Abstract
The regional economic burdens of obesity have not been fully quantified. This study incorporated bariatric surgery demographics collected from a large university hospital with regional economic and employment data to evaluate the cost of obesity for the South Plains region of Texas. Data were collected from patients who underwent laparoscopic gastric bypass and laparoscopic banding between September 2003 and September 2005 at Texas Tech University Health Sciences Center. A regional economic model estimated the economic impact of lost productivity due to obesity. Comparisons of lost work days in the year before and after surgery were used to estimate the potential benefit of bariatric surgery to the South Plains economy. Total output impacts of obesity, over $364 million, were 3.3% of total personal income; total labor income impacts neared $60 million: the losses corresponded to $2,389 lost output and $390 lost labor income per household. Obesity cost the South Plains over 1,977 jobs and decreased indirect business tax revenues by over $13 million. The net benefit of bariatric surgery was estimated at $9.9 billion for a discount rate of 3%, $5.0 billion for a discount rate of 5%, and $1.3 billion for a discount rate of 10%. Potential benefits to the South Plains economy of performing bariatric surgery more than outweigh its costs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rising health care costs pressure insurers, doctors, and individuals to concentrate on the economic efficacy of medical and surgical interventions. Because obesity incidence increased from 15% to 30% over the past few decades, the problem is considered epidemic [1–3]. Cost–benefit analyses of bariatric surgery require accurate assessments of obesity’s costs, e.g., the economic burdens of obesity not only include higher health care costs but also lower productivity and wages [4–9]. Several cost–benefit analyses have compared the direct and indirect costs of obesity to the benefits of various treatments [10–12]. Researchers have identified as obesity costs such things as lost days of work [13–18]. Some studies show that bariatric surgery increases quality-adjusted life years and may be cost-effective 2–3 years postsurgery [16, 19–21].
This study approaches matters from the opposite perspective by evaluating obesity’s impact on the economy of the South Plains Region of Texas. Regions differ with respect to the prevalence of obesity, the cost of and access to medical assistance, and the nature of the local economy; these variations mandate state and local studies of obesity’s costs and treatment’s benefits. Combining patient information from a large university hospital with a regional economic model permitted an estimate of the economic impact of obesity for the South Plains region in Texas. Defined in this manner, obesity’s costs were described as lost business output, employment, income, and indirect business taxes. The monetization permits region-specific cost–benefit analyses of bariatric surgery.
Methods
Acquired was demographic information for patients who underwent laparoscopic gastric bypass and laparoscopic banding at Texas Tech University Health Sciences Center (TTUHSC) between September 2003 and September 2005; the TTUHSC Institutional Review Board approved the collection of age, gender, race, and procedure. Patients resided in the South Plains region of Texas and in eastern New Mexico, an area with a similar sociodemographic and economic profile. Other information, such as annual income, occupation, and number of days absent from work, was recorded at follow-up visit and telephone interviews.
Economic impact analyses estimate direct benefits and/or costs to local, regional, or national economies of events, industries, activities, and phenomena. Total payroll spending, business or enterprise operating expenses, was first obtained. A multiplier effect, the change in income, jobs, and economic activity resulting from changes in the initial sums, can then be estimated by using an input–output (I–O) model. I–O models use margins, purchase prices for goods and services, and regional purchase coefficients, the percent of spending by local suppliers. IMPLAN modeling software [22] permits one to use data obtained from patients to estimate local economic accounts, yielding an industry-by-industry formulation of I–O accounts to calculate regional-specific multipliers. The corresponding I–O model estimated final demands, value added, output, and employment. Bureau of Labor Statistics and the Bureau of Economic Analysis data validated the results. In general, the quantity of goods and services purchased correlate with economic activity, which in turn corresponds to multiplier magnitudes. A formal description of the theory of input–output analysis can be found in a 2005 paper published in American Scientist [23]; in brief, the quantity of goods and services purchased correlates with economic activity, which in turn reflects the size of multipliers; a larger multiplier implies greater correlations between economic activity and purchases made.
Demographic observations of bariatric surgery patients, combined with measures of absenteeism and compared to that of normal-weight persons, were used to estimate lost productivity attributable to obesity. Regional worker earnings were used to monetize the lost productivity, which was then entered into the regional economic model [22].
Dollar-denominated data, including patient income, were expressed in 2008 dollars using the consumer price index. Patients residing in the Llano Estacado region of Texas, which includes the South Plains and Permian Basin, as well as parts of New Mexico, were included in the sample; persons residing within the West Texas and Eastern New Mexico region are representative of residents of the South Plains in general. Data from these persons were used to construct a South Plains I–O model and to estimate obesity’s economic impact on the South Plains economy.
The Bureau of Labor Statistics [24] reports lost work time rate due to illness or injury for full-time employed workers 16 years old and above. Lost work time rates are proportions of hours usually worked that are hours absent. Lost productivity was derived from patient and employment data, in this case being defined as days obese persons were not working beyond that of normal-weight persons, with total work days per year assumed to be 250. After-tax worker earnings were used to monetize productivity losses. Thus defined, obese worker’s decreased productivity was used to calculate obesity’s adverse economic impacts. According to regional economic data (Congressional Budget Office and US Census Table HINC-05), average worker earnings on the South Plains were $49,405, assuming an effective total federal income tax rate of 19.8%; Texas lacks a state income tax. Regional economic data may be used to extrapolate patient data on lost work days to the general population in order to monetize the lost productivity without subjecting the analysis to potential self-selection bias due to higher income or insured patients electing for surgery at a higher rate than lower income or under-insured individuals.
Economic impact analysis is generally comprised of inputs, a regional input–output model with associated multipliers, and the estimated economic impact. Figure 1 provides a schematic overview of the model used in this study. The input is the monetized earnings capacity of obese workers. The input–output model consists of region-specific multipliers computed from county-level (representative) economic characteristics and data. The estimated regional economic impact is the sum of direct productivity effects and secondary spending effects and stated in terms of losses to total output, jobs, household income, and indirect business taxes.
Bariatric surgical costs were obtained from the American Society for Metabolic and Bariatric Surgery [25]. The change in lost productivity was assessed by calculating the mean number of lost work days in the year before and the year after surgery for the patients in the study. The analysis compared the discounted present value of lost output to the cost of surgery.
Results
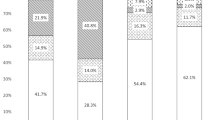
Of the 150 patients who met study criteria, 130 (87.5%) were female, 93 (62%) were Caucasian, 42 (28%) were Hispanic, seven (4.5%) were African-American, and one (0.5%) was Native American. Ages were distributed as follows: 12.6% were 20–29 years old, 28.7% were 30–39 years old, 38.5% were 40–49 years old, 18.2% were 50–59 years old, and 2.1% were 60–69 years old. Patients were diversely educated: three (1.5%) had an education up to the 11th grade, 75 (50%) completed high school, 39 (26%) had a degree from a 2- or 4-year college, 19 (13%) had a Master’s degree, two (1%) had a Ph.D., one (0.5%) had a veterinary assistant certificate, and one (0.5%) had an MD. Of the patients, 15 (10%) were homemakers; 123 (82%) were full-time employees, including 48 (32%) nurses, secretaries, or managers, seven (4.5%) supervisors, five (3%) students, six (4%) teachers, four (2.5%) customer service employees, and a wide array of other occupations.
Texas Health Institute (THI) [26] obesity prevalence rate is 27.8% (range 24.1–29.1%) for the 15-county region; this corresponds to 62,307 of the South Plains, 386,518 persons being obese workers after employment data are taken into account. THI does not provide county-level morbid obesity rates. Estimates of economic costs from obesity are based on data for morbidly obese patients, and accordingly the use of THI obesity rates may over-state the true costs. However, THI rates are based on self-reported height and weight information in the Behavioral Risk Factor Surveillance System, and this may understate the true prevalence [27]. Thus, the basic conclusions from this study are unlikely to be affected.
The average US worker loses 3.0 days of productivity per year due to illness or injury. Patients reported a median and mean of 33 (SD 10) days lost from work due to illness or injury in the year before surgery. For workers in general, the lost work time rate is 1.2% [24], equivalent to 3 days of a 250-day work year. In the year after surgery, patients reported a median 0 and a mean 1 (SD 4) days lost from work. Patient surveys were conducted on an ongoing basis where individual patient information on preoperative lost work days was collected at or near the time of surgery and information on post-operative lost work days was collected within 1 year of their surgery. Whereas average workers have 250 − 3 = 247 productive days per year, obese workers have 250 − 33 = 217 productive days; the productivity of one obese worker is 87.8% of workers in general. Self-reported data may produce bias if patients systematically under- or over-report days lost from work. Individual patient self-reporting error for pre- and post-operative days lost is assumed to be in similar direction and magnitude, resulting in mitigation of bias.
Table 1 displays costs, in terms of lost output, labor income, employment, and indirect business taxes, of obesity in the South Plains, as estimated by a regional economic model that took into account multiplier effects associated with lost productivity from obesity. Obese workers are less productive due to fewer days at work. In economic terms, the lost work time represents an opportunity cost to society in which the value of what the obese worker would have produced or the potential output foregone by using or reallocating other workers to make up for the lost work time. Total output impacts, over $364 million, were 3.3% of total personal income; total labor income impacts neared $60 million: the losses corresponded to $2,389 lost output and $390 lost labor income per household. I–O model estimated multiplier effects implied obesity cost the South Plains about 1,977 jobs and decreased indirect business tax revenues by over $13 million.
Bariatric surgery costs between $17,000 and $25,000 per procedure, with a median $21,000 total cost [25]. South Plains area bariatric surgery cost (hospital and anesthesia) was found to be around $10,000 at the facility in which patients in this study were treated [28]. Lower cost may be due to several regional factors such as degree of insurance coverage, competition, and medical infrastructure such as county hospital and university medical center. Data do not capture costs related to complications, readmissions, etc. nor do they include costs associated with missed days of work required for convalescence from surgery. Use of the national average cost data in this study is a conservative approach for evaluating the net benefits of bariatric surgery and allows for economic benefits to be independent of where surgery is performed and compensate for other unmeasured or unobservable costs. Overall, treatment costs are small relative to the economic losses of not treating obesity.
Given ongoing economic impacts, future values must be discounted to present value so that all money amounts are shown in today’s dollars and direct comparisons can be made between surgical costs (one-time sum) and benefits (ongoing gains to productivity). Table 2 shows the capitalized or present value of obesity’s costs at discount rates of 3%, 5%, and 10%, with net benefits displayed in the last column. The net benefit was $9.9 billion for a discount rate of 3%, $5.0 billion for a discount rate of 5%, and $1.3 billion for a discount rate of 10%. Figure 2 shows the relationship between net benefit from surgery and the discount rate; net benefits decline as the discount rate rises. The net benefit in today’s dollars is positive at all discount rates. Thus, economists would infer that bariatric surgery is a net gain for the region and is not dependent on the state of the regional economy.
Discussion
Utilizing bariatric surgery demographics from a sample of patients combined with regional economic data, this study estimated economic loss from diminished worker productivity and compared that loss with the net economic gain that might be acquired via bariatric surgery, taking into account the cost of the surgery. Estimated was obesity’s burden to the South Plains in terms of lost output, jobs, income, and indirect business tax revenue. Also estimated was the net benefit to the economy of performing the surgery.
Previous studies focused on obesity’s impact on wages, with somewhat mixed results, generally indicating that obese persons earn less over their lifetime than normal-weight individuals [29, 30]. Recent papers show that, for policy holders, net economic benefits from bariatric surgery appear in 4 years or less [31–33]. The current study expands this analysis, showing that bariatric surgery provides immediate benefits to the economy at large by decreasing lost work days. This analysis is a logical conclusion when one considers that multiplier effects captured in analyses of regional economic impact models confer to society benefits and costs that are much larger than those that can be ascertained from the perspective of the individual payer or patient. A regional economy that faces liquidity or borrowing constraints may lack resources to follow recommendations of such cost–benefit analyses; government intervention, in the form of added taxes or regulations, can then incentivize collective actions to obtain desired results [34].
Study results have implications for bariatric surgeons and centers. Cost–benefit estimates for bariatric surgery in this region may be extended to other areas with appropriate adjustments for regional economic multipliers and patient demographics. Estimates will become even more important as health policy moves to cost–benefit or cost-effectiveness analysis of treatment options as a decision tool, especially when alternatives are available. Bariatric practices within university medical centers and community health clinics can use these results to demonstrate the magnitude of regional net benefits. This study does not account for all the benefits from surgery; patients that had surgery experience reduced costs associated with the comorbidities from obesity. From a public health perspective, the aggregate economy benefits from a healthier population and reduced medical expenditures. The reduced medical expenditures free up household disposable income to be spent on other goods and services in the local economy, resulting in additional benefits to society.
Conclusion
Using bariatric patient data in an input–output model of the regional economy, this paper estimates the economic burden of obesity on the South Plains region of Texas and the net benefit to the region of the performance of bariatric surgery. Obesity costs the South Plains about 1,977 jobs and decreases indirect business tax revenues by over $13 million per year. Providing patients bariatric surgery would yield to the South Plains economy a benefit of between $1.3 and $9.9 billion in today’s dollars. This net benefit consists of one-time, upfront costs of surgical treatment and ongoing gains from improvements in worker productivity.
References
Flegal KM, Carroll MD, Ogden CL, et al. Prevalence and trends in obesity among US adults, 1999–2000. JAMA. 2002;288:1723–7.
Calle EE, Rodriguez C, Walker-Thurmond K, et al. Overweight, obesity and mortality from cancer in a prospectively studied cohort of US adults. N Engl J Med. 2003;348:1625–38.
Must A, Spadano J, Coakley EH, et al. The disease burden associated with overweight and obesity. JAMA. 1999;282:1523–9.
Swinburn B, Ashton T, Gillespie J, et al. Health care costs of obesity in New Zealand. Int J Obes. 1997;21:891–6.
Thompson D, Edelsberg J, Colditz GA, et al. Lifetime health and economic consequences of obesity. Arch Intern Med. 1999;159:2177–83.
Thompson D, Wolf AM. The medical-care cost burden of obesity. Obes Rev. 2001;2:189–97.
Wang G, Zheng ZJ, Heath G, et al. Economic burden of cardiovascular disease associated with excess body weight in U.S. adults. Am J Prev Med. 2002;23:1–6.
Weintraub M. Long-term weight control study conclusions. Clin Pharmocol Ther. 1992;51:642–6.
Frezza EE, Wachtel MS, Ewing BT. The impact of morbid obesity on the state economy: an initial evaluation. Surg Obes Reat Dis. 2006;2(5):504–8.
Colditz GA. Economic costs of obesity and inactivity. Med Sci Sports Exerc. 1999;31 Suppl 11:S663–7.
Wittgrove AC, Clark GW. Laparoscopic gastric bypass, Roux-en-Y—500 patients: technique and results, with 3–60 month follow up. Obes Surg. 2000;10:233–9.
Wolf AM. What is the economic case for treating obesity? Obes Res. 1998;6 Suppl 1:2S–7.
Strum R. Increases in clinically severe obesity in the United States, 1986–2000. Arch Surg. 2003;163:2146–8.
Sturm R. The effects of obesity, smoking, and drinking on medical problems and cost outranks both smoking and drinking in its deleterious effects on health and health costs. Health Aff (Millwood). 2002;21(2):245–53.
Finkelstein EA, Fiebelkom IC, Wang G. National medical spending attributable to overweight and obesity: how much, and who’s paying? Health Aff (Millwood). 2003;Jan–Jun(Suppl Web exclusives):W3-219-26.
Thompson D, Edelsberg J, Kinsey KL, et al. Estimated economic costs of obesity on business. Am J Health Promot. 1998;13:120–7.
Thorpe KE, Florence CS, Howard DH, et al. The impact of obesity on rising medical spending. Health Aff (Millwood). 2004;July–Dec(suppl Web exclusives):W4-48-0-86.
Tucker LA, Friedman GM. Obesity and absenteeism: an epidemiologic study of 10,825 employed adults. Am J Health Promot. 1998;12:202–7.
van Gemert WG, Adang EM, Kop M, et al. A prospective effectiveness analysis of vertical banded gastroplasty for the treatment of morbid obesity. Obes Surg. 1999;9:484–91.
Craig BM, Tseng DS. Cost-effectiveness of gastric bypass for severe obesity. Am J Med. 2002;113:491–8.
Clegg A, Colquitt J, Sidhu M, et al. Clinical and cost effectiveness of morbid obesity: a systematic review and economical evaluation. Int J Obes Relat Metab Disord. 2003;27:1167–77.
Olson D, Lindall S. IMPLAN user’s guide. Stillwater: Minnesota IMPLAN Group; 2002.
Bedzek RH, Wendling RM. Fuel efficiency and the economy. Am Sci. 2005;93:132–9.
Bureau of Labor Statistics. Employment and earnings. Washington, DC: Bureau of Labor Statistics; 2006. Table 46.
American Society for Metabolic and Bariatric Surgery. Fact sheet—metabolic and bariatric surgery. Gainesville: American Society for Metabolic and Bariatric Surgery; 2007.
Eschbach K. Texas Health Institute, appendix to the executive summary, findings about the obesity epidemic in Texas, Methodology statement and data tables by county. January 2009.
Flood V, Webb K, Lazarus R, et al. Use of self-report to monitor overweight and obesity in populations: some issues for consideration. Aust NZ J Public Health. 2007;24:96–9.
Frezza EE, Wachtel MS, Ewing BT. Bariatric surgery costs and implications for hospital margins: comparing laparoscopic gastric bypass and laparoscopic gastric banding. Surg Laparosc Endosc Percutan Tech. 2007;17:239–44.
Fisher BL, Schauer P. Medical and surgical options in the treatment of severe obesity. Am J Surg. 2002;184:S9.
Flum DR, Salem L, Elrod JA, et al. Early mortality among Medicare beneficiaries undergoing bariatric surgical procedures. JAMA. 2005;294(15):1903–8.
Finkelstein MM. Obesity, cigarette smoking and the cost of physicians’ services in Ontario. Can J Public Health. 2001;92:437–40.
Sampalis JS, Liberman M, Auger S, et al. Impact of weight reduction health-care costs in morbidly obese patients. Obes Surg. 2004;14:939–47.
Finkelstein EA, Brown DS. A cost-benefit simulation model of coverage for bariatric surgery among full-time employees. Am J Manag Care. 2005;11:641–6.
Frezza EE, Wachtel MS, Ewing BT. Economic considerations for bariatric surgery and morbid obesity. ClinicoEconomics and Outcomes Research. 2009;1:1–5.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ewing, B.T., Thompson, M.A., Wachtel, M.S. et al. A Cost–Benefit Analysis of Bariatric Surgery on the South Plains Region of Texas. OBES SURG 21, 644–649 (2011). https://doi.org/10.1007/s11695-010-0266-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-010-0266-0