Abstract
Introduction
Despite increases in obesity prevalence, awareness of obesity as a disease requiring active treatment remains lacking in Korea. We investigated differences in medical problems and expenditures and mortality across obesity categories using 12-year data from the National Health Insurance Service.
Materials and Methods
Individuals aged 40–79 years who underwent medical examinations during 2003–2004 (n = 415,201) were divided based on Asian body mass index (kg/m2) criteria: normal weight (18.5 to < 23.0, 36.4%), overweight (23.0 to < 25.0, 28.3%), obesity (25.0 to < 30.0, 32.5%), and severe obesity (≥ 30.0, 2.8%). Medical problems and expenditures were fitted to linear mixed models. Mortality was analyzed via Cox proportional-hazards model.
Results
More severe obesity was associated with a higher rate of medical problems, relative to normal weight: coefficient = 0.31 (95% confidence interval [CI], 0.30–0.32) for overweight, 0.61 (0.60–0.61) for obesity, and 1.07 (1.04–1.09) for severe obesity. A similar association was observed for medical expenditure: coefficient = 8.85 (95%CI, 6.80–10.89) for overweight, 20.04 (18.07–22.01) for obesity, and 48.76 (43.66–53.86) for severe obesity. Relative to overweight participants, those with normal weight and severe obesity exhibited a higher mortality risk (hazard ratio [HR] 1.21 [95%CI, 1.18–1.25] for normal; 1.27 [1.19–1.36] for severe obesity). In age-specific analyses, mortality risk was the highest for participants with severe obesity, aged < 60 years (HR, 1.58 [95%CI, 1.41–1.77]).
Conclusion
Disease burden including medical problems and expenditure, and mortality in middle-aged adults, increased proportionally to the degrees of obesity. Health policies and medical systems aimed at reducing the burden of obesity may help reduce the burden of disease on society.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
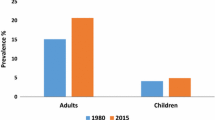
The rapid growth in the prevalence of overweight and obese populations is considered a global pandemic [1, 2]. According to recent data from the Global Burden of Disease study, a high body mass index (BMI) is the risk exposure factor with the largest growth over the past 20 years [3,4,5]. Furthermore, obesity is an independent risk factor for many chronic diseases, such as type-2 diabetes, cardiovascular disease, and cancer [6,7,8,9]. In addition to being a leading risk for mortality worldwide [10, 11], obesity has an important impact on physical and mental health, health-related quality of life, and on economic burden (indirect and direct costs) [12, 13].
Several studies in Western countries have documented the prevalence of obesity and its treatment outcomes [14, 15]. Compared with other countries, the Republic of Korea has relatively lower levels of overweight and obese individuals [16]. However, in recent years, the prevalence of obesity has increased in Korea [17,18,19], possibly due to the rapid westernization of dietary habits and lifestyles [20, 21]. Although the prevalence of obesity in Korea is steadily increasing, a broad awareness of obesity as a disease requiring active treatment and appropriate medical policy remains lacking.
In Korea, previous studies using large real-world databases have revealed the medical and social problems caused by obesity [22, 23]. However, because these studies were typically based on data obtained prior to 2000, the latest Korean trends on obesity were not reflected. Epidemiological studies investigating the contemporary trends in this disease are necessary for accurate recognition of its burden and to inform appropriate medical policies for proactive management and treatment.
The development of a more accurate and reliable estimation of the medical burden of obesity will serve as a basis for developing and prioritizing appropriate health interventions in order to reduce the obesity-related health burden. Here, we investigated and described the differences in medical problems and costs, and mortality across the obesity categories in Korea using the National Health Insurance Service (NHIS) database (DB).
Methods
Study Design and Data Sources
This longitudinal retrospective cohort study used data from the Korean NHIS-National Health Screening (NHIS-HEALS) cohort DB. The Korean NHIS is a mandatory social insurance system, which covers the medical expenses of 97% of the South Korean population [1]. Although NHIS information is representative of medical trends and practices in Korea, access and use by investigators are restricted due to the large volume of data and issues related to the protection of identifiable personal information. Thus, the NHIS has constructed the Sample Research DB, containing standardized data in a sharable form, by extracting five specific cohorts from the large sample: the National Sample cohort [24], National Health Screening (HEALS) cohort [25], Senior cohort [26], Working women cohort, and Birth cohort [27] (https://nhiss.nhis.or.kr). We here used the Korean NHIS-HEALS.
Among the qualified NHIS subscribers in 2002, participants aged 40–79 years who underwent health screening during 2002–2003 and who were followed up biennially through to 2015 were identified for potential study inclusion. From this population, 10% (n = 514,866) of randomly selected participants were included in the NHIS-HEALS cohort [25]. The NHIS-HEALS DB represents the entire Korean population and consists of four datasets: qualification, treatment, medical check-up, and clinic.
Participant Categorization
To analyze the 12-year longitudinal trajectories of the biannual health screening results of the NHIS-HEALS cohort (n = 514,866), only participants who received a health screening record between January 1, 2003, and December 31, 2004 (index date) were included. Participants with a normal weight or higher according to the Asian BMI criteria (BMI ≥ 18.5 kg/m2) at their index-date screening visit were included in this study (Supplementary Fig. 1). Participants were excluded if they had (1) no health screening record at the index date (n = 87,375), (2) no BMI information (n = 385), BMI < 18.5 kg/m2 (n = 11,721) at the time of the index visit, or (3) a medical history within 90 days prior to the index screening visit that may have affected BMI (cancer and gastrointestinal disorder [n = 184]; Supplementary Fig. 1). After applying these inclusion and exclusion criteria, 415,201 participants were enrolled.
The primary endpoint of our study was BMI measured at five time-points every 2 years after the index date. Therefore, missing BMI values were imputed by the last-observation-carried-forward for subjects who did not undergo a health screening test at each time-point (within ± 1-year windows). Approximately a quarter of the BMI levels at every time-point after the index date were imputed.
While the criteria for being underweight are the same in both Asians and Westerners, the definition of obesity according to BMI differs slightly between these populations (Supplementary Fig. 1). The degree of obesity was classified into four groups according to the Asian BMI criteria: normal weight (18.5 to < 23.0 kg/m2), overweight (23.0 to < 25.0 kg/m2), obese (25.0 to < 30.0 kg/m2), and severely obese (≥ 30.0 kg/m2) [28]. Each qualifying participant was categorized according to their BMI at the index screening date.
Outcomes
Participant Characteristics
Characteristics, socioeconomic factors, participant sex, age, BMI, socioeconomic status, smoking, drinking, and physical activity status in each BMI group were investigated and described using data from the qualification and medical check-up datasets.
Medical Problems
Twenty-five diseases that may be clinically associated with obesity were selected according to the codes in the treatment database: metabolic syndrome (type 2 diabetes, hypertension, and dyslipidemia), cardiovascular disease (myocardial infarction, cardiomyopathy, angina pectoris, ischemic stroke, and congestive heart failure), cancer (breast, colorectal, endometrial, pancreatic, kidney, prostate, urinary bladder, and gallbladder cancers), and others (depression, osteoarthritis, hypoventilation, sleep apnea, asthma, gastroesophageal reflux disease, non-alcoholic fatty liver, polycystic ovary syndrome, and pseudotumor cerebri). The number of comorbidities per patient at the index date and biannually through 12 years of follow-up was assessed and described.
Medical Expenditures
Medical expenditures, including the payer’s amount and the patient’s out-of-pocket cost for all healthcare activities, were identified within the treatment dataset. The sum of per-participant medical expenses was analyzed for each 2-year period from the index date through the 12-year study trajectory. All the healthcare service costs reflected the cumulative per-patient costs for each 2-year period, averaged for each obesity category.
Mortality
The overall survival for each participant was analyzed using the qualification dataset. For subgroup analysis, the participants were divided into two age categories: < 60 and ≥ 60 years. In the Cox proportional hazards regression analysis, we set overweight criteria as the reference, based on the obesity paradox theory [29, 30].
Statistical Analysis
Demographic, clinical, and pathological characteristics were described using chi-square tests for categorical variables, and analysis of variance for continuous variables. Changes in BMI over time were estimated using generalized linear mixed models with a gamma distribution and a logarithmic transformation link function. Linear mixed models were used to analyze the differences in number of comorbidities and total medical costs over time for each group. The grouping model considered only the passage of time, and repeated measure analysis of variance was used to test for differences between groups. The full linear mixed model included adjustments for age, sex, income level, smoking status, physical activity, and BMI to estimate the expected values and 95% CI. The Kaplan–Meier method was used for univariate analysis of overall survival according to the BMI level. The log-rank test was used to calculate the statistical significance of between-group differences. For multivariate analysis, a time-varying Cox proportional hazards regression model was used for factors that showed statistical significance in the univariate analysis. Hazard ratios (HRs) and 95% confidence intervals (CIs) were calculated for mortality. All the statistical tests were set at a two-sided significance level of 0.05. The Statistical Package for SAS (version 9.4; SAS Institute Inc., Seoul, Korea) and R statistical software (version 3.3.3; R Foundation for Statistical Computing, Vienna, Austria) were used to perform the statistical analyses.
Results
The inclusion criteria for this study was met by 415,201 participants, with the proportions, counts, and mean (SD) BMI within each category at index date as follows: 36.43%, n = 151,278, BMI 21.34 ± 1.16 kg/m2 for normal weight; 28.3%, n = 117,516, BMI 23.99 ± 0.57 kg/m2 for overweight; 32.52%, n = 135,009, BMI 26.70 ± 1.26 kg/m2 for obesity; and 2.75%, n = 11,398, BMI 31.81 ± 2.54 kg/m2 for severe obesity. During the 12-year follow-up, there was no significant changes in the BMI in any of the four groups (all beta = 0.00, [95%CI, 0.00–0.00]) (Supplementary Table 1).
Characteristics and Socioeconomic Factors
The demographic, lifestyle, and behavioral characteristics of each group are shown in Table 1. Severe obesity was significantly associated with older age (54.26 ± 9.13 years), female sex (59.23%), a lower income level (25.21% with income level 0–3), a higher portion of never smokers (72.57%), non-drinkers (60.85%), and non-exercisers (55.27%) (all p < 0.001). In contrast, the overweight group was younger (53.53 ± 9.24 years), more often male (57.40%), with a higher income level (47.93% with income level 8–10), and relatively lower portions of never smokers (63.64%), non-drinkers (52.61%), and non-exercisers (47.68%) (all p < 0.001).
Medical Problems
As shown in Table 2, the higher BMI group had a higher number of comorbidities at the index date (normal, 1.00 ± 1.32; overweight, 1.19 ± 1.44; obesity, 1.43 ± 1.55; and severe obesity, 1.88 ± 1.71). In general, the number of comorbidities increased during the follow-up period as the study participants aged (12 years after the index date: normal; 2.24 ± 1.89; overweight; 2.60 ± 1.96; obesity; 2.98 ± 2.02; and severe obesity; 3.60 ± 2.04). Increases in comorbidity counts over time were also higher for the higher BMI groups (within the 12-year follow-up period: beta = 0.11 for normal, 0.13 for overweight, 0.14 for obesity, and 0.15 for severe obesity [all p < 0.011]). In the multivariate analysis, a higher BMI was associated with an increased number of comorbidities relative to normal weight: coefficient = 0.31 [95% confidence interval, 0.30–0.32] for overweight, 0.61[0.60–0.61] for obesity, 1.07 [1.04–1.09] for severe obesity (Table 3).
Medical Expenditures
As shown in Table 4, BMI was associated with medical expenditure. The highest BMI group spent more on healthcare service costs (all expressed in 1,000,000 Korean Won) by the index date (normal; 0.69 ± 1.67; overweight; 0.68 ± 1.52; obesity; 0.73 ± 1.50; and severe obesity; 0.84 ± 1.68). As the participants aged, the medical costs also increased (12 years after index date: normal; 2.52 ± 6.43; overweight; 2.66 ± 6.70; obesity; 2.90 ± 6.79; and severe obesity; 3.45 ± 7.69). The magnitude increase in healthcare service costs over time was higher in the higher BMI categories: beta = 0.17, normal, 0.18 for overweight, 0.20 for obesity, and 0.25 for severe obesity (all p < 0.001). In multivariate analysis, a higher BMI category was associated with increased total healthcare service costs relative to normal weight (all expressed in 10,000 Korean Won): coefficient = 8.85 [95%CI, 6.80–10.89] for overweight, 20.04 [18.07–22.01] for obesity, and 48.76 [43.66–53.86] for severe obesity (Table 5).
Mortality
Across all participants, the 12-year survival was higher in the obesity and overweight categories than in the severe obesity and normal weight categories: obesity (93%), overweight (93%), severe obesity (92%), and normal (90%) (p < 0.001) (Supplementary Table 2 and Fig. 2). In multivariate analysis, across all participants, normal weight, and severe obesity posed a higher mortality risk relative to overweight (adjusted HR, 1.21 [1.18–1.25] for normal; 1.27 [1.19–1.36] for severe obesity; Table 6). When subgroup analysis was performed by age group, the participants in the severe obesity group had the lowest survival rate among participants aged 40–59 years, and those in the normal weight group had the lowest survival rate in the 60 + year category (Supplementary Fig. 3 and Table 3). The Cox regression analysis showed that participants with severe obesity had the highest mortality risk among participants aged < 60 years (HR, 1.58 [95%CI, 1.41–1.77]), whereas those with normal weight had the highest mortality risk among participants aged ≥ 60 years (HR, 1.2 [95%CI, 1.16–1.24]; Table 6).
Discussion
Within the data variables provided by the NHIS-HEALS cohort, the characteristics and lifestyles of a representative cohort of South Koreans aged 40–79 years were investigated as a function of BMI categories. Medical problems and expenditures, and mortality were selected a priori to characterize the burden of obesity over a 12-year period. We showed that disease burden and medical expenditure increased proportionally to the obesity burden and that the highest mortality risk was associated with middle-aged participants with severe obesity.
The prevalence of obesity has been increasing worldwide, and it is a major risk factor for various chronic diseases [4]. Western countries consider obesity as a disease that requires active treatment, starting with changes in long-term lifestyle [15, 31, 32]. When this is not sufficient, medication may be added, and bariatric surgery is considered. However, this awareness is less common in Korea, possibly due to the lower prevalence of obesity [16, 33]. Recently, interest in active treatment of obesity has increased in Korea [17, 34], with bariatric surgery receiving insurance coverage [35]. Several previous studies with large data from public institutions have described the increasing prevalence of obesity in Korea, but considered varying time periods and institutions [18, 22, 23, 36]. Thus, our contemporary, national-level data can help to inform appropriate treatment, insurance policies, and insurance systems in Korea.
Compared with the normal, overweight, and obese groups, the severe obesity group had a significantly higher mean age, higher proportion of females, and lower socioeconomic activity (never smoker, non-drinker, and non-exerciser) (Table 1). Participants in the overweight group, but not those in the normal group, had outcomes that contrasted most with those in the severe obesity group. Contrary to expectations, participants who neither smoked nor drank alcohol had higher obesity levels than those who did. Prior studies demonstrated that, in general, the prevalence of obesity was low among drinkers and smokers, but high among “binge drinkers” and “heavy smokers” [37, 38]. Therefore, the smoking and drinking categories within the dataset available for this study may not have been sufficiently detailed to allow analysis of these interactions.
Using a linear mixed model, the effect of obesity on medical problems and expenditure was quantified from the index date through the 12-year follow-up period. As in prior studies, our results showed that the increased medical problems and expenditure rates correlated positively with the increase in time and BMI category. Song et al. used the NHIS-HEALS cohort to describe discrete characteristics at baseline and at the end of a 10-year follow-up [39], whereas our study considered time trends throughout the 12-year period. Since the NHIS data comprised 12 years of longitudinal data for each individual, the time factor is reflected in the analysis and demonstrated the degree of increase in the number of comorbidities and medical expenses in each group over time.
Since our study cohort comprised all health screening participants (including those with a low medical burden), a high 12-year survival rate of > 90% was observed. Nevertheless, a significant difference was observed in survival rates across the BMI categories (Supplementary Table 2 and Fig. 2). Contrary to our expectations, the overweight and obesity groups had the highest survival rates, at 93%, and the survival rate was higher in the severe obesity group (92%) than in the normal group (90%). These mortality results should be considered in the context of previous findings of U-shaped or J-shaped relationships between all-cause mortality and BMI [29, 30, 40, 41]. A previous study that investigated the association between BMI and overall and cause-specific mortality in a population-based cohort of 3.6 million adults in the UK showed a J-shaped association between BMI and all-cause mortality, with the lowest mortality seen at BMI 25 kg/m2, which is borderline between overweight and obesity in the Asian population [41]. Another study conducted in Korea using the NHIS-NSC cohort showed that participants with a BMI < 23 kg/m2 or ≥ 30 kg/m2 had higher risks of all-cause and cause-specific mortality than the reference group (BMI 23–24.9 kg/m2) [29]. Therefore, considering the obesity paradox, we set the overweight category as the reference group in the Cox regression analysis.
The mortality risk was higher in the normal and severe obesity groups than in the overweight and obesity groups. This may be due to definition of the Asian BMI classification in the early 2000s [42]. Although there are many ways to measure obesity, BMI is the most widely used method. BMI classifications are based on the risk of cardiovascular disease adopted by the World Health Organization (WHO) for white, Hispanic, and black individuals. According to the WHO classification, overweight is defined as a BMI of 25–29.9 kg/m2, whereas BMI ≥ 30 kg/m2 defines obesity [1]. However, Asians have slighter builds than Caucasians and therefore have less muscle mass and connective tissue [43]. Since applying Western cutoffs may underestimate risks in Asian populations, the WHO recommended using lower cutoffs for overweight and obesity classifications among Asians (overweight: BMI 23–24.9 kg/m2; obesity: BMI > 25 kg/m2) [28, 42]. However, using BMI alone to define obesity does not correctly reflect the extent of excess body fat, which is the main characteristic of obesity. It does not distinguish between excess fat, muscle, or bone mass, or indicate the distribution of fat in individuals. Different BMI components contribute differently to the health status of individuals and are further influenced by factors such as age, sex, and ethnicity. Additionally, the correlation between BMI and mortality is also influenced by cardiopulmonary fitness, which may be one of the factors responsible for the observation.
In subgroup analysis, severe obesity was associated with the highest mortality risk among participants aged < 60 years, while normal weight was associated with the highest mortality risk among participants aged > 60 years. Concordant with a previous study [23], we found that the association between BMI and mortality risk varied according to age, with little evidence of increased risk for obese subjects aged > 60 years. Consistent with our findings, previous studies have reported high BMI as a direct risk factor for mortality in middle age [44, 45]. Most associations between BMI and mortality attenuated with age, potentially because BMI is less well correlated with obesity in older individuals, and there is a high probability of undiagnosed diseases in the older group.
There are some limitations to consider when interpreting the result of this study. Since analysis were conducted on a large database, the possibility of selection bias may not be completely ruled out. Despite this, we did our best to extract as much pure data as possible. In this study, inclusion criteria were planned in a strict and detailed manner to reduce selection bias as much as possible, and the codes for specific diseases and medical costs included in the data were thoroughly examined before the study began. Another limitation is that NHIS-HEALS only provides overall survival data, without specifying the cause of death. Therefore, even though our results suggest that overall mortality is the highest in middle-aged, severely obese people, we cannot state that all deaths were obesity related. Lastly, this study was based on the national database, had a very large number of patients, and a sufficient study period, all of which strengthened the validity of our results. However, that is also why the results did not deviate much from our expectation, and why our results are relatively simple for such a complex study.
Conclusions
Medical problems and expenditures increased with an increase in the degree of obesity. Among middle-aged individuals, those with severe obesity had the highest mortality rate. This study may be a significant indicator that health promotion and treatment policies that aim to reduce the burden of severe obesity may help reduce the overall burden of disease in society. On the other hand, we have also found that individuals with normal weight show higher mortality rates after 60 years of age. Therefore, more studies should be carried out to identify the causes of mortality, and perhaps to redefine criteria for being overweight in the Asian population, or to assess whether higher health spending (medication) is causing this difference.
References
WHO. World Health Organization Obesity fact sheet. 2021. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Accessed 1 March 2022.
GBD 2015 Obesity Collaborators, Afshin A, Forouzanfar MH, et al. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377:13–27. https://doi.org/10.1056/NEJMoa1614362.
Ezzati M, Lopez AD, Rodgers A, et al. Selected major risk factors and global and regional burden of disease. Lancet. 2002;360:1347–60. https://doi.org/10.1016/S0140-6736(02)11403-6.
Ng M, Fleming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:766–81. https://doi.org/10.1016/S0140-6736(14)60460-8.
GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1223–49. https://doi.org/10.1016/S0140-6736(20)30752-2.
Keramat SA, Alam K, Rana RH, et al. Obesity and the risk of developing chronic diseases in middle-aged and older adults: findings from an Australian longitudinal population survey, 2009–2017. PLOS ONE. 2021;16 (November 11):e0260158. https://doi.org/10.1371/journal.pone.0260158.
Yoon KH, Lee JH, Kim JW, et al. Epidemic obesity and type 2 diabetes in Asia. Lancet. 2006;368:1681–8. https://doi.org/10.1016/S0140-6736(06)69703-1.
Kivimäki M, Kuosma E, Ferrie JE, et al. Overweight, obesity, and risk of cardiometabolic multimorbidity: pooled analysis of individual-level data for 120 813 adults from 16 cohort studies from the USA and Europe. Lancet Public Health. 2017;2:e277–85. https://doi.org/10.1016/S2468-2667(17)30074-9.
Arnold M, Jiang L, Stefanick ML, et al. Duration of adulthood overweight, obesity, and cancer risk in the Women’s Health Initiative: a longitudinal study from the United States. PLOS Med. 2016;13: e1002081. https://doi.org/10.1371/journal.pmed.1002081.
Flegal KM, Graubard BI, Williamson DF, et al. Excess deaths associated with underweight, overweight, and obesity. JAMA. 2005;293:1861–7. https://doi.org/10.1001/jama.293.15.1861.
Xu H, Cupples LA, Stokes A, et al. Association of obesity with mortality over 24 years of weight history: findings from the Framingham heart study. JAMA Netw Open. 2018;1: e184587. https://doi.org/10.1001/jamanetworkopen.2018.4587.
Katz DA, McHorney CA, Atkinson RL. Impact of obesity on health-related quality of life in patients with chronic illness. J Gen Intern Med. 2000;15:789–96. https://doi.org/10.1046/j.1525-1497.2000.90906.x.
Withrow D, Alter DA. The economic burden of obesity worldwide: a systematic review of the direct costs of obesity. Obes Rev. 2011;12:131–41. https://doi.org/10.1111/j.1467-789X.2009.00712.x.
Ogden CL, Carroll MD, Lawman HG, et al. Trends in obesity prevalence among children and adolescents in the United States, 1988–1994 through 2013–2014. JAMA. 2016;315:2292–9. https://doi.org/10.1001/jama.2016.6361.
Gloy VL, Briel M, Bhatt DL, et al. Bariatric surgery versus non-surgical treatment for obesity: a systematic review and meta-analysis of randomised controlled trials. BMJ. 2013;347: f5934. https://doi.org/10.1136/bmj.f5934.
Heo YS, Park JM, Kim YJ, et al. Bariatric surgery versus conventional therapy in obese Korea patients: a multicenter retrospective cohort study. J Korean Surg Soc. 2012;83:335–42. https://doi.org/10.4174/jkss.2012.83.6.335.
Park DJ, An SN, Park YS, et al. Bariatric surgery versus medical therapy in Korean obese patients: prospective multicenter nonrandomized controlled trial (KOBESS trial). Ann Surg Treat Res. 2021;101:197–205. https://doi.org/10.4174/astr.2021.101.4.197.
Kang HT, Shim JY, Lee HR. Trends in prevalence of overweight and obesity in Korean adults, 1998–2009: the Korean national health and nutrition examination survey. J Epidemiol. 2014;24:109–16. https://doi.org/10.2188/jea.JE20130017.
Yoon YS, Oh SW. Recent shift of body mass index distribution in Korea: a population-based Korea national health insurance database, 2002–2013. J Korean Med Sci. 2017;32:434–8. https://doi.org/10.3346/jkms.2017.32.3.434.
Seidell JC, Visscher TL, Hoogeveen RT. Westernization in daily dietary and lifestyle has progressed rapidly in Korea, the pattern of obesity is becoming similar to that of Westerners. Med Sci Sports Exerc. 1999;31(11):S597–601.
Lim S, Shin H, Song JH, et al. Increasing prevalence of metabolic syndrome in Korea: the Korean National Health and Nutrition Examination Survey for 1998–2007. Diabetes Care. 2011;34:1323–8. https://doi.org/10.2337/dc10-2109.
Oh SW, Shin SA, Yun YH, et al. Cut-off point of BMI and obesity-related comorbidities and mortality in middle-aged Koreans. Obes Res. 2004;12:2031–40. https://doi.org/10.1038/oby.2004.254.
Jee SH, Sull JW, Park J, et al. Body-mass index and mortality in Korean men and women. N Engl J Med. 2006;355:779–87. https://doi.org/10.1056/NEJMoa054017.
Lee J, Lee JS, Park SH, et al. Cohort profile: the National Health Insurance Service-national sample Cohort (NHIS-NSC), South Korea. Int J Epidemiol. 2017;46: e15. https://doi.org/10.1093/ije/dyv319.
Seong SC, Kim YY, Park SK, et al. Cohort profile: the National Health Insurance Service-National Health Screening Cohort (NHIS-HEALS) in Korea. BMJ Open. 2017;7: e016640. https://doi.org/10.1136/bmjopen-2017-016640.
Kim YI, Kim YY, Yoon JL, et al. Cohort profile: National Health Insurance Service-senior (NHIS-senior) cohort in Korea. BMJ Open. 2019;9: e024344. https://doi.org/10.1136/bmjopen-2018-024344.
Kim JH, Lee JE, Shim SM, et al. Cohort profile: National Investigation of Birth Cohort in Korea study 2008 (NICKs-2008). Clin Exp Pediatr. 2021;64:480–8. https://doi.org/10.3345/cep.2020.01284.
WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63. https://doi.org/10.1016/S0140-6736(03)15268-3.
Kim NH, Lee J, Kim TJ, et al. Body mass index and mortality in the general population and in subjects with chronic disease in Korea: a nationwide cohort study (2002–2010). PLoS ONE. 2015;10: e0139924. https://doi.org/10.1371/journal.pone.0139924.
Donini LM, Pinto A, Giusti AM, et al. Obesity or BMI paradox? Beneath the tip of the iceberg. Front Nutr. 2020;7:53. https://doi.org/10.3389/fnut.2020.00053.
Bolen SD, Clark JM, Richards TM, et al. Trends in and patterns of obesity reduction medication use in an insured cohort. Obesity (Silver Spring). 2010;18:206–9. https://doi.org/10.1038/oby.2009.175.
Welbourn R, Hollyman M, Kinsman R, et al. Bariatric surgery worldwide: baseline demographic description and one-year outcomes from the fourth IFSO global registry report 2018. Obes Surg. 2019;29:782–95. https://doi.org/10.1007/s11695-018-3593-1.
Kim TN. Barriers to obesity management: patient and physician factors. J Obes Metab Syndr. 2020;29:244–7. https://doi.org/10.7570/jomes20124.
Lim S, Oh B, Lee SH, et al. Perceptions, attitudes, behaviors, and barriers to effective obesity care in South Korea: results from the ACTION-IO study. J Obes Metab Syndr. 2020;29:133–42. https://doi.org/10.7570/jomes20013.
Kim BY, Kang SM, Kang JH, et al. Korean society for the study of obesity guidelines for the management of obesity in Korea. J Obes Metab Syndr. 2020;30(81):2021.
Kong JW, Park T, Lee DR, et al. Trajectories of body mass index and their associations with mortality among older adults in Korea: analysis of the Korean longitudinal study of aging. Ann Geriatr Med Res. 2020;24:195–203. https://doi.org/10.4235/agmr.20.0030.
Arif AA, Rohrer JE. Patterns of alcohol drinking and its association with obesity: data from the third national health and nutrition examination survey, 1988–1994. BMC Public Health. 2005;5:126. https://doi.org/10.1186/1471-2458-5-126.
Dare S, Mackay DF, Pell JP. Relationship between smoking and obesity: a cross-sectional study of 499,504 middle-aged adults in the UK general population. PLoS ONE. 2015;10: e0123579. https://doi.org/10.1371/journal.pone.0123579.
Song HJ, Hwang J, Pi S, et al. The impact of obesity and overweight on medical expenditures and disease incidence in Korea from 2002 to 2013. PLoS ONE. 2018;13: e0197057. https://doi.org/10.1371/journal.pone.0197057.
Aune D, Sen A, Prasad M, et al. BMI and all cause mortality: systematic review and non-linear dose-response meta-analysis of 230 cohort studies with 3.74 million deaths among 30.3 million participants. BMJ. 2016;353:i2156. https://doi.org/10.1136/bmj.i2156.
Bhaskaran K, dos-Santos-Silva I, Leon DA, et al. Association of BMI with overall and cause-specific mortality: a population-based cohort study of 3·6 million adults in the UK. Lancet Diabetes Endocrinol. 2018;6:944–53. https://doi.org/10.1016/S2213-8587(18)30288-2.
World Health Organization. International association for the study of obesity IOTF. The Asia-Pacific perspective: redefining obesity and its treatment; 55p. Sydney: Health Communications Australia. Published online.p. 44; 2000.
Deurenberg P, Deurenberg Yap MD, Wang J, et al. The impact of body build on the relationship between body mass index and percent body fat. Int J Obes Relat Metab Disord. 1999;23:537–42. https://doi.org/10.1038/sj.ijo.0800868.
Ng TP, Jin A, Chow KY, et al. Age-dependent relationships between body mass index and mortality: Singapore longitudinal ageing study. PLoS ONE. 2017;12: e0180818. https://doi.org/10.1371/journal.pone.0180818.
Winter JE, MacInnis RJ, Nowson CA. The influence of age the BMI and all-cause mortality association: a meta-analysis. J Nutr Health Aging. 2017;21:1254–8. https://doi.org/10.1007/s12603-016-0837-4.
Acknowledgements
We are deeply grateful to Health Economics & Market Access, Johnson & Johnson Medical Korea for research grant.
Funding
This study used the National Health Insurance Service (NHIS)-National Health Screening (HEALS) Cohort database (NHIS-2021–2-061) provided by the NHIS. This study was supported by a research grant from Health Economics & Market Access, Johnson & Johnson Medical Korea (grant number 0620202510).
Author information
Authors and Affiliations
Contributions
Ji-Hyeon Park: conceptualization, methodology, formal analysis, writing-original draft preparation, visualization, investigation, data curation, writing—reviewing and editing.
Do Joong Park: conceptualization, methodology, formal analysis, writing—reviewing and editing, supervision, project administration.
Hyesung Kim: investigation, data curation, resources, funding acquisition.
Hyejin Park: investigation, data curation, resources, funding acquisition.
Bora Lee: methodology, software, formal analysis, data curation, validation.
Hyeryeong Nam: methodology, software, formal analysis, data curation.
Sara Kim: investigation, data curation, visualization.
Sa-Hong Kim: investigation, data curation, visualization.
Seong-Ho Kong: conceptualization, writing—reviewing and editing, Supervision.
Hyuk-Joon Lee: conceptualization, writing—reviewing and editing, supervision.
Han-Kwang Yang: conceptualization, writing—reviewing and editing, supervision.
Corresponding author
Ethics declarations
Ethics Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study was approved by the Institutional Review board of the Seoul National University Hospital (approval number E-2006–057-1131). For this type of study, formal consent is not required.
Informed Consent
Informed consent was not required because the patient records from the NHIS-HEALS were anonymized and de-identified.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• Medical problems/expenditures increased with an increase in the degree of obesity.
• Mortality risk was the highest for middle-aged participants with severe obesity.
• Reducing the burden of obesity may help reduce the burden of disease on society.
Supplementary Information
Below is the link to the electronic supplementary material.
11695_2022_6327_MOESM1_ESM.docx
Supplemental Digital Content, Supplementary Table 1 (docx): Categorization of subjects according to BMI level of the index date and 12-year follow-up (DOCX 18 kb)
11695_2022_6327_MOESM2_ESM.docx
Supplemental Digital Content, Supplementary Table 2 (docx): Twelve-year survival rate according to each BMI category (DOCX 17 kb)
11695_2022_6327_MOESM3_ESM.docx
Supplemental Digital Content, Supplementary Table 3 (docx): Twelve-year survival rate according to each BMI category and age (DOCX 22 kb)

11695_2022_6327_Fig1_ESM.png
Supplemental Digital Content, Supplementary Figure 1: Flow chart of subject enrollment process from National Health Insurance Service Database (PNG 260 kb)

11695_2022_6327_Fig2_ESM.png
Supplemental Digital Content, Supplementary Figure 2: Kaplan–Meier survival curve according to each BMI category (PNG 408 kb)

11695_2022_6327_Fig3_ESM.png
Supplemental Digital Content, Supplementary Figure 3: Kaplan–Meier survival curve according to each BMI category and age (PNG 1002 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Park, JH., Park, D.J., Kim, H. et al. Twelve-Year Trajectory of Disease Burden and Mortality by Obesity Level in Korea: Analysis of the National Health Insurance Service Database. OBES SURG 33, 105–116 (2023). https://doi.org/10.1007/s11695-022-06327-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-022-06327-y