Abstract
Background
Although weight loss before bariatric surgery may carry advantages during the surgical procedure (decreased liver volume, operation duration, and blood loss), it is still debated whether it induces a greater long-term weight loss.
Methods
We conducted a retrospective analysis over 539 patients operated by the same surgeon until September 2008. Five hundred seven primary bariatric surgical procedures were performed: gastric bypass in 381, gastric banding in 97, and sleeve gastrectomy in 29. Preoperative multidisciplinary care was similar for all the patients over a period of 12 months. Relationship between weight changes during this period and the percentage of excess weight loss (%EWL) over the 48 month after surgery was analyzed by logistic regression.
Results
No relationship could be evidenced between pre- and postoperative weight loss, regardless of the surgical technique performed. Whether patients were male or female, and whether they had an initial BMI greater or lower than 50 kg/m2, did not make a difference in the relationship between EWL at any point and weight loss prior to surgery. Despite a large range of weight changes before surgery, there was no trend for a relationship.
Conclusions
This study suggests that weight loss before surgery should not be considered a pre-requisite. Although it can reduce the difficulties of the surgical procedure, advantages for long-term weight loss are not validated.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bariatric surgery is a reliable method for long-term weight loss in morbidly obese people [1, 2]. Whereas the size of the gastric pouch, diabetes, initial BMI, and open as opposed to laparoscopic procedure are factors associated with poorer weight outcomes [3], it is still debated whether preoperative weight loss can lead to better weight loss. This hypothesis is based on the impact of behavioral changes, which are usually associated with successful long-term weight loss (for example [4, 5]).
The majority of published data (essentially on Roux-en-Y gastric bypass (RYGB)) did not show any positive impact of preoperative weight loss on the 2-year postoperative weight curve [6–13]. It is noticeable however that these studies were retrospective. Furthermore, when weight loss was a pre-requisite for surgery, no difference in postoperative percentage of excess weight loss (%EWL) was shown between those who lost or gained weight preoperatively [7, 9]. Two studies showed a positive weight outcome: one is a 6-month randomized controlled trial (RCT) with a modest benefit of pre-surgery weight loss [8] and the other is an 18-month retrospective trial where a 1% weight loss before surgery is associated with a 1.8% weight loss after surgery [14].
Only two trials have described EWL outcomes observed 24–36 months after surgery. One was negative [15], and the other found a correlation between weight loss before and after surgery without mentioning the magnitude of relationship [16].
Most of these studies involved a limited number of subjects, and only one describes results with gastric banding.
Therefore, the aim of this study was to analyze the relationship between weight changes between the first visit to the multidisciplinary team and the time of surgery, and excess weight loss from 6 to 48 months, postoperatively. Furthermore, this relationship was compared between the three surgical procedures performed (gastric banding, sleeve gastrectomy, and RYGB).
Materials and Methods
The database of the “Société de chirurgie, Clinique de l’Anjou, Angers” stores anthropometric data and details of the surgical procedure for all the patients undergoing bariatric surgery. Data of 539 patients operated by the same surgeon prior to September 2008 are available. This database was searched for patients with a primary bariatric surgery. Five hundred and seven patients were considered: 381 had RYGB, 97 had adjustable gastric banding (GB), and 29 had a sleeve gastrectomy (SG).
Patients were adults who had given informed consent for surgery. Their initial characteristics are described in Table 1.
The multidisciplinary team approach was standardized following the French recommendations for the surgery of obesity [17]. Briefly, patients were considered for surgery after an evaluation performed by a surgeon, an endocrinologist, a dietician, and a psychiatrist. The evaluation took place during an observation period of at least 12 months during which dietary counseling and recommendations for increased physical activity were given. The same recommendations were made to all the patients. Weight loss prior to surgery was neither a pre-requisite nor a contra-indication to surgery (some patients fear that surgery is not indicated if they can lose weight with non-surgical means). Indication for surgery was confirmed based on the multidisciplinary review of the 12-month evaluation. There was no formal decision tree to choose between the techniques. Before 2003, all procedures were gastric banding when we introduced RYGB. The two techniques overlapped, until sleeve gastrectomy became available. The latter technique was indicated for the first “time” of the biliopancreatic diversion and for people older than 60 years.
A single surgeon performed standardized laparoscopic procedures. RYGB was performed as previously described [18] with a mean alimentary limb of 127 ± 24 cm; the sum of the alimentary and the biliopancreatic limbs was 216 ± 34 cm. The volume of the gastric pouch was set at about 30 ml. Gastric banding was performed using the pars flascida technique with the Swedish adjustable band (Ethicon Endosurgery, Cincinnati, OH, USA). Sleeve gastrectomy was performed over a 40-Fr bougie.
Body weight was measured in light clothing at each visit. Weight was recorded at the very first visit (Wgt V1), when admitted for surgery (Wgt bef surgery), and when discharged from the clinic (Wgt disch). Patients were weighted at least every 3 months during the first year, and every 6 months thereafter, and the results were expressed as %EWL.
Calculations and Statistics
Changes in weight were calculated:
-
Between Wgt V1 and Wgt bef surgery, i.e., the changes in weight over the 12 months or so between the first contact with the team and surgery
-
Between Wgt bef surgery and Wgt disch, i.e., weight loss during the hospital stay
When one data point was missing, the closest observation in time was used.
Statistics
Results are expressed as mean ± SD. Differences were considered significant at the 5% level. Cross-sectional differences between surgical techniques were assessed by analysis of variance. Logistic regressions were performed to relate changes in weight before and around surgery to EWL over the following 48 months.
Results
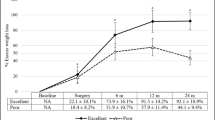
Table 1 reports weight changes before and around surgery. Weight loss before surgery was not different between surgical procedures (P = 0.094). Fig. 1 shows the postoperative %EWL according to the different techniques. As expected, %EWL increased and followed a plateau until 24 months, then started to decline, although data after 24 months were not available for the sleeve gastrectomy. %EWL was significantly greater after RYGB or SG compared to GB.
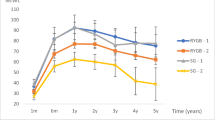
The postoperative weight loss was not correlated to the weight changes during the 12 months of the multidisciplinary evaluation (Table 2). This was also the case when the group was broken down into the three different procedures. Whether patients were male or female, and whether they had an initial BMI greater or lower than 50 kg/m2, did not make a difference in the relationship between EWL at any time point and weight loss prior to surgery. Fig. 2 illustrates that despite a large range of weight changes before surgery, there was no trend for a relationship.
The postoperative weight loss was not correlated to the weight changes during the hospital stay except at months 18, 24, and 36. The greater weight loss was during the hospital stay, and the greater excess was weight loss 18, 24, and 36 months, postoperatively. However, this relationship was weak with low R 2 (0.036 to 0.17), i.e., explaining a very modest part of the variance.
Discussion
This study, based on a large population, confirms that weight loss that may occur during the 12-month preoperative evaluation within the bariatric program is not associated with greater weight loss over 48 months following surgery.
The majority of papers investigating this question have failed to prove any advantage of losing weight preoperatively on the amount of weight lost after surgery [6, 7, 9–13, 15]. Only three studies suggested the contrary [8, 14, 16]: one in the short term (6 months [8]), one without mentioning the magnitude of the relationship [14], the last one with a follow-up of 4 years.
The present study does not show any advantage of preoperative weight loss despite large differences in weight over the 12 months preceding surgery (Fig. 2; −32 to +20 kg). Indeed, Fig. 2 suggests that no correlation exists neither for large nor small amounts of weight loss before surgery. This is confirmed by the analysis of EWL at any time point, which did not differ between the two extreme tertiles of the weight changes observed before surgery (analysis of variance, data not shown). Neither the BMI before surgery, nor gender, nor the surgical procedure influenced EWL.
The main limitation of our study is its retrospective design. It has however some strong points. The number of subjects offers a sufficient statistical power to conclude. There is a high degree of standardization in the procedures, since the multidisciplinary team has remained the same since the beginning, and the same surgeon (GB) performed all the surgeries. This study also shows that the conclusions are valid for gastric bypass and gastric banding. Finally patients were followed up to 4 years. Only one RCT was published with short-term benefits of weight loss [16]. One hundred patients were randomized prior to surgery to either a “10% weight loss” group or a group that had “no weight loss requirements.” Data were available for 26 patients in the weight loss group and 35 in the “no weight loss requirements.” %EWL was about 10% greater at 3 months in “the 10% weight loss” group but was similar at 6 months. The present study and other published reports did not include behavioral changes as a covariate. This is however one possible bias in weight outcomes since appetite sensation control and changes in physical activity are related to weight changes and weight maintenance on the long-term both with non-surgical weight loss [4] and in patients with a gastric banding [5].
We have no explanation for the weak statistical relationship between weight loss during the hospital stay and %EWL at 24 months.
Weight loss before surgery may however have some advantages. It is associated with a smaller liver volume [19], a reduction of visceral adipose tissue, and a reduction of the surgery duration and blood loss [6, 8, 11, 12, 14]. However, it does not appear to lower the rate of postoperative complications. No study has evaluated the technical ease for the surgeon.
In conclusion, this study adds some data to suggest that weight loss before bariatric surgery should not be a pre-requisite since it is not associated with better weight loss outcomes. Further well-designed and controlled studies would be necessary to investigate whether behavioral changes and their maintenance after surgery would be beneficial. In order to reduce liver volume, short-term intense calorie restrictions are equally efficient [19].
References
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292(14):1724–37.
Sjöström L. Bariatric surgery and reduction in morbidity and mortality: experiences from the SOS study. Int J Obes (Lond). 2008;32 Suppl 7:S93–7.
Campos GM, Rabl C, Mulligan K, et al. Factors associated with weight loss after gastric bypass. Arch Surg. 2008;143(9):877–83.
Teixeira PJ, Silva MN, Coutinho SR, et al. Mediators of weight loss and weight loss maintenance in middle-aged women. Obesity (Silver Spring). 2009; PubMed PMID: 19696752.
Colles SL, Dixon JB, O’Brien PE. Hunger control and regular physical activity facilitate weight loss after laparoscopic adjustable gastric banding. Obes Surg. 2008;18(7):833–40.
Huerta S, Dredar S, Hayden E, et al. Preoperative weight loss decreases the operative time of gastric bypass at a Veterans Administration hospital. Obes Surg. 2008;18(5):508–12.
Mrad BA, Stoklossa CJ, Birch DW. Does preoperative weight loss predict success following surgery for morbid obesity? Am J Surg. 2008;195(5):570–3.
Alami RS, Morton JM, Schuster R, et al. Is there a benefit to preoperative weight loss in gastric bypass patients? A prospective randomized trial. Surg Obes Relat Dis. 2007;3(2):141–5.
Carlin AM, O’Connor EA, Genaw JA, et al. Preoperative weight loss is not a predictor of postoperative weight loss after laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2008;4(4):481–5.
Fujioka K, Yan E, Wang HJ, et al. Evaluating preoperative weight loss, binge eating disorder, and sexual abuse history on Roux-en-Y gastric bypass outcome. Surg Obes Relat Dis. 2008;4(2):137–43.
Harnisch MC, Portenier DD, Pryor AD, et al. Preoperative weight gain does not predict failure of weight loss or co-morbidity resolution of laparoscopic Roux-en-Y gastric bypass for morbid obesity. Surg Obes Relat Dis. 2008;4(3):445–50.
Riess KP, Baker MT, Lambert PJ, et al. Effect of preoperative weight loss on laparoscopic gastric bypass outcomes. Surg Obes Relat Dis. 2008;4(6):704–8.
Jantz EJ, Larson CJ, Mathiason MA, et al. Number of weight loss attempts and maximum weight loss before Roux-en-Y laparoscopic gastric bypass surgery are not predictive of postoperative weight loss. Surg Obes Relat Dis. 2009;5(2):208–11.
Alvarado R, Alami RS, Hsu G, et al. The impact of preoperative weight loss in patients undergoing laparoscopic Roux-en-Y gastric bypass. Obes Surg. 2005;15(9):1282–6.
Ali MR, Baucom-Pro S, Broderick-Villa GA, et al. Weight loss before gastric bypass: feasibility and effect on postoperative weight loss and weight loss maintenance. Surg Obes Relat Dis. 2007;3(5):515–20.
Alger-Mayer S, Polimeni JM, Malone M. Preoperative weight loss as a predictor of long-term success following Roux-en-Y gastric bypass. Obes Surg. 2008;18(7):772–5.
HAS. Obésité: prise en charge chirurgicale chez l’adulte. www.has-sante.fr/portail/jcms/c_765529/obesite-prise-en-charge-chirurgicale-chez-l-adulte
Topart P, Becouarn G, Ritz P. Biliopancreatic diversion with duodenal switch or gastric bypass for failed gastric banding: retrospective study from two institutions with preliminary results. Surg Obes Relat Dis. 2007;3(5):521–5.
Colles SL, Dixon JB, Marks P, et al. Preoperative weight loss with a very-low-energy diet: quantitation of changes in liver and abdominal fat by serial imaging. Am J Clin Nutr. 2006;84(2):304–11.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Becouarn, G., Topart, P. & Ritz, P. Weight Loss Prior to Bariatric Surgery Is Not a Pre-requisite of Excess Weight Loss Outcomes in Obese Patients. OBES SURG 20, 574–577 (2010). https://doi.org/10.1007/s11695-010-0083-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-010-0083-5