Abstract
Background
The potential effect of bariatric surgery on weight reduction and improvement of associated comorbidities is known, but the ratio obtained between the components of body weight, including lean body mass, body fat mass, and bone mass, is still not determined. This study aims to verify the changes in body composition during the first year after bariatric surgery.
Methods
We conducted a prospective observational cohort study. Fifty patients who underwent bariatric surgery and maintained follow-ups were selected. Patients were assessed preoperatively and postoperatively for periods of 1, 3, 6, and 12 months using tetrapolar bioelectrical impedance analysis and laboratory testing of lipids and serum albumin levels. Data were statistically analyzed.
Results
Statistically significant differences (p < 0.001) were obtained between the preoperative and 12-month evaluation respectively, for body mass index (BMI) (45.8 ± 7.5 to 30.0 ± 4.8 kg/m2), FM (64.7 ± 15.5 to 30.6 ± 9.8 kg), PFM (51.6 ± 4.17 to 37.3 ± 7.6%), and total cholesterol levels (197.1 ± 49.8 to 169.8 ± 31.0 mg/dL). The decrease in PFM shows a better proportion between the body components. PFM showed significantly higher decrease in males than in females (p = 0.012). Lean body mass (p = 0.000) reduction was highest for patients operated by the Unified Health System (SUS, Government of Brazil) probably because of its few financial resources to maintain postoperative care.
Conclusion
The change in body composition of patients who underwent Roux-en-Y gastric bypass was statistically significant for all variables examined during the first year postoperatively. This shows the effectiveness of the surgical procedure and clinical protocol set, which tends to favor a better health prognosis and weight maintenance in the long term.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The benefits of bariatric surgery for weight reduction and the improvement or regression of comorbidities associated with obesity are well known and documented. However, some patients regain weight or symptoms of comorbidities reoccur in the long term. It could be related to an excessive reduction in lean body mass and a consequent decrease in basal metabolism and/or associated with a high residual body fat mass [1, 2]. Few studies have focused on demonstrating that changes occurring after surgery on body composition and quality are able to provide a prognosis of good health and weight maintenance in the long term.
The bioelectrical impedance analysis (BIA) is one of the methods for body composition analysis and is based on the principle of resistance and reactance that cells impose to the electric current frequency emitted by the device. Within this method, there are several configurations of the device. The InBody520® is a multifrequencial bioelectrical impedance tetrapolar device with eight tactile electrodes for assessing segmental body composition [3]. Additionally, it has validation by the Food and Drug Administration (FDA).
Body composition means much more to the health-disease process than the isolated weight check. Seeking the long-term health of patients undergoing bariatric surgery makes it necessary to know the alteration of body composition during weight reduction so that the ducts are reviewed whenever necessary. In Brazil, many people with low socioeconomic conditions perform the surgical procedure through the Unified Health System, a governmental system to provide medical care to the needy population. Unfortunately, many of these people will not be able to perform adequate feeding in the postoperative period, and this may impair the surgical outcome.
The objective of this study was to verify the real modification of the body composition during the first year after bariatric surgery (gastric bypass) of the patients followed by the team of the Center for Obesity and Metabolic Syndrome of Brazil, which serves private patients and the Unified Health System.
Materials and Methods
A prospective longitudinal observational cohort study was conducted. Patients eligible for the study met the following inclusion criteria: age range between 18 and 65 years; obese eligible for bariatric surgery with the Roux-en-Y gastric bypass technique (RYGBP) during the first semester of 2009 at the Tertiary Center for Obesity and Metabolic Syndrome where the study was performed; signature of consent to participate in the research; and committed to maintaining postoperative follow-up of the above mentioned center during the first year after surgery.
Exclusion criteria were patients with diseases that significantly interfere with metabolism, including hyperthyroidism (levels of thyroid-stimulating hormone < 0.01 μIU/mL); malignant tumor disease; use of immunosuppressants; Cushing’s syndrome (suspected or chronic use of corticosteroids); and patients with conditions that impede the execution of bioelectrical impedance (tests should be performed in an environment with a temperature of 20–25 °C, the patient should not perform strenuous exercise before the test, take the test after a bath or sauna, have metal parts, have a pacemaker or other electromedical equipment, weight > 250 kg, be less than 95 cm in height, no menstrual measurements should be taken, and amputated).
Based on the inclusion and exclusion criteria, a sample of 50 patients was reached. Patients underwent routine care before and after the bariatric surgery. All patients followed the dietary guidelines of the nutrition team. Patients were evaluated before RYGBP (between 1 and 7 days prior to the procedure), and in periods of 1, 3, 6, and 12 months postoperatively, with acceptance of deviations of 10 days of the assessment date.
The following parameters were assessed by the researcher of the study:
-
1.
Height: to measure the height, Tonelli model of stadiometer was used. During the procedure, the patient was standing with his back facing the marker, feet closed together, faced forward, and arms placed at the sides. The measurement was made to the nearest centimeter, when the horizontal rod of the vertical scale bar leaned against the head.
-
2.
Analysis of body composition: weight (kg), body mass index (BMI) (kg/m2), body water (L), protein (kg), minerals (kg), bone mass (kg), body fat mass (kg), percent fat mass (%), lean body mass (kg), skeletal muscle mass (kg), waist-to-hip ratio, and basal metabolic rate (kcal).
These parameters were estimated using multifrequency tetrapolar bioelectrical impedance analysis (BIA) method with eight tactile electrodes (equipment InBody 520-Biospace®) which are already used in research worldwide. According to the BIA principle, the mineral mass cannot be calculated in a direct way and that presented by the InBody520 is an estimated value. However, a comparative experiment with DEXA shows a very high correlation so that it can be utilized as a primary screening data.
-
3.
Laboratory tests: for all periods of bioelectrical impedance evaluation, routine laboratory tests were performed and test results of blood serum albumin, total cholesterol, high-density lipoprotein HDL cholesterol, and triglycerides levels were recorded.
For data analysis, the parameters were recorded in a worksheet and exported to a Statistical Package for Social Sciences for statistical analysis. Quantitative variables were expressed as mean and standard deviation and compared between groups by Student’s t test for independent samples (symmetrical distribution). Quantitative variables were compared over time by analysis of variance for repeated measures followed by the Bonferroni test for multiple comparisons. Categorical variables were expressed as frequencies and percentages. To evaluate the correlation between quantitative variables, Pearson’s correlation coefficient test was used. Significance level was set at 5% (p ≤ 0.05).
The project was submitted to the Ethics Committee in Research and was approved (PUCRS-CEP 09/04544). Informed consent was obtained from all individual participants included in the study.
Results
In total, 50 patients were selected and three patients who abandoned follow-up with the team during the first postoperative year were excluded from the study. Out of 47 patients evaluated, 41 (87.23%) were female patients, 26 (55.31%) had health insurance plans, and 21 (44.68%) were patients of the Unified Health System (SUS, Ministry of Health, Federal Government of Brazil). The average age was 38 ± 10.6 years.
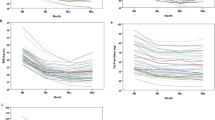
The results of body composition assessment with segmental multifrequency tetrapolar BIA in patients undergoing RYGBP surgery showed significant changes in the variables analyzed during the first postoperative year (Table 1).
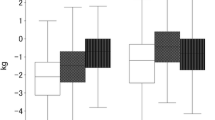
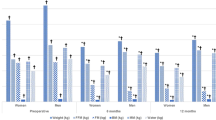
The results were as follows: total body weight reduced by 34.69%, lean body mass (LBM) decreased by 21.70%, skeletal muscle mass (SMM) decreased by 18.80%, the body fat mass decreased (BFM) by 78.39%, and percent fat mass (PFM) reduced by 27.71%. The reduction rate of BFM was more significant than the reduction rate of LBM; consequently, PFM was lower than before surgery was achieved resulting in a qualitative improvement in the proportion between LBM and BFM.
The LBM comprises all our vital organs, bones, fat-free muscles, and water. The term SMM refers only to muscles that you can actively grow and develop through proper exercise and nutrition. SMM is indeed a different type of mass from your LBM, but is part of LBM.
With weight reduction, the mean BMI also reduced to 30.0 ± 4.8 kg/m2, changing the classification of obesity grade III to grade I. Some variables have been more unstable during the year, not showing significance during all periods of evaluation (Bonferroni test, which verified the significance between the intervals). The variables, including weight, BMI, FM, PFM, and waist-to-hip ratio, had a continuous reduction in their values with statistical significance throughout the study period. The variables, including body water, body protein, LBM, SMM, and basal metabolic rate (BMR), behaved similarly to each other.
Their values significantly reduced until the sixth month postoperatively and then stabilized leading to no statistically significant difference in reduction between them. The components of minerals and bone mass variation evaluated by bioelectrical impedance were irregular and low quantitative values of mineral and osseous compartments were obtained over time. Serum albumin had no statistical significance in any evaluation period. Total cholesterol levels reduced significantly by the third month postoperatively and later showed elevation. A decrease in serum levels of HDL cholesterol was observed in the first month after surgery, which then increased continuously while blood levels of triglycerides gradually decreased. Thus, a reduction in total cholesterol and triglycerides was present while there was an increase in HDL cholesterol levels.
A statistically significant difference in the change of PFM was observed between the sexes, while the other variables showed no significant differences. This result shows that men achieve a greater reduction in the percent fat mass (Table 2).
The reduction in weight (p = 0.021), BMI (p = 0.043), body water (p = 0.000), protein (p = 0.000), SMM (p = 0.000), and BMR (p = 0.022) that occurred in patients subsidized by the Unified Health System (SUS, Ministry of Health, Federal Government of Brazil) is significantly more pronounced (Table 3).
The study does not show a strong correlation between age and variables. However, it shows that age has a slight influence on weight and BMI. This relationship between age, weight, and BMI is more pronounced on LBM and SMM.
Discussion
Body mass index is an analytical method, not laboratory method, which allows the indirect assessment of body composition. Its great advantage is the ease of application and data collection. In many situations, the BMI does not express the health state of the body. In order to create a more accurate assessment, new methods for body composition analysis have been developed. Modern technologies in science allow an increase in accuracy of equipment used in this area. Equipment for assessing body composition is more accurate and complete which allows a better and more effective performance of the health professional. The LBM consists of a variety of components that should not be overlooked during the assessment of body composition in weight loss processes in order not to compromise physiological functions [4].
The BIA is widely used as a method for assessing body composition because of its technical simplicity, high reproducibility, noninvasive method, and relatively low cost. The first BIA method was monofrequencial, 50 kHz, making it ineffective in detecting different cell sensitivities in water power. Leal et al. in 2011 described limitations of the monopolar method, especially in the male sex. The new generation of bioelectrical impedance devices sought to remedy these discrepancies, as InBody520®, which shows excellent correlation when compared with magnetic resonance imaging (MRI), as shown in the validation study [5]. InBody520® adopts the method of multifrequency analysis using three different frequencies (5 kHz, 50 kHz, and 500 kHz) that allow measurements of internal and external cellular water, proteins, minerals, and fat.
The validity of bioelectrical impedance to detect changes in body composition in intervention programs was found in a study of Jebb et al. [6]. The segmental tetrapolar multifrequency BIA presented satisfactory results when evaluating patients undergoing weight loss, being a useful method for assessing fat mass, fat-free mass, and percent fat mass. Moreover, it is an appropriate method to assess the segmental distribution of lean body mass compared with dual-energy X-ray absorptiometry (DEXA) [7, 8]. Deurenberg et al. [9] observed measurement errors in single-frequency BIA with increased physical variability of the population. Several studies reveal that the accuracy of the multifrequency BIA with eight-electrode estimate is high and it can accurately estimate the body of obese individuals and athletes [10, 11]. Stolarcczyck [12] showed that tetrapolar BIA produces estimates with smaller errors when compared with other methods. Within the protocol of our healthcare service among existing methodologies, we opted for assessment of body composition using segmented tetrapolar multifrequency BIA (InBody520®), which is an accessible, science-based technology that is compatible with the population used.
Olbers et al. [1] compared techniques of bariatric RYGBP surgery (37 patients) with vertical sleeve gastrectomy (VSG) (46 patients) by evaluating patients preoperatively and 1 year after surgery. Body composition was assessed using DEXA and tomography scans and the basal metabolic rate was assessed using indirect calorimetry and nutritional status. They concluded that patients undergoing RYGBP surgery showed better results in relation to body composition, including reduced weight, BMI, waist-to-hip circumference, and FM (26.9 kg). There was also a reduction of 90 g in bone mass. In VSG, there was an increase in bone mass (50 g). Basal metabolism decreased in both techniques (VSG, 481 kcal and RYGBP, 498 kcal). The patients who underwent RYGBP in our department also had a significant improvement in their body composition: reduced weight, BMI, waist-to-hip circumference, and FM (34.1 kg). Additionally, there was a reduction in bone mass (100 g) and basal metabolism (215.90 kcal), remembering that these are estimated values. The results corroborate those of Olbers et al. [1]. RYGBP and VSG were compared on the basis of their performance in improving body composition. The VSG is a restrictive technique that leads to a significant reduction of ghrelin hormone. The smaller stomach causes the patient to feel less hungry and full sooner while eating, thus reducing food intake and leading to significant and rapid weight loss. RYGBP is characterized by a mixed surgery, based on food restriction and derivation of gastrointestinal absorption, reducing the area of nutrient absorption.
Thus, as is known, the more efficient surgical procedure for weight reduction requires a greater nutritional care to avoid malnutrition. The biliopancreatic diversion and RYGBP surgeries result in greater influence on the percentage of fat-free mass than gastric band [13]. This was also a conclusion of a study by Chaston [13] where the gastric band was described as a purely restrictive technique.
The anthropometric results obtained in the study showed significant changes in all variables during the first postoperative year. The study design of our study was similar to that of Palazuelos-Genis et al. [14]; 50 patients, RYGBP technique, postoperative control of 1 year, and bioelectrical impedance method of evaluation (Tanita) were used in both studies. The authors expressed their data as mean and standard deviations. The weight of 1-year pre- and postoperation was 148.9 ± 21.8/93.8 ± 11.2 kg in men and 111.1 ± 13.6/72.5 ± 11.5 kg in women, obtaining a mean weight of 130/83.15 kg. Rates similar to those were obtained in this study with 124.8 ± 25.6/81.5 ± 15.6 kg and to the values of Das et al. [2] 124.3 ± 24.1/79.6 ± 19.1 kg. It is important to note that Das et al. [2] carried out the study in 20 female patients undergoing RYGBP procedure and evaluated these patients during the first year of postoperation having as a body composition evaluation the use of plethysmography with isotope dilution (PDA). There is similarity in the results when comparing BMI, PFM, LBM, and body water content between this study and those of Palazuelos-Genis et al. [14] and Das et al. [2]. The following results were obtained before and after surgery, in this study and in the studies by Genis and Das, respectively: BMI 45.8 ± 7.5 kg/m2 to 30.0 ± 4.8 kg/m2, 44.4 ± 7.4 kg/m2 to 28.3 ± 4.3 kg/m2, and 47.8 ± 8.8 kg/m2 to 30.5 ± 7 kg/m2; PFM 51.6 ± 4.17% to 37.3% ± 7.6, 47.7 ± 5.1% to 28.8 ± 8%, and 51.4 ± 3.6% to 34.6 ± 9.3%; LBM 56.9 ± 11.4 to 47.5 ± 9.5 kg, 68.4 ± 6.3 kg to 59.5 ± 6.85 kg, and 60.0 ± 9.5 kg to 50.9 ± 7.7 kg; body water 44.4 ± 9.0 kg to 37.4 ± 7.4 kg, 50.12 ± 4.38 kg to 43.74 ± 4.17 kg, and 45.5 ± 7.3 kg to 38.2 ± 5.8 kg. Dietary guidelines and postoperative conducts for patients differ minimally when they follow the recommendations of the International Federation of Obesity Surgery (IFSO), which allows patients to evolve postoperative in a similar way. Study designs differ in the routine evaluation of the data. In this study, patients were evaluated preoperatively and after the procedure in five distinct stages: the first, third, sixth, ninth, and twelfth month after surgery. In other studies, the postoperative evaluation was performed only 1 year after the completion of procedure. The results are quite consistent with the results of the study by Das et al. [2]; although only female patients participated in the study by Das, their analysis is believed to be very accurate because of the reference method used, the plethysmography displacement of air with isotope dilution. The method used in the study by Das et al. [2] reinforces the estimates provided by InBody520®. Palazuelos-Genis et al. [14] also reported a finding of greater reduction in weight and body fat mass in male patients. Additionally, there were a lot of similarities in the reduction of lean body mass between the sexes. In our patients, the differences in variables between the two sexes were also assessed; a statistically significant difference was observed only for the percent fat mass. This demonstrated that men reach a better ratio between the body components, i.e., a better body composition. Whenever we evaluated morbidly obese patients that were operated on, we observed that more than 80% of the patients were women, which may hinder statistical analyses. Our study evaluated only six men and, even with the small population size, we observed a statistically significant difference. The limitation of mono-circumferential bioelectrical impedance in men was highlighted by Leal et al. However, we did not find any studies that show the same limitation when using multifrequency bioelectrical impedance.
Madan et al. [15] evaluated 151 patients that underwent RYGBP. The evaluation was performed using bioelectrical impedance (Tanita) at five distinct periods: preoperatively, and one, three, six, and 12 months postoperatively. Thus, the study design was similar to that used in this study, allowing the evaluation of experimental data at different times. Patients in our department were evaluated preoperatively and after the procedure at five distinct stages: the first, third, sixth, ninth, and twelfth months. There are similarities in results when comparing FM, PFM, body water, and waist-to-hip ratio between this study and that of Madan et al. [15]. The comparison of the results obtained in our study (A) and in Madan et al. (B), respectively, is presented for each variable with the result in the different evaluation periods: preoperatively and at one, three, six, and 12 months postoperatively:
-
FM: (A) 64.7, 58.6, 49.0, 40.7, and 30.6 kg; (B) 64.0, 57.0, 46.0, 35.0, 30,0 Kg;
-
PFM: (A) 51.6, 50.8, 47.8, 43.9, and 37.3%; (B) 49.0, 48.0, 43.0, 37.0, and 35.0%;
-
Body water: (A) 44.4, 41.3, 39.4, 37.8, and 37.4 kg; (B) 49.0, 46.0, 45.0, 44.0, and 42.0 kg;
-
Waist-to-hip ratio: (A) 1.1, 1.0, 1.0, 0.9, and 0.9; (B) 0.9, 0.9, 0.9, 0.85, and 0.8
Evaluation of control patients at different times in both studies allowed verification of differences in variables. It appears that although there are significant variations in parameters measured preoperative and 1 year postoperative, there are moments in the course of the process of stagnation, with no statistical significance between them.
Weight, BMI, FM, PFM, and waist-to-hip ratio reduced during the entire study period reaching statistical significance. Body water, body protein, LBM, SMM, and basal metabolism behaved similarly to each other; their values decreased significantly until the sixth month after surgery. The abovementioned variables that maintain continuous significant decrease of their values are related to disease state and the major focus is on reducing these values. In contrast, the variables that stabilize after 6 months are all linked with the healthy state. Early in the process of slimming, the body will always lose lean body mass reaching equilibrium later. Therefore, it is a good indicator of halted dramatic decrease in basal metabolism but continuous fat loss allowing reduction in body fat percentage and improved quality of body composition. Thus, metabolic diseases associated with excess body fat tend to improve as well as metabolic and physiological functioning of the body. With the reduction of the decline in basal metabolic rate and fat-free mass, weight maintenance becomes more stable in the long run [13, 16]. We aim to improve the health conditions of patients, largely through the developments in this process.
Caloric restriction often used in clinical and surgical weight reduction programs alone or in conjunction with other process components can also cause the decrease of FM and loss of LBM [16, 17]. Caloric restriction in patients undergoing surgery is severe, which raises concerns about the development of free body fat component. Lean body mass is the main determinant of basal metabolism, corresponding to 70% of it [18]. Basal metabolism, in the process of weight loss, has been named as one of the factors that hinder preservation of body weight loss after surgery and further process of weight loss [19, 20]. These factors justify the studies aiming to preserve LBM or mitigate its loss during the treatment [17]. The desirable outcome in any weight control program in obese people is the reduction of FM, promotion of LBM maintenance, and an increase in BMR.
Some authors suggest an acceptable degree of LBM reduction during weight loss [21]. Prentice et al. [21] suggested the reason for the FM loss of 75% and LBM loss of 25% in obese individuals. Thus, it is suggested that a loss of 20 to 30% of LBM is acceptable when reducing weight [19]. In this study, the weight loss achieved a sustained rate of 21.70% reduction in LBM and 78.39% reduction in FM. This result showed the efficiency of the surgical procedure for weight reduction and the clinical protocol followed by the staff of our department for follow-up of their patients. Thus, when the patient gains SMM, the BMR increases.
In the current study, modifications in weight, BMI, body water, protein, SMM, and basal metabolic rate were significantly more pronounced than in patients subsidized by the Health System of the Government of Brazil, which seems to refer to the socioeconomic interferes in the postoperative course. This might lead to a worse long-term outcome. It may be a consequence of food quality maintained by these patients [22,23,24,25]. Our study failed to evaluate the patient’s stratification of salaries; however, in our setting, patients using the Unified Health System had a markedly lower financial condition than people with better social and economic conditions. According to Schiavo, Lunardelli, and Oliveira [26], there is a roughly inverse relationship between levels of triglycerides and HDL, so that high triglyceride levels tend to be associated with low HDL levels, which corroborates with the findings in our service. In this study, total cholesterol reduced dramatically by the third month postoperatively and later demonstrated a certain elevation. Serum levels of HDL decreased during the first month after surgery and then continuously increased, while blood levels of triglycerides showed a gradual reduction. Changes observed in blood lipids demonstrate improvement in the metabolic behavior of the organism, including reduced values of the most harmful blood lipids in conjunction with the largest excess body fat loss and increase in HDL cholesterol, which in turn improves quality of life.
In their study, Santos et al. [27] concluded that although serum albumin is a parameter commonly used as a marker of nutritional status of hemodialysis patients, it must be associated with other nutritional indicators. During the evaluation of patients in our department, serum albumin did not change significantly. In clinical practice, a bariatric patient’s albumin level is used as a marker of protein malnutrition and, based on their values, supplementation is imposed. Although bariatric patients in the study have shown an adequate proportion of lean body mass loss in relation to body fat, there was a significant loss of body components suggesting that albumin should not be supported in measuring protein malnutrition because it is a predictive marker of a state of inflammation that contemplates obese patients and surgical procedures.
Studies of body composition are becoming more important in clinical practice. A choice of science-based, high-quality analysis method is essential for a proper professional performance. Obesity is growing at alarming levels; therefore, there are serious chronic patients that should be evaluated in detail to propose the most appropriate treatment and monitoring system. The ultimate goal of treatment is for it to be successful and to meet the following criteria: satisfactory weight loss, loss of maintenance and preservation of health, seeking to avoid nutritional deficiencies, obesity-related and clinical treatment, and/or surgical treatment of obesity [28].
The changes in the body composition of the patients evaluated by the tetra electrical bioelectrical impedance (InBody520®) during the first year of RYGB post-bariatric surgery were statistically significant indicating the surgical efficacy of the patients monitored by the Center for Obesity and Metabolic Syndrome where the study was performed. The results of the variables examined favor a better prognosis of health and better maintenance of the weight in the long term. In addition, the quality of body composition improved. Special attention should be given to patients in the Unified Health System so that they have better access to adequate food in order to promote more positive results than those currently achieved.
References
Olbers T, Björkman S, Lindroos A, et al. Body composition, dietary intake, and energy expenditure after laparoscopic Roux-en-Y gastric bypass and laparoscopic vertical banded gastroplasty: a randomized clinical trial. Ann Surg. 2006;244:715–22.
Das SK, Roberts SB, Kehayias JJ, et al. Body composition assessment in extreme obesity and after massive weight loss induced by gastric bypass surgery. Am J Physiol Endocrinol Metab. 2003;284(6):1080–8.
Biospace Co. Ltda. Manual InBody520®. 1996–2005 All rights reserved.
Heyword VH, Stolarczyk LM. Applied body composition assessment. Hum Kinet. 1996:21–43.
Thomas EL, Frost G, Harrington T, et al. Validation of ‘InBody’ bioelectrical impedance by whole body MRI. Laboratory Report. 2001;
Jebb SA, Siervo M, Murgatroyd PR, et al. Validity of the leg-to-leg bioimpedance to estimate changes in body fat during weight loss and regain in overweight women: a comparison with multi- compartment models. Int J Obes. 2007;31:756–62.
Alvarez VP, Dixon JB, Strauss BJ, et al. Single frequency bioelectrical impedance is a poor method for determining fat mass in moderately obese women. Obes Surg. 2007;17(2):211–21.
Salmi JA. Body composition assessment with segmental multifrequency bioimpedance method. J Sports Sci Med. 2003;2(Suppl.3:1–29.
Deurenberg P, van der Kooy K, Leenen R, et al. Body impedance is largely dependent on the intra- and extra-cellular water distribution. Eur J Clin Nutr. 1989;43:845.
Demura S, Sato S, Kitabayashi T. Percentage of total body fat as estimates by three automatic bioelectrical impedance analyzers. J Physiol Anthropol Appl Hum Sci. 2004;233:93–9.
Deurenberg P. Limitations of the bioelectrical impedance method for the assessment of body fat in severe obesity. Am J Clin Nutr. 1996;64(Suppl.3:449S–52S.
Stolarczyk LM, Heyward VH, Loan MDV, et al. The fatness-specific bioelectrical impedance analysis equations of Segal et al: are they generalizable and practical? Am J Clin Nutr. 1997;66(1):8–17.
Chaston TB, Dixon JB, O’Brien PE. Changes in fat free mass during significant weight loss: a systematic review. Int J Obes. 2007;31(5):743–50.
Palazuelos-Genis T, Mosti M, Sanches S, et al. Weight loss and body composition during the first postoperative year of a laparoscopic Roux-en-Y gastric bypass. Obes Surg. 2008;18:1–4.
Madan AK, Kuykendall S, Orth WS, et al. Does laparoscopic gastric bypass result in a healthier body composition? An affirmative answer. Obes Surg. 2006;16:465–8.
Disschuneit HH, Flechtnes-Mors M, Johnson TD, et al. Metabolic and weight loss effects of a long-term dietary intervention in obese patients. Am J Clin Nutr. 1999;69:198–204.
Garrow JS, Summerbell CD. Meta-analysis: effect of exercise, with and without dieting, on body composition of overweight subjects. Eur J Clin N. 1995;49:1–10.
Van Gemert WG, Werterterp KR, Van Acker BAC, et al. Energy, substrate and protein metabolism in morbid obesity before, during and after massive weight loss. Int J Obes. 2000;24:711–8.
Marks BL, Ward A, Morris DH, et al. Fat free mass is maintained in women following a moderate diet and exercise program. Med Sci Sports Exerc. 1995;27:1243–51.
Ballor D, Poehlman ET. A meta-analysis of the effects of exercise and/or dietary restriction on resting metabolic rate. Eur J Appl Physiol. 1995;71:535–42.
Prentice AM, Oldberg GR, Jebb AS, et al. Physiological responses to slimming. Proc Nutr Soc. 1991;50:441–58.
Molarius A, Seidell JC, Sans S, et al. Educational level, relative body weight, and changes in their association over 10 years: an international perspective from the WHO MONICA Project. Am J Public Health. 2000;90(8):1260–8.
Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. Am J Clin Nutr. 2004;79(1):6–16.
Drewnowski A, Darmon N. The economics of obesity: dietary energy density and energy cost. Am J Clin Nutr. 2005;82(1):265S–73S.
Galobardes B, Costanza MC, Bernstein MS, et al. Trends in risk factors for lifestyle-related diseases by socioeconomic position in Geneva, Switzerland, 1993–2000: health inequalities persist. Am J Public Health. 2003;93(8):1302–9.
Schiavo M, Lunardelli A, Oliveira JR. Influência da dieta na concentração sérica de triglicerídeos. Jornal Bras de Patologia e Medicina Clínica e Laboratorial. 2003;39(4):283–8.
Dos Santos NSJ, Draibe AS, Kamimura MA, et al. Albumina sérica como marcador de pacientes em hemodiálise. Rev Nutr Campinas. 2004;17(3):339–49.
Leite S et al. Nutrição e cirurgia bariátrica. Rev Bras Nutr Clin. 2003;18(4):183–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Statement of Informed Consent
Informed consent was obtained from all individual participants included in the study and only the patients who agreed to participate were included.
Ethical Approval
All procedures of the study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
de Paris, F.G.C., Padoin, A.V., Mottin, C.C. et al. Assessment of Changes in Body Composition During the First Postoperative Year After Bariatric Surgery. OBES SURG 29, 3054–3061 (2019). https://doi.org/10.1007/s11695-019-03980-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-03980-8