Abstract
Purpose
Roux-en-Y gastric bypass (RYGB) and sleeve gastrectomy (SG) are the two most popular procedures performed. The decision of which technique is most appropriate depends on the surgeon’s preferences and experience. However, several factors strongly influence the decision of the procedure performed, including gastrointestinal disorders or asymptomatic upper gastrointestinal endoscopy (UGE) findings.
This study aimed to describe the pathological endoscopic findings in morbidly obese patients undergoing preoperative routine UGE.
Materials and Methods
A retrospective review of a prospectively collected database of all UGEs performed before bariatric surgery was performed. UGE was routinely performed to all the patients as part of the preoperative evaluation protocol.
Results
A total of 790 patients were included. Surgical technique included 610 (77.2%) RYGB and 180 (22.8%) SG. Twenty-one asymptomatic patients presented esophagitis at UGE. In only seven patients (0.89%), the endoscopic findings of esophagitis had changed the initial surgical decision. The presence of ulcers or adenomatous or incompletely resected polyps was an indication for SG, to assure future endoscopic access in case it is needed. In 25 patients (3.17%), the initial operation would have been changed based on UGE findings.
Conclusion
Preoperative UGE allows the diagnosis of asymptomatic esophagitis related to gastroesophageal reflux disease and the identification of asymptomatic polyps and ulcers, with the potential ability for malignant transformation. In up to 3.17% of the cases, the endoscopic findings changed the operative strategy. As the complication rate associated with the procedure is low, we recommend the routine performance of preoperative UGE before bariatric surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bariatric surgery has become the most powerful tool as a long-term solution to both obesity and its associated pathologies [1,2,3,4,5,6,7,8,9,10,11]. Currently, Roux-en-Y gastric bypass (RYGB) and sleeve gastrectomy (SG) are the two most popular bariatric procedures performed [6, 8]. There is no ideal or worldwide standardized bariatric operative procedure. The trend is to perform the simplest, easiest, and least-invasive procedure [12,13,14]. The decision of which technique is most appropriate for a patient depends often on the surgeon’s preferences and experience. However, several factors strongly influence the decision of the procedure performed, including gastrointestinal disorders or even asymptomatic endoscopic findings.
Many upper digestive pathologies are directly associated with morbid obesity: hiatal hernia, gastroesophageal reflux disease (GERD), and its complications, including erosive esophagitis, Barrett’s esophagus, and esophageal adenocarcinoma [15]. These pathologies are not exclusive in population with obesity, but are more common among them, because the esophageal sphincter is affected, due to the excessive visceral fat that increases intra-abdominal pressure. Consequently, the gastric pressure is increased and the gastric emptying is altered [3, 15,16,17].
The performance of a routine upper gastrointestinal endoscopy (UGE) is still controversial. Despite UGE is associated with a low complication rate [18], some groups defend that it is unnecessary to expose patients to a routine UGE, given the low prevalence of asymptomatic findings that may change the surgeons’ decision of the bariatric technique to be performed [19,20,21].
This study aimed to describe the pathological endoscopic findings in morbidly obese patients undergoing preoperative routine UGE.
Patients and Methods
A retrospective review of a prospectively collected database of all UGEs performed before primary bariatric surgery between 2014 and 2018 was performed.
UGE was routinely performed to all the patients as part of the preoperative evaluation protocol.
Preoperative Evaluation
Preoperative assessment included routine abdominal ultrasound, upper gastrointestinal endoscopy (UGE) with Helicobacter pylori diagnostic test, functional respiratory tests, and nutritional analytical evaluation that included serum levels of calcium, iron, and vitamins A, D, E, B12, and folic acid. Psychiatrists assessed interviews to evaluate the implication of the patient in the postoperative course. Patients received information about possible perioperative complications and necessary postoperative nutritional supplementation.
Endoscopic findings of esophagitis were classified according to the Los Angeles classification in stages A to D [22].
Selection Criteria of the Surgical Technique
All the patients considered for bariatric surgery had either BMI ≥ 40 kg/m2 or BMI ≥ 35 kg/m2 with inadequately controlled obesity-related comorbidities (e.g., T2D, hypertension, dyslipidemia, or sleep apnea/hypopnea syndrome). At our institutions, SG and RYGB are the only techniques performed as primary bariatric procedures. All the techniques were laparoscopically performed. Patients with a BMI over 50 kg/m2, high surgical risk due to comorbidities (ASA IV), a known severe nutritional deficit (preoperative hypoproteinemia or uncontrolled vitamin or mineral deficiencies), comorbidities requiring chronic medication (such as corticoids, immune suppressors,…) intestinal inflammatory disease, and a probability of technical difficulty before surgery (multiple previous surgeries or known anatomic modifications) were assigned for SG procedure. In patients with clinical symptoms of GERD, RYGB was considered the bariatric technique of choice. GERD was assessed using the questionnaire for GERD detection designed by Manterola et al. and validated in the Spanish language [23]. Those patients presenting endoscopic gastric or duodenal findings, which may require an eventual endoscopic follow-up (ulcers, partially resected polyps, or adenomatous polyps), were selected for SG. The cases with a positive diagnosis of Helicobacter pylori were treated with diverse treatment lines to achieve a preoperative eradication; if this was not finally achieved, the patient was selected for SG or, if GERD diagnosis coexists, to RYGB with resection of the gastric remnant; SG associated with hiatal repair was not considered as an alternative approach, as in our previous experience, we have various cases with severe recurrence of GERD symptoms, requiring a further RYGB. In the rest of the cases, without any of these mentioned conditions, the surgical technique was decided in the weekly meetings of the multidisciplinary team, customizing the decision based on age, comorbidities, and the expected results with each approach. At our institution, we have a wide experience performing RYGB, with excellent long-term results; for SG, we do not have enough long-term experience yet. Thus, most cases without contraindications for RYGB were selected to undergo this technique. The recommendation of the multidisciplinary team was communicated to the patients and their opinion was also considered for the final decision.
Hiatal hernias and their size were not routinely recorded as we consider that UGE is not the best method to assess them. Anyway, if a hiatal hernia is detected intraoperatively, it is repaired, independently of the selected bariatric approach.
Variables
Baseline age, gender, and comorbidities were recorded. Findings assessed at UGE included esophagitis, and esophageal, gastric or duodenal erythema, ulcers or polyps. Erythema was defined as the finding of mottled patchy redness in the gastric or duodenal mucosa, histologically correlated with mild-to-moderate mucosal inflammation.
Statistical Analysis
Data analysis was performed using SPSS Version 22.0 (SPSS Inc., Chicago, IL). Results are expressed as means ± SD or number and percentages. Student’s t tests were used to compare quantitative variables between groups. A P value < 0.05 was considered statistically significant.
Results
A total of 790 patients were included, 536 females (67.8%) and 254 males (32.2%), with a mean age of 45 ± 10.5 years; 547(69.3%) were under 50 years. Comorbidities and symptoms of GERD are also reported in Table 1.
Surgical technique included 610 (77.2%) RYGB and 180 (22.8%) SG. In two patients undergoing RYGB, resection of the gastric remnant was performed, due to impossibility of eradication of Helicobacter pylori and GERD coexistence. The distribution of surgical techniques depending on gender and age over or under 50 years is described in Table 2. Patients over 50 years (69.1%) and females (72.3%) underwent more frequently RYGB.
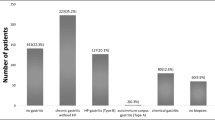
As previously mentioned, UGE was carried out in all the patients, as it was part of the routine preoperative protocol. There were no complications associated with the UGE procedure. Endoscopic findings are summarized in Table 3. Only 82 patients (10.4%) presented a normal UGE. Clinical symptoms of GERD were present in 142 patients; all of them were confirmed with endoscopic signs of esophagitis. However, 21 asymptomatic patients also presented esophagitis. Esophagitis was more frequent among patients over 50 years (110 cases; 67.4%) and females (108 cases; 66.3%). A total of 76.2% (16 patients) of asymptomatic esophagitis appeared in patients over 50 years and 61.9% (13 patients) were females.
Barrett’s esophagus appeared in 18 patients (2.3%), all of them clinically symptomatic. This entity was also more frequent among patients over 50 years (72.2%), whereas the incidence was similar in both genders. All the patients with Barrett’s esophagus underwent RYGB. Endoscopic follow-up was performed at 3, 6, and 12 months after surgery, with complete disappearance of Barrett’s esophagus in 12 patients (66.7%) and partial remission in the rest of the cases.
The rest of endoscopic findings, gastric or duodenal erosions, ulcers, or polyps were asymptomatic or coexisted with clinical manifestations of GERD. Histological examination of all these lesions did not show features of malignancy in any of the cases.
Changes in Surgical Decision Based on Endoscopic Findings
Following the selection criteria for the bariatric technique, 610 patients (77.2%) underwent RYGB and 180 patients (22.8%) SG. Assuming that all the patients with clinical symptoms of GERD will be selected for RYGB, only 21 patients (2.7%) with asymptomatic esophagitis could be initially indicated for SG, changing the decision to carry out RYGB. We have reviewed the clinical history of these patients in the multidisciplinary team meeting and have discussed if we would have indicated an SG in the absence of UGE. In such cases, in 14 of the 21 cases (66.7%), the decision of advising RYGB would have been independent of the endoscopic findings, as these patients presented with metabolic syndrome, which would be more prone to improvement with RYGB than SG in our experience. Thus, in only seven patients (0.89%), the endoscopic findings of esophagitis had changed the surgical decision.
Gastric or duodenal erosions at UGE did not change the indication of surgical technique in any cases. However, the presence of ulcers, adenomatous or, partially resected polyps were indications for SG, to assure future endoscopic access when necessary. Patients with gastric or duodenal ulcers did not undergo a repeat UGE to ensure healing prior to bariatric surgery. Gastric and duodenal ulcers were present in 14 patients and adenomatous or partially resected polyps in 10 patients. These conditions represent in 24 patients (3%). After reviewing the clinical histories, in 18 patients (2.28%), the initial indication would have been RYGB, but it has been changed to SG.
The persistence of Helicobacter pylori despite several eradication lines has not been considered as a cause for changes in the surgical decisions based on endoscopic findings. The lack of eradication of Helicobacter pylori can be determined with the urease test and the surgical decision can be just based on these results in the absence of UGE.
Altogether, we can estimate that the UGE findings have changed the decision of surgical technique in 3.17% of the cases.
Discussion
The recently published Spanish guidelines for bariatric surgery recommend performing a routine UGE or contrast-enhanced esophago-gastro-duodenal series only in those patients who will undergo a procedure including a gastric remnant and duodenal exclusion [24]. The European Association for Endoscopic Surgery (EAES) recommends one of these complementary tests to all patients in the preoperative assessment. [18] The Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) and the American Society of Gastrointestinal Endoscopy (ASGE) recommend UGE to be individualized in cases when a gastric pathology is suspected or Helicobacter pylori infection is present, deciding the selected bariatric procedure after the UGE investigation [25, 26]. Finally, the guidelines of the American Society for Metabolic & Bariatric Surgery (ASMBS) only recommend it in selected cases with the symptomatic gastric disease [18]. Independently of the planned bariatric technique, they recommend a mandatory UGE for those patients with preoperative symptoms of GERD or gastritis [27, 28].
All these societies pay special attention to the presence of GERD and mostly recommend to carry out a UGE when clinical symptoms are present. In our experience, 18% of the patients that planned to undergo bariatric surgery showed clinical symptoms of GERD. In all of them, a certain degree of esophagitis has been confirmed, and additionally, 2.7% of the patients presented features of esophagitis despite they were clinically asymptomatic. In our opinion, it is quite more important to diagnose asymptomatic esophagitis rather than confirm symptomatic cases, as in the first situation, the patients may be indicated to undergo a SG, which can aggravate the esophagitis and will induce symptoms, which can be difficult to be controlled with conservative treatment. [29]. Yeung et al. have reported in a recently published meta-analysis that the increase of postoperative GERD after SG can reach up to 19% of the patients and the appearance of de novo reflux rate was 23%. Their long-term prevalence of esophagitis was 28% and Barrett’s esophagus was 8%. Four percent of all patients undergoing SG required conversion to RYGB for severe reflux [30]. However, several studies defend that SG is not a contraindication for GERD without Barrett’s esophagus and even describe a symptomatic improvement and a reduction in the DeMeester score at pH-metry [31]. In our previous experience, we observed a worsening of GERD symptoms after SG, even in those cases with hiatal hernia after repair of the hiatus, requiring in many cases a further conversion to RYGB for uncontrolled symptomatology.
Moreover, UGE is not the best diagnostic method for GERD; the gold standard test for its confirmation is the pH-metry [32]. In our protocol, pH-metry is only considered for patients with clinical manifestations for GERD, but without endoscopic features of esophagitis. In such cases, pH-metry is indicated to confirm the diagnosis of GERD or to rule out other circumstances that may mimic the symptomatology of GERD. In the present series, no patients underwent pH-metry. Schwameis et al. reported that all the patients with esophagitis grade C and D presented abnormal values at pH-metry, whereas 79% and 75% of patients with grade A and B esophagitis, respectively, presented abnormal pH scores. Consequently, they recommend pH testing prior to antireflux surgery in patients with grade A or B esophagitis [33]. It is true that all of our clinically asymptomatic patients, initially advised undergoing a SG, but later changed the indication to RYGB based on the UGE findings, presented grade A or B esophagitis. Despite that we can assume that up to 25% of esophagitis cannot be secondary to acid reflux, they can probably be due to bile reflux caused by duodeno-gastro-esophageal reflux because of pyloric incompetence. Even in these cases, we would also recommend RYGB rather than SG, in order to distance the bile from the esophagus.
In our series, in only seven patients (0.89%), the endoscopic findings of esophagitis had changed the surgical decision, based on endoscopic findings of esophagitis. However, we must take into consideration that 77.2% of our patients underwent RYGB. Actually, SG is the most frequent procedure performed worldwide. Thus, this percentage could be significantly increased when applied to other populations. Saarinen et al. described in their study that a great majority (92%) of the clinically significant findings in UGE are relevant if the chosen operation is SG (hiatal hernia, esophagitis, Barrett’s esophagus) [34].
UGE also evaluates other conditions that may change the planned surgical procedure (peptic ulcers, polyps,..). The routine performance of UGE may lead to minimizing complications in the postoperative period, especially related to ulcer’s perforations or the development of malignancies on ulcers or polyps [3, 15, 35,36,37]. In our series, in 30 patients (3.8%), the decision of surgical technique was changed based on these items. As most of our bariatric procedures are RYGB, this percentage is probably higher than among other groups undergoing more frequently SG.
Duodenal and especially gastric ulcers have been associated with the coexistence of neoplasms in up to 14% of the cases and with a close follow-up new-onset neoplasms arising on the ulcer has been observed in up to 4.9% of the cases [38]. In our series, 1.3% of the patients presented gastric ulcers and 0.5% duodenal ones. Several studies have demonstrated that with the eradication of H. pylori, this risk significantly decreases. On the other hand, ulcers are also at risk of bleeding, and having endoscopic access to control it is recommendable. Consequently, given the risk of complications related to the ulcer, it seems to be mandatory, first to diagnose them preoperatively and second to have endoscopic access to them, in order to control an eventual evolution to neoplasms or the appearance of complications (perforations or bleedings) [39]. Up to 2% of patient candidates for bariatric surgery may present these entities preoperatively. Moreover, it has been described that gastric and duodenal ulcers are also associated with postoperative complications. Therefore, it is recommendable to know their presence before deciding the most appropriate technique [37].
More controversial is the issue referring to gastric or duodenal polyps. In our series, the prevalence of these entities is 5.7%, similar to that reported by other series of non-bariatric patients [40, 41]. Among our patients presenting gastric polyps, 32 out of 41 (78%) were hyperplastic polyps and 9 (22%) adenomatous ones. Seventy-five percent of the duodenal polyps showed hyperplasia and 25% adenoma. Adenomatous polyps are at risk of evolving to a malignant entity; however, the malignant transformation of hyperplastic ones is rare. [41]. Thus, we assume in our protocol that all patients with adenomatous polyps or those ones not completely excised at preoperative UGE are not suitable candidates for RYGB, because of leaving a gastric remnant without the possibility of endoscopic control.
Altogether, we can assume that endoscopic findings have changed the decision of the bariatric technique to be performed in 3.17% of the patients. Iman Ghaderi 2019 [35] reported a 3.34% of changes in the selection of the technique, and given this small rate, they do not recommend routine preoperative UGE. In contrast, a recently published paper of a German group, including 636 bariatric patients, reports a change in the operative strategy in only 1.6%; however, they found the performance of preoperative UGE essential, as it allows the identification of a wide range of abnormal endoscopic findings, which may have a significant impact on decision-making [42]. However, several papers have reported greater percentages of changes in decision. Parikh et al., in a systematic review, observed 7.6% of preoperative endoscopic findings that influenced, altered, or delayed the surgical treatment of obesity [21]. Schneider et al. described that preoperative endoscopy led to a change of the bariatric approach in 16% of the patients, specifically 16.5% in the RYGB group and 15.9% in the SG group [43].
Conclusion
Preoperative UGE allows the diagnosis of asymptomatic esophagitis related to GERD, and the identification of asymptomatic polyps and ulcers, with the potential ability for malignant transformation. In up to 3.17% of the cases, the endoscopic findings changed the operative strategy. As the complication rate associated with the procedure is low, we recommend the routine performance of preoperative UGE prior to bariatric surgery.
References
Obesity and overweight facts sheet. World Health Organization Website. https://www.who.int/news-room/fact-sheets/detail/ obesity-and-overweight. Updated. Accessed March 2, 2020. February 16, 2018:3.
Diabetes facts sheet. World Health Organization Website. https://www.who.int/news-room/fact-sheets/detail/diabetes. Updated October 30, 2018. Accessed March 2, 2020.
Wolter S, Duprée A, Miro J, et al. Upper gastrointestinal endoscopy prior to bariatric surgery-mandatory or expendable? An analysis of 801 cases. Obes Surg. 2017;27(8):1938–43.
Sjostrom L. Review of the key results from the Swedish Obese Subjects (SOS) trial—a prospective controlled intervention study of bariatric surgery. J Intern Med. 2013;273(3):219–34.
Jans A, Näslund I, Ottosson J, et al. Duration of type 2 diabetes and remission rates after bariatric surgery in Sweden 2007–2015: a registry-based cohort study. PLoS Med. 2019;16(11):e1002985.
Zhao H, Jiao L. Comparative analysis for the effect of Roux-en-Y gastric bypass vs sleeve gastrectomy in patients with morbid obesity: evidence from 11 randomized clinical trials (meta-analysis). Int J Surg. 2019;72:216–23.
Gastrointestinal surgery for severe obesity: National Institutes of Health Consensus Development Conference Statement. Am J Clin Nutr. 1992;55(2 Suppl):615S–619S.
Canil AM, Iossa A, Termine P, et al. Histopathology findings in patients undergoing laparoscopic sleeve Gastrectomy. Obes Surg. 2018;28(6):1760–5.
Wang Y, Song Y, Chen J, et al. Roux-en-Y gastric bypass versus sleeve gastrectomy for super super obese and super obese: systematic review and meta-analysis of weight results, comorbidity resolution. Obes Surg. 2019;29(6):1954–64.
Kang JH, Le QA. Effectiveness of bariatric surgical procedures. Medicine. 2017;96(46):e8632.
Brunt EM, Wong VW, Nobili V, et al. Nonalcoholic fatty liver disease. Nat Rev Dis Primers. 2015;1:15080.
Pories WJ. Bariatric surgery: risks and rewards. J Clin Endocrinol Metab. 2008;93(11 Suppl 1):S89–96.
Stefater MA, Wilson-Pérez HE, Chambers AP, et al. All bariatric surgeries are not created equal: insights from mechanistic comparisons. Endocr Rev. 2012;33(4):595–622.
Wolfe BM, Kvach E, Eckel RH. Treatment of obesity: weight loss and bariatric surgery. Circ Res. 2016;118(11):1844–55.
Abou Hussein B, Khammas A, Shokr M, et al. Role of routine upper endoscopy before bariatric surgery in the Middle East population: a review of 1278 patients. Endoscopy International Open. 2018;06:E1171–6.
Öner Rİ, Özdaş S. Histopathological findings in morbid obese patients undergoing laparoscopic sleeve Gastrectomy: does H. pylori infection effective on pathological changes? Obes Surg. 2018;28(10):3136–41.
Bou Daher H, Sharara AI. Gastroesophageal reflux disease, obesity and laparoscopic sleeve gastrectomy: the burning questions. World J Gastroenterol. 2019;25(33):4805–13.
Sauerland S, Angrisani L, Belachew M, et al. Obesity surgery: evidence-based guidelines of the European Association for Endoscopic Surgery (EAES). Surg Endosc. 2005;19:200–21.
Dhariwal A, Plevris JN, Lo NT, et al. Age, anemia, and obesity associated oxygen desaturation during upper gastrointestinal endoscopy. Gastrointest Endosc. 1992;38:684–8.
Bennett S, Gostimir M, Shorr R, et al. The role of routine preoperative upper endoscopy in bariatric surgery: a systematic review and meta-analysis. Surg Obes Relat Dis. 2016;12:1116–25.
Parikh M, Liu J, Vieira D, et al. Preoperative endoscopy prior to bariatric surgery: systematic review and meta-analysis of the literature. Obes Surg. 2016;26:2961–6.
Kasyap AK, Sah SK, Chaudhary S. Clinical spectrum and risk factors associated with asymptomatic erosive esophagitis as determined by Los Angeles classification: a cross-sectional study. PLoS One. 2018;13:e0192739.
Manterola C, Munoz S, Grande L, et al. Initial validation of a questionnaire for detecting gastrooesophageal reflux disease in epidemiological settings. J Clin Epidemiol. 2002;55:1041–5.
Martın Garcıa-Almenta E, Ruiz-Tovar J, Sanchez SS. Vıa clınica en cirugıa bariatrica. Albacete: Im3diA comunicacion S.L.; 2017.
SAGES guideline for clinical application of laparoscopic bariatric surgery. Surg Obes Relat Dis. 2009;5:387–405.
Evans JA, Muthusamy VR, Acosta RD, et al. The role of endoscopy in the bariatric surgery patient. Gastrointest Endosc. 2015;29:1007–17.
Schreiner MA. Endoscopy in the obese patient. Gastroenterol Clin N Am. 2010;39:87–97.
SAGES Guidelines Committee. SAGES guideline for clinical application of laparoscopic bariatric surgery. Surg Endosc. 2008;22:2281–300.
Melissas J, Braghetto I, Molina JC, et al. Gastroesophageal reflux disease and sleeve gastrectomy. Obes Surg. 2015;25(12):2430–5.
Yeung KTD, Penney N, Ashrafian L, et al. Does sleeve gastrectomy expose the distal esophagus to severe reflux?: a systematic review and meta-analysis. Ann Surg. 2020;271:257–65.
Gagner M. Is sleeve gastrectomy always an absolute contraindication in patients with Barrett's? Obes Surg. 2016;16:715–7.
Pérez de la Serna y Bueno J, Ruiz de León San Juan A. pH-metry/impedance-24 hours pH-metry. Rev Esp Enferm Dig. 2015;107(4):243.)
Schwameis K, Lin B, Roman J, et al. Is pH testing necessary before antireflux surgery in patients with endoscopic erosive esophagitis? J Gastrointest Surg. 2018;22:8–12.
Saarinen T, Kettunen U, Pietiläinen KH, et al. Is preoperative gastroscopy necessary before sleeve gastrectomy and Roux-en-Y gastric bypass? Surg Obes Relat Dis. 2018;14:757–63.
Ghaderi I, Gondal AB, Samamé J, et al. Preoperative endoscopic and radiologic evaluation of bariatric patients: what do they add? J Gastrointest Surg. 2019; https://doi.org/10.1007/s11605-019-04219-8.
Peker KD, Sahbaz NA, Seyit H, et al. An alternative view on the necessity of EGD before sleeve gastrectomy. Surg Obes Relat Dis. 2017;13(12):1959–64.
Fernandes SR, Meireles LC, Carrilho-Ribeiro L, et al. The role of routine upper gastrointestinal endoscopy before bariatric surgery. Obes Surg. 2016;26:2105–10.
Rosai J. Stomach. In: Rosai J, editor. Ackerman’s surgical pathology. St Louis: Mosby; 1996. p. 616–66.
Kashiwagi H. Ulcers and gastritis. Endoscopy. 2003;35(1):9–14.
Genta RM, Schuler CM, Robiou CI, et al. No association between gastric fundic gland polyps and gastrointestinal neoplasia in a study of over 100,000 patients. Clin Gastroenterol Hepatol. 2009;7:849–54.
Carmack SW, Genta RM, Schuler CM, et al. The current spectrum of gastric polyps: a 1-year national study of over 120,000 patients. Am J Gastroenterol. 2009;104:1524–32.
Moulla Y, Lyros O, Mehdorn M, et al. Preoperative upper-GI endoscopy prior to bariatric surgery: essential or optional? Obes Surg. 2020; https://doi.org/10.1007/s11695-020-04485-5.
Schneider R, Lazaridis I, Kraljevic M, et al. The impact of preoperative investigations on the management of bariatric patients; results of a cohort of more than 1200 cases. Surg Obes Relat Dis. 2018;14:693–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Statement of Informed Consent
Informed consent was obtained from all individual participants included in the study.
Statement of Human Rights
All procedures performed in this study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
García-Gómez-Heras, S., Garcia, A., Zubiaga, L. et al. Prevalence of Endoscopic Findings Before Bariatric Surgery and Their Influence on the Selection of the Surgical Technique. OBES SURG 30, 4375–4380 (2020). https://doi.org/10.1007/s11695-020-04800-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-04800-0