Abstract
Purpose
This study investigates the long-term effects of biliopancreatic diversion with duodenal switch (BPD-DS) on patients with advanced type 2 diabetes mellitus (T2DM) while paying special attention to preoperative diabetes severity.
Materials and Methods
A retrospective analysis was conducted using prospective and current data on patients who underwent an open BPD-DS 6–12 years ago. Patients were stratified according to preoperative diabetes severity into 4 groups (group 1: oral antidiabetic drugs only; group 2: insulin < 5 years; group 3: insulin 5–10 years; group 4: insulin > 10 years). The primary endpoint was T2DM remission rate 6–12 years after BPD-DS as a function of preoperative diabetes severity.
Results
Ninety-one patients with advanced T2DM were included. Sixty-two patients were available for follow-up (rate of 77%). Follow-up was performed (mean ± SD) 8.9 ± 1.3 years after surgery. Glycated hemoglobin (HbA1c) levels were 9.4 ± 2.0% before surgery and decreased to 5.1 ± 0.8% after 1 year and 5.4 ± 1.0% after 6–12 years. Insulin discontinuation rate after surgery as well as the rate of long-term remission decreased steadily from groups 1 to 4, while long-term mortality increased. T2DM remission rates were 93%, 88%, 45%, and 40% in groups 1, 2, 3, and 4, respectively. Late relapse of T2DM occurred in 3 patients (5%).
Conclusions
BPD-DS causes a rapid and long-lasting normalization of glycemic metabolism in patients with advanced T2DM. T2DM remission rate after 6–12 years varies significantly (from 40% to more than 90%) and is highly dependent on preoperative diabetes severity.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Type 2 diabetes mellitus (T2DM) is a chronic progressive metabolic disease [1]. Treatment includes lifestyle modification, administration of oral and injectable drugs, and the use of insulin; these therapies are usually initiated in a stepwise manner [2]. Conservative treatment is used to prevent or delay glycemic metabolism, delay the next therapeutic step, and postpone the onset of micro- and macrovascular complications [2,3,4]. Before the era of metabolic surgery, long-term remission of T2DM was not considered a therapeutic goal.
The introduction of metabolic surgery completely changed our understanding of T2DM [5]. Although earlier reports showed that gastrointestinal surgery can result in T2DM remission [6, 7], treatment of T2DM using gastrointestinal surgery is a novel concept [5]. In a landmark study by Pories et al., obese patients with diabetes who underwent a Roux-en-Y gastric bypass (RYGB) had an 83% chance of T2DM remission as well as normal glycemia and glycated hemoglobin (HbA1c) levels without being dependent on antidiabetic medication for up to 14 years [8]. In their meta-analyses, Buchwald et al. [9, 10] showed the varying efficacy of several gastrointestinal procedures with regard to T2DM remission. Biliopancreatic diversion (BPD), according to Scopinaro [11], and biliopancreatic diversion with duodenal switch (BPD-DS) [12, 13] were the most effective antidiabetic surgical procedures, with a diabetes remission or improvement rate of 95%.
Schauer et al. [14] classified T2DM severity from least severe to most severe according to the treatment required to maintain reasonable glycemic control. Severity classifications included patients with IFG (impaired fasting glucose), diet controlled T2DM, oral agent users, and insulin users. With data from a maximum of 4 years after Roux-en-Y gastric bypass (RYGB), these authors found that T2DM remission rate depends on disease severity and duration (≤ 5 years, 6–10 years, and > 10 years). Kapeluto et al. [15] studied 141 patients with insulin-treated T2DM who underwent BPD-DS over 10 years of follow-up and demonstrated an overall complete T2DM remission rate of 68%. However, Kapeluto et al. did not stratify their patients according to T2DM severity or disease duration. Here, we report on long-term effects in a cohort of patients, largely with advanced T2DM, that is comparable to that of Kapeluto. However, the major aim of this study was to investigate whether the evolution of T2DM after BPD-DS is dependent on preoperative T2DM severity and insulin therapy duration.
Materials and Methods
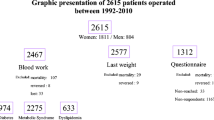
Ninety-four patients who underwent a BPD-DS between February 2005 and June 2011 were eligible for this retrospective analysis; data were collected prospectively. Three patients with type 1 diabetes mellitus (T1DM) were excluded, leaving 91 patients to be enrolled in the study. Current data were obtained during personal interviews or telephone calls, or from answers to mailed questionnaires, in addition to data collected during outpatient visits.
The indication for surgery was based mainly on T2DM severity, and not on the patient’s weight and body mass index (BMI). Main inclusion criteria were advanced T2DM and treatment with insulin or treatment with oral antidiabetic drugs (OAD) for at least 3 years without achieving a stable glycemic state with an HbA1c level of less than 7%. Although most of the patients had severe obesity, about 10% (n = 9) had a BMI below 35 kg/m2 [16].
T2DM severity was classified according to the treatment required to ensure an acceptable glycemic control [14], which was defined as a stable HbA1c level of < 7%, according to the current guidelines [2, 17]. All patients in the present study belong to class III or IV according to Schauer’s classification [14] and (with few exceptions) used either insulin or used OAD without achieving acceptable glycemic control. None of the patients suffered from initial or early-stage diabetes. Therefore, all cases were defined as advanced T2DM.
A multidisciplinary team, including a diabetologist, concluded that surgery was the best treatment option and offered surgery to the patient. All patients were well-informed about the risks and benefits of the procedures, and the necessity of lifelong surveillance and dietary supplementation with vitamins, micronutrients, calcium, iron (occasionally), and proteins, according to standard guidelines.
Surgical Technique
All surgical procedures were performed at the Department of General and Visceral Surgery, St. Josef Hospital Monheim, 40789 Monheim, Germany. One of the authors (Michael Frenken) performed all procedures in a highly standardized manner; he either performed the BPD-DS himself or assisted one of his colleagues in the operation. At the time these surgeries were performed, BPD-DS was an open procedure, performed either with a median incision or transverse upper abdominal incision with a median extension to the xiphoid (Mercedes star incision). A gastric sleeve resection was performed along a 44 French bougie. Resection was begun 6–8 cm above the pylorus to preserve antral motility. The total length of the small bowel was measured with a slide stretch on the antimesenteric side of the small bowel. The small bowel was transected either 250 cm proximal to the ileocolic valve, or at 300 cm if the total length of the small bowel exceeded 600 cm. An end-to-side duodenoileostomy was performed, and the oral end of the transected small bowel was anastomosed to the ileum at 100 cm proximal to the ileocolic valve, thus creating a common channel of 100 cm. A cholecystectomy and an appendectomy were routinely performed simultaneously in all patients if these organs were still present.
Follow-up
All patients were re-examined 3, 6, and 12 months after surgery at the cooperating Diabetes Center Rheinland, St Josef Hospital Haan, 42781 Haan, Germany, and annually thereafter in the Surgical Department of the St. Josef Hospital Monheim, 40789 Monheim, Germany. Between August 2016 and October 2017, one of the authors (Olga Kemmet) contacted all of the patients and asked them to participate in this study. After written informed consent was obtained, a patient-reported outcome questionnaire was sent by postal mail or e-mail. Ethical approval was obtained from the Ethics Committee of the Philipps University in Marburg, 35032 Marburg, Germany (file number 65/16).
Patient Stratification and Outcome Assessment
All patients were stratified into four groups based on mode of therapy and duration of insulin treatment (Table 1): group 1, oral antidiabetic drugs only; group 2, insulin < 5 years; group 3, insulin 5–10 years; and group 4, insulin > 10 years. The primary endpoint was T2DM remission rate 6–12 years after BPD-DS. In a short-term study on patients with advanced T2DM undergoing BPD-DS, we showed that T2DM remission rate after 2 years was 100, 97, 88, and 66% in groups 1, 2, 3, and 4, respectively [18]. Patient outcome was classified according to Brethauer et al.’s definition of glycemic outcome after bariatric surgery [19], which has 5 categories: complete remission, partial remission, improvement, unchanged, and recurrence. In short, complete remission is defined as normal measures of glucose metabolism (HbA1c < 6%, fasting blood glucose (FBG) < 100 mg/dL) in the absence of antidiabetic medications, partial remission as subdiabetic hyperglycemia (HbA1c 6–6.4%, FBG 100–125 mg/dL) in the absence of antidiabetic medications, improvement as statistically significant reduction in HbA1c and FBG not meeting criteria for remission or decrease in antidiabetic medications requirement, unchanged as the absence of remission or improvement, and recurrence as FBG or HbA1c in the diabetic range (≥ 126 mg/dL and ≥ 6.5%, respectively) or need for antidiabetic medication after any period of complete or partial remission. The most recent data available were used to determine glycemic outcome.
Mortality Analysis
Aminian et al. [20, 21] proposed and evaluated the Individualized Diabetes Complications (IDC) Risk Score to predict 10-year risk of end-organ complications from T2DM with and without metabolic surgery. They found that the IDC Risk Scores provide personalized evidence-based risk information for patients with type 2 diabetes and obesity regarding future cardiovascular outcomes and mortality with and without metabolic surgery based on their current status of obesity, diabetes, and related cardiometabolic conditions. For each patient in the present study, the preoperative 10-year all-cause mortality rate, the 10-year all-cause mortality rate after metabolic surgery, and the absolute change in the 10-year mortality rate were estimated using the IDC Risk Score by Aminian et al. [20, 21]. The IDC Risk Score is based on demographic data, medical history, clinical and laboratory data, and current medications. All data were extracted from a prospectively maintained database.
Statistical Analysis
Weight is expressed in kg and BMI in kg/m2. Percent excess weight loss (%EWL) and percent total weight loss (%TWL) were calculated using the following formulas: %EWL = (preoperative weight − current weight) × 100 / (preoperative weight − 25 × m2), and %TWL = (preoperative weight − current weight) × 100 / (preoperative weight). Ideal weight is defined as the weight corresponding to a BMI of 25 kg/m2. Data are expressed as mean ± standard deviation (SD). Standard error of the mean (SEM) is given when appropriate. An unpaired t test was used to compare the means of two groups. For comparison of categorial outcomes, the two-tailed Fisher’s exact test was used. A P value of 0.05 was considered statistically significant.
Results
Study Population
The mean patient age was 50 ± 10 years. Fifty-seven percent of the patients were female. All of the patients were White/Caucasian. Duration of preoperative medical treatment for T2DM (either OAD or insulin) was 9.7 ± 7.5 years, and 80% (73/91) of the patients were treated with insulin for an average duration of 6.6 ± 5.1 years. The mean preoperative HbA1c was 9.4 ± 2.0%. The mean weight and BMI were 141 ± 30 kg and 47 ± 9 kg/m2, respectively. Nine patients had a BMI below 35 kg/m2, with a mean BMI of 33.1 (range 28–34.9 kg/m2). Demographic and clinical baseline characteristics including estimated mortality rates are outlined in Table 2.
Early and Late Mortality
Ten deaths (14%, 10/84 patients, excluding patients lost to follow-up) were recorded during the study period. Two patients died within 30 days after the procedure (mortality 2.2%, 2/91). One patient died on postop day 6 due to fulminant pneumonia and sepsis. The second patient suffered from acute peritonitis caused by a small perforation of the distal esophagus and developed a fatal pulmonary embolism. This patient died on postop day 9. A third patient died on postop day 59 from acute respiratory distress syndrome, sepsis, and multiorgan failure.
Seven deaths occurred after this period. One patient died 21 months after surgery from myocardial infarction related to a preexisting coronary heart disease. A second patient died in another hospital 33 months after surgery from multi-organ failure following severe inflammation of a diabetic foot and sepsis. Late death occurred 6 years after BPD-DS in a third patient who suffered from lymph node metastases of a malignancy of unknown primary. The cause of death was unknown for 4 other patients. The last contact with these 4 patients was 6 months, 12 months, 2 years, and 5 years after surgery, and in no case was a fatal disease or deteriorating health situation noticed.
Among the ten patients who died, none was from group 1 (0/18), two were from group 2 (2/32), four from group 3 (4/28), and four from group 4 (4/13), with a mortality rate of 0%, 6%, 14%, and 31%, respectively.
Follow-up
Besides the patients who died (n = 10), two refused to participate, ten were located and contacted but did not return the questionnaires despite multiple phone calls, and seven were lost to follow-up. Thus, follow-up data are available for 62 patients. Follow-up was performed 8.9 ± 1.3 (range 6.3–12.0) years after surgery. The follow-up rate was 77% (62 with available follow-up data out of 81 patients eligible for follow-up) [22]. Follow-up was available for 14, 25, 18, and 5 patients from groups 1, 2, 3, and 4, respectively.
Evolution of T2DM and Diabetes Remission
Daily insulin requirement as well as early and late glycemic levels of all patients was assessed. Figure 1A shows the daily amount of insulin used. Preoperatively, 73/91 (80%) patients used insulin (131 ± 92 I.U. daily). At the time of discharge, 21 patients required insulin to maintain maximum glycemic levels below 200 mg/dL. These 21 patients used only small amounts of insulin (26 ± 12 I.U.) daily. After 1 year, 6 patients still used 14 ± 9 units of insulin daily. After 6–12 years, five patients used 20 ± 7 units of insulin daily (including three recurrences, see Fig. 2B). Thus, complete discontinuation of insulin therapy was achieved in 90% (43/48) of the patients. Figure 1B shows the development of HbA1c levels after BPD-DS. In addition to the development data of HbA1c after 6–12 years, a subgroup with the longest follow-up consisting of 16 patients followed up for 10–12 years was analyzed separately. In 11 of those 16 patients, HbA1c levels with an average follow-up duration of 10.6 ± 0.5 years and a mean HbA1c of 5.6 ± 0.8% (range, 4.6–7.0%) were available. These findings suggest that the 6–12-year data are also likely valid for a time span of 10 or more years. Figure 2 demonstrates the evolution of T2DM after BPD-DS dependent on the mode of diabetes therapy and insulin treatment duration (see Table 1 for stratification). Data for the 62 patients available for follow-up are shown. Figure 2A shows (for each group) the number of patients who used insulin preoperatively, upon discharge from the hospital, and at 1 month and 6–12 months after surgery. The longer the duration of preoperative insulin use, the lower the discontinuation rate of insulin during hospitalization (96%, 67%, and 20% of the patients in groups 2, 3, and 4, respectively), 1 year after surgery (100%, 94%, and 60% in groups 2, 3, and 4), and 6–12 years after BPD-DS (96%, 83%, and 80% in groups 2, 3, and 4, respectively). Six to 12 years after surgery, insulin therapy was necessary for two patients who exhibited a continuous need of small amounts of insulin over the years, and for three patients who suffered a disease recurrence (relapse). Figure 2B shows the rate of complete and partial remission, improvement, unchanged glycemic state, and recurrence in each of the four groups. The percentage of remission decreased as the intensity of diabetes therapy and the duration of treatment with insulin increased. Few patients relapsed (3/62, 5%). The three patients with T2DM recurrence were analyzed in detail but no specific explanation for the recurrence in these patients could be detected.
Evolution of T2DM as assessed by daily insulin requirement and HbA1c levels up to 12 years after BPD-DS. Panel A: The amount of insulin required before surgery (Pre-op), at discharge from hospital, after 1 year, and after 6–12 years in patients with advanced T2DM treated with insulin before undergoing BPD-DS. The number of patients (n) using insulin (numerator) and the number of patients available for follow-up at each time point or period (denominator) are also shown. Panel B: HbA1c levels preoperatively, after 1 year, and after 6–12 years. Additionally, data of all patients with a follow-up of more than 10 years is indicated (rightmost column, dotted lines, and dotted area). The number of patients available for follow-up is also shown. The dotted horizontal line at the HbA1c level of 6% indicates the upper limit of the normal range of HbA1c levels. Panels A and B: The columns show the mean (filled symbols), standard error of the mean (SEM, small bars), standard deviation (SD, narrow rectangles, base and top representing mean ± SD), and the minimum and maximum values (connected to the rectangles by dotted lines). BPD-DS, biliopancreatic diversion with duodenal switch; HbA1c, glycated hemoglobin; I.U., international units; SD, standard deviation; SEM, standard error of the mean; T2DM, type 2 diabetes mellitus
Effect of BPD-DS on percentage of patients requiring insulin observed at 4 different time points (A) and long-term T2DM remission rates up to 12 years after BPD-DS (B); both effects analyzed according to the T2DM severity groups. Sixty-two patients were available for follow-up. All patients were stratified at the time of surgery into 1 of 4 T2DM severity groups (see Table 1). Panel A shows the percentage of patients using insulin in each T2DM severity group: preoperatively (black circles), at discharge from the hospital (black triangles), 1 year after surgery (black squares), and 6–12 years after surgery (black squares standing on the tip). The numbers of patients using insulin (n, bottom line) and the number of all patients in that specific group (below the group classification on top) are shown. Panel B illustrates the long-term rates of remission, improvement, and recurrence of T2DM 6–12 years after BPD-DS. Glycemic outcome was divided into 5 categories following current recommendations [19]: complete remission (CR, open circles and open columns), partial remission (PR, open triangle standing on the tip and dotted column on top of CR), improvement (Im, open triangles and hatched columns), unchanged (open squares), and recurrence (Rec, open squares standing on the tip and reversed hatched columns). The bottom line shows the number of patients with remission, improvement, or recurrence in each of the 4 T2DM severity groups. BPD-DS, biliopancreatic diversion with duodenal switch; OAD, oral antidiabetic drugs; T2DM, type 2 diabetes mellitus
Re-operation to Modify Limb Length
Three patients had to be re-operated because of recurrent and life-threatening protein deficiency 2–3 years after BPD-DS. In 2 cases, the common channel was elongated at the expense of the biliopancreatic limb by 100 cm, and in one case by 150 cm. All three patients were eligible for follow-up more than 9 years after primary surgery. One patient belongs to group 1, another patient to group 2, and the third patient to group 3. At the time of the last follow-up, none of the three patients used any antidiabetic drugs. The most recent HbA1c levels for the first two patients were 4.8% and 4.9%. The third patient did not know his HbA1c, but, according to his general practitioner, his diabetes was resolved. Weight loss was excellent in 2 patients (BMI 50.5 to 24 and 49 to 25 kg/m2, respectively). In the third patient, BMI dropped from 55 to 27 kg/m2 after 2–3 years and increased to 45 kg/m2 after 6–12 years.
Weight and Weight Stability
Body weight, BMI, and %EWL are shown in Fig. 3. Preoperative weight and BMI amounted to (mean ± SD) 139 ± 31 kg and 46.0 ± 8.8 kg/m2 before surgery and 89 ± 21 kg and 29.3 ± 0.6 kg/m2 at 6–12 years after surgery, respectively. EWL was 80 ± 24% at 6–12 years after surgery. TWL amounted to 37 ± 8%, 39 ± 8%, and 35 ± 11% at 1, 4–5, and 6–12 years after surgery, respectively.
Development of body weight, body mass index (BMI), and percentage of excess weight loss. Mean (filled symbols), minimum (bar), and maximum (bar) values are shown. Standard deviation is depicted only at the time of surgery (OP) and at 6–12 years after surgery. Periods of 2–3 years, 4–5 years, and 6–12 years are indicated by symbols at 2.5 years, 4.5 years, and 9 years, respectively. Filled circles represent mean values of body weight, filled squares represent BMI, and filled triangles represent %EWL. Only those patients who were available for follow-up 6–12 years after surgery are shown. A number of patients at a specified time are indicated. Three patients with BMI ≤ 32 kg/m2 were excluded from the calculation of % EWL as calculations of %EWL in patients with low BMI do not provide reasonable results. BMI, body mass index; BPD-DS, biliopancreatic diversion with duodenal switch; %EWL, percent excess weight loss
Discussion
This study shows the evolution of T2DM up to 12 years after BPD-DS in a cohort of patients with advanced diabetes. For further analysis, the cohort was divided into four groups according to mode of diabetes therapy and duration of insulin treatment. The classification into groups according to T2DM treatment intensity serves as a surrogate for diabetes severity.
The main characteristics of the undivided cohort are as follows: first, 80% (73/91) of the patients were treated with insulin; second, the average duration of T2DM from onset of medical therapy was approximately 10 years, with an average duration of insulin therapy of approximately 7 years; third, despite the use of daily average insulin doses above 130 I.U., the mean HbA1c was as high as 9.4 ± 2.0% at the time of surgery; and fourth, since the primary indication for surgery was advanced T2DM regardless of weight or BMI, some patients (n = 9, 10%) did not meet the criteria of the National Institutes of Health [23]. Thus, although this is a population of patients with mostly higher-class obesity, the main indication for surgery was an advanced stage of T2DM.
This cohort exhibited sustainable long-term remission or improvement after 6–12 years, even in those patients who had used insulin for many years, as well as a low recurrence rate. The rate of complete remission was 71% (44/62), the rate of improvement combined with partial remission was 24% (15/62), and recurrence was observed in 5% (3/62) of patients. These results are consistent with two earlier studies on the long-term effects of BPD-DS on T2DM. Kapeluto et al. [15] reported 10-year remission rates in 141 patients with exclusively insulin-treated T2DM after BPD-DS and comparable patient characteristics (age, 48.5 years; female, 60%; BMI, 51.9 ± 7.8 kg/m2). Their study described a complete remission rate of 68.1%, a partial remission rate of 2.3%, an improvement rate of 15.9%, an unchanged rate of 2.3%, and a relapse rate of 11.4% [15]. Another study [24] on long-term outcomes for 153 patients who underwent laparoscopic BPD-DS found that only 24 patients had T2DM, including seven who were not insulin-dependent and seven who were on insulin treatment. The other ten patients were diagnosed with diabetes only perioperatively. The remission rate was 87.5% (21/24). Their results resemble those of groups 1 and 2 in our study.
The impact of diabetes severity on the metabolic effects of BPD-DS is investigated by dividing the study population into four different severity groups according to mode of therapy and duration of treatment with insulin. To the best of our knowledge, this is the first long-term study involving patients with advanced T2DM who underwent BPD-DS to stratify patients according to T2DM severity. We found that the absence of insulin therapy in group 2 was significantly higher at discharge from the hospital than in patients in groups 3 and 4. Because insulin requirement after 1 year and 6–12 years was low in all T2DM severity groups, no statistical difference was found among groups 2 to 4. Complete remission rate was similar between groups 1 and 2, but significantly different between group 2 and groups 3 and 4 combined. Thus, if patients do not use insulin for more than 5 years, a rapid discontinuation of insulin and complete remission of T2DM will likely occur. Even among patients in the groups with the most severe disease who were treated with insulin for more than 5 years, the remission and improvement rates after 6–12 years following BPD-DS were remarkable.
Ten patients died within the study period. Three patients died early (< 90 days, early mortality 3.3% [3/91]), and seven died within 6–12 postoperative years (late mortality 8.3% [7/84]). The mortality rates in this study are similar to those in the study by Kopeluto et al. (early mortality, 2.1%; late mortality, 9.9%) [15]. This relatively high surgery-related early mortality rate of 2–3% may be partly due to surgical complexity, open surgery technique, and lack of perioperative experience available more than 10 years ago. With the introduction of laparoscopic surgery for BPD-DS, 30-day mortality was reduced, but 90-day mortality was still 2.0% in one large study [24]. Thus, the main reason for the relatively high surgery-related early mortality rate may be due to the high proportion of patients with risk factors and co-morbidities. DeMaria et al. [25] showed a dramatic increase in early (90-day) mortality among patients who underwent gastric bypass surgery that was dependent on preoperative factors. The difference in mortality rate among the three risk classes was significant: class A, 0.31%; class B, 1.9%; and class C, 7.56%. Most of our patients were in classes B and C; therefore, this may be the main factor for the high early mortality rate.
Late mortality might best be explained by recently developed prediction models estimating the 10-year risk of end-organ complications (including death) in obese patients with T2DM who have or have not undergone metabolic surgery [20, 21]. Using preoperative data, we analyzed the 10-year all-cause mortality rate for each patient. Mean and SD for the four diabetes severity groups are shown in Table 2. This study’s observed mortality rates (0%, 6%, 14%, and 31% of groups 1, 2, 3, and 4, respectively) demonstrate a steady increase in mortality parallel to T2DM severity. This increase is likely not only due to a more advanced T2DM, including microvascular and macrovascular complications, but also due to increased age (see Table 2) and a higher incidence of other metabolic diseases such as arterial hypertension, dyslipidemia, hepatic steatosis, or similar. However, due to insufficient data, this hypothesis cannot be confirmed. Regardless of possible confounders, the observed mortality rate was consistently lower than predicted. One probable reason is that our mean follow-up time was only 8.9 years. Another possibility is that the extent of reduction of mortality following BPD-DS is higher than that of RYGB or sleeve gastrectomy, the two most commonly performed surgical procedures, when estimating mortality according to IDC Risk Scores [21]. The 10-year all-cause mortality risk without surgery increases substantially in conjunction with diabetes severity (see Table 2). Therefore, the absolute change in 10-year mortality risk significantly increases from groups 1 to 4, a compelling and unexpected finding that suggests that patients with the highest risks and lowest life expectancy may benefit the most from BPD-DS. On the other hand, BPD-DS might also be a good choice for patients with less advanced diabetes, since the mortality rate is low, the T2DM remission rate is high, and the chance of diabetes relapse is very low.
Also, of interest is the disappearance of insulin resistance within a few days postop, a fact demonstrated by the low postoperative insulin requirements. From the early postoperative period until postoperative year 12, the daily insulin requirement of the few patients who still needed insulin therapy was low, a sign of permanent normal insulin sensitivity (the opposite of insulin resistance) after BPD-DS (Fig. 1A). The insulin dose was nearly always lower or equivalent to the physiological secretion of insulin in non-insulin-resistant healthy adults [26, 27] or the amount needed in insulin-sensitive patients with destroyed β-cells in T1DM or missing β-cells after pancreatectomy. Mingrone et al. [28] and Harris et al. [29] examined this phenomenon in detail in patients who underwent BPD and RYGB and found that insulin sensitivity was higher after BPD than RYGB. The rapid disappearance of insulin resistance was analyzed earlier [30] in 27 patients after BPD-DS with repeated measurements of insulin resistance using the HOMA-IR index [31, 32]. The mean HOMA-IR index decreased from a preoperative value of 14.3 to 3.6 and 1.9 three and 7 days after surgery, respectively. There was no significant difference between the patients treated with OADs or insulin. Also, three patients who were discharged from the hospital with small amounts of insulin (a maximum of 36 units per day) had a low postoperative HOMA-IR index ranging from 1.3 to 2.6 [30]. Thus, the current study shows that, after BPD-DS, insulin sensitivity remains normal for at least the next 12 years.
This study had some limitations. The retrospective design, lack of a control group or any element of randomization, and the limited follow-up rate may have affected our results. However, we enrolled the patients consecutively and patients were registered prospectively according to a given standardized surveillance protocol. Furthermore, a standardized surgical protocol was used to eliminate the risk of bias from learning curve effects and inhomogeneity in surgical technique.
Conclusion
This study shows that long-term normalization of glycemia and insulin sensitivity, and a high rate of complete T2DM remission can be maintained up to 12 years after BPD-DS. Most importantly, the T2DM remission rate after BPD-DS depends on the preoperative treatment intensity and duration of insulin therapy, and ranges from approximately 90% in patients using no insulin or for less than 5 years to approximately 40% in patients using insulin for more than 5 years. The rate of discontinuation of insulin therapy after surgery, as well as predicted and observed mortality rates, is also dependent on T2DM severity. For different reasons, the use of BPD-DS should be seriously considered in all patients with advanced T2DM as it yields good outcomes in patients with moderate to severe T2DM. However, further research is required to confirm this claim.
References
Nathan DM. Diabetes: advances in diagnosis and treatment. JAMA. 2015;314:1052–62.
Nathan DM, Buse JB, Davidson MB, et al. Medical management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy: a consensus statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2009;32:193–203.
Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403.
American Diabetes Association. Standards of medical care in diabetes–2009. Diabetes Care. 2009;32(Suppl 1):S13–261.
Rubino F, Schauer PR, Kaplan LM, et al. Metabolic surgery to treat type 2 diabetes: clinical outcomes and mechanisms of action. Annu Rev Med. 2010;61:393–411.
Friedman MN, Sancetta AJ, Magovern GJ. The amelioration of diabetes mellitus following subtotal gastrectomy. Surg Gynecol Obstet; 1955;100(2):201–4.
Angervall L, Dotevall G, Tillander H. Amelioration of diabetes mellitus following gastric resection. Acta Med Scand 1961;169:743–8.
Pories WJ, Swanson MS, MacDonald KG, et al. Who would have thought it? An operation proves to be the most effective therapy for adult-onset diabetes mellitus. Ann Surg. 1995;222:339–50 (discussion 350–22).
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292:1724–37.
Buchwald H, Estok R, Fahrbach K, et al. Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am J Med. 2009;122:248–2256.e5.
Scopinaro N, Gianetta E, Civalleri D, et al. Bilio-pancreatic bypass for obesity: II. Initial experience in man. Br J Surg. 1979;66:618–20.
Hess DS, Hess DW. Biliopancreatic diversion with a duodenal switch. Obes Surg. 1998;8:267–82.
Marceau P, Hould FS, Simard S, et al. Biliopancreatic diversion with duodenal switch. World J Surg. 1998;22:947–54.
Schauer PR, Burguera B, Ikramuddin S, et al. Effect of laparoscopic Roux-en Y gastric bypass on type 2 diabetes mellitus. Ann Surg. 2003;238:467–84 (discussion 84–25).
Kapeluto JE, Tchernof A, Masckauchan D, et al. Ten-year remission rates in insulin-treated type 2 diabetes after biliopancreatic diversion with duodenal switch. Surg Obes Relat Dis. 2020;16:1701–12.
Frenken M, Cho EY. Metabolic intestinal bypass surgery for type 2 diabetes in patients with a BMI <35 kg/m2: comparative analysis of 16 patients undergoing either BPD, BPD-DS, or RYGB. Obes Facts. 2011;4 Suppl 1(Suppl 1):13–7.
American Diabetes Association. Standards of medical care in diabetes–2008. Diabetes Care. 2008 Jan;31(Suppl 1):S12–254.
Cho EY, Kemmet O, Frenken M. Biliopancreatic diversion with duodenal switch in patients with type 2 diabetes mellitus: is the chance of complete remission dependent on therapy and duration of insulin treatment? Obes Facts. 2011;4 Suppl 1(Suppl 1):18–23.
Brethauer SA, Kim J, el Chaar M, et al. Standardized outcomes reporting in metabolic and bariatric surgery. Surg Obes Relat Dis. 2015;11:489–506.
Aminian A, Zajichek A, Arterburn DE et al. Association of metabolic surgery with major adverse cardiovascular outcomes in patients with type 2 diabetes and obesity. JAMA 2019;322(13):1271–282.
Aminian A, Zajichek A, Arterburn DE, et al. Predicting 10-year risk of end-organ complications of type 2 diabetes with and without metabolic surgery: a machine learning approach. Diabetes Care. 2020;43:852–9.
Renquist K, Jeng G, Mason EE. Calculating follow-up rates. Obes Surg. 1992;2(4):361–7.
Gastrointestinal surgery for severe obesity. Proceedings of a National Institutes of Health Consensus Development Conference. Am J Clin Nutr. 1992:615S–2619S.
Bolckmans R, Himpens J. Long-term (10 yrs) outcome of the laparoscopic biliopancreatic diversion with duodenal switch. Ann Surg. 2016;264:1029–37.
DeMaria EJ, Portenier D, Wolfe L. Obesity surgery mortality risk score: proposal for a clinically useful score to predict mortality risk in patients undergoing gastric bypass. Surg Obes Relat Dis. 2007;3:134–40.
Polonsky KS, Given BD, Hirsch L, et al. Quantitative study of insulin secretion and clearance in normal and obese subjects. J Clin Invest. 1988;81:435–41.
Nyholm B, Walker M, Gravholt CH, et al. Twenty-four-hour insulin secretion rates, circulating concentrations of fuel substrates and gut incretin hormones in healthy offspring of type II (non-insulin-dependent) diabetic parents: evidence of several aberrations. Diabetologia. 1999;42:1314–23.
Mingrone G, Castagneto M. Bariatric surgery: unstressing or boosting the beta-cell? Diabetes Obes Metab. 2009;11(Suppl 4):130–42.
Harris L-A, Kayser BD, Cefalo C, et al. Biliopancreatic diversion induces greater metabolic improvement than Roux-en-Y gastric bypass. Cell Metab. 2019;30:855–2864.e3.
Frenken M, Cho EY, Karcz WK, et al. Improvement of type 2 diabetes mellitus in obese and non-obese patients after the duodenal switch operation. J Obes. 2011;2011: 860169.
Matthews DR, Hosker JP, Rudenski AS, et al. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9.
Wallace TM, Levy JC, Matthews DR. Use and abuse of HOMA modeling. Diabetes Care. 2004;27:1487–95.
Author information
Authors and Affiliations
Contributions
Study conception and design: Michael Frenken, Olga Kemmet, Miriam Frenken, Ingo Röhrig, Lars Fischer, Achim Hellinger.
Acquisition of data: Michael Frenken, Olga Kemmet.
Analysis and interpretation of data: Michael Frenken, Olga Kemmet.
Drafting of manuscript: Michael Frenken, Olga Kemmet.
Critical revision: Michael Frenken, Olga Kemmet, Miriam Frenken, Ingo Röhrig, Lars Fischer, Achim Hellinger.
Corresponding author
Ethics declarations
Ethical Approval
All procedures performed in studies involving human participants were done so in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For the retrospective part of the study, formal consent was not required.
Consent to Participate
Informed consent was obtained from all participants in the study who participated in the last follow-up.
Conflict of Interest
The authors declare no competing interests.
Confirmation of STROBE Statement
The present study complies with each item on the STROBE checklist.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• Patients with advanced T2DM were analyzed 6–12 years after BPD-DS.
• Overall, complete T2DM remission rate was 71% with an improvement rate of 23%.
• Remission rate, absence of insulin, and mortality were dependent on T2DM severity.
• BPD-DS offers favorable outcomes for patients with moderate to severe T2DM.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Frenken, M., Kemmet, O., Frenken, M. et al. Long-term Remission of Type 2 Diabetes and Patient Survival After Biliopancreatic Diversion with Duodenal Switch. OBES SURG 32, 3340–3350 (2022). https://doi.org/10.1007/s11695-022-06223-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-022-06223-5