in the World. An appreciably higher proportion of surgeons practicing in the USA would offer a robotic-assisted approach for primary VIH repair, while a similar proportion would choose an open or laparoscopic/hybrid approach compared to their colleagues throughout the World. Additional studies are warranted to investigate the potential explanations behind practice pattern differences as they relate to robotic-assisted VIH repair.
References
Speer AL, Kao LS (2017) The Association for Academic Surgery 2011-present: standing on the shoulders of giants. J Surg Res 217:20–24
Wagner JP, Cochran AL, Jones C et al (2018) Professional use of social media among surgeons: results of a multi-institutional study. J Surg Educ 75:804–810. https://doi.org/10.1016/j.jsurg.2017.09.008
Koball AM, Jester DJ, Domoff SE et al (2017) Examination of bariatric surgery Facebook support groups: a content analysis. Surg Obes Relat Dis 13:1369–1375
Khalifeh JM, Kaafarani HMA (2017) Surgery goals social: the extent and patterns of social medical utilization by major trauma, acute and critical care surgery societies. J Emerg Trauma Shock 10:103–110
Oyewumi M, Lee J, Vescan A (2017) Social media in otolaryngology–head and neck surgery. Ear Nose Throat J 96:E29–E33
Petrucci AM, Chand M, Wexner SD (2017) Social media: changing the paradigm for surgical education. Clin Colon Rectal Surg 30:244–251
Sorice SC, Li AY, Gilstrap J et al (2017) Social media and the plastic surgery patient. Plast Reconstr Surg 140:1047–1056
Samuel N, Alotaibi NM, Lozano AM (2017) YouTube as a source of information on neurosurgery. World Neurosurg 105:394–398
Lui DH, McDonald JJ, de Beaux Z et al (2017) Contemporary engagement with social media amongst hernia surgery specialists. Hernia 21:509–515
Huntington CR, Cox TC, Blair LJ et al (2016) Nationwide variation in outcomes and cost of laparoscopic procedures. Surg Endosc 30:934–946
Dietz UA, Fleischhacker A, Menzel S et al (2017) Risk-adjusted procedure tailoring lead to uniformly low complication rates in ventral and incisional hernia repair: a propensity score analysis and internal validation of classification criteria. Hernia 21:569–582
Bittner JG, Alrefai S, Vy M et al (2017) Comparative analysis of open and robotic transversus abdominis release for ventral hernia repair. Surg Endosc 32:727–734
Carbonell AM, Warren JA, Prabhu AS et al (2018) Reducing length of stay using robotic-assisted approach for retromuscular ventral hernia repair: a comparative analysis from the Americas Hernia Society Quality Collaborative. Ann Surg 267:210–217
Martin del Campo LA, Weltz AS, Belyansky I et al (2017) Comparative analysis of perioperative outcomes of robotic versus open transversus abdominis release. Surg Endosc 32:840–845
Liang MK, Holihan JL, Itani K et al (2017) Ventral hernia management: expert consensus guided by systematic review. Ann Surg 265:80–89
Jones DB, Stefanidis D, Korndorffer JR Jr et al (2017) SAGES University MASTERS Program: a structured curriculum for deliberate, lifelong learning. Surg Endosc 31:3061–3071
Acknowledgements
The authors would like to thank the surgeon members of the International Hernia Collaboration who contributed to this study.
Funding
No funding was received for the conduct of this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. James G. Bittner IV receives honoraria for speaking/teaching and fees for consulting from Intuitive Surgical, Inc. and BD Bard, Inc. unrelated to this work. Dr. Mercedeh Baghai has no conflicts of interest. Dr. Brian P. Jacob receives honoraria for speaking/teaching, fees for consulting, and funds for research from Medtronic, Inc., fees for consulting from Ethicon, Inc., and serves as Founder and President of International Hernia Collaboration, Inc.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bittner, J.G., Baghai, M. & Jacob, B.P. Management of a primary ventral incisional hernia: a survey of the International Hernia Collaboration. J Robotic Surg 14, 95–99 (2020). https://doi.org/10.1007/s11701-019-00940-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-019-00940-3