Abstract
Purpose
Laparoscopy is advised under the lowest possible intra-peritoneal pressure. The aim of this study is to analyze the safety/feasibility of low pneumoperitoneum pressure (LPP) during laparoscopic sleeve gastrectomy (LSG).
Materials and Methods
All primary LSGs who completed a 3-month follow-up were included. Re-do operations and LSGs performed with concomitant procedures were excluded. All LSGs were performed by the senior author. Upon trocar insertions, pressure was set to 10 mmHg, and the procedure was started. The pressure was increased step-wise, according to the senior author’s assessment of the quality of exposure. Doing so, three pressure groups were formed: groups 1 (10 mmHg), 2 (11–13 mmHg), and 3 (14 mmHg). All data was retrieved from our database. Statistical analysis was performed using one-way ANOVA/Tukey’s HSD test/Chi-square test. P values < 0.05 were regarded as significant.
Results
Between February 2018 and October 2022, 708 consecutive/primary LSGs were studied. No mortality/conversion/thromboembolic event was observed. Groups 1, 2, and 3 comprised 376 (53.1%), 243 (34.3%), and 89 (12.6%) patients, respectively. Demographics, initial weight, duration of surgery, history for abdominoplasty, drain output, length of stay, and %total weight loss were evenly distributed among groups. Among 16 bleeding episodes, 14 occurred in the LPP group (p = 0.019). Including the only leak and stenosis, 8/9 of Clavien-Dindo 3b + 4 complications were observed in the LPP group (p = 0.092).
Conclusions
LSG with LPP is feasible in about half of the patients. However, almost all potentially life-threatening complications occurred in the LPP group where a significantly higher rate of bleeding was observed. Our findings suggest caution for routinely using LPP during LSG.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Laparoscopic sleeve gastrectomy (LSG) mandates pneumoperitoneum. Pneumoperitoneum has adverse effects on cardiovascular/pulmonary/hepatic/renal function [1,2,3], portal/femoral venous flow [3, 4], and postoperative pain [5]. These can be more consequential in morbidly obese patients. Hypothetically, provided that there is no increase in complications, it would be ideal if LSG can be performed under low pneumoperitoneum pressure (LPP) without an increase in the operating time and any loss in the bariatric benefit. Interestingly, there are only anecdotal reports on the use of LPP during bariatric procedures.
The primary aim of this study was to evaluate the safety and feasibility of LPP by utilizing a step-wise pressure increase method during primary LSGs. To our knowledge, this is the first study addressing the safety/feasibility of LPP during LSG.
Materials and Methods
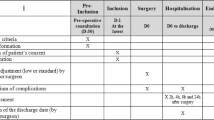
The study was approved by the institutional ethics committee, and written informed consent was obtained from all participants for both surgery and for the use of their data anonymously. This is a retrospective, observational study which followed the STROBE guidelines.
Inclusion and Exclusion Criteria
Following the introduction of our LPP protocol, all consecutive primary LSGs who completed a 3-month follow-up were studied. Secondary LSGs done with re-do bariatric intent (re-sleeves, patients having prior or concurrent lap-bands); patients having a prior anti-reflux operation; patients in whom a fundoplication/cholecystectomy were combined with the LSG and cases where giant para-esophageal hernias (PEH) were repaired concomitantly were excluded.
Preoperative Workout/Surgical Technique
Our protocols on preoperative workout, surgical technique, and virus-related changes during the COVID-19 pandemic were the same for all body mass indexes (BMI, kg/m2) and have been reported [6,7,8]. For the prevention of venous thromboembolism (VTE), all patients received low molecular weight heparin (LMWH) by pre-operative subcutaneous injection according to BMI (BMI > 50 received 60 mg, BMI < 50 received 40 mg of enoxaparin sodium, repeated every 24 h, for 10 days) (Clexane, pre-filled syringe, Sanofi, Türkiye). Patients who were already on oral or novel anti-coagulants were managed by bridging with LMWH and weaning off other anti-coagulation. Pneumatic stocking usage during surgery/hospitalization and early mobilization were routine. In patients with a VTE history, hypercoagulability, and with any condition that may prolong immobility, LMWH use was extended individually.
Neuromuscular blockage was achieved by rocuronium bromide (Muscobloc, Polifarma İlaç San ve Tic A.Ş, Ergene, Tekirdağ, Türkiye) 0.5 mg/kg iv, which was repeated every 20–25 min (0.2 mg/kg) during surgery and reversed by 150–250 mg of Sugammedex (Bridion, Merck Sharp Dohme İlaçları Ltd Şti, Levent, İstanbul, Türkiye) at the end. This was at the anesthesiologist’s discretion. No kinemyography was used to titrate the rocuronium dose by Train of Four (TOF) analysis.
All LSGs were performed by the senior author (M.A.Y.) or partly by the surgical staff under his direct supervision using a 5-trocar technique. A 6th trocar was inserted if deemed necessary for exposure at the surgeon’s discretion. LSGs were done routinely over a 42F blunt-tipped flexible solid bougie starting a few centimeters away from the pylorus. All staple lines were reinforced with continuous full-thickness suturing utilizing barbed suture (V-Loc 180; Medtronic, Minneapolis, MN, USA) as reported [7]. The leak test was used selectively. All patients were drained with a 7-mm Jackson Pratt drain, which was removed on the third postoperative day after the total output was recorded.
Postoperative Protocols/Definitions
The first postoperative day upper GI series was routine. All patients were discharged on the 3rd postoperative day unless there was a complication.
Postoperative fever was measured from the ear digitally with 2 hourly intervals on the day of surgery and with 4 hourly intervals during the rest of the hospitalization. In any patient with a fever ≥ 37.3 °C, chest x-ray, white blood cell count, c-reactive protein, and urine analysis were routine.
Leak was defined as the presence of extra-gastric contrast material in tomography. Bleeding was defined as hemorrhage requiring surgery or transfusion. High drain output consistent with a hemoglobin drop managed without transfusion/surgery was also recorded as bleeding. Stenosis was defined as acute (i.e., inability to start oral liquids, nausea, vomiting) or chronic complaints (i.e., intolerance to solids, frequent vomiting, increased reflux complaints, low weight, malnutrition) in the presence of findings at contrast swallow studies and gastroscopy.
Weight loss data is presented as percent total weight loss (%TWL). Patients were followed up at 3, 6, and 12 months after surgery and yearly thereafter. Patients who were unable to attend follow-up at 1st year were reached by phone to record their weight and stenosis-related symptoms. Data on demographics, previous history for abdominoplasty, the need for the 6th trocar, duration of surgery (minutes), length of stay (days), total drain output (milliliters), intra-operative problems, blood product use, early/late complications, and outcome/follow-up parameters were retrieved from our prospectively updated database.
LPP Protocol
During all LSGs, an optical trocar was used as the 1st trocar from the left upper quadrant to initiate pneumoperitoneum. Upon 1st trocar insertion, the pressure was set to 14 mmHg for the insertion of all the other trocars for a couple of minutes. Then, the pneumoperitoneum pressure was decreased to 10 mmHg, and the dissection was started. All LSGs were carried out under 10 mmHg pneumoperitoneum unless there was an exposure problem necessitating higher pressures. In such cases, the pressure was gradually increased to provide enough exposure at the senior surgeon’s discretion. Doing so, we had 3 distinct groups: LSGs performed with 10 mmHg (group 1), with 11–13 mmHg (group 2), and with 14 mmHg (group 3).
Statistics
Using SPSS software, version 23 (IBM Corp., Armonk, NY, USA), differences among groups were evaluated by one-way ANOVA analysis, and multiple comparisons between the groups were performed with Tukey’s HSD test. The Chi-square test was used for categorical data. P values < 0.05 were regarded as significant.
Results
Between February 2018 and October 2022, 755 consecutive LSGs were performed. Excluding 47 patients (secondary sleeves with re-do bariatric intent (n: 8), concomitant cholecystectomy (n: 26)/fundoplication (n: 2)/PEH repair (n: 8), prior anti-reflux operation (n: 3)), LPP was attempted in 708 consecutive-primary LSGs. The distribution of patients in 3 pressure groups according to BMI is shown in Table 1.
Demographics, duration of surgery, previous abdominoplasty history, need for a 6th trocar, total drain output, postoperative length of stay, and %TWL at 1st year in 3 groups are shown in Table 2. Among 559 patients who completed 1-year follow-up, weight loss data was missing in 63 (11.3%). Therefore, the %TWL at 1 year was calculated in 496 patients. The number of patients with missing data when calculating the %TWL was 34 (9%) in group 1, 23 (8.6%) in group 2, and 6 (6.7%) in group 3 and were similar.
There was no mortality or conversion to open surgery. No clinically evident VTE including mesenteric venous thrombosis was observed. Table 3 summarizes the complications in all groups. The only leak was observed in a patient in the LPP group and managed by stenting without sequela. It occurred due to a stapling error coupled with problematic stitching and was due to technical reasons as reported [9]. The only clinically evident stenosis also occurred in another patient in the LPP group and was managed by pneumatic balloon dilatation 3 months following the LSG without further sequela. Among 16 bleedings, all were intraabdominal except 1. One intra-luminal bleeding was managed by re-laparoscopic stitching under gastroscopic guidance with a novel approach as recently reported [10]. Fourteen of 16 bleedings occurred in the LPP group, and this was significantly more common (p = 0.019, Table 3). Major complications, leak (n: 1), stenosis (n: 1), and bleeding requiring surgery (n: 7), when evaluated separately, were evenly distributed among the groups, although 8 out of 9 occurred in group 1. Therefore, we also compared the cumulative risk of these major complications between the groups according to the Clavien-Dindo classification [11]. The risk for grade 3b + 4 complications in group 1 was 8/376; in group 2 was: 1/243; and in group 3 was 0/89. These differences were not statistically significant (p = 0.092). The sole minor complication that was significantly more common in group 2 was atelectasis, but this had no clinical consequence in any of the patients (Table 3).
Discussion
In an effort to decrease the potential ill effects of pneumoperitoneum and increase the benefit in pain reduction, international guidelines [12] advised laparoscopy with the lowest possible intra-peritoneal pressure that still provides sufficient exposure.
For achieving LPP, the step-wise pressure increase is an already described option during laparoscopic cholecystectomy [13], colectomy [14], and gastric bypass [15] with deep neuromuscular blockage under continuous kinemyographic monitoring of TOF. Utilizing the step-wise pressure increase guided by the quality of the surgical field, our experience in 708 consecutive LSGs showed that LPP is feasible in 53% of the patients without an increase in the operating time. The bariatric benefit remained uncompromised (Table 2). This step-wise pressure increase was also used during laparoscopic cholecystectomy [13] and Roux-en-Y gastric bypass [15] with 70% and 60% feasibility rates, respectively. It is noteworthy that differing from these studies, we did not use monitoring to maintain deep neuromuscular blockage, and this may be a reason of lower feasibility. Additionally, lower distensibility of the abdominal wall in obese patients may be another reason for lower feasibility compared with the 70% rate in the laparoscopic cholecystectomy article [13]. Importantly, a significant increase in bleeding episodes was observed in the LPP group. It is also noteworthy that 8/9 of potentially life-threatening (Clavien-Dindo 3b + 4) complications such as leak, stenosis, and bleeding requiring surgery were observed in the LPP group. The finding that atelectasis was more common in group 2 compared with groups 1 and 3 seemed a trivial issue clinically. Since all patients having fever reaching 37.3 °C had a chest x-ray, we were able to identify high numbers of atelectasis which all resolved with incentive spirometer usage.
Our findings are in accordance with the recently reported systematic review and meta-analysis of 44 randomized trials which focused on the clinical consequences of low vs standard pneumoperitoneum pressures during laparoscopic cholecystectomy [5]. With the exception of a debatable decrease in pain scores, most previous studies on laparoscopic cholecystectomy failed to show a measurable change in any clinical outcome parameter. A couple of studies on laparoscopic colorectal surgery reported improved recovery and early discharge by the use of LPP [14, 16]. It must be noted that the reduction in pain scores/pain medication usage decrease with low pressure is controversial. In a recent systematic review assessing pain after low vs standard pneumoperitoneum pressure during laparoscopic cholecystectomy, among 21 studies evaluated, there was a high risk of bias and low/very low quality of evidence in 20 of them [17]. In another systematic review including 42 articles on LPP, the authors, finding only moderate quality evidence regarding lower pain scores, concluded that any benefit is arguable because of weak evidence [1]. Not surprisingly, when surgeons are blinded to pneumoperitoneum pressure, no benefit in pain decrease could be shown in 2 recent prospective-randomized-double blind trials [13, 18]. In our study, since postoperative pain was not evaluated by a scoring system, the impact of LPP on pain is not possible to assess. This is a limitation of our study.
Some studies showed decreased lung compliance and volume/cardiac output/hepatic and renal blood flow and increased airway pressure/arterial partial pressure of CO2/peripheral vascular resistance during pneumoperitoneum which all can be managed without sequelae [1,2,3,4, 19]. It has also been shown that increased intraabdominal pressure and reverse Trendelenburg position during laparoscopy reduce not only portal but also femoral venous flow [1, 4]. Possibly due to our aggressive VTE prophylaxis protocol utilizing sequential compression stockings throughout the hospitalization and use of LMWH for 10 days, we have never experienced even a single case of clinically evident VTE including mesenteric vein thrombosis. Therefore, any impact of LPP on VTE could not be shown in this study.
Not surprisingly, the vast majority of the previous reports on low vs standard pneumoperitoneum were on laparoscopic cholecystectomy, and to our knowledge, only 2 studies [15, 20] were reported comparing low vs standard pressure pneumoperitoneum outcomes after bariatric operations. Recently, Leeman et al. [15] failed to show any clinical benefit of LPP in 29 patients undergoing laparoscopic Roux-en-Y gastric bypass. No advantage in pain was observed, and surgery took longer when LPP was used. The other article reported the use of LPP during LSG in only 20 patients and reported no advantage on hepatic/renal function compared to standard pressure [20]. This study was not a safety/feasibility analysis, and the step-wise approach was not used. Our study is the first to address the safety/feasibility of LPP during LSG in a large cohort of patients.
One of the weaknesses of our study is that we might have underdiagnosed some VTEs since no routine imaging was done. This would have been difficult to justify in asymptomatic patients. Similarly, our stenosis rate reflects a minimum because of patients lost to follow-up. A few stenoses might have remained undiagnosed. However, our report describes prospectively recorded complications in a large consecutive series of LSGs without exclusions that were performed by an experienced surgeon and followed up by the same team, under a protocol.
Conclusions
LPP, although technically feasible in about half of the patients undergoing LSG, is associated with significantly higher bleeding rates and slightly increased major complications. Given the absence of improvement in all parameters studied, depending on a possible but arguable reduction in pain, it is not possible to recommend LPP routinely for LSG candidates.
Data Availability
The data set of this article can be found in synapse.org at: https://doi.org/10.7303/syn51169055.
References
Özdemir-van Brunschot DMD, van Laarhoven KCJHM, Scheffer GJ, et al. What is the evidence for the use of low-pressure pneumoperitoneum? A systematic review. Surg Endosc. 2016;30:2049–65.
El-Dawlatly AA, Al-Dohayan A, Abdel-Meguid ME, et al. The effects of pneumoperitoneum on respiratory mechanics during general anesthesia for bariatric surgery. Obes Surg. 2004;14:212–5.
Nguyen NT, Anderson JT, Budd M, et al. Effects of pneumoperitoneum on intraoperative pulmonary mechanic and gas exchange during laparoscopic gastric bypass. Surg Endosc. 2004;18:64–71.
Nguyen NT, Wolfe BM. The physiological effects of pneumoperitoneum in the morbidly obese. Ann Surg. 2005;241:219–26.
Ortenzi M, Montori G, Sartori A, et al. Low-pressure versus standard-pressure pneumoperitoneum in laparoscopic cholecystectomy: a systematic review and meta-analysis of randomized controlled trials. Surg Endosc. 2022;36:7092–113.
Şen O, Çalıkoğlu İ, Özgen G, et al. Sleeve gastrectomy in class 1 obesity: assessment of operative outcomes. Surg Obes Relat Dis. 2021;17:170–6.
Özgen G, Çalıkoğlu İ, Acunaş B, et al. Staple-line enforcement using barbed sutures in 1008 sleeve gastrectomies. Langenbecks Arch Surg. 2021;406:1683–90.
Yerdel MA, Özgen G. Eighty-seven consecutive sleeve gastrectomies between the two peaks of the Covid-19 pandemic. An opening phase experience. Obes Surg. 2021;31:3026–30.
Özgen G, Yerdel MA. Leak after sleeve gastrectomy: a videoscopic documentation on occurrence, diagnosis, and treatment. Videoscopy. 2022;32. https://doi.org/10.1089/vor.2021.0045.
Çalıkoğlu İ, Hamzaoğlu H, Yerdel MA. Combined use of endoscopy to guide laparoscopic management of intraluminal bleeding from the staple-line after sleeve gastrectomy: a video case report. Surg Obes Relat Dis. 2020;16:1156–7.
Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250:187–96.
Neudecker J, Sauerland S, Neugebauer E, et al. The European Association for Endoscopic Surgery clinical practice guideline on the pneumoperitoneum for laparoscopic surgery. Surg Endosc. 2002;16:1121–43.
Gin E, Lowen D, Tacey M, et al. Reduced laparoscopic intra-abdominal pressure during laparoscopic cholecystectomy and its effect on post-operative pain: a double-blinded randomized control trial. J Gastrointest Surg. 2021;25:2806–13.
Diaz-Canbronero O, Mazzinari G, Flor Lorente B, et al. Effect of individualized versus standard pneumoperitoneum pressure strategy on postoperative recovery: a randomized clinical trial in laparoscopic colorectal surgery. Br J Surg. 2020;107:1605–14.
Leeman M, Ulas Biter L, Apers JA, et al. Low-pressure pneumoperitoneum with deep neuromuscular blockage in metabolic surgery to reduce postoperative pain: a randomized pilot trial. Surg Endosc. 2020;35:2838–45.
Celarier S, Monziols S, Célérier B, et al. Low-pressure versus standard pressure laparoscopic colorectal surgery (PAROS trial): a phase III randomized controlled trial. Br J Surg. 2021;108:998–1005.
Gurusamy KS. Low pressure versus standard pressure pneumoperitoneum in laparoscopic cholecystectomy. Cochrane Database Syst Rev. 2014;18:CD006930.
Moro ET, Pinto PCC, Neto AJMM, et al. Quality of recovery in patients under low- or standard-pressure pneumoperitoneum. A randomized controlled trial. Acta Anesthesiol Scand. 2021;65:1240–7.
Köksoy C, Kuzu MA, Kurt I, et al. Haemodynamic effects of pneumoperitoneum during laparoscopic cholecystectomy: a prospective comparative study using bioempedance cardiography. Br J Surg. 1995;82:972–4.
Akkurt G, Birben B, Akçay FK, et al. Effects of different intraabdominal pressures on internal jugular vein, liver and kidney functions in obese patients undergoing laparoscopic sleeve gastrectomy. Acta Chir Bel. 2021;15:1–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
All procedures performed were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key points
• Safety/feasibility of low abdominal pressure during sleeve gastrectomy is unknown.
• Sleeve gastrectomy under low abdominal pressure was feasible in 53% of the patients.
• In the low-pressure group, bleeding occurred at a significantly higher rate.
• Our findings suggest caution for using low pressure during sleeve gastrectomy.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Özgen, G., Toydemir, T. & Yerdel, M.A. Low-Pressure Pneumoperitoneum During Laparoscopic Sleeve Gastrectomy: a Safety and Feasibility Analysis. OBES SURG 33, 1984–1988 (2023). https://doi.org/10.1007/s11695-023-06625-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-023-06625-z