Abstract
Background/Aim
Adipose tissue can increase levels of inflammation and oxidative stress, which explains the relationship between obesity and many chronic diseases. Weight loss, changes in adipose tissue metabolism, and dietary nutrient intake changes following bariatric surgery could affect a number of oxidative- and inflammation-related factors. Therefore, this study aimed to assess the potential relationship between dietary intake and inflammatory/antioxidant markers in the 6 months following Roux-en-Y gastric bypass surgery (RYGB).
Material and Methods
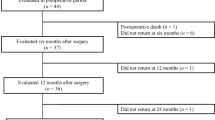
This pilot prospective cohort study included 45 patients with severe obesity who underwent RYGB. The patients were assessed at three different time points: baseline, 3 months, and 6 months post-surgery. Throughout the study, dietary intake data, levels of total antioxidant capacity (TAC), NF-κB, and serum levels of certain micronutrients were measured three times. Dietary macro- and micronutrient intake data were obtained three times throughout the study using the 24-h food recall questionnaire.
Results
The analysis of dietary indices in the present study found a significant positive correlation between the dietary intake of zinc, copper, MUFA, and serum TAC levels. It also revealed a significant inverse correlation between serum levels of NF-κB with vitamin E and PUFA intake. Additionally, there was a significant positive association between the amount of dietary carbohydrates and saturated fatty acids intake and the levels of NF-κB. Furthermore, within 3 to 6 months after the surgery, patients experienced an increase in serum levels of TAC, ferritin, vitamin D3, vitamin B12, and folate. However, there was a decrease in serum levels of NF-κB, zinc, and copper.
Conclusions
Weight loss and nutritional status may potentially impact oxidative stress and inflammation levels within 6 months following RYGB surgery. Further research is necessary to comprehensively investigate the different facets of this correlation and elucidate the precise underlying mechanism.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity is defined as an excess fat accumulation in the adipose tissue due to various factors such as genetics or lifestyle [1]. The adipose tissue itself can cause higher levels of inflammatory cytokines and oxidative markers, which could explain the correlation between obesity and many chronic diseases [2, 3]. The macrophages present in the adipose tissue could cause the generation of pro-inflammatory cytokines [4, 5]. The antioxidant defense system could also change in obese individuals. For example, reduced levels of catalase and glutathione could occur due to obesity, indicating a weakened antioxidant activity in patients with obesity [6,7,8]. Changes in dietary intake could also affect the level of inflammation and oxidative stress in individuals. Lower intakes of antioxidants such as vitamin C, E, and beta-carotene could also affect the oxidative balance [7,8,9].
Various approaches are recommended for the management of obesity, among which bariatric surgery is considered the most effective way for rapid and long-term weight loss in patients with severe obesity. Weight reduction could have a beneficial effect on the levels of inflammation and oxidative stress and could lower the risk of chronic diseases as well [4, 6]. However, the surgery itself could cause inflammatory responses and increase the levels of inflammatory mediators and reactive oxygen or nitrogen species. In addition, lower absorption of some dietary nutrients could also occur as a harmful effect of bariatric surgery [10]. Furthermore, many dietary changes would occur following bariatric surgery. Many food restrictions could occur after the surgery, which could affect the patients’ dietary nutrient intake, especially during the first year after the operation [11]. Recommendations for selecting healthy dietary patterns guide these patients towards higher consumption of specific foods or food groups such as fish, poultry, skim milk, and fruits, and lower consumption of sweets, red meat, soft drinks, and the like after bariatric surgery, which could affect their nutrient intake [12]. A complete diet, including appropriate daily nutrient intake, could affect oxidative stress and related diseases. Many nutrients could affect the antioxidant system, either as a component of this system or as direct antioxidants. However, the effect of various nutrients on oxidative balance is a matter of controversy [13]. Additionally, the clear association between inflammation and diet [14] shows the necessity of assessing this association in patients’ post-bariatric surgery.
As mentioned, many changes regarding oxidative and inflammatory markers could occur due to changes in adipose tissue following weight reduction after bariatric surgery. These changes are accompanied by dietary changes in this population due to dietary restrictions or changes in dietary habits. There are limited reports regarding changes in dietary intake post-operatively and their correlations with inflammatory and antioxidant markers. Hence, this pilot study aimed to assess the relationship between dietary intake of macro- and micronutrients and inflammatory and antioxidant markers in the period of 6 months after Roux-en-Y gastric bypass surgery (RYGB).
Materials and Methods
Ethics Statement
This study was approved by the Ethics Committee of the Tehran University of Medical Sciences (Ethics number: IR.TUMS.MEDICINE.REC.1400.011). Participants were provided with an explanatory letter detailing the study, and written informed consent was obtained from all participants before they entered the project.
Study Design, Setting, and Participants
This pilot prospective cohort study was conducted from December 2022 to July 2023. It included 45 patients between the ages of 20 and 50 with severe obesity who underwent bariatric surgery and had a BMI between 40 and 50 kg/m2. All surgeries were performed by a specific surgeon (A.P) at Hazrat-e Rasool General Hospital, Tehran, which is recognized as a Center of Excellence by the International Federation for Surgery of Obesity. The surgical technique used was Roux-en-Y gastric bypass, with a pouch size of 25–30 mL and a Roux-en-Y limb of 130–150 cm. The laparoscopic technique with a five-port approach was utilized.
To be eligible for the study, participants had to be willing to participate and have not been involved in any specific diet program such as vegetarian, ketogenic, or intermittent fasting diet (apart from the usual post-operative protocol) before and during the 6 months following the surgery. Patients who had previously undergone bariatric surgery or reversal; were pregnant or breastfeeding; smoked at least five cigarettes per day for the past 6 months; had kidney disease, pancreatitis, cancer, uncontrolled thyroid disorders, inflammatory, neurological, or autoimmune diseases; or had a history of heart attacks and strokes were excluded from the study. Patients who withdrew from surgery, cooperation in the study, or became pregnant during the follow-up were also excluded.
Clinical, anthropometric, and biochemical variables were assessed in all patients at 3 and 6 months after the surgery.
Variables, Data Sources/Measurement
Anthropometric and Dietary Intake Measurements
Height was measured without shoes using a measuring tape attached to a wall, with a nearest 0.5 cm precision. Body weight was measured through a scale with maximum accuracy (the SECA 711 scale, Medical Measuring Systems, and Scales Factory, USA), requesting participants to remove heavy clothes and shoes. Patients’ height was measured using a strip gauge with an accuracy of 0.1 cm and without shoes, while the back of the head, shoulder blades, buttocks, and heels were touching the stadiometer. All of the participants completed the 24-h food recall questionnaire three times throughout the study period.
Weight loss was assessed using % total weight loss (TWL) and % excess weight loss (EWL). % TWL was calculated as [(preoperative weight − weight at follow-up) / preoperative weight] × 100. % EWL was calculated as [(preoperative weight − weight at follow-up) / (preoperative weight − ideal body weight)] × 100. % EBMIL was calculated using the formula: (Excess BMI Loss) = 100 * (Initial BMI – Post-operative BMI) / (Initial BMI − 25). In addition, ΔBMI was calculated as (Initial BMI – Post-operative BMI). Ideal weight was defined as the weight corresponding to a BMI of 25 kg/m2.
Laboratory Measurement
The participants completed fasting blood samples (10 ml) for biochemical assessments. Samples were taken at baseline and at the end of each study phase in the early morning after an overnight fast. The samples were immediately centrifuged (Hettich D-78532, Tuttlingen, Germany) at 3500 rpm for 10 min to separate serum and then stored at − 80 °C before laboratory analysis. ELISA kits (Human ELISA Kit, Shanghai Crystal Day Biotech Co., Ltd) were used to measure the levels of TAC and NF-κB. All measurements were performed using the ELISA method. In addition, serum laboratory parameters including serum hemoglobin (Hb), ferritin, albumin, vitamin D3, vitamin B12, folic acid, zinc, and copper were recorded. The 24-h food recall questionnaire was completed three times throughout the evaluation period.
Post-OperativeCare
All patients were required to visit the obesity clinic for multiple assessments of weight loss, blood sample collection, and food recall at 1, 3, and 6 months after the surgery. According to international bariatric surgery guidelines, patients started taking daily multivitamins and mineral supplements, as well as calcium citrate (500 mg) twice daily, beginning the day after surgery. Additionally, all patients received monthly intramuscular neurobion injections (including 1000 μg of vitamin B12, 100 mg of vitamin B1, and 100 mg of vitamin B6) and oral vitamin D3 (50,000 IU) following the surgery. The diet protocol for patients undergoing bariatric surgery was thoroughly explained during regular post-surgery visits. This included a clear liquid diet for the first 2 days, a full liquid diet from the second to the fourteenth day, a soft diet from the 14th to the 28th day, a puree diet from the 28th day to 1.5 months post-operation, and finally, the usual table food at 1.5 months post-operation. All patients were advised to engage in exercise, specifically aerobic and strength activities.
Statistical Methods
We used the Kolmogorov–Smirnov test to check the normal distribution of variables. Continuous variables were presented as means and standard error. To assess the interaction effect of time and surgery on each outcome, we conducted repeated measures ANOVA analysis. Multivariate linear regression models were used to predict the association between the mean changes of TAC/NF-κB and other clinical variables, including anthropometric indices, dietary intake measurements, and biochemical parameters. Age, sex, and BMI were adjusted as covariates in the multivariable analysis. Statistical significance was defined as a P-value less than 0.05, and we performed the analysis using SPSS 26.0.
Results
Patient Characteristics
The mean age of our study population was 40.47 ± 9.6 years, with a total of 45 patients. Of these patients, 41 (91%) were female, 15 (33.3%) had diabetes, and 13 (28.8%) had hypertension. The average weight and BMI of the patients were 119.65 kg and 44.66 kg/m2, respectively. To analyze food habits, we categorized the patients into four subgroups: volume eating (36 patients, 80%), emotional eating (26 patients, 57.7%), grazing (30 patients, 66.7%), and sweet eating (28 patients, 62.2%). Table 1 presents the clinical and demographic characteristics of the study participants.
Weight Loss and Dietary Intake Trends at Four Time Points Before and After Surgery
The repeated measures ANOVA (with Greenhouse–Geisser correction) showed consistent trends in changes in weight and BMI patterns. However, no consistent trends were observed in changes in the proportion of dietary intake patterns across visits. The present study found that at 1, 3, and 6 months after surgery, patients experienced significant decreases in weight and BMI compared to the baseline (P < 0.001). Additionally, the percentage of total weight loss (TWL), excess weight loss (EWL), and excess BMI loss (EBMIL) increased over time (P < 0.001) (Table 2). In terms of nutrient intake, the mean intakes of selected nutrients sharply decreased during the first month after surgery. However, a gentle increasing trend was observed at 3 and 6 months post-surgery (P < 0.001) (Table 3) (Fig. 1).
Serum Levels of TAC, NF-κB, and Dietary Intake Indicators Before and After Surgery
Following the surgery, the mean levels of TAC, NF-κB, Hb, ferritin, albumin, vitamin D3, vitamin B12, folate, zinc, and copper were sequentially measured at two different time points. The changes in TAC levels observed during the study indicated an increasing trend in patients, while the serum levels of NF-κB showed a decreasing trend. The repeated measures ANOVA (with Greenhouse–Geisser correction) revealed that within 3 and 6 months after the surgery, the serum levels of TAC, ferritin, vitamin D3, vitamin B12, and folate increased in patients, while the serum levels of NF-κB, zinc, and copper decreased (Table 4).
Predictive Validity of Dietary Intake Indicators for Total Antioxidant Capacity (TAC) Levels 6 Months After Surgery
We investigated the relationship between serum TAC levels and specific micro-/macronutrients in patients who underwent bariatric surgery. Analysis of the dietary intake indicators revealed a significant positive correlation between serum TAC levels and the intake of zinc, copper, and MUFA. This means that an increase in the intake of zinc, copper, and MUFA was associated with an increase in TAC levels. Furthermore, there was a significant negative correlation between TAC levels and dietary cholesterol levels. This indicates that an increase in cholesterol intake was linked to a decrease in TAC levels. There was no significant correlation between TAC concentrations and other dietary intake indicators (Table 5).
Predictive Validity of Dietary Intake Indicators for NF-κB Values 6 Months After Surgery
We investigated the relationship between serum NF-κB values and specific micro-/macronutrients in patients who underwent bariatric surgery. Analysis of dietary intake indicators showed a significant inverse correlation between serum NF-κB values and intake of vitamin E and PUFA. This means that a higher intake of vitamin E and PUFA was linked to lower NF-κB values. Additionally, we found a significant positive correlation between NF-κB values and dietary intake of SFA and carbohydrates. This suggests that a higher intake of dietary SFA and carbohydrates was associated with increased NF-κB values. No significant association was found between NF-κB values and other dietary intake indicators (Table 6).
Discussion
Dietary changes and weight reduction after bariatric surgery can affect various metabolic disorders, inflammatory markers, and oxidative markers. Regarding dietary changes in the present study, there was a decrease in some dietary intakes during the first month post-surgery, while others increased at 3 and 6 months post-surgery. Many studies have examined the dietary intakes of patients at different time points after surgery. For example, a study by Ziadlou et al. reported that most dietary intakes of micro/macronutrients increased between 6 and 12 months post-surgery [11]. The variations in dietary intakes observed between studies were mainly due to differences in surgical procedures, participant characteristics, patient education, follow-up duration, and other factors. Based on repeated measurements analysis in present study, serum levels of TAC, ferritin, vitamin D3, vitamin B12, and folate increased in patients, while serum levels of NF-κB, zinc, and copper decreased at 3 and 6 months after surgery.
Furthermore, the assessment of the relationship between dietary intakes and total antioxidant capacity (TAC) levels in patients undergoing bariatric surgery revealed a significant positive association between serum TAC levels and zinc, copper, and monounsaturated fatty acid (MUFA) intake. Therefore, increasing dietary intake of zinc, copper, and MUFA can significantly enhance TAC levels. Conversely, there was a significant negative association between TAC and dietary cholesterol levels, indicating that an increase in dietary cholesterol intake could decrease TAC levels.
According to the findings of the present study, it is clear that the dietary changes that happened after the bariatric surgery could explain the reason for some changes. For example, higher protein intake in the present study could increase the dietary intake of zinc, and this could in turn increase the level of TAC as it was seen. Several mechanisms could possibly describe the association between dietary intakes and oxidative stress. Considering the positive association between dietary copper intake and TAC, it can be mentioned that copper is considered as a pro-oxidant or antioxidant agent depending on the situation. It is asserted that copper could induce the antioxidant activity of Cn/Zn/SOD (copper-zinc-superoxide dismutase) and this could possibly describe the positive association observed [15]. On the other hand, it is clear that zinc deficiency is correlated with oxidative stress [16], and this could justify the positive relationship between dietary zinc intake and TAC level. Zinc, as important mineral, can interact with some groups such as the sulfhydryl or thiol groups in proteins, and in this way, it can decrease their reactivity for causing oxidative stress [17]. Moreover, zinc is essential for the production of metallothioneins (MTs) as the proteins rich in cysteine [18], and this protein can act as a scavenger for ameliorating oxidative stress. In addition, zinc could increase the level of glutathione (GSH) as a potent antioxidant [19] which is a component of antioxidant system in the body. Hence, the aforementioned effects attributed to zinc could possibly justify the positive association between dietary zinc and TAC. As another mechanism for the relationship between dietary intakes and oxidative stress, it was found that dietary MUFAs could decrease the chance of lipid peroxidation in the membranes and this could enhance the antioxidant system by inhibiting the production of DNA-modifying factors [20]. Hence, it seems logical to see a positive association between dietary intakes of MUFAs and TAC due to the protective effects of MUFAs against oxidative stress.
On the other hand, the negative correlation between TAC and dietary cholesterol intake could be explained by the detrimental effects of cholesterol on oxidative damage and mitochondrial dysfunction [21]. This oxidative damage and increase in free radicals may be accompanied by a decrease in endogenous antioxidants. Therefore, it is possible that dietary cholesterol intake indirectly decreases TAC levels through a direct increase in oxidative stress [22]. Furthermore, the present study found a significant negative association between serum NF-κB values and vitamin E and PUFA intake. This means that an increase in dietary consumption of vitamin E and PUFA is accompanied by a decrease in NF-κB levels. Additionally, there was a significant positive association between NF-κB levels and dietary SFA and carbohydrate, suggesting that an increase in SFA and carbohydrate intake could lead to an increase in NF-κB levels. The inverse association observed between dietary vitamin E and NF-κB levels highlights the anti-inflammatory effects of vitamin E, as it can reduce C-reactive protein and pro-inflammatory cytokines [23]. Vitamin E also inhibits cyclooxygenase-2 (COX-2), which further contributes to its anti-inflammatory effects [24]. Additionally, the inhibition of interleukin-1 (an NF-κB inducer) by vitamin E [25] may explain the inverse association between vitamin E intake and NF-κB levels. Another dietary component with an inverse association with NF-κB is PUFA. Dietary fatty acids, such as PUFAs, can affect membrane features, including fluidity, receptor function, and lipid raft formation [26, 27]. The type of PUFA plays an essential role in the balance between pro- and anti-inflammatory cytokines [28]. Omega-3, which is an important PUFA, has been shown to have anti-inflammatory properties [29]. Therefore, the inverse correlation observed in the present study may be attributed to omega-3 as a significant PUFA.
As demonstrated in the present study, dietary changes were observed after bariatric surgery that could potentially impact the levels of inflammatory markers. For example, the current study reported a decrease in carbohydrate intake after surgery, which would likely lead to reduced inflammation, consistent with the findings of this study. Another study also found that higher carbohydrate intake was associated with weight regain after bariatric surgery, which may indicate fat accumulation. Based on this evidence, it is known that any increase in adipose tissue is linked to elevated levels of inflammation [30]. The direct relationship between dietary carbohydrate intake and NF-κB can be explained by mechanisms that focus on the effects of high dietary carbohydrate on inflammation. Higher intake of dietary carbohydrates can lead to increased MCP-1, a chemokine that has pro-inflammatory effects. Additionally, dietary carbohydrate intake can potentially decrease galectin-3, an anti-inflammatory agent [31]. Furthermore, high dietary carbohydrate intake can result in elevated blood glucose levels and phosphorylation of IκB kinase, which activate the NF-κB pathway and subsequently trigger the secretion of inflammatory signals [32, 33]. Therefore, it can be argued that dietary carbohydrate, particularly at higher levels, can induce the NF-κB pathway and promote inflammation. This may explain the direct association between dietary carbohydrate intake and NF-κB. Regarding the last finding, the positive correlation between dietary SFAs and NF-κB can be explained by certain facts about the inflammatory effects of SFAs. Dietary SFAs can activate NF-κB and mitogen-activated protein kinase, both of which enhance the genes associated with inflammation in various tissues [34]. Thus, it is reasonable and expected to observe a direct association between SFA intake and NF-κB.
Regarding the changes in TAC and NF-κB after bariatric surgery, previous studies have clearly demonstrated their positive effects on oxidative stress levels at the 6-month mark after the procedure [35, 36]. Consistent with this study, Pinto et al. also observed a decrease in oxidative stress markers at 3 and 12 months post-surgery in individuals who underwent RYGB [37]. Furthermore, various studies have reported a decrease in inflammatory markers and an increase in antioxidants over a 6-month period following RYGB surgery [38, 39]. These changes can be attributed to the reduction in NF-κB, a factor that triggers inflammation [40]. There are several mechanisms that could explain the observed changes after bariatric surgery. One potential mechanism is related to the impact of weight loss on NF-κB. Weight loss following bariatric surgery has the potential to increase the levels of the receptor for the soluble form of advanced glycation end-products (sRAGE). This receptor, which is present in the plasma, can bind to RAGE and prevent the interaction between RAGE and the inflammatory pathway ligands mediated by NF-κB [41, 42].
This study had some limitations. First, the study only followed up with participants for 6 months, which may not be long enough to observe weight regain and dietary changes that could be associated with changes in oxidative stress and inflammation. This study was also limited by the small sample size. Unfortunately, we were unable to increase the sample size due to research budget constraints. Additionally, due to the design of the study, it was not possible to establish causal relationships. On the other hand, assessing dietary intakes to determine nutrient levels before and after surgery may be limited by recall bias. Another limitation is that the study only considered one type of bariatric surgery (RYGB), while other types of surgery may result in different changes post-operatively. It would be interesting to compare various types of surgery. However, a strength of the study is that it comprehensively assessed dietary intakes and serum levels, as well as inflammatory and antioxidant markers before and after surgery. Furthermore, it examined changes over time. However, further studies are needed to confirm the observed relationships.
Conclusion
This study showed that in patients undergoing RYGB, higher intakes of zinc, copper, and MUFA, as well as lower intakes of cholesterol, were associated with higher TAC levels, emphasizing the protective effects of dietary changes on oxidative balance. On the other hand, higher dietary vitamin E and PUFA, and lower carbohydrate and SFA intakes, were associated with lower NF-κB levels as a marker of inflammation. Therefore, weight reduction and dietary management after bariatric surgery may potentially impact oxidative stress and inflammation levels within a 6-month period after RYGB. The clinical implications of this study suggest that training the individuals underwent bariatric surgery to adhere to a healthy, nutritious diet containing an abundance of unsaturated fatty acids and antioxidants, while restricting their consumption of carbohydrates and saturated fatty acids post-bariatric surgery, can enhance the metabolic outcomes of the surgery by promoting antioxidant/inflammatory balance.
However, further studies are needed to better understand the exact correlations between dietary intakes and oxidative stress and inflammation after bariatric surgery, particularly over longer durations and with larger sample size.
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Change history
26 August 2024
A Correction to this paper has been published: https://doi.org/10.1007/s11695-024-07436-6
References
Consultation W. Obesity: preventing and managing the global epidemic. World Health Organization technical report series 2000;894:1–253.
Serra A, Granada M, Romero R, et al. The effect of bariatric surgery on adipocytokines, renal parameters and other cardiovascular risk factors in severe and very severe obesity: 1-year follow-up. Clin Nutr. 2006;25(3):400–8.
Uzun H, Zengin K, Taskin M, et al. Changes in leptin, plasminogen activator factor and oxidative stress in morbidly obese patients following open and laparoscopic Swedish adjustable gastric banding. Obes Surg. 2004;14(5):659–65.
Higdon JV, Frei B. Obesity and oxidative stress: a direct link to CVD? Am Heart Assoc. 2003;23:365–7
Choi JW, Pai SH, Kim SK, et al. Increases in nitric oxide concentrations correlate strongly with body fat in obese humans. Clin Chem. 2001;47(6):1106–9.
Kisakol G, Guney E, Bayraktar F, et al. Effect of surgical weight loss on free radical and antioxidant balance: a preliminary report. Obes Surg. 2002;12(6):795–800.
Tungtrongchitr R, Changbumrung S, Tungtrongchitr A, et al. The relationships between anthropometric measurements, serum vitamin A and E concentrations and lipid profiles in overweight and obese subjects. Asia Pac J Clin Nutr. 2003;12(1):73–9.
Brown LA, Kerr CJ, Whiting P, et al. Oxidant stress in healthy normal-weight, overweight, and obese individuals. Obesity. 2009;17(3):460–6.
Suzuki K, Inoue T, Hioki R, et al. Association of abdominal obesity with decreased serum levels of carotenoids in a healthy Japanese population. Clin Nutr. 2006;25(5):780–9.
Olusi S. Obesity is an independent risk factor for plasma lipid peroxidation and depletion of erythrocyte cytoprotectic enzymes in humans. Int J Obes. 2002;26(9):1159–64.
Ziadlou M, Hosseini-Esfahani F, Mozaffari Khosravi H, et al. Dietary macro-and micro-nutrients intake adequacy at 6th and 12th month post-bariatric surgery. BMC Surg. 2020;20:1–9.
Benaiges D, Parri A, Subirana I, et al. Most of qualitative dietary changes observed one year post-bariatric surgery can be achieved with a preoperative dietary intervention. Endocrinol Diabetes Nutr. 2020;67(1):20–7.
Arrigo T, Leonardi S, Cuppari C, et al. Role of the diet as a link between oxidative stress and liver diseases. World J Gastroenterol: WJG. 2015;21(2):384.
Graff E, et al. Dietary intake and systemic inflammation: can we use food as medicine? Curr Nutr Rep 2023;12(2):247–54.
Boesing F, Moreira EAM, Wilhelm-Filho D, et al. Roux-en-Y bypass gastroplasty: markers of oxidative stress 6 months after surgery. Obes Surg. 2010;20:1236–44.
Abulmeaty MM, Ghneim HK, Alkhathaami A, et al. Inflammatory cytokines, redox status, and cardiovascular diseases risk after weight loss via bariatric surgery and lifestyle intervention. Medicina. 2023;59(4):751.
Monte SV, Caruana JA, Ghanim H, et al. Reduction in endotoxemia, oxidative and inflammatory stress, and insulin resistance after Roux-en-Y gastric bypass surgery in patients with morbid obesity and type 2 diabetes mellitus. Surgery. 2012;151(4):587–93.
Gletsu-Miller N, Hansen JM, Jones DP, et al. Loss of total and visceral adipose tissue mass predicts decreases in oxidative stress after weight-loss surgery. Obesity. 2009;17(3):439–46.
Sledzinski T, Goyke E, Smolenski R, et al. Decrease in serum protein carbonyl groups concentration and maintained hyperhomocysteinemia in patients undergoing bariatric surgery. Obes Surg. 2009;19:321–6.
Pinto SL, Juvanhol LL, de Oliveira LL, et al. Changes in oxidative stress markers and cardiometabolic risk factors among Roux-en-Y gastric bypass patients after 3-and 12-months postsurgery follow-up. Surg Obes Relat Dis. 2019;15(10):1738–45.
Melissas J, Malliaraki N, Papadakis JA, et al. Plasma antioxidant capacity in morbidly obese patients before and after weight loss. Obes Surg. 2006;16(3):314–20.
Brix J, Höllerl F, Kopp H, et al. The soluble form of the receptor of advanced glycation endproducts increases after bariatric surgery in morbid obesity. Int J Obes. 2012;36(11):1412–7.
Furukawa S, Fujita T, Shimabukuro M, et al. Increased oxidative stress in obesity and its impact on metabolic syndrome. J Clin Investig. 2017;114(12):1752–61.
Marfella R, Barbieri M, Ruggiero R, et al. Bariatric surgery reduces oxidative stress by blunting 24-h acute glucose fluctuations in type 2 diabetic obese patients. Diabetes Care. 2010;33(2):287–9.
Bo S, Durazzo M, Gambino R, et al. Associations of dietary and serum copper with inflammation, oxidative stress, and metabolic variables in adults. J Nutr. 2008;138(2):305–10.
King JC, Brown KH, Gibson RS, et al. Biomarkers of nutrition for development (BOND)—zinc review. J Nutr. 2015;146(4):858S-S885.
Bray TM, Bettger WJ. The physiological role of zinc as an antioxidant. Free Radical Biol Med. 1990;8(3):281–91.
Westin G, Schaffner W. A zinc-responsive factor interacts with a metal-regulated enhancer element (MRE) of the mouse metallothionein-I gene. EMBO J. 1988;7(12):3763–70.
Cortese MM, Suschek CV, Wetzel W, et al. Zinc protects endothelial cells from hydrogen peroxide via Nrf2-dependent stimulation of glutathione biosynthesis. Free Radical Biol Med. 2008;44(12):2002–12.
Pamplona R, et al. Membrane fatty acid unsaturation, protection against oxidative stress, and maximum life span: a homeoviscous‐longevity adaptation? Annals of the New York Academy of Sciences 2002;959(1): 475–90.
Rauchbach E, Zeigerman H, Abu-Halaka D, et al. Cholesterol induces oxidative stress, mitochondrial damage and death in hepatic stellate cells to mitigate liver fibrosis in mice model of NASH. Antioxidants. 2022;11(3):536.
Rochette L, Zeller M, Cottin Y. Vergely C (2014) Diabetes, oxidative stress and therapeutic strategies. Biochim Biophys Acta (BBA)-Gen Subj. 1840;9:2709–29.
Singh U, Devaraj S. Vitamin E: inflammation and atherosclerosis. Vitam Horm. 2007;76:519–49.
Jiang Q, Yin X, Lill MA, et al. Long-chain carboxychromanols, metabolites of vitamin E, are potent inhibitors of cyclooxygenases. Proc Natl Acad Sci. 2008;105(51):20464–9.
Jimi E, Nakamura I, Ikebe T, et al. Activation of NF-κB is involved in the survival of osteoclasts promoted by interleukin-1. J Biol Chem. 1998;273(15):8799–805.
Simons K, Toomre D. Lipid rafts and signal transduction. Nat Rev Mol Cell Biol. 2000;1(1):31–9.
Stillwell W, Wassall SR. Docosahexaenoic acid: membrane properties of a unique fatty acid. Chem Phys Lipid. 2003;126(1):1–27.
Raphael W, Sordillo LM. Dietary polyunsaturated fatty acids and inflammation: the role of phospholipid biosynthesis. Int J Mol Sci. 2013;14(10):21167–88.
Poulsen RC, Gotlinger KH, Serhan CN, et al. Identification of inflammatory and proresolving lipid mediators in bone marrow and their lipidomic profiles with ovariectomy and omega-3 intake. Am J Hematol. 2008;83(6):437–45.
Berg AH, Scherer PE. Adipose tissue, inflammation, and cardiovascular disease. Circ Res. 2005;96(9):939–49.
Karimi E, Yarizadeh H, Setayesh L, et al. High carbohydrate intakes may predict more inflammatory status than high fat intakes in pre-menopause women with overweight or obesity: a cross-sectional study. BMC Res Notes. 2021;14:1–6.
Noh H-J, Kim H-C, Lee S-S, et al. The inhibitory effect of siRNAs on the high glucose-induced overexpression of TGF-β1 in mesangial cells. J Korean Med Sci. 2006;21(3):430–5.
Acknowledgements
The authors extend their sincere thanks to all participants and Minimally Invasive Surgery Research Center, Iran University of Medical Sciences, Tehran, Iran.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The present project was approved by the ethics committee of the Tehran University of Medical Sciences with the ID number IR.TUMS.MEDICINE.REC.1400.011.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key points
1. Higher dietary intakes of zinc, copper, and MUFA were associated with higher antioxidant defense.
2. Lower intakes of cholesterol, SFA, and carbohydrate intakes were associated with higher antioxidant/inflammation ratio level.
3. Higher dietary vitamin E and PUFA intakes were associated with lower level of inflammatory factor.
4. Weight reduction and dietary management after bariatric surgery may impact oxidative stress/inflammation levels.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hatami, M., Haghighat, N., Sohrabi, Z. et al. Association Between Dietary Intake After Roux-en-Y Gastric Bypass Surgery and Antioxidant/inflammatory Status: A 6-Month Pilot Prospective Cohort Study. OBES SURG 34, 2499–2507 (2024). https://doi.org/10.1007/s11695-024-07293-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-024-07293-3