Abstract
Background
This investigation assessed the long-term outcome of patients with gastric banding implanted more than 10 years ago.
Methods
A total of 73 patients undergoing laparoscopic gastric banding between 1997 and 2003 were identified. Patients who had their band removed were converted to a laparoscopic gastric bypass procedure.
Results
The mean preoperative body mass index (BMI) was 44.4 (SD 5.3). The mean follow-up was 11.6 (SD 2.1) years. The reasons for reoperation were leakage (N = 16, 21.9 %), slipping (N = 15, 20.5 %), and insufficient weight loss (N = 9, 12.3 %). The band was left in situ in 33 patients (45.2 %). The 5- and 10-year survival rates for the banding were 82.2 % (95 %CI 73.9–91.5 %) and 53.4 % (95 %CI 43.1–66.2 %). Best results were observed in male patients (10-year survival rate 76.5 %, 95 %CI 58.7–99.5 %, HR = 0.44, P = 0.043) and patients older than 50 years (10-year survival rate 63.8 %, 95 %CI 51.5–79.2 %, HR = 0.41, P = 0.006). Overall, the BMI was 31.0 (SD 6.3) at follow-up, excess weight loss was 68.1 % (SD 26.4), and the score for the Moorehead-Ardelt Questionnaire was 1.6 (SD 1.0). Similar results were obtained for patients with and without banding failure.
Conclusion
The present investigation provides evidence that gastric banding remains effective after more than 10 years in less than 50 % of initially operated patients. Older (>50 years) and male patients seemed to maintain the banding as long-time carriers with good results, and these patients subjectively profited from this method. Good results can be achieved if patients are followed thoroughly, and alternative surgical options for patients who fail may be offered with longstanding success.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Laparoscopic gastric banding, especially in Europe, was a breakthrough for bariatric surgery more than 10 years ago. Currently, this predominantly restrictive bariatric procedure does not play an important role, and it has gradually been replaced by other techniques, such as sleeve gastrectomy and Roux-en-Y gastric bypass [1]. Many enthusiastic reports and promising publications were published during the 1990s and later, when gastric banding was compared to precedent operative techniques (e.g., vertical banded gastroplasty). However, most of the published data only report 2- and 5-year follow-up results. Only a few studies published a follow-up of more than 10 years [2–6]. This lack of data is likely due to the recommendation of many national regulations to follow-up these patients for 5 years or less (www.smob.ch). Bariatric surgery has been performed for more than 20 years in our bariatric reference center and university teaching hospital. We have always periodically monitored and documented all patients’ physical data in our outpatient clinic. This study retrospectively analyzed the clinical outcome of 73 patients who underwent laparoscopic gastric banding 10 or more years ago. When we successfully introduced subsequent new techniques such as laparoscopic gastric bypass, we initially hypothesized that gastric banding procedures would remain a good choice for a subgroup of patients, generally young women with a body mass index (BMI) < 45 kg/m2 and big eaters.
This analysis investigated whether this initial hypothesis remained true by assessing the health of patients who have been supported and followed thoroughly, as proposed by Dixon [7] and other groups. We identified problems that occurred over the long-term after banding procedures and the time points at which these problems arose. The influence of these problems on patients’ quality of life was also examined. Differences between patients who maintained the gastric band and patients who had it removed and replaced by another bariatric procedure were compared.
Patients and Methods
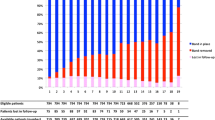
The present retrospective study was based on the bariatric database of the Kantonsspital Frauenfeld. Overall, 100 patients undergoing laparoscopic gastric banding between January 1997 and December 2003 were identified. In-hospital mortality did not occur in these 100 patients. Patients were followed on a regular basis after discharge with annual visits in the outpatient clinic. Twenty-seven patients were lost to follow-up, and these patients did not respond to the actual questionnaire. Therefore, a total of 73 patients remained for further analyses.
Data Collection and Definitions
Data on patient demographics, comorbidity, postoperative mortality, and morbidity were obtained from medical charts. Follow-up data were obtained from annual outpatient clinic reports. An actual questionnaire that included the Moorehead-Ardelt quality of life questionnaire [8] was sent to the patients for this study.
Experienced bariatric surgeons performed or supervised all banding surgeries. An adjustable silicon gastric band (Swedish adjustable gastric banding (SAGB): OBTech, Zug, Switzerland) was implanted laparoscopically using a pars-flaccida technique. To prevent slipping, sutures were placed between the gastric pouch and the gastric fundus. The subcutaneous reservoir was positioned on the upper part of the rectus abdominis muscle, and it was filled 6 weeks after surgery in the outpatient clinic. Subsequently, patients were seen after 3, 6, 12, 18, and 24 months and thereafter every year. If patients reported problems with the adjustment of the band, they were seen on extra appointments. Patients who had a failure of the banding because of slipping, leakage, or insufficient weight loss had their band removed, and these patients were converted to a laparoscopic proximal gastric bypass procedure as described by Whitgrove and Clark [9]. Patients were not advised to convert to a gastric bypass with levity. For weight regain, the conservative support with dietary counseling and band adjustments was always the first choice. Revisions for leakages at the port or tubing system are not reported and were fixed by replacement of the port reservoir. Especially in cases of a first leakage in the intraabdominal banding system (not the port or tubing system), rebandings were also performed. For slippages, rebandings have been performed as well.
Statistical Analysis
Statistical analyses were performed using R statistical software (www.r-project.org). A two-sided P value <0.05 was considered statistically significant. Continuous data are expressed as means ± standard deviation. Chi-squared tests and Mann–Whitney U tests were used to compare proportions and continuous variables, as appropriate. Missing data were imputed using the random survival forest method [10].
Failure of gastric banding was assessed as time-to-event data beginning on the date of the operation. Any subsequent conversion from band to bypass was counted as an event.
First, survival of the banding was assessed using a univariate Kaplan–Meier analysis. Thereafter, age, gender, grade of obesity, BMI, maximum weight, excess weight, and comorbidities (risk set) were assessed as potentially prognostic factors for banding survival using Cox regression analysis. Finally, the risk set was included in multivariate logistic regression as a sensitivity analysis to predict the failure of gastric banding (coded as a binary variable).
Results
Objective Outcomes
The analysis was based on 73 patients who underwent laparoscopic gastric banding between 1997 and 2003 at the Kantonsspital Frauenfeld. The mean follow-up time was 11.6 ± 2.1 years, with a range of 9 to 13 years. The band was definitely removed in 40 patients (54.8 %), and a gastric bypass procedure was performed. The reasons for band removal were leakage (N = 16, 21.9 %), slipping (N = 15, 20.5 %), and insufficient weight loss (N = 9, 12.3 %).
In a total of seven patients, conversion to a gastric bypass was the second revisional operation. In two patients who had a rebanding previously for slipping and leakage, a gastric bypass was performed because of insufficient weight loss. In five patients previously revised with a rebanding for leakage (n = 4) and slipping (n = 1), the gastric bypass was performed because of a second leakage.
The band was left in situ in 33 patients (45.2 %) at the end of follow-up. Table 1 summarizes the characteristics of patients with and without band removal and outlines the lack of significant differences between these groups, except for age and gender.
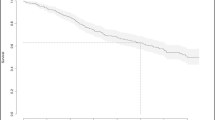
The 5- and 10-year survival rates for the gastric banding group were 82.2 % (95 %CI 73.9–91.5 %) and 53.4 % (95 %CI 43.1–66.2 %), respectively (Fig. 1). Band removal for leakage and slipping occurred over the entire timeframe, but band removal because of insufficient weight loss occurred 5 years postoperatively and later.
Multivariate Analysis
Table 2 summarizes the multivariate analysis for survival of the gastric banding. The failure rate of gastric banding depended on gender and age but not on the measurements of preoperative weight or covariates. The risk of band removal was reduced by 59 % for patients aged 50 years or more (hazard ratio [HR] = 0.41, 95 %CI 0.22–0.77, P = 0.006) and 56 % in male patients (HR = 0.44, 95 %CI 0.18–1.05, P = 0.043). Figure 2 displays the time course of band survival according to age and gender. The 5- and 10-year survival rates of gastric banding for patients aged less than 50 years (N = 47) were 69.2 % (95 % CI 53.6–89.5 %) and 34.6 % (95 % CI 20.4–58.7 %), respectively, compared to 89.4 % (95 % CI 81.0–98.6) and 63.8 % (95 % CI 51.5–79.2 %), respectively, in patients aged 50 or more years (N = 47). The 5- and 10-year survival rates of gastric banding in female patients (N = 56) were 80.4 % (95 % CI 70.6–91.5 %) and 46.4 % (95 % CI 35.0–61.5 %), respectively, compared to 88.2 % (95 % CI 74.2–100.0 %) and 76.5 % (95 % CI 58.7–99.5 %), respectively, in male patients (N = 17). The fraction of male patients did not differ significantly for the two age groups (N = 7/26 vs. 10/47, P = 0.594), which precluded colinearity because the main cause for the dependency of banding survival was age and gender. Logistic regression for sensitivity analyses that ignored the time-to-event character of the data confirmed gender and age as significant predictors of band removal. The odds ratios for patients aged 50 years or older were 0.21 (95 % CI 0.06–0.64, P = 0.005) and 0.25 for male patients (95 % CI 0.06–0.83, P = 0.023).
Survival of gastric banding according to gender and age. This figure displays the Kaplan–Meier curves according to age (left panel) and gender (right panel). Also depicted are the hazard ratios and P values in the multivariate Cox regression. The number of patients at risk is depicted below each figure
Subjective Outcomes
Table 3 depicts the subjective outcome measures. Patients with and without band removal did not differ in subjective symptoms of dysphagia, reflux, regurgitation, and the frequency of vomiting per month. Patients with and without band removal did not differ in their overall or subscale scoring on the Moorehead-Ardelt quality of life questionnaire. The overall quality of life was good on average and in the subscales of the questionnaire, except sexual life and the approaching of food, which was scored as a fair to good quality of life.
Discussion
The present investigation provides compelling evidence on the long-term results of laparoscopic gastric banding with a follow-up rate of 73 % over more than 10 years in our clinic. The 10-year banding survival rate was 53 %, but only 45 % of the patients kept their banding and were not converted to a Roux-en-Y gastric bypass by the end of the follow-up period.
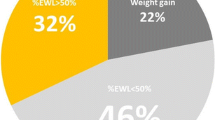
The excess weight loss (EWL) of 68 % in this study is comparable to, or higher than, other data in the literature, and more than three quarters of the patients (76 %) had an EWL >50 %, which are very good long-term results [3, 11]. Patients with gastric banding alone did not exhibit different outcomes in weight and comorbidities than patients who underwent a laparoscopic conversion of failed laparoscopic gastric banding to a Roux-en-Y gastric bypass. Our band survival rate was lower (53.4 %) than rates from previous reports, in which the graft survival of the implanted band was 85.0 % after 10 years [3]. Notably, younger and female patients more frequently had their bands removed, and older and male patients kept the banding as a stand-alone procedure, which contradicts our earlier hypothesis. No other predictive factors for band removal, such as preoperative weight or comorbidities, were found.
The good results were partially due to the thorough and continuous follow-up visits and aftercare of all patients in our bariatric program including conservative support, dietary counseling, and psychological support, which have always been considered key factors for success [7]. Therefore, patients with gastric banding should not be abandoned after 5 years because good results can be achieved beyond this point, and subsequent surgeries must be available for patients who need them beyond the 5-year time frame.
The reasons for band removals included insufficient weight loss, leakage, or slipping of the banding. Our policy to remove nonfunctioning or complication-causing bands based on the following facts: Banding is a less successful bariatric procedure in comparison to gastric bypass [12]; rebanding is as well less successful than conversion to gastric bypass[13], because of a high secondary failure rate [14]. These positions are shared by many bariatric programs worldwide, as numbers for banding procedures are decreasing globally [15].
It can be criticized that the conversion from band to bypass is the team’s subjective decision; but over the years, with the rise of gastric bypass as an alternative procedure, also patients demand for conversion was an important factor. It might seem unusual to remove the band for a leak and to convert to a bypass, but if patients additionally had esophageal dismotility disorders before, we believe that it is the right decision; as overall, banding complications after only 3 years median follow-up are reported up to 50.4 % with the same banding system [16].
Although banding procedures are declining, there are still patients successfully carrying a band. These patients are as successful as the ones after conversion to a gastric bypass procedure, because they represent a positive selection. This policy was a key factor to achieve these good results for the long-term band carriers.
The frequency of band removals for slippage and leakage were equally distributed, but band removal for insufficient weight loss tended to increase in the latter half of the 10-year time frame. Leakages and band slipping can occur any time after banding, but the acceptance for band removal and conversion to a bypass procedure because of insufficient weight loss seemed to rise over time. We hypothesize that these patients self-select themselves for a subsequent procedure, and they keep their satisfaction and quality of life at a high level (i.e., Moorehead sum score +1.6; score range from −3.0 to +3.0).
The quality of life indexes remained high even in patients who underwent a subsequent bariatric operation, and the majority of these patients considered their decision to undergo banding as the right decision. No differences in quality of life indexes were observed between band removers and continuous band carriers. Satisfaction with the placement of a gastric band was higher in this study (69 %) than previous studies (60 %) [17]. Only the patients who had a conversion of gastric banding to gastric bypass would less frequently have undergone the banding procedure again retrospectively (82 vs. 60 %; p 0.048).
In summary, this study showed that gastric bandings have continuous successful outcomes after 10 or more years. However, less than half of the gastric band patients had their bandings after this time period. This low retention percentage is the primary reason that the laparoscopic banding procedure is no longer recommended as a first-line procedure for morbid obesity. Therefore, the numbers for new band implantations are consequently decreasing [1]. Nonetheless, thousands of patients still have a band in situ. Notably, more male and older patients accounted for the group of long-term band carriers. These results might influence our follow-up programs and the aftercare of these patients in our bariatric programs, including our indication to convert banding to gastric bypass.
Conclusions
The present investigation provides compelling evidence that gastric banding is a feasible and effective method over the long-term. Older and male patients retained the banding as long-time carriers with good results and subjectively profited from this method. Good results can be achieved if patients are followed thoroughly over the long term and if other surgical options associated with longstanding success can be offered to banding patients who experience failures.
References
Buchwald H, Oien D. Metabolic/bariatric surgery worldwide 2011. Obes Surg. 2013;23:427–36.
Schwartz ML, Drew RL, Chazin-Caldie M. Factors determining conversion from laparoscopic to open Roux-en-Y gastric bypass. Obes Surg. 2004;14:1193–7.
Naef M, Mouton WG, Naef U, et al. Graft survival and complications after laparoscopic gastric banding for morbid obesity—lessons learned from a 12-year experience. Obes Surg. 2010;20:1206–14.
Reither EN, Hauser RM, Yang Y. Do birth cohorts matter? Age-period-cohort analyses of the obesity epidemic in the United States. Soc Sci Med. 2009;69:1439–48.
Spivak H, Favretti F. Avoiding postoperative complications with the LAP-BAND system. Am J Surg. 2002;184:31S–7.
Schmid C, Goede DL, Hauser RS, et al. Increased prevalence of high body mass index in patients presenting with pituitary tumours: severe obesity in patients with macroprolactinoma. Swiss Med Wkly. 2006;136:254–8.
Dixon JB, Dixon ME, O’Brien PE. Pre-operative predictors of weight loss at 1-year after lap-band surgery. Obes Surg. 2001;11:200–7.
Schwartz ML, Vaccarino F, Chacon M, et al. Chronic neonatal hypoxia leads to long term decreases in the volume and cell number of the rat cerebral cortex. Semin Perinatol. 2004;28:379–88.
Wittgrove AC, Clark GW, Tremblay LJ. Laparoscopic gastric bypass, roux-en-y: preliminary report of five cases. Obes Surg. 1994;4:353–7.
Ishwaran H, Kogalur UB. Consistency of random survival forests. Stat Probab Lett. 2010;80:1056–64.
Soteriades ES, Hauser R, Kawachi I, et al. Obesity and cardiovascular disease risk factors in firefighters: a prospective cohort study. Obes Res. 2005;13:1756–63.
Weber M, Muller MK, Bucher T, et al. Laparoscopic gastric bypass is superior to laparoscopic gastric banding for treatment of morbid obesity. Ann Surg. 2004;240:975–82. discussion 982–973.
Weber M, Muller MK, Michel JM, et al. Laparoscopic Roux-en-Y gastric bypass, but not rebanding, should be proposed as rescue procedure for patients with failed laparoscopic gastric banding. Ann Surg. 2003;238:827–33. discussion 833–824.
Muller MK, Attigah N, Wildi S, et al. High secondary failure rate of rebanding after failed gastric banding. Surg Endosc. 2008;22:448–53.
Angrisani L, Santonicola A, Iovino P, et al. Bariatric Surgery Worldwide 2013. Obes Surg. 2015.
Mittermair RP, Obermuller S, Perathoner A, et al. Results and complications after Swedish adjustable gastric banding-10 years experience. Obes Surg. 2009;19:1636–41.
Himpens J, Cadière G, Bazi M, et al. Long-term outcomes of laparoscopic adjustable gastric banding. Arch Surg. 2011;146:802–7.
Limitations
The study was a retrospective analysis.
Conflict of Interest
All authors declare that they have no conflict of interest.
Statement of Informed Consent
Informed consent was obtained from all individual participants included in the study.
Statement of Human and Animal Rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Author information
Authors and Affiliations
Corresponding author
Additional information
Martha R. Trujillo and Dominik Muller are equally contributing authors
Rights and permissions
About this article
Cite this article
Trujillo, M.R., Muller, D., Widmer, J.D. et al. Long-Term Follow-Up of Gastric Banding 10 Years and Beyond. OBES SURG 26, 581–587 (2016). https://doi.org/10.1007/s11695-015-1800-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-015-1800-x